Abstract
Objectives:
To evaluate levels of physical activity among physicians in Riyadh, Saudi Arabia and to study the possible factors affecting physical inactivity. In addition, the study aims to estimate the prevalence of major non-communicable diseases (NCDs) and a possible correlation between physical inactivity and major NCDs.
Method:
A cross-sectional approach was used for this study conducted on 370 randomly-selected outpatient physicians of both genders working at 4 leading healthcare institutions in Riyadh, Kindom of Saudi Arabia between December 2013 and January 2014. Using a modified World Health Organization (WHO) STEPwise questionnaire. Data was analyzed using the Statistical Package for Social Sciences version 21.
Results:
The findings of the present study demonstrated a prevalence of physical activity among Riyadh physicians (63%), which is higher than the general population (32.4%). The main reason for not engaging in physical activity was lack of time (58.1%) followed by work duties (22.5%). The prevalence of the most frequently reported NCDs (cardiovascular diseases, diabetes, chronic respiratory diseases, and cancers) was 21.9%. No significant association between physical inactivity and major NCDs among physicians in our sample was found.
Conclusion:
The participating physicians are physically active and suffer from a small percentage of the most reported NCDs. The main factor associated with physical inactivity was lack of time. No association was detected between physical inactivity and major NCDs.
Physical activity is defined as “any bodily movement produced by skeletal muscles that results in energy expenditure”.1 There are varying types of physical activities, usually classified by their effect on the heart rate and the effort required by the subject. Activities that require hard physical effort and cause a significant increase in breathing or heart rate, such as running and playing football, are known as ‘vigorous intensity activities’. Whereas activities, which require moderate effort and cause a small increase in breathing or heart rate, for example, brisk walking and swimming, are defined as ‘moderate intensity activities’.2 It has been scientifically proven that regular physical activity among all age groups has physical and mental benefits. Improvement of life quality, sleep, and stress management are some of the physical benefits; the enhancement of social relationships is a mental benefit.3 Physical inactivity is one of the most important risk factors for developing chronic diseases and increasing morbidity and mortality.4 In fact, it has been reported that (9%) of premature deaths in 2008 worldwide were associated with inactivity.5 Many important factors have been studied and reported as determinants of inactivity including insufficient time, injuries, obesity, and lack of encouragement by family and friends. Furthermore, environmental factors, such as hot weather and lack of facilities such as proper walking or jogging areas, can also affect the level of physical activity.6 Non-communicable diseases (NCDs) may be defined as a group of chronic illnesses which are not infectious or contagious in nature, and may cause disability or even premature death. They result in prolonged, slowly-progressing consequences that require long-term care. The major NCDs identified by the World Health Organization (WHO) include cancers, chronic respiratory diseases, cardiovascular diseases, and diabetes.7 Research studies and reviews indicated that NCDs are the major cause of death in the world,8,9 killing more people annually than all other causes.4 Data from a WHO study conducted in 2014 on NCDs in Saudi Arabia reported proportional mortality as follows: cardiovascular diseases (46%), cancers (10%), chronic respiratory diseases (3%), diabetes (5%), and other NCDs (14%). Compared with a total of 22% of all other causes of death, this proves that NCDs are the major causes of mortality, both nationally and internationally.10 Physical inactivity was found to be associated with an increase in the occurrence of NCDs; thus, physical inactivity contributes to deaths and disabilities.3,5 In particular, physical inactivity has major effects on the occurrence of coronary heart disease, type 2 diabetes and cancer, specifically breast and colon cancers.5 A study published in 2012 reported that (6-10%) of global deaths from NCDs were directly related to physical inactivity.5 Conversely, improvement of physical activity contributes to NCD prevention, as it is considered one of the most important risk factors.11,12 The Kingdom of Saudi Arabia (KSA) has recently experienced enormous lifestyle changes associated with less and less physical activity among large sectors of the population. These changes may be strongly related to the currently witnessed epidemic level of NCDs and their associated complications.13 Overall, (67.7%) of different age groups of the Saudi population aged 15-64 years, (60.9 %) of men and (74.3%) of women, were reported to be physically inactive according to a STEPwise surveillance in 2005.14 These statistics highlight that national physical inactivity is a serious and prevalent issue. Many national and international studies have been published on physical activity.4,13,15-17 However, there is a lack of statistics from KSA, especially among sub-population groups. Physicians are one such subgroup worth studying given that they are highly educated and supposedly more engaged in physical activity than others.6,12,18,19 Furthermore, physicians’ level of activity can improve their consultations regarding physical exercise, increase job satisfaction, and decrease rates of depression, all of which, promote patient care.20 In recent years, a local study on physical activity levels among physicians in a single center in Riyadh targeted the physicians of a residency training program.21 Moreover, despite the observed impact of physical inactivity on the occurrence of NCDs, few studies have attempted to link them. This study aims to assess the practice of and factors affecting physical activity among Riyadh physicians, to estimate the prevalence of major NCDs and test the possible association between physical inactivity and major NCD occurrence among the same group.
