Abstract
Most patients complaining of pharyngeal pain have an upper respiratory tract infection or other local explanation for their pain. Here we show 3 rare cases of patients visiting our Otorhinolaryngology Department who had an initial symptom of pharyngeal pain caused by acute coronary syndrome (ACS). An electrocardiogram and a cardiac biomarker test are recommended to exclude ACS with atypical presentation in cases without pharyngolaryngeal findings comparable to pharyngeal pain.
Key words: Pharyngeal pain, myocardial infarction, acute coronary syndrome
Competing interest statement
Conflict of interest: the authors declare no potential conflict of interest.
Introduction
Pharyngeal pain is one of the most common symptoms of which outpatients complain. Although almost all of them have an upper respiratory tract infection, tumor or other local inflammation, the symptom rarely indicates acute coronary syndrome (ACS).1 An ACS patient who complains only of sore throat without any vegetative symptom is difficult to diagnose and treat. Misdiagnosis can lead to delayed treatment and increased motility. We present 3 such cases of patients visiting the otorhinolaryngology department of our hospital with symptoms of pharyngeal pain alone, which were brought about by ACS.
Case Reports
Case #1
A 72-year-old woman presented to the ENT department of our hospital with a 5-day history of sore throat. There were no other symptoms of an upper respiratory tract infection. She and her family had no cardiovascular disease history. She took no regular medication and had no allergies. She was a nonsmoker and did not consume alcohol. She had no other cardiac risk factors. On examination, she was 138 cm in height and 45 kg in weight with a body mass index of 23.6. She seemed not to be in distress. She only complained of a moderate sore throat, which she had never had before. She has no tenderness on her neck or swallowing pain. She denied chest pain, shortness of breath, or nausea. Her body temperature was 95 F. Her heart rate was 70 bpm, regular and her blood pressure was 122/64 mmHg. Her oxygen saturation was 98% on room air .She had an inflamed tonsil. On the laryngeal fiberscope test, she had no swelling or inflamed pharyngolarynx mucosa (Figure 1). She had no cervical lymphadenopathy. Her lungs were clear on auscultation and her heart sounds were dual with no murmur. The lab data showed that WBC was 10,700/µL (neutrophil=81.8%), CRP was under 0.03 and other data were normal. Because there was no symptom apart from a sore throat, we could not make an initial diagnosis. Nine hours after the initial examination, she said to a nurse that she had a severely stiff shoulder. Finally, she suffered from severe back pain and chest pain with nausea and cold sweats 16 hours after she came to our examination room. The symptoms strongly suggested acute myocardial infarction. An ECG and cardiac biomarker rapid check (troponin T and H-FABP) were ordered. The ECG showed ST-segment elevation in V1-V5 (Figure 2). Blood tests showed elevated cardiac enzymes. An echocardiography showed hypo kinesis of the anteroseptal wall. A diagnosis of AMI was made based on the elevated cardiac enzymes combined with the ECG changes and the echogram. Cardiac catheterization and angiography (CAG) were performed by a cardiologist. The CAG showed that the left anterior descending coronary artery was completely occluded and the right coronary artery and left circumflex coronary artery were 90% occluded (arrows head in Figure 3A). The left anterior descending coronary artery lesion was opened successfully with the placement of a drug-eluting stent (Figure 3B). Following this, the throat pain was improved.
Figure 1.
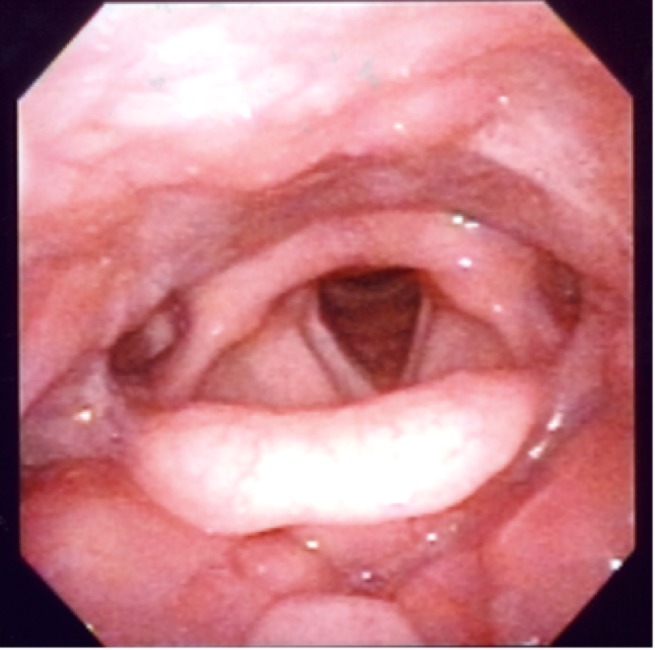
Neither swelling nor inflammation of the mucosa was seen in the pharyngolarynx.
