Abstract
Background
Exposure to both occupational and non-occupational noise is recognized as a risk factor for noise-induced hearing loss (NIHL). Although audiologists routinely inquire regarding history of noise exposure, there are limited tools available for quantifying this history or for identifying those individuals who are at highest risk for NIHL. Identifying those at highest risk would allow hearing conservation activities to be focused on those individuals.
Purpose
To develop a detailed, task-based questionnaire for quantifying an individual’s annual noise exposure arising from both occupational and non-occupational sources (aim 1) and to develop a short screening tool that could be used to identify individuals at high risk of NIHL (aim 2).
Research Design
Review of relevant literature for questionnaire development followed by a cross-sectional descriptive and correlational investigation of the newly developed questionnaire and screening tool.
Study Sample
One hundred fourteen college freshmen completed the detailed questionnaire for estimating annual noise exposure (aim 1) and answered the potential screening questions (aim 2). An additional 59 adults participated in data collection where the accuracy of the screening tool was evaluated (aim 2).
Data Collection and Analysis
In study aim 1, all subjects completed the detailed questionnaire and the potential screening questions. Descriptive statistics were used to quantify subject participation in various noisy activities and their associated annual noise exposure estimates. In study aim 2, linear regression techniques were used to identify screening questions that could be used to predict a subject’s estimated annual noise exposure. Clinical decision theory was then used to assess the accuracy with which the screening tool predicted high and low risk of NIHL in a new group of subjects.
Results
Responses on the detailed questionnaire indicated that our sample of college freshmen reported high rates of participation in a variety of occupational and non-occupational activities associated with high sound levels. Although participation rates were high, annual noise exposure estimates were below highest-risk levels for many subjects because the frequency of participation in these activities was low in many cases. These data illustrate how the Noise Exposure Questionnaire (NEQ) could be used to provide detailed and specific information regarding an individual’s exposure to noise. The results of aim 2 suggest that the screening tool, the 1-Minute Noise Screen, can be used to identify those subjects with high- and low-risk noise exposure, allowing more in-depth assessment of noise exposure history to be targeted at those most at risk.
Conclusions
The NEQ can be used to estimate an individual’s annual noise exposure and the 1-Minute Noise Screen can be used to identify those subjects at highest risk of NIHL. These tools allow audiologists to focus hearing conservation efforts on those individuals who are most in need of those services.
Keywords: Noise, Hearing Loss, Noise-Induced, Screening, Self Report
INTRODUCTION
Noise-induced hearing loss (NIHL) is a common condition in the United States, with an estimated 15% of Americans aged 20 to 69 years of age, or 26 million individuals, experiencing hearing loss due to noise exposure encountered during occupational or leisure activities (NIDCD, 2008). Noise exposure may first cause only a temporary worsening of hearing, called a temporary threshold shift (TTS). Repeated exposure to loud sound eventually leads to permanent threshold shift (PTS), when the auditory system is so severely damaged that it can no longer recover. Traditional views of TTS include the idea that, if thresholds return to normal, no permanent damage has been done. Recent data from animal models have challenged this viewpoint. Kujawa and colleagues induced TTS in mouse (Kujawa & Liberman, 2009) and guinea pig (Lin et al., 2011). Histology was completed on the animals following full TTS recovery (as measured by recovery of distortion-product otoacoustic emission and auditory brainstem response thresholds). Results indicated permanent loss of up to 50% of synapses between inner hair cells and afferent auditory nerve fibers in the frequency region that experienced the greatest TTS. Recent data suggests a similar mechanism may be operating in human ears (Stamper & Johnson, 2015). These data provide evidence suggesting noise exposures resulting in TTS have the potential to lead to permanent damage in the inner ear even though hearing thresholds for pure-tone stimuli are normal.
Although NIHL is widespread and noise exposure may be more hazardous than previously believed, noise exposure is widely recognized as one of the leading preventable causes of hearing loss (Dobie, 2008). Indeed, decreasing the prevalence of NIHL is a goal of the Healthy People 2020 initiative (Healthy People, n.d.). One strategy that might help meet this goal is to target people who are at greatest risk for developing NIHL and focus hearing conservation efforts accordingly.
A variety of regulatory agencies have made recommendations for noise exposure limits, primarily for work-place exposure. The selection of an exposure limit typically depends on defining a maximum acceptable hearing loss over a lifetime and determining the percentage of the noise-exposed population for which the maximum acceptable hearing loss will be tolerated (NIOSH, 1998; Suter, 2000). Three agencies that have issued recommendations for exposure limits include the Occupational Safety and Health Administration (OSHA), the National Institute for Occupational Safety and Health (NIOSH), and the U.S. Environmental Protection Agency (EPA). The exposure limits issued by each of these agencies take into account three parameters related to the exposure: level (“how loud”), frequency (“how often”), and duration (“how long”).
Typically, OSHA and NIOSH recommendations are applied to an occupational setting where recommendations are based on an 8-hr work day over the course of a 40-yr working lifetime. OSHA’s permissible exposure limit is 90 dBA with a 5-dB exchange rate (e.g., 90 dBA for 8 hrs, 95 dBA for 4 hrs, etc.). Adherence to the OSHA limits could result in hearing impairment for 25% of the working population over a 40-year working lifetime (NIOSH, 1998). NIOSH’s recommended exposure limit (REL) is more conservative at 85 dBA with a 3 dB exchange rate (e.g., 85 dBA for 8 hrs, 88 dBA for 4 hrs, etc.). NIOSH estimates that adherence to these limits could result in hearing impairment in 8% of the working population (NIOSH, 1998). The EPA specifies a recommended exposure limit of 70 dBA over the course of the entire year (not restricted to working hours). Adherence to the EPA limit is intended to protect the entire population (EPA, 1974) and is considered a safe level for protection from hearing loss (Hammer et al., 2014).
The NIOSH and OSHA limits were designed for occupational settings; however, noise exposure is not limited to the workplace. Many non-occupational activities can reach sound levels that have the potential to be damaging to the auditory system. Neitzel et al. (2004a) surveyed sound levels reported in the literature for various leisure and recreational activities, including operating equipment (e.g., power tools, motorcycles, snowmobiles, and light aircraft), and attendance at loud recreational events (e.g., rock concerts or commercial sporting events). Based on this literature survey, Neitzel et al. obtained the range of levels encountered for common recreational activities and computed an average level for each activity. The average level was > 90 dBA for all activities. This suggests some recreational activities are associated with sound levels that may be hazardous, particularly if the activity is engaged in regularly or when combined with occupational noise exposure.
More recently, Flamme et. al (2012) collected exposure data from a sample of 210 men and 76 women. Subjects wore dosimeters for extended time periods ranging from 23 hours to 20 days, with a median of 9.8 days. Because the subjects wore the dosimeters continuously, the data reflect both occupational and non-occupational exposures. The Flamme et al. data indicated that 65–70% of subjects exceed the EPA recommended exposure limit while approximately 7% of women and 18% of men exceeded the NIOSH limit. Although the Flamme et al. data did not directly assess the source of noise exposure, it appears that, for many subjects, occupational noise was a substantial contributor to exposure levels, even though the study did not target subjects working in traditionally noisy occupations. Flamme et al. note that it was necessary to sample exposure over a time period of at least one to two weeks to capture infrequent, high-level exposures.