Methods
Search strategy
We conducted a literature search utilizing the following databases: PubMed, TRIP, and Cochrane library. The included articles were all English-language studies published in peer-reviewed journals. We found articles relevant to our objectives using the following search terms: physical activity, physical inactivity, major non-communicable diseases, cancer, diabetes, cardiovascular diseases, chronic respiratory diseases, doctors, and physicians. A total of 670 of studies were reviewed individually and 25 met our objectives.
Study design
An observational cross-sectional study design was used. The study was carried out in 2013-2014 at out-patient clinics in 4 tertiary healthcare facilities representing different healthcare delivery sectors: King Saud University hospitals, (King Khalid University Hospital [KKUH], King Abdulaziz University Hospital [KAUH]), King Faisal Specialist Hospital and Research Center [KFSHRC], and National Guard Health Affairs [NGHA], Kingdom of Saudi Arabia.
Study sample
Considering a (68%) prevalence of physical inactivity level among the Saudi population (WHO STEPwise survey, 2006), with a confidence level of (95%), and accepting a difference up to (5%), the study needed to have 336 subjects. The following equation can be applied:
n=Z2aP(1-P)/d2=1.962*0.677*(1-0.677))/0.052=336.
Adding a (10%) increment to compensate for potential non-response, the sample size was increased to 370 physicians. A simple random technique, enrolling physicians working the morning shift on Sundays, Tuesdays, and Thursdays from December 2013 to January 2014, was used.
Inclusion criteria
Male and female physicians 1) working in out-patient care in one of the previously mentioned hospitals, 2) of different professional ranks (residents, registrars, and consultants), and 3) aged 24-65 years were eligible to participate.
Data collection methods
After obtaining the required research ethics approval, data collection began. The team was made up of 3 people, the co-investigators and the principal investigator. A modified self-administrated WHO STEPwise questionnaire was used to collect data regarding physical activity level and measure the prevalence of major NCDs, in participants.2 The purpose of the study was explained to all physicians and they were assured that their information would be kept confidentially and anonymously. The questionnaire was subdivided into 3 sections, namely: demographics, physical activity status and major NCDs. Firstly, the demographics section included questions on gender, age, marital status, highest educational degree, year of graduation from the highest degree, professional title, working years, and monthly income. The second section assessed the physical activity status on 3 levels: “vigorous-intensity activities” are activities that require hard physical effort and cause a significant increase in breathing or heart rate for example, running or playing football; “moderate-intensity activities” require moderate physical effort and cause a small increase in breathing or heart rate for example, brisk walking or swimming; or ‘neither’. If the individuals are physically active, they had to estimate how many days in a typical week they are physically active and the approximate time that they spend on performing these activities on a typical day. However, if they are not physically active, they had to specify the most important reason behind not engaging in physical activity. Lastly, data on the prevalence of major NCDs was collected in the third section by asking regarding the history of (diagnosis, under management) diabetes, cardiovascular diseases, cancers, and chronic respiratory diseases.