Figure 2.
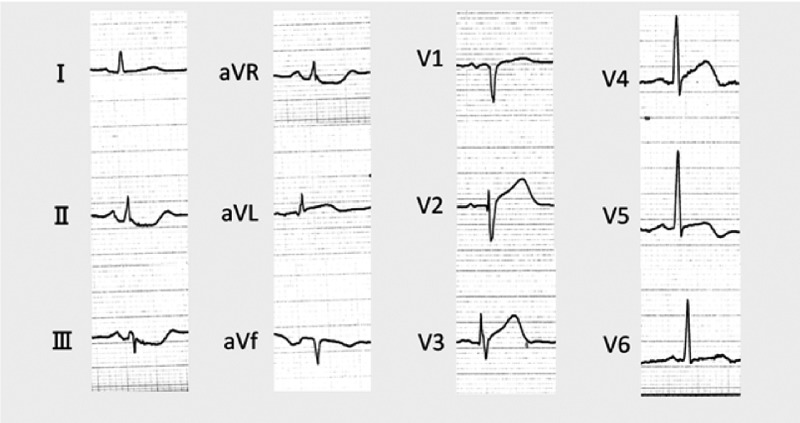
The electrocardiogram showed ST segment elevation in V1-V5.
Figure 3.
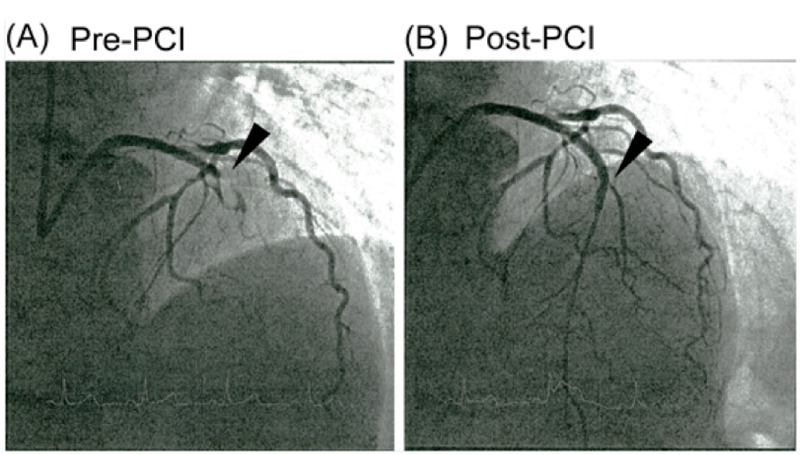
The left anterior descending coronary artery was completely occluded (arrows head in A) and the right coronary artery and left circumflex coronary artery were 90% occluded. The lesion was successfully opened placement of a drug-eluting stent (arrows head in B).
Case #2
An 84-year-old man presented with a 3- day history of sore throat and dyspnea. His medical history included chronic renal failure (Cre: 2.21 mg/dL), large thoracic aortic aneurysm, transient ischemic attack and diabetes mellitus. His heart rate was 113 bpm and regular and his blood pressure was 140/64 mmHg. His oxygen saturation was 91% on room air. He had no upper respiratory tract infection but had a sore throat and dyspnea. The ECG showed CRBBB. Blood tests showed elevated cardiac enzymes and creatinine kinase (245 U/L). A chest x-ray showed bilateral pleural effusions and cardiomegaly. A chest computed tomography (CT) showed high calcification in three coronary artery branches. An echocardiography showed hypo kinesis and low ejection fraction, 25%. A diagnosis of acute heart failure due to AMI was made.
Because of the low renal function, physical status and severe stenosis indicated by chest CT, CAG was not performed. Although the patient received intensive treat, he was died 2 weeks later.
Case #3
An 89-year-old woman presented with a 7-day history of sore throat. This symptom worsened day by day. Two months before, she had been treated for unstable angina by placement of a stent at another hospital. Her current medications included aspirin, ethyl icosapentate, nicorandil and ezetimibe. Her heart rate was 70 bpm and regular and her blood pressure was 120/60 mmHg. Her oxygen saturation was 98% on room air. Her throat mucosa is not inflamed or swollen. The ECG showed a non-ST segment elevation, but a QS pattern in V1-V3. Blood tests showed elevated cardiac enzymes. A diagnosis of non-ST-segment elevation of MI (NSTEMI) was suspected based on the elevated cardiac enzyme. Although we strongly recommended CAG, the patient refused further treatment and was lost to follow up.