Although it is clear that sound levels for some recreational activities may be hazardous and it is widely recognized that exposure to all noise sources (occupational and non-occupational) is cumulative, few studies have attempted to characterize exposures for non-occupational noise (Carter et al., 2014). The most detailed information on non-occupational noise comes from studies conducted at the University of Washington as part of a multi-year evaluation of noise exposure in the construction industry (Seixas, 2004). This project included evaluation of the contribution of non-occupational noise exposures to NIHL risk for 112 apprentice construction workers. Neitzel and colleagues (2004a, 2004b) used a variety of approaches to quantify workers’ exposure, including a task-based approach where the workers completed a detailed questionnaire describing their participation in a variety of activities over the previous year. The task-based approach used by Neitzel et al. is an extension of the original application of the task-based exposure assessment model described by Stephenson (1995), where activities are broken into specific tasks that have specific associated sound-exposure values. Responses on the Neitzel questionnaire were used to provide an estimate of annual non-occupational exposure by using the sound levels associated with each of these activities (as determined through the literature survey described above) and integrating them into an exposure level (dBA). Based on this work, Neitzel and colleagues (2004a) reported that 19% of apprentice workers had non-occupational noise exposures that exceeded the NIOSH recommended exposure limit of 85 dBA. In other words, 19% of apprentice workers reported participation in leisure activities that exceeded what was considered to be safe per NIOSH occupational recommendations; this was in addition to being in a loud work environment on a regular basis.
Although the Neitzel et al. (2004a) data suggest that a task-based questionnaire could be used to estimate noise-exposure, it was not clear from their data if subjects could recall their activities with sufficient precision to provide an accurate estimate of their actual exposure levels, as measured by dosimetry. To address this question, Reeb-Whitaker et al. (2004) assessed the relationship between exposure levels obtained via a task-based recall questionnaire of workplace activities occurring 6 months prior and the dosimetry measures taken from those subjects on the same day. Although the sound level estimates obtained from both the task-based recall and the dosimetry were not identical, there was a strong correlation between the two (r=0.77), with an average difference between the two exposure-level estimates of approximately 2 dB. Based on these findings, the authors concluded that construction workers were able to accurately report past noise exposures using the task-based recall questionnaire approach.
A task-based questionnaire for quantifying noise exposure has also been used with professional symphony musicians (Schmidt et al., 2014) and for quantifying other occupational hazards such as exposure to fumes (Susi et al, 2000) or repetitive work tasks (Fallentin et al., 2001). It is impractical to have members of the general population wear dosimeters for long periods of time to assess their occupational and non-occupational exposures. Therefore, the development of a task-based questionnaire for use in the general population is one possible way to assist clinicians with targeting hearing conservation efforts to individuals who may be at highest risk for NIHL. Because the Neitzel et al. (2004a) questionnaire only queries non-occupational exposures and the Schmidt et al. (2014) questionnaire can only be used to query workplace exposures for a very specific group (symphony musicians), a more general task-based questionnaire is needed.
The purpose of this project was to develop a task-based questionnaire to quantify noise exposure history in the general public by querying both occupational and non-occupational exposures. This metric could be used by clinicians and researchers to identify individuals at risk for NIHL. The second objective was to establish a subset of questions from the task-based questionnaire that could be used to screen for individuals who are at higher risk for NIHL and, therefore, might benefit from a more in-depth assessment of their noise exposure history.
METHODS
Participants
A sample of 114 college freshmen (18–19 years old) participated in the first aim of the study, 49 males and 65 females. Students from local colleges were recruited with the assistance of introductory-level course instructors. An additional 59 subjects (19 males, 40 females) were recruited to participate in activities where the accuracy of a screening model was evaluated. These additional subjects were 19–30 years old. All study procedures were approved by the University of Kansas Medical Center institutional review board.
Aim #1: Development of the Noise Exposure Questionnaire
Questionnaire Overview
Each subject completed the self-administered Noise Exposure Questionnaire (NEQ; Appendix A), which required approximately 10 minutes to complete. Subjects were asked to recall participation in specific noisy activities during the past year. A one-year time period was chosen to capture noisy activities that are seasonal and infrequent (e.g., hunting, snowmobiling, attending sporting events). The NEQ consisted of three sections: 1) basic demographic information (gender and age), 2) six potential screening questions for determining individuals with high-risk noise exposure (Q#1–6), and 3) eleven detailed questions related to participation in loud, noisy activities used to quantify the annual noise exposure (Q#7–17).
The NEQ was based on the task-based questionnaire described in Neitzel et al. (2004a) but differed in several ways. First, two questions (Q#16–17) pertaining to occupational noise exposure (school year and summer) were inserted. Secondly, questions pertaining to playing a musical instrument (Q#13) and music listening via earphones (Q#14) or speakers (Q#15) were incorporated. Finally, response options were added to each question to query, on average, how many hours each noisy activity lasted.
Calculation of the Annual Noise Exposure Estimate
Protocols used to compute the annual noise exposure (ANE) estimate for each subject were based on those previously described by Neitzel et al. (2004a). In this approach, episodic (occasional) and routine (daily) exposures are calculated separately and then combined to produce an overall ANE estimate. Examples of activities that would be considered episodic exposures in this approach include the use of power tools and heavy machinery, attendance at loud sporting or entertainment events, and playing or listening to music. In contrast, routine exposures include daily actions not readily associated with high-risk noise exposures such as sleeping, reading, computer work, travel by bus or car, shopping, etc. The frequency of participation in each episodic noise activity was gathered from NEQ responses.
Representative sound levels for each episodic exposure activity queried were determined by a review of the available literature and are summarized in Table 1. Studies included in the determination of sound levels for each activity were drawn from several sources. For those activities queried by Neitzel et al. (2004a), the studies and associated sound levels they reported were used. For those activities not queried by Neitzel et al., we surveyed the relevant literature. In order for sound levels from a study to be included, the study was required to report A-weighted sound levels measured at appropriate distances and representative (not maximum) sound levels. These are the same inclusion criteria used by Neitzel et al. For studies meeting these inclusion criteria, the “low” values reported in Table 1, represent the mean of the lowest sound levels reported for the activity across studies. Likewise, the “high” values represent the mean of the highest reported sound levels. The “mid” values are the mean of the high and low values.
Table 1.
Sound levels obtained from review of the literature for various episodic noise activities queried on the Noise Exposure Questionnaire (NEQ).