Data analysis
Data was collected and coded before being entered into the Statistical Package for Social Sciences version 21 (SPSS Inc., Chicago, IL, USA), Descriptive statistics was carried out for all variables. Univariate analysis Chi square was used to find any association between physical activity and other predicted variables. A p-value of less than 0.05, was set to be significance of the results
Results
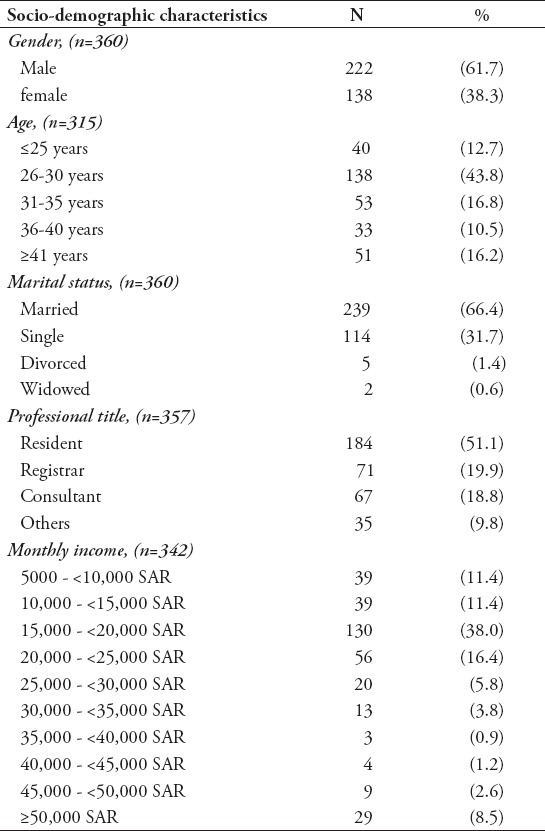
A total of 370 questionnaires were distributed. The response rate was (98.6%). Thus, data were analyzed for 360 physicians. The 360 physicians who participated in this study were working in 4 studied Riyadh hospitals. The mean ± standard deviation age was 33.11 ± 9.27 years with a range of 24-65 years. Approximately 2 thirds of them were married (66.4%) males (61.7%)”. Approximately half of the population were residents (51.1%). Most participants (77.2%) reported earning a monthly-income that ranged from 5,000 to 25,000 Saudi Riyals (Table 1).
Table 1.
Socio-demographic characteristics of 360 physicians from 4 leading healthcare institutions in Riyadh, Kingdom of Saudi Arabia (n=360).
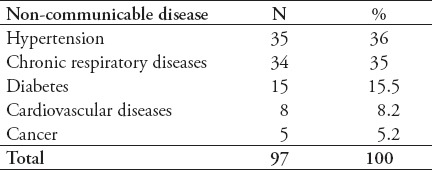
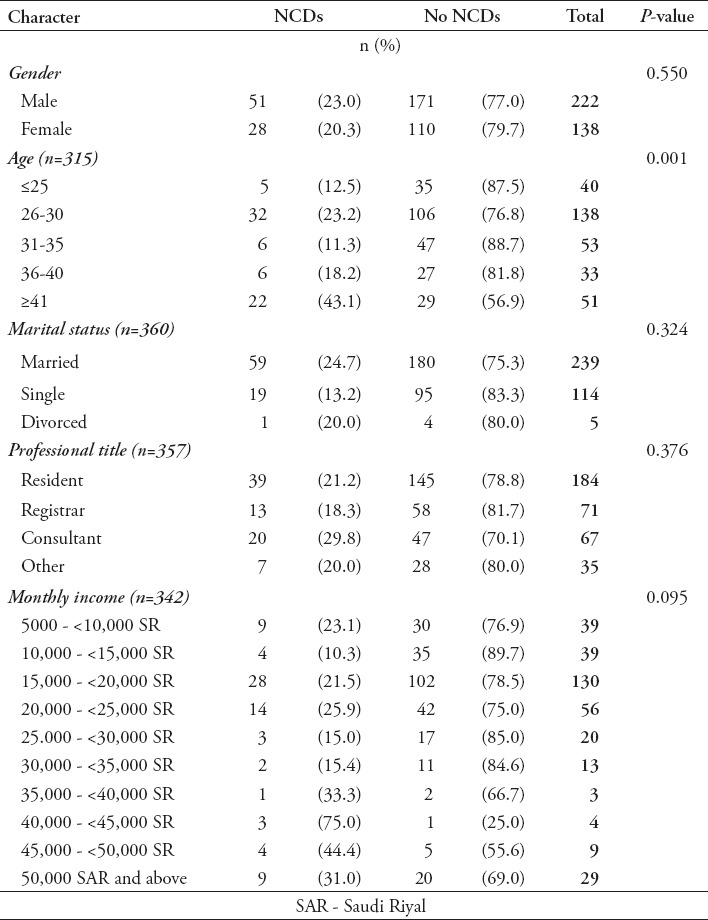
The findings indicated that physical activity is relatively high among the participants; a total of 227 (63.1%) participate in physical activity. Among them, 58 (25.6%) reported practicing vigorous physical activities, while 169 (74.4%) reported practicing moderate physical activities. The type of physical activity that was most practiced by the vigorous active group was running (63.8%) followed by carrying heavy loads (39.7%), playing football (22.4%), and digging or construction work (1.7%). The average number of days spent performing vigorous intensity activity was 3.79 days per week with a mean time of 1.42 hours per day. Among the moderate active group, brisk walking was the most reported practiced type of activity (69.8%), followed by swimming (16%), carrying