Discussion and Conclusions
An atypical presentation of myocardial infarction can include epigastric pain, nausea, sore throat and toothache. Table 1 shows a summary of the clinical profiles of the present cases. All 3 patients consulted us nearly 1 week after pharyngeal pain began. Pharyngeal pain is thought to be atypical symptoms for ACS, but one of the common symptoms for upper airway infection or inflammation. It is well understood that the patients complaining of pharyngeal pain alone are delayed to visit at clinic. Two of three patients had neither history of nor risk factors for cardiac disease, which may be attributed to a delay in correct diagnosis. Case #2 had several risk factors for cardiac disease, which promoted us to perform a cardiac examination. Case #3 had a history of myocardial infarction, but revealed no evidence of abnormality in the ECG, although an elevation of cardiac enzymes was recognized.
Table 1.
Patient characteristics.
| Age | Sex | Symptom | Length of symptom | Past history | Medical history | ECG | Cardiac enzyme | Diagnosis | |
|---|---|---|---|---|---|---|---|---|---|
| Case #1 | 72 | F | Only pharyngeal pain | 5 days | None | None | ST segment elevation | Elevated | AMI |
| Case #2 | 84 | M | Pharyngeal pain and dyspnea | 5 days | None | TIA CRF | CRBBB | Elevated | Acute heart failure |
| Case #3 | 88 | F | Only pharyngeal pain | 7 days | OMI | Hypertension | Non ST segment elevation | Elevated | AMI |
OMI, old myocardial infarction; TIA, transient ischemic attack; CRF, chronic renal failure; CRBBB, complete right bundle branch block; AMI, acute myocardial infarction.
Sampson et al. pointed out that only 2% of ACS patients complained of neck pain alone.1 Briegaer et al.2 showed that 8.4% of patients with ACS presented without chest pain. Previously a few cases who complained of pharyngeal pain alone were reported.3-5 In some cases, ACS can present as isolated mandibular or jaw pain, and this could be confused with a sore throat, especially in elderly population. On the other hand, infection (i.e., upper respiratory tract infection) could lead to heart decompensation, particularly with underlying ischemic heart disease. Due to unusual and atypical symptoms, the initial diagnosis was mistaken in 24% of ACS cases, which could have resulted in delayed treatment and increased mortality as compared to patients with typical presentations.6 It was also reported that patients who never experienced chest pain had a 3 times higher risk of death than patients whose chest pain persisted or recurred in the Emergency Department.7 Therefore, it is important that the physicians make a correct initial diagnosis. An ECG and a cardiac biomarker test are recommended to exclude ACS with atypical presentation in cases with pharyngolaryngeal findings suggesting pharyngeal pain.
References
- 1.Sampson JJ, Cheitlin MD. Pathophysiology and differential diagnosis of cardiac pain. Prog Cardiovasc Dis 1971;13:507-31. [DOI] [PubMed] [Google Scholar]
- 2.Brieger D, Eagle KA, White K, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the global registry of acute coronary events. Chest 2004;126:461-9. [DOI] [PubMed] [Google Scholar]
- 3.Sone M, Koizumi A, Tamiya E, et al. Angina pectoris with pharyngeal pain alone: a case report. Angiology 2009;60:259-61. [DOI] [PubMed] [Google Scholar]
- 4.Yanagawa Y, Nishimura M, Ohkawara J, et al. Acute myocardial infarction presenting with pharyngeal pain alone. J Emerg Med 2012;43:e287-8. [DOI] [PubMed] [Google Scholar]
- 5.Auer J, Weber T, Berent R, et al. Throat pain as the only symptom of inferior wall myocardial infarction. J Otolaryngol 2006;35:424-6. [DOI] [PubMed] [Google Scholar]
- 6.Canto JG, Shlipak MG, Lambrew CT, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA 2000;283:3223-9. [DOI] [PubMed] [Google Scholar]
- 7.Comeau A, Jensen L, Burton JR. Can symptom presentation predict unstable angina/non-ST-segment elevation myocardial infarction in a moderate-risk cohort? Eur J Cardiovasc Nurs 2006;5: 127-36. [DOI] [PubMed] [Google Scholar]