| Q# | Noise activity category and description of activities | Representative LAeq (dBA) levels from literature | References | ||
|---|---|---|---|---|---|
| Low | Mid | High | |||
| For the following: Representative dBA levels were identified by Neitzel et al., 2004a; references used by Neitzel et al., 2004a listed for each category. | |||||
| 7 | Power Tools: use power tools, chain saws, other shop tools, outside of a paid job | 75 | 94 | 113 | Cohen et al., 1970; U.S. Office Noise Abatement & Control, 1978; McClymont & Simpson, 1989 |
| 8 | Equipment/Machinery: drive heavy equipment, use loud machinery (such as tractors, trucks, or farming or lawn equipment like movers/leaf blowers), outside of a paid job | 87 | 97 | 106 | Jones & Oser, 1968; U.S. Office Noise Abatement & Control, 1978; Holt, 1993 |
| 9 | Sporting/Entertainment: attend car/ truck races, commercial/school sporting events, music concerts/ dances, and any other events with amplified PA/music systems | 81 | 94 | 106 | Axelsson, 1996; Cohen et al., 1970; Yassi et al., 1993; Roberts, 1999 |
| 10 | Motorized Vehicles: ride/operate motorized vehicles such as motorcycles, jet skis, speed boats, snowmobiles, or four-wheelers | 88 | 98 | 107 | Cohen et al., 1970; U.S. Office Noise Abatement & Control, 1978; Ross, 1989; McCombe et al., 1994; Bess & Poynor, 1974; Anttonen et al., 1994 |
| 11 | Aircraft: ride/pilot small aircraft/private airplanes | 88 | 91 | 94 | Tobias, 1969; Cohen et al., 1970; Smith et al., 1975 |
| For the following: Not addressed by Neitzel et al., 2004a; Representative dBA levels identified by authors’ review of literature | |||||
| 13 | Musical Instrument: play a musical instrument | 74 | 87 | 99 | O’Brien et al., 2008; Chasin, 2009 |
| 14 | Music Listening (earphones): listen to music, radio programs, etc. using personal headsets or earphones | 60 | 76 | 93 | Airo et al., 1996; Fligor & Ives, 2006; Portnuff et al., 2009; Rice et al., 1987; Smith et al., 2000; Williams, 2005; Worthington et al., 2009 |
| 15 | Music Listening (other speakers): listen to music, radio programs, etc. from audio speakers in a car or at home (other than music concerts and earphone use) | 70 | 78 | 85 | Neitzel et al., 2004b; Neitzel personal communication, 2009* |
| 16 & 17 | Occupational Noise: work a noisy paid job during summer or school year | 80 | 90 | 100 | Lempert & Henderson (1973); OSHA (1981)** |
| For the following: Impact-type noise cannot be included in annual LAeq exposure calculation | |||||
| 12 | Firearms: around/shoot firearms such as rifles, pistols, shotguns, etc. | non-applicable (impact noise cannot be integrated into annual LAeq) | |||
Personal communication from R. Neitzel (4/15/2009) indicated the range for music listening in Neitzel et al. (2004b) was 70 to 85 dBA.
Due to OSHA requirements, occupational data are computed using a 5-dB exchange rate; therefore, 5-dB exchange rate data were included to represent the range of typical noisy job exposures. The discrepancy between 3 and 5 dB exchange rates is expected to be small for most occupational situations, 1–3 dB (Royster et al., 2000).
For purposes of the present study, estimates of each subject’s ANE were expressed in LAeq8760h. In this metric, “L” represents sound pressure level in dB, “A” represents use of an A-weighted frequency response, “eq” represents a 3-dB exchange rate for calculation of the time/level relationship, and “8760h” represents the total duration of the noise exposure in hours (24 hrs/day × 365 days/yr).
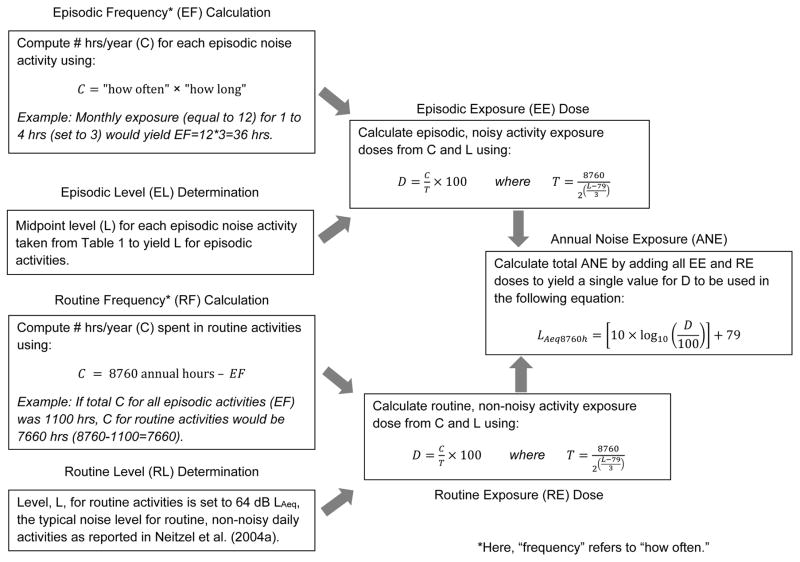
Figure 1 provides an overview of the ANE exposure computation. Using NIOSH-recommended formulas (NIOSH, 1998) and following the approach used by Neitzel et al. (2004a), doses were computed for each of the episodic, continuous-noise exposure activities queried on the NEQ (Q#7–11 and 13–17, Appendix A) and for routine exposure activities using the following equation:
Figure 1.
Overview of the computation of annual noise exposure (ANE) in LAeq8760h from responses to the Noise Exposure Questionnaire (NEQ). These procedures follow protocols described by Neitzel et al.(2004a) and noise exposure calculations extrapolated from those recommended by the National Institute for Occupational Safety and Health (NIOSH, 1998) for computing occupational exposures for a 40-hour work week.
Here, C refers to the number of hrs/yr reported by the subject for the activity. Frequency of participation responses on the NEQ were assigned values as follows: ‘daily’=200, ‘weekly’=50, ‘monthly’=12, ‘every few months’=1, and ‘never’=0. Similarly, for duration responses, the values were as follows: ‘8 hrs or more’=8, ‘4 to 8 hrs’=6, ‘1 to 4 hrs’=3, and ‘less than 1 hr’=1. The frequency of participation and duration values were multiplied to arrive at the episodic frequency value, or C. The calculation of C for routine exposure activities is 8760 minus the combined episodic values across all episodic exposures. In other words, C for routine exposures is the number of hours in a year not spent in noisy, episodic activities. The NEQ queries one additional episodic activity (Q#12, Appendix A) whose value is not included in the computation of D. This activity, firearm use, is associated with impulse-noise exposure. Because there currently is no accepted protocol for integrating impulse-noise exposures with the continuous-noise exposures queried for other questions, firearm exposures were not included in the dose calculation and will be described separately.
T represents the number of hrs/yr at which the activity is considered hazardous using our recommended exposure limit over a one-year time period. It is calculated using the following equation, with L representing the “mid” values listed in Table 1:
These computations will yield 10 episodic exposure doses and 1 routine exposure dose. Individual doses can be added arithmetically to result in a final ANE dose (see Appendix B for an example calculation). This total dose, D, is subsequently used in the following equation to calculate ANE:
Determination of NIHL Risk
The NIOSH recommended exposure limit, or 100% dose, for occupational settings is 85 dBA, weighted over 2000 hours with a 3-dB exchange rate, or 85 LAeq2000h. This limit represents hearing risk from occupational noise exposures over a typical work year (8 hr/day × 250 workdays/yr). For purposes of assessing annual exposures consisting of both occupational and non-occupational sources, it is necessary to consider an entire year’s time, or 8760 hours (24hr/day × 365 days). The U.S. Environmental Protection Agency recommends an annual exposure limit of 70 dBA to prevent hearing loss in the entire population (EPA, 1974). The purpose of the current study, however, was to identify individuals at highest risk of NIHL. Therefore, we referenced the NIOSH occupational noise limit of 85 LAeq2000h (NIOSH, 1998). Using the recommended 3-dB exchange rate, we extrapolated the NIOSH REL of 85 LAeq2000h to an annual equivalent exposure limit of 78.6 LAeq8760h. For purposes of our study, subjects with LAeq8760h values of 79 or greater were considered to be at highest risk for developing NIHL.