light loads (10.1%), cycling (7.7%), and volleyball (3%). The average number of days spent performing moderate intensity activity was 3.65 days per week with a mean time of 1.3 hours per day (Table 2). Further analysis of the inactive group (36.9%) revealed that the most important reported reasons for not engaging in physical activity included lack of time (58.1%), work duties (22.5%), lack of interest and motivation (12.4%), lack of suitable facilities (3.9%), hot weather (1.6%), and suffering from chronic illness (0.8%) (Figure 1). Gender was the only significant variable related to physical activity, but no significant association was found between p-values of age (p=0.520), marital status (p=0.442), professional title (p=0.107), monthly income (p=0.175), with the level of physical activity. Male physicians were more likely to perform vigorous intensity activities (20.3%) than female physicians (9.4%) However, female physicians were engaging more in moderate intensity activities (58%) than male physicians (40.1%) this difference was found to be statistically significant (p=0.001) (Table 3). Table 4 illustrates the reported prevalence of major non-communicable diseases, which is (21.9%) among 360 physicians. Hypertension was most frequently reported (36%) followed by chronic respiratory diseases (35%), diabetes (15.5%), cancers (5.2%), and cardiovascular diseases (8.2%).
Table 2.
Types of vigorous and moderate physical activities of the sample of Riyadh, Kingdom of Saudi Arabia physicians.
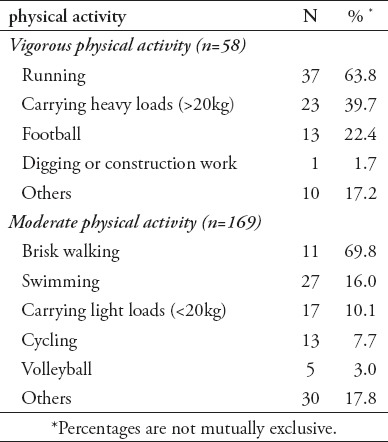
Figure 1.
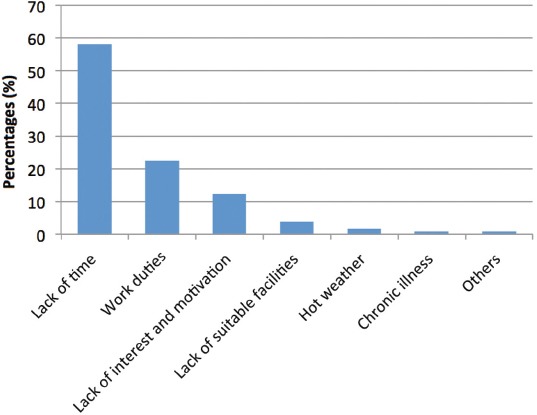
The most important reason for not engaging in physical activity among the inactive group of the sample of 360 physicians from 4 leading healthcare institutions in Riyadh, Kingdom of Saudi Arabia (n=360).
Table 3.
Association between physical activity level and socio-demographic characteristics of 360 physicians from 4 leading healthcare institutions in Riyadh, Kingdom of Saudi Arabia (n=360).