Statistical Approach
The Kappa Test was used to determine intra-test reliability of the NEQ by analyzing responses to repeated questions about firearm use and working a noisy job. Descriptive statistics were used to quantify subject participation in noisy activities and their associated ANE.
Aim #2: Development of the 1-Minute Noise Screen
Six screening questions (Q#1–6) were used as potential predictors of high risk noise exposure. The first three items (Q#1–3) pertained to time spent firing guns, working a noisy job, and exposure to any other type of loud sounds (e.g., power tools, lawn equipment, and loud music). Firearms and occupational noise are generally considered to pose the greatest risk to hearing (Johnson & Riffle, 1982; Franks, Davis, & Krieg, 1989; Neitzel et al., 2004a,b; Fligor, 2010). The next three potential screening items (Q#4–6) addressed the presence of common physiologic symptoms related to noise exposure: tinnitus, temporary hearing loss/TTS, and pain, fullness, or discomfort of the ears following exposure to loud sounds. These ear/hearing symptoms were selected as potential screening questions because they are generally accepted to be among the most common physiologic indicators of harmful noise exposure (Dobie, 2001; Ward et al., 2000).
Statistical Analysis
Multiple linear regression analyses were used to test the ability of each of the six screening questions (singly and in combination) to predict ANE values in LAeq8760h. Accuracy of the screening model identified from the regression analysis was assessed using clinical decision theory (Swets, 1988; Swets & Pickett, 1982).
RESULTS
Aim #1: Development of the Noise Exposure Questionnaire
Reliability
To test the internal consistency of the NEQ, intra-subject reliability was assessed using repeated questions regarding the regularity of firearm exposure (Q#1, 12) and working a noisy job (Q#2, 16, 17). Kappa statistics of agreement across these matched data were 0.871 (p < 0.001) for firearms and 0.590 for noisy jobs (p < 0.001), which represents almost perfect and moderate agreement for firearms and noisy jobs, respectively (Landis & Koch, 1977). Therefore, the NEQ was considered to be a reliable indicator of subjects’ noise activities.
Participation in Episodic Noise Activities
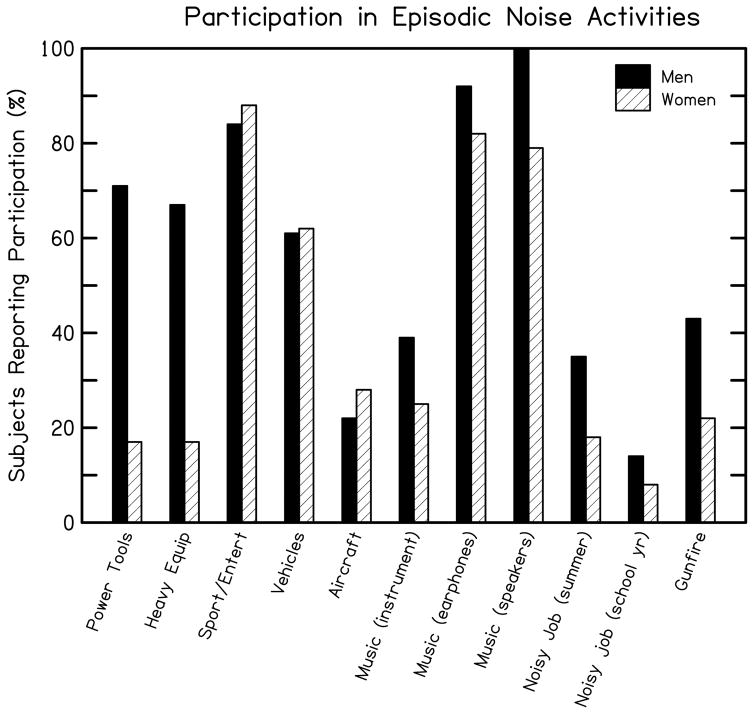
Subject responses to the NEQ provide information regarding the noise sources and activities to which these 18 and 19 year old subjects were exposed in the previous year. Figure 2 and Table 2 provide a summary of these data for our sample. Figure 2 shows the reported involvement in the eleven episodic activities included in the NEQ (10 continuous-type noise activities and 1 impulse-type noise activity). Data are reported separately for men and women in Fig. 2, but are described here as a combined sample. Music listening received the highest rate of participation, with 86% reporting listening to music via earphones and 98% listening to music via speakers. Commercial sporting/entertainment event attendance was also high at 86%. Use of recreational motorized vehicles was reported by 61% of subjects. Occupational noise exposures were less frequent, with 25% of subjects reporting working a noisy summer job and 11% working a noisy school year job. Participation in other continuous-type episodic noise activities varied, with 25% reporting flying in small/private aircraft during the past year, nearly 40% reporting using power tools or heavy equipment, and 31% reporting playing a musical instrument. For impulse-type episodic noise, 31% of subjects reported exposure to gunfire. In general, women reported less exposure to power tools, heavy equipment/machinery, firearms, and occupational noise than men. These data suggest many of our subjects participated in activities associated with high sound levels.
Figure 2.
Percentage of subjects reporting participation in each of the 10 continuous-noise activities and 1 impulse-noise activity queried on the Noise Exposure Questionnaire (NEQ) in aim 1. Results for men and women are displayed separately, as indicated in the legend.
Table 2.
Episodic frequency* (EF) and routine frequency* (RF) overview. Number of hours per year reported for broad categories of continuous-type episodic noise activities and number of hours per year for routine (everyday) activities.
| Episodic Activity Category(continuous-type noise) |
|
|||||
|---|---|---|---|---|---|---|
| EF: # hours/year for episodic activities | ||||||
| Range | 10thPercentile | 50thPercentile | 90thPercentile | Mean | ||
| General recreational activities (power tools, equipment/machinery, sporting/entertainment events, motorized vehicles, aircraft) | All Subjects | 0–903 | 0 | 39 | 309 | 119 |
| Men | 0–903 | 0 | 153 | 639 | 202 | |
| Women | 0–408 | 0 | 10 | 157 | 56 | |
| Music-related activities (playing musical instrument, music listening-earphones, music listening-speakers) | All Subjects | 0–1950 | 153 | 643 | 1400 | 765 |
| Men | 2–1800 | 153 | 653 | 1800 | 800 | |
| Women | 0–1950 | 163 | 636 | 1350 | 739 | |
| Occupational noise activities (noisy summer job, noisy school year job) | All Subjects | 0–1550 | 0 | 0 | 500 | 148 |
| Men | 0–1250 | 0 | 0 | 870 | 214 | |
| Women | 0–1550 | 0 | 0 | 400 | 98 | |
|
|
||||||
| Overall EF: hours per year for all continuous-type episodic activities combined | All Subjects | 5–2985 | 205 | 862 | 2050 | 1032 |
| Men | 5–2985 | 239 | 896 | 2480 | 1217 | |
| Women | 54–2959 | 187 | 807 | 1649 | 893 | |
|
|
||||||
| RF: # hours/year for routine activities | ||||||
| Routine Activities | Range | 10th Percentile | 50th Percentile | 90th Percentile | Mean | |
|
| ||||||
| Overall RF: hours per year spent in routine/everyday, non-noisy activities (calculated for each subject by subtracting subject’s EF from 8760 total hours per year) | All Subjects | 5775–8755 | 6710 | 7899 | 8555 | 7728 |
| Men | 5775–8755 | 6280 | 7864 | 8521 | 7543 | |
| Women | 5801–8706 | 7111 | 7953 | 8573 | 7868 | |
Here, “frequency” refers to “how often.”