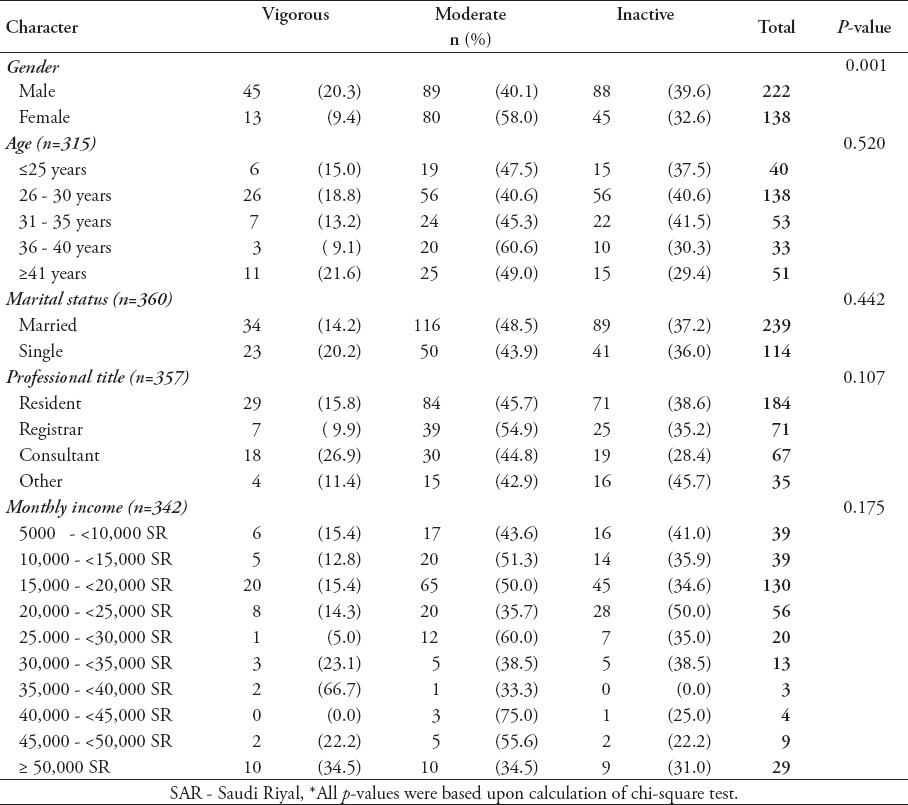
Table 4.
Reported prevalence of major non communicable diseases among the sample of Riyadh physicians
No statistically significant difference was found between physicians who suffer from one or more type of NCD and those who do not have any type of NCD with respect to their gender (p=0.550), marital status (p=0.324), professional title (p=0.376), and monthly income (p=0.095). The proportion of physicians who reported suffering from one or more major NCD were mostly above 40 years old, which was significantly statistically different when compared with other age groups of selected physicians (p=0.001) (Table 5). Testing the association between physical inactivity and major NCDs in our sampled physicians was inconclusive (odds ratio= 1.3; (95%) confidence interval [CI]= 0.463, 1.282; p=0.314).
Table 5.
Association between the major non-communicable diseases (NCDs) and socio-demographic characteristics of 360 physicians from 4 leading healthcare institutions in Riyadh, Kingdom of Saudi Arabia (n=360).
Discussion
A previous national physical activity assessment conducted by the Saudi Ministry of Health, using the WHO STEPwise approach for NCD surveillance, in 2005 involved 3,547 men and women between 25 and 64 years old. It indicated that physical inactivity is highly prevalent among the Saudi population (67.6%).14 Conversely, this study reported physical activity in our sample was higher (63%) than in the general Saudi population (32.4%).14 The possible reasons behind this difference may be that physicians are highly educated and are fully aware of the benefits of physical activity. Moreover, the working lifestyle of most physicians makes them more physically active. A national study published in 2015 supports the fact that physicians are more physically active. It showed that (65.2%) of primary health care physicians in selected centers in the Aljouf region were performing moderate to vigorous physical activities, while (34.8%) of them were physically inactive.22 Another study carried out in Estonia 23 2010 among female family doctors reported that (92%) of participants were physically active. Among the vigorous and moderate intensity activities, running (63.8%) and brisk walking (69.8%) were the most reported types. Such types of exercise are expected as they are the most available, easy to perform, suitable for physicians’ work duties and they are free.
According to analysis of the level of physical activity in our study, most of men reported performing vigorous intensity activities while women reported performing moderate intensity activities. This may be due to the fact that vigorous intensity activities for example, football are the most available in sports’ centers or play grounds, which are more accessible to men than to women in Riyadh, while moderate intensity activities for example, swimming can be performed at home.