An additional, and perhaps more important, parameter to consider is the amount of time spent in the activity. Table 2 presents episodic frequency of participation data overall and summarized for broad general categories of continuous-type episodic noise: noisy general recreational activities (power tools, equipment/machinery, sporting/entertainment events, motorized vehicles, aircraft), music-related activities, and job-related noise activities. This group of college freshmen reported far more hours per year spent in music-related activities (mean of 765 hrs/yr) than spent participating in noisy general recreational activities (mean of 119 hrs/yr) or working a noisy job (mean of 148 hrs/yr). The total time spent across all continuous-type episodic activities ranged from 5 hrs/yr to 2985 hrs/yr, with a mean of 1032 hrs/yr (or approximately 20 hrs/wk). Overall, men reported more hours engaged in noisy activities than women (1217 hrs/yr and 893 hrs/yr, respectively). For impulse-type episodic noise (not shown in Table 2), men reported more shots/yr than women for firearms (193 versus 26). While a high percentage of subjects in this study reported participating in various noisy activities, the number of hours (episodic frequency) spent in each of these activities was fairly low.
Participation in Routine Activities
Table 2 also includes a summary of participation in routine, non-noisy activities. For our purposes, routine activities were considered to be those daily activities not readily associated with risk of high noise exposure. These activities included time spent at home engaged in eating, sleeping, reading, computer/television use, travel by bus/car, shopping, or eating at a quiet restaurant. Routine activies would also include any other activity not considered to be associated with high noise levels and not specifically queried on the NEQ. The number of hours spent in these activities (routine frequency) was calculated as 8760 hrs minus the subject’s reported episodic frequency of participation hrs. As a direct reflection of the calculated episodic frequency of participation values for this group of subjects, overall routine frequency of participation data ranged from 5775 hrs/yr to 8755 hrs/yr, with a mean of 7728 hrs/yr (or approximately 149 hrs/wk). As expected, men spent less time in routine (non-noisy) activities than woman (mean of 7543 hrs/yr versus 7868 hr/yr). Overall, although subjects reported a high rate of participation in noisy activities, hrs/yr spent engaged in episodic noise activities were much less than the number of hrs/yr spent in routine (non-noise) daily activities.
Annual Noise Exposure (ANE) Values
ANE values were calculated for each subject by combining the episodic exposure values for non-impulse noise categories (i.e., all episodic categories except gunfire) with routine exposure values according to the methods described above. An example of the ANE calculation for an individual subject is given in Appendix B.
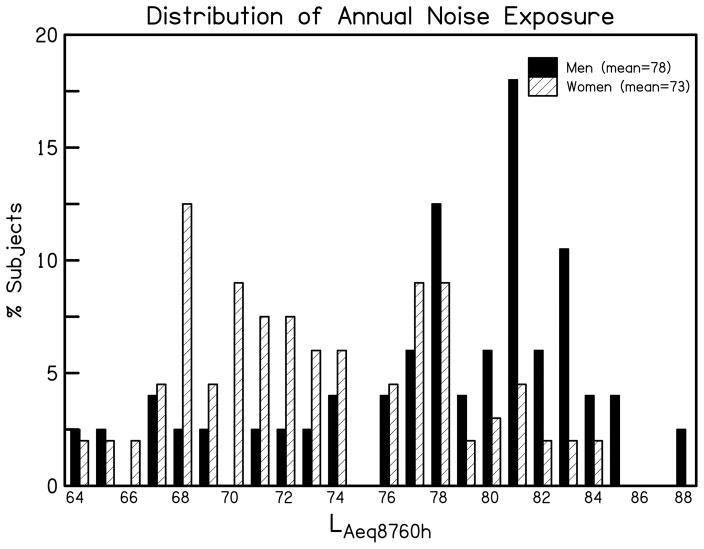
Figure 3 and Table 3 show the range of ANE values for all subjects. If a subject reported minimal or no participation in episodic noise activities, then routine exposures would form the basis of their ANE, resulting in an annual exposure of 64 LAeq8760h (the minimum possible value). ANE values for the group ranged from 64 to 88 LAeq8760h with a mean of 75 LAeq8760h. The mean ANE was higher in men than women (78 LAeq8760h versus 73 LAeq8760h). This was expected, given men reported more frequent participation in high-level episodic noise activities, such as the use of power tools and heavy equipment.
Figure 3.
Distribution of Annual Noise Exposure (ANE) values in LAeq8760h for the subjects participating in aim 1. Results for men and women are displayed separately, as indicated in the legend.
Table 3.
Annual Noise Exposure (ANE) in LAeq8760h for all subjects.
| LAeq8760h
|
|||||
|---|---|---|---|---|---|
| Range | 10thPercentile | 50thPercentile | 90thPercentile | Mean | |
| All Subjects | 64–88 | 68 | 77 | 83 | 75 |
| Men | 64–88 | 68 | 80 | 83 | 78 |
| Women | 64–84 | 68 | 72 | 80 | 73 |
Determination of “Highest Risk” Noise Exposures
The determination of what LAeq8760h value is considered “high risk” varies depending on which criterion is used to assess risk. Basing extrapolated annual risk on an occupational criterion such as NIOSH (1998) results in values ≥ 79 LAeq8760h being considered highest risk. The EPA considers ANE values ≥ 71 LAeq8760h as high risk. Table 4 summarizes the number and percentage of subjects in the current study who met highest-risk criteria for NIHL based on their responses to the questionnaire. As expected, when using the higher cutoff of 79 LAeq8760h, a smaller number of subjects are considered at high risk for NIHL when compared to the EPA criterion. Because unprotected exposure to gunfire is generally considered to pose a risk to hearing (e.g., Dobie, 2001; Fligor, 2010; Neitzel et al, 2004a, b), Table 4 also lists subjects who reported firearm exposure, regardless of whether or not the subjects reported wearing hearing protection. We will return to the issue of hearing protection in the discussion.
Table 4.
Subjects meeting high risk criteria for NIHL.
| Subjects Meeting Criteria
|
||||
|---|---|---|---|---|
| All Subjects(n=114) | Men(n=49) | Women(n=65) | ||
| Current Study (≥ 79 LAeq8760h) | Count | 36 | 27 | 9 |
| Percentage | 32% | 55% | 14% | |
|
| ||||
| EPA (≥ 71 LAeq8760h) | Count | 85 | 43 | 42 |
| Percentage | 75% | 88% | 65% | |
|
| ||||
| Firearm Exposure | Count | 35 | 21 | 14 |
| Percentage | 31% | 43% | 22% | |
Aim #2: Development of the 1-Minute Noise Screen
The second objective of this study was to develop a set of screening questions that could be used to identify individuals at high risk for NIHL. This could be of interest to clinicians in busy practices and school settings because it would allow them to more quickly identify individuals likely to be highest risk who would benefit from a more in-depth assessment of their ANE.
The six potential screening questions (Q#1–6) were evaluated for their ability to predict self-reported noise exposure (i.e., as defined by the ANE value). Multiple linear regression analyses revealed that a model consisting of all six screening questions was statistically significant (F = 12.65; p < 0.001). The r2 value indicated that approximately 42% (r2=0.415) of the variance in ANE could be accounted for by the six screening questions. However, only three items significantly contributed to the overall model. These three variables included firearm usage (Q#1; p=0.001, B=2.24, SE=0.65), working a noisy job (Q#2; p=0.000, B=1.56, SE=0.34), and exposure to any other loud noise (Q#3; p=0.002, B=1.36, SE=0.43). As expected, the relationship between these variables was positive; indicating that increasing frequency of participation in these noisy activities was associated with increasing ANE.
In contrast, the three screening items that assessed rate at which auditory symptoms were experienced (Q#4: tinnitus, Q#5: TTS, or Q#6: other ear symptoms) were not found to be significant predictors of ANE. Two symptoms, TTS and other ear symptoms, showed a negative relationship with the high-risk measure. In other words, for these subjects a higher occurrence of these symptoms was associated with lower ANE values, although this relationship was not statistically significant (p>0.05).
Based on results of the regression analyses, the following questions were selected for inclusion in the 1-Minute Hearing Screen: Q#1, gunfire usage (p<0.001, B=2.40, SE=0.62); Q#2, noisy job (p<0.001, B=1.50, SE=0.33); Q#3, any other loud noise (p=0.003, B=1.23, SE=0.41). Screening items based on symptoms (tinnitus, temporary shift in hearing, and ear pain/fullness/other symptom) were rejected due to insufficient association with LAeq8760h. The final regression model indicated that these three screening questions were able to account for 40% of the variance (r2=0.400, p=<0.0001) in LAeq8760h.
Sensitivity and Specificity of the 1-Minute Noise Screen
While the regression model containing Q#1–3 described above was statistically significant, clinical decision theory (Swets, 1988; Swets & Pickett, 1982) was used to evaluate the accuracy with which the 1-Minute Noise Screen could be used to screen for subjects at highest risk for NIHL. To complete this analysis, data were collected from a new group of 59 subjects. These subjects completed both the 1-Minute Noise Screen (Q#1–3) and the full, detailed NEQ (Q#7–17). This yielded a screening score for each subject that could be compared to the LAeq8760h value obtained from the full NEQ. Here, the subject’s LAeq8760h value is considered the gold-standard for determination of NIHL risk. Using our cutoff for exposure limit, subjects with LAeq8760h values ≥ 79 were considered highest risk. Screening scores were generated by assigning numerical values to each of the five possible response alternatives on the screening questions (never=0, every few months=1, monthly=2, weekly=3, and daily=4). By obtaining a mathematical sum, a screening score was generated (0 to 12) and evaluated for its ability to predict the LAeq8760h value.
When using the screening score to predict risk based on the LAeq8760h value, the area under the relative operating characteristic curve (AROC) was 0.937, significantly better than chance (p<0.0001). This suggests that the screening score can be used to identify those subjects at highest risk for NIHL. Table 5 lists sensitivity and specificity values for several possible screening scores. A screening score of ≥ 5 provides the best balance between sensitivity and specificity. However, it is possible to choose other scores to indicate risk according to the needs of a given population. For example, a screening score of ≥ 3 could be chosen to indicate risk in cases where it is more important to identify individuals who may be at highest risk of NIHL than it is to reduce the number of individuals who complete the detailed NEQ but do not have high LAeq8760h values. In this scenario, the high sensitivity obtained for a screening score of 3 was prioritized over the lower specificity.
Table 5.
Sensitivity and specificity values for several possible screening scores. A score greater than or equal to the screening score value would be interpreted as positive for noise exposure exceeding our criterion for highest risk(LAeq8760h > 79).
| ScreeningScore | Sensitivity | Specificity |
|---|---|---|
| ≥ 3 | 1.00 | 0.596 |
| ≥ 4 | 0.917 | 0.702 |
| ≥ 5 | 0.917 | 0.830 |
| ≥ 6 | 0.833 | 0.894 |
DISCUSSION
Quantification of Annual Noise Exposure
The data reported here describe the development of a task-based questionnaire that can be used to quantify an individual’s annual noise exposure (ANE). The Noise Exposure Questionnaire (NEQ) differs from other similar questionnaires that have been developed (i.e., Neitzel et al., 2004a; Schmidt et al., 2014) by querying both occupational and non-occupational exposures and by being applicable to the general population. One potential advantage of using a questionnaire like the NEQ to query history of noise exposure is that the respondents are asked to report not only participation in noisy activities but also to quantify the time spent in those activities. It is the combination of sound level and duration that increases a subject’s risk. It is difficult to fully ascertain an individual’s risk through standard case history approaches. These typically focus on whether a person participates in noisy activities but typically do not systematically quantify the time spent in these activities or the level to which the individual is exposed during each activity.
An example of this is that, although reported participation in episodic noise activities, such as music listening under earphones, is commonly viewed as evidence that young people are exposed to a great deal of noise, simple rates of participation miss the more important combination of both sound level and duration or regularity of exposure. In our sample (aim 1), listening to music through earphones was reported by 86% of subjects and represents an activity with high frequency of participation (mean of 250 hours per year), but a relatively low sound level (mean typical listening level of 76 LAeq). Listening to music via earphones would, therefore, contribute only a 1.5% dose to an individual’s overall ANE calculation. In contrast, operating heavy machinery such as tractors or lawn equipment carries a relatively low participation frequency (mean for our group was 20 hours per year) but high sound level (mean typical sound level of 97 LAeq). Exposure to heavy equipment/machinery for only 20 hours per year would contribute a much higher dose, 15%, to an individual’s ANE calculation. Therefore, when estimating an individual’s risk of developing NIHL, it is imperative that both sound level and exposure time be taken into account.
When compared to reports in the literature, our overall ANE results (mean for all subjects LAeq8760h =75, see Table 3) are comparable to the available 24-hour LAeq studies. Investigations of daily non-occupational noise exposures of adults in the United States have resulted in mean values of 74 to 77 LAeq24h (Banach & Berger, 2003; Berger & Kieper, 1994; Neitzel et al., 2004b; Schori & McGatha, 1978; Thompson et al., 2003). Studies outside the United States have yielded similar results, 73 to 76 LAeq24h (Garcia & Garcia, 1993; Kono et al., 1982; Zheng et al., 1996). Our data are also comparable to the annual non-occupational exposures reported by Neitzel et al. (2004a) for construction workers. Neitzel et al. reported the mean annual exposure for their group to be 73 LAeq6760h. The 6760-hour non-occupational exposure metric can be considered interchangeable with LAeq8760h values in cases where there is no occupational exposure (i.e., it is assumed that the subject’s activities for the remaining 2000 hours would be equivalent to the derived non-occupational exposure values). Although our quantification of ANE included occupational exposures, because the majority of our subjects were full-time students, occupational noise exposure rates were relatively low (see Fig. 3) and the majority of the exposures for our subjects came from non-occupational sources.
Although the NEQ can be used to provide a more complete picture of a subject’s noise exposure history and his or her risk of NIHL compared to standard clinical history techniques, it is important to recognize the limitations of the instrument. Reliance on questionnaires for calculating ANE values may be limited by subject recall or understanding of the survey. Surveys such as the NEQ also rely on typical sound levels as reported in the literature for various noise activities. In reality, there are large ranges of possible sound level experiences, and assuming all subjects are exposed to midpoint sound levels may result in a somewhat crude estimate. Despite these limitations, protocols utilized here were previously validated in other studies (Neitzel et al., 2004a; Reeb-Whitaker et al., 2004; Seixas, 2004). Furthermore, estimates of annual exposure require consideration of infrequent (episodic) noise activities, not just daily (routine) exposures. Capturing both frequent and infrequent exposures with dosimetry would require a subject to wear the dosimeter continuously for a year, which is not realistic. A task-based questionnaire, such as the NEQ, is a more feasible approach to obtaining an ANE estimate.