For the physicians who were physically inactive (36.9%), lack of time was the most reported reason for not engaging in physical activities. Similarly, a study carried out in Bahrain in 20036 among physicians, revealed that lack of time was the most common cited barrier for non-participation in physical activity. Such a result is expected as physicians’ working hours and related responsibilities consume most of their time.18 This study also found that (21.9%) of the sampled physicians reported suffering from one or more NCD, (9.7%) reported having hypertension, which is lower than the population prevalence (21.8%);7 (4.2%) have diabetes, much lower than the (18.3%) of the general population reported in the STEPwise WHO surveillance.7 This may be explained by better health awareness and the healthier life-style of physicians, compared with the general population, but we also recognize that such results are not easy to explain, given that diabetes runs in families and hypertension is known to be predominantly idiopathic. The results showed no significant association between inactivity and the appearance of one or more type of NCD. Therefore, it is not possible to conclude that physical inactivity precipitates the occurrence of NCDs or not. This is especially true because this was a cross-sectional study and it was a crude estimation of the prevalence of NCDs. However, a systematic review study 24 published in 2013 revealed that physical activity has a positive long-term impact on the incidence of major non-communicable diseases.
The limitations of this study include the fact that the self-reporting of physical activity level differs from one person to another. Secondly, since it is a cross-sectional study, it is not possible to ascertain the association between physical inactivity and developing NCDs. Moreover, some NCD risk factors such as tobacco use, genetic factors, and lipid profile were not investigated in our study. We hope that our research will widen the scope of knowledge regarding physical activity among physicians and physical activity’s possible link with major NCDs. For future studies, we recommend including a larger sample size of physicians from different healthcare institutions. Using a case control approach might be more useful than a cross sectional study in detecting possible associations between physical inactivity and major NCDs.
In conclusion, the findings of the present study demonstrated a high prevalence (63%) of physical activity among our sample of Riyadh physicians in comparison with the general population (32.4%). Among the inactive group, the main reasons for not engaging in physical activity were lack of time (58.1%) and work duties (22.5%). The prevalence of having one or more major NCD among Riyadh physicians was reported to be (21.9%). No association was found between physical inactivity and major NCDs among the sampled physicians.
Acknowledgment
The authors gratefully acknowledge Dr. Ahmed Bahnassy, King Fahad Medical City, Riyadh, Kingdom of Saudi Arabia for his contribution and assistance of the statistical analysis.
Footnotes
Statistics.
Excerpts from the Uniform Requirements for Manuscripts Submitted to Biomedical Journals updated November 2003.
Available from www.icmje.org
Describe statistical methods with enough detail to enable a knowledgeable reader with access to the original data to verify the reported results. When possible, quantify findings and present them with appropriate indicators of measurement error or uncertainty (such as confidence intervals). Avoid relying solely on statistical hypothesis testing, such as the use of P values, which fails to convey important information about effect size. References for the design of the study and statistical methods should be to standard works when possible (with pages stated). Define statistical terms, abbreviations, and most symbols. Specify the computer software used.