It should be noted that the NEQ includes a question regarding impulse noise exposure (firearms, Q#12) that is not used in the calculation of the ANE estimate. Although it is well known that high-level impulse noise exposure can be hazardous to hearing, there are no accepted protocols for integrating impulse noise exposure into an ANE estimate based on continuous noise sources. Although exposure to gunfire was not used in the computation of LAeq8760h, participation in this activity should be considered to place the person at risk for NIHL. The NEQ also queries regarding use of hearing protection devices (HPDs) when participating in the various episodic noise activities. No attempt was made to adjust the sound level estimates to account for the use of HPDs because the NEQ was designed to quantify the environmental exposure, as is typical in occupational noise monitoring programs, and not the quality of the protection strategy.
Although neither impulse noise exposure nor HPD use are incorporated into the calculation of LAeq8760h, their inclusion on the NEQ provides the audiologist important information for counseling individuals regarding risks associated with impulse noise and use of HPDs. While 31% of our sample reported exposure to gunfire, only 47% of our subjects reported using HPDs sometimes or always when firing a gun. Similar findings were reported recently by Stewart et al. (2014) where 25% of young (10–17 years) recreational firearm users reported usually or always wearing HPDs while hunting and 72% reported usually or always wearing HPDs while target shooting. Counseling regarding the hazards associated with impulse noise and need to use HPDs consistently remains an area of need. By examining an individual’s responses regarding the frequency with which HPDs were used for various episodic noise activities, the audiologist can more appropriately counsel regarding the need to add, modify, or continue HPD use.
Screening for Individuals at High Risk of NIHL
In addition to developing a tool for quantifying ANE, our second aim was to develop a tool, the 1-Minute Noise Screen, for screening for high-risk noise exposure. Regression analyses revealed that only three of our six proposed screening items adequately predicted high risk noise exposure for our subjects. The three questions included in the final screening model assessed a subject’s exposure over the previous year to firearms (Q#1), a noisy job (Q#2), and any other loud (recreational) noise (Q#3). The proposed screening questions that assessed regularity of ear/hearing symptoms (tinnitus, TTS, other ear symptoms) did not contribute to the prediction capabilities of the final screening model and were excluded from the 1-Minute Noise Screen.
Because NIHL is a result of damage to the inner ear, certain ear/hearing symptoms are often associated with the progression of hearing loss due to noise exposure. TTS and tinnitus are frequently reported in the NIHL literature (e.g., Chung et al., 2005; Holgers & Pettersson, 2005), while ear pain or a feeling of fullness in the ears are only occasionally listed as possible symptoms of noise exposure (IOM, 2005; Ward et al, 2000). Other studies have found that subjects attribute ear symptoms, including tinnitus, to causes other than noise (Jokitulppo & Bjork, 2002) and that there may be a long delay (23 years, on average) in the appearance of tinnitus as a clinical complaint following the start of a noisy job (Axelsson & Prasher, 2000). Given this inconclusive relationship between ear symptoms and noise exposure, it may not be surprising that tinnitus, TTS, and other ear pain/symptoms were not clear predictors of ANE. It is likely that these ear symptoms are not highly specific to noise and/or are not sufficiently predictive of early noise exposure.
The three items that were included in the 1-Minute Noise Screen were shown to predict risk based on ANE values in a new group of subjects (aim 2) with a high degree of accuracy (AROC=0.937). The data provided in Table 5, where sensitivity and specificity values are given for various screening scores, allow flexibility in the implementation of the screening tool. Circumstances where it may be important to identify all individuals at risk would suggest the use of a lower screening score (i.e., 3 or 4) as the referral criterion. In contrast, in circumstances where it is more important to reduce the number of likely false positives, a higher screening score (i.e., 5 or 6) would be a more appropriate criterion. The costs associated with a false positive are primarily the time involved in administering and interpreting results of the full NEQ and time spent discussing hearing-conservation activities, so there may be less incentive to reduce false positives than for other screening tests where the diagnostic procedure is more costly or invasive.
It should be emphasized that the current study relied on higher cutoff exposure limits than those recommended by the EPA (1974) due to our desire to identify subjects who may be at highest risk. Should future investigators wish to apply more stringent criteria, or if the state of knowledge regarding noise risk changes, then adjustments to the recommended exposure limit can be made accordingly. Stamper and Johnson (2015) explored the relationship between ABR wave I amplitude and ANE (quantified via the NEQ) in a group of normal-hearing, young adults. Their data suggested that ABR amplitude for high-level stimuli decreased as ANE increased. There was considerable variability in their data, but there did not appear to be one exposure level that would clearly separate those with small ABR amplitudes from those with large ABR amplitudes. Instead, the relationship between the two variables appeared to be continuous. The Stamper and Johnson data need to be replicated; however, to the extent that ABR amplitude reflects the number of afferent fibers contributing to the response in humans, as has been shown in animals (e.g., Kujawa & Liberman, 2009), these results may indicate the need to reassess noise hazards. Until it is clearer whether noise exposure can produce permanent damage in humans prior to permanent threshold shift, tools like the NEQ can be useful for counseling subjects regarding their behavior and risk of damage to their auditory systems.
Conclusions
In summary, the data described here illustrate the development of a task-based questionnaire, the NEQ, that can be used to estimate a subject’s annual noise exposure, and the development of a screening tool, the 1-Minute Noise Screen, that can be used to screen for subjects who are at risk of NIHL. The final version of the detailed NEQ is available in Appendix C and the 1-Minute Noise Screen is available in Appendix D. Additionally, an Excel worksheet that can be used to calculate ANE based on responses on the NEQ is available by contacting the authors. These tools can be used by audiologists to help focus hearing-conservation efforts on those individuals who are at greatest risk of NIHL.
Supplementary Material
Acknowledgments
This work was supported by a Dissertation Fellowship from the University of Kansas Graduate School and a grant from the National Institutes of Health (NIH) National Institute on Deafness and Other Communication Disorders (NIDCD) R03 DC011367. Portions of this work were presented at the 2013 Innovations in Noise-Induced Hearing Loss and Tinnitus Prevention in Kids Conference, St. Paul, MN.