References
- 1.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. STEPS Planning and Implementation: STEPS Instruments for NCD Risk Factors (Core and Expanded Version 1.4) Geneva (CH): WHO; 2003. Available from: www.who.int/chp/steps/manual/en/index5.html . [Google Scholar]
- 3.Das P, Horton R. Rethinking our approach to physical activity. Lancet. 2012;380:189–190. doi: 10.1016/S0140-6736(12)61024-1. [DOI] [PubMed] [Google Scholar]
- 4.Al-Hazzaa HM, Abahussain NA, Al-Sobayel HI, Qahwaji DM, Musaiger AO. Physical activity, sedentary behaviors and dietary habits among Saudi adolescents relative to age, gender and region. In J Behav Nutr Phys Act. 2011;8:1. doi: 10.1186/1479-5868-8-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bahram S, Abbas B, Kamal J, Fakhro E. Leisure-time physical activity habits among physicians. Bahrain Med Bull. 2003;25:80–82. [Google Scholar]
- 7.World Health Organization. Global status report on noncommunicable diseases 2014. Geneva (CH): WHO; 2014. Available from: http://www.who.int/nmh/publications/ncd-status-report-2014/en/ [Google Scholar]
- 8.Aira T, Wang W, Riedel M, Witte SS. Reducing risk behaviors linked to noncommunicable diseases in Mongolia: a randomized controlled trial. Am J Public Health. 2013;103:1666–1674. doi: 10.2105/AJPH.2012.301175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of noncommunicable diseases. Kidney Int. 2011;80:1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Non-communicable Diseases Country Profiles 2014: Saudi Arabia. Geneva (CH): WHO; 2014. Available from: http://www.who.int/nmh/publications/ncd-profiles-2014/en/ [Google Scholar]
- 11.Amin TT, Ali Salah Al Khoudair MAA, Harbi ARAA. Leisure time physical activity in Saudi Arabia: prevalence, pattern and determining factors. APJCP. 2012;13:351–360. doi: 10.7314/apjcp.2012.13.1.351. [DOI] [PubMed] [Google Scholar]
- 12.Abd TT, Kobylivker A, Perry A, Miller J, III, Sperling L. Work-Related Physical Activity Among Cardiovascular Specialists. Clin Cardiol. 2012;35:78–82. doi: 10.1002/clc.21954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Zalabani AH, Al-Hamdan NA, Saeed AA. The prevalence of physical activity and its socioeconomic correlates in Kingdom of Saudi Arabia: A cross-sectional population-based national survey. Journal of Taibah University Medical Sciences. 2015;10:208–215. [Google Scholar]
- 14.Saudi Ministry of Health / World Health Organization. WHO Stepwise approach to NCD Surveillance. Country Specific Standard Report: Saudi Arabia. MoH/WHO:2005. Available from: http://www.who.int/chp/steps/2005_SaudiArabia_STEPS_Report_EN.pdf .
- 15.Macniven R, Bauman A, Abouzeid M. A review of population-based prevalence studies of physical activity in adults in the Asia-Pacific region. BMC Public Health. 2012;12:1. doi: 10.1186/1471-2458-12-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Owoeye O, Tomori A, Akinbo S. Pedometer-determined physical activity profile of healthcare professionals in a Nigerian tertiary hospital. Niger Med J. 2016;57:99. doi: 10.4103/0300-1652.182070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amin TT, Al Khoudair A, Al Harbi M, Al Ali A. Leisure time physical activity in Saudi Arabia: prevalence, pattern and determining factors. Asian Pac J Cancer Prev. 2012;13:351–360. doi: 10.7314/apjcp.2012.13.1.351. [DOI] [PubMed] [Google Scholar]
- 18.Thorndike A, Milla S, Sonnenberg L, Palakshappa D, Gao T, Pau C, et al. Activity Monitor Intervention to Promote Physical Activity of Physicians-In-Training: Randomized Controlled Trial. PLoS One. 2014:9e100251. doi: 10.1371/journal.pone.0100251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glickman D, Parker L, Sim LJ, et al. Committee on Accelerating Progress in Obesity Prevention; Food and Nutrition Board;Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation (2012) Washington (DC): National Academies Press (US); 2012. p. 14. [PubMed] [Google Scholar]
- 20.Williams AS, Williams CD, Cronk NJ, Kruse RL, Ringdahl EN, Koopman RJ. Understanding the exercise habits of residents and attending physicians: a mixed methodology study. Family Medicine. 2015;47:118–123. [PubMed] [Google Scholar]
- 21.Reshidi FS. Level of Physical Activity of Physicians Among Residency Training Program At Prince Sultan Military Medical City, Riyadh, KSA 2014. Int J Health Sci (Qassim) 2016;10:39. doi: 10.12816/0031215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lobelo F, de Quevedo IG. The evidence in support of physicians and health care providers as physical activity role models. Am J Lifestyle Med. 2016;10:36–52. doi: 10.1177/1559827613520120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suija K, Pechter Ü, Maaroos J, Kalda R, Rätsep A, Oona M, et al. Physical activity of Estonian family doctors and their counselling for a healthy lifestyle: a cross-sectional study. BMC Family Practice. 2010;11:48. doi: 10.1186/1471-2296-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity–a systematic review of longitudinal studies. BMC Public Health. 2013;13:1. doi: 10.1186/1471-2458-13-813. Gender was the only. [DOI] [PMC free article] [PubMed] [Google Scholar]