Abbreviations
- ABR
auditory brainstem response
- ANE
annual noise exposure
- AROC
area under the relative operating characteristic curve
- C
number of hours per year in which a subject is engaged in an activity; used in calculation of sound-exposure dose
- D
sound exposure dose
- dB
decibels
- dBA
A-weighted decibels
- EPA
Environmental Protection Agency
- HPD
hearing protection device
- LAeq24h
continuous sound level averaged over 24 hours using a 3-dB exchange rate and A-weighted sound levels
- LAeq2000h
continuous sound level averaged over 2000 hours using a 3-dB exchange rate and A-weighted sound levels
- LAeq8760h
continuous sound level averaged over 8760 hours using a 3-dB exchange rate and A-weighted sound levels
- NEQ
Noise Exposure Questionnaire
- NIHL
noise-induced hearing loss
- NIOSH
National Institute for Occupational Safety and Health
- OSHA
Occupational Safety and Health Administration
- T
number of hours of exposure per year at which the activity is considered hazardous using recommended exposure limits; used in the calculation of sound-exposure dose
- TTS
temporary threshold shift
References
- Airo E, Pekkarinen J, Olkinuora P. Listening to music with earphones: An assessment of noise exposure. Acta Acust United Acust. 1996;82:885–894. [Google Scholar]
- Anttonen H, Virokannas H, Sorri M. Noise and hearing loss in reindeer herders. Arctic Med Res. 1994;53(Suppl 3):35–40. [PubMed] [Google Scholar]
- Axelsson A. Recreational noise exposure and its effects. Noise Control Engineering Journal. 1996;44:127–34. [Google Scholar]
- Axelsson A, Prasher D. Tinnitus induced by occupational and leisure noise. Noise Health. 2000;8:47–54. [PubMed] [Google Scholar]
- Banach J, Berger EH. What we do to ourselves: Noise exposures beyond work. CAOHC Update. 2003;15:6–7. [Google Scholar]
- Berger EH, Kieper RW. Representative 24-hour Leqs arising from a combination of occupational and non-occupational noise exposures. J Acoust Soc Am. 1994;95:2890. [Google Scholar]
- Bess F, Poynor R. Noise-induced hearing loss and snowmobiles. Arch Otolaryngol. 1974;99:45–51. doi: 10.1001/archotol.1974.00780030049008. [DOI] [PubMed] [Google Scholar]
- Carter L, Williams W, Black D, Bundy A. The leisure-noise dilemma: hearing loss or hearsay? What does the literature tell us? Ear Hear. 2014;35:491–505. doi: 10.1097/01.aud.0000451498.92871.20. [DOI] [PubMed] [Google Scholar]
- Chasin M. Hearing loss prevention for musicians. In: Chasin M, editor. Hearing Loss in Musicians: Prevention and Management. San Diego: Plural Publishing; 2009. p. 3. [Google Scholar]
- Chung JH, Des Roches CM, Meunier MS, Eavey RD. Evaluation of noise-induced hearing loss in young people using a web-based survey technique. Pediatrics. 2005;115:861–7. doi: 10.1542/peds.2004-0173. [DOI] [PubMed] [Google Scholar]
- Cohen A, Anticaglia J, Jones H. ‘Sociocusis’ –hearing loss from non-occupational noise exposure. Sound and Vibration. 1970;4:12–20. [Google Scholar]
- Dobie RA. Medical-Legal Evaluation of Hearing Loss. 2. San Diego: Singular Publishing Group; 2001. pp. 138–173. [Google Scholar]
- Dobie RA. The burdens of age-related and occupational noise-induced hearing loss in the United States. Ear Hear. 2008;29:565–77. doi: 10.1097/AUD.0b013e31817349ec. [DOI] [PubMed] [Google Scholar]
- Environmental Protection Agency. Information on levels of environmental noise requisite to protect public health and welfare with an adequate margin of safety. Washington, DC: 1974. EPA Rep. No. 550/9-74-004. [Google Scholar]
- Fallentin N, Juul-Kristensen B, Mikkelsen S, Andersen JH, Bonde JP, Frost P, Endahl L. Physical exposure assessment in monotonous repetitive work – the PRIM study. Scand J Work Environ Health. 2001;27:21–9. doi: 10.5271/sjweh.583. [DOI] [PubMed] [Google Scholar]
- Flamme GA, Stephenson MR, Deiters K, Tatro A, VanGessel D, Geda K, Wyllys K, McGregor K. Typical noise exposure in daily life. Int J Aud. 2012;51:S3–S11. doi: 10.3109/14992027.2011.635316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fligor B. Recreational noise and its potential risk to hearing. Hearing Review. 2010;17:48–55. [Google Scholar]
- Fligor B, Ives T. Does earphone type affect risk for recreational noise-induced hearing loss?. Paper presented at Noise-Induced Hearing Loss in Children at Work and Play Conference; October; Cincinnati, OH. 2006. [Google Scholar]
- Franks JR, Davis RR, Krieg EF. Analysis of a hearing conservation program database: Factors other than workplace noise. Ear Hear. 1989;10:273–80. doi: 10.1097/00003446-198910000-00001. [DOI] [PubMed] [Google Scholar]
- Garcia A, Garcia AM. Measurements of noise exposure in daily life. Noise as a Public Health Problem. 1993;2:367–70. [Google Scholar]
- Hammer MS, Swinburn TK, Neitzel RL. Environmental noise pollution in the United States: Developing an effective public health response. Environ Health Perspect. 2014;122:115–119. doi: 10.1289/ehp.1307272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy People 2020 [Internet] Washington, DC: U.S Department of Health and Human Services, Office of Disease Prevention and Health Promotion; [retreived July 10, 2015 ]. Available from: http://www.healthypeople.gov/ [Google Scholar]
- Holgers K, Pettersson B. Noise exposure and subjective hearing symptoms among school children in Sweden. Noise Health. 2005;7:27–37. doi: 10.4103/1463-1741.31635. [DOI] [PubMed] [Google Scholar]
- Holt J, Broste S, Hansen D. Noise exposure in the rural setting. Laryngoscope. 1993;103:258–62. doi: 10.1288/00005537-199303000-00004. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Noise and Military Service: Implications for Hearing Loss and Tinnitus. Washington, DC: National Academies Press; 2005. [Google Scholar]
- Johnson DL, Riffle C. Effects of gunfire on hearing level for selected individuals of the inter-industry noise study. J Acoust Soc Am. 1982;72:1311–4. doi: 10.1121/1.388410. [DOI] [PubMed] [Google Scholar]
- Jokitulppo JS, Bjork E. Estimated leisure-time noise exposure and hearing symptoms in a Finnish urban adult population. Noise Health. 2002;5:53–62. [PubMed] [Google Scholar]
- Jones H, Oser J. Farm equipment noise exposure levels. Am Ind Hyg Assoc J. 1968;29:146–61. doi: 10.1080/00028896809343288. [DOI] [PubMed] [Google Scholar]
- Kono S, Sone T, Nimura T. Personal reaction to daily noise exposure. Noise Control Engineering. 1982;19:4–16. [Google Scholar]
- Kujawa SG, Liberman MC. Adding insult to injury: Cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci. 2009;29:14077–85. doi: 10.1523/JNEUROSCI.2845-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, Koch GC. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- Lempert B, Henderson TL. Occupational Noise and Hearing 1968–1972. Cincinnati, OH: 1973. NIOSH Report TR-201-74. NTIS No. PB-232 284. [Google Scholar]
- Lin HW, Furman AC, Kujawa SG, Liberman MC. Primary neural degeneration in the Guinea pig cochlea after reversible noise-induced threshold shift. J Assoc Res Otolaryngol. 2011;12:605–16. doi: 10.1007/s10162-011-0277-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClymont L, Simpson D. Noise levels and exposure patterns of do-it-yourself power tools. J Laryngol Otol. 1989;103:1140–41. doi: 10.1017/s0022215100111211. [DOI] [PubMed] [Google Scholar]
- McCombe A, Binnington J, Nash D. Two solutions to the problem of noise exposure for motorcyclists. Occup Med (Lond) 1994;44:239–42. doi: 10.1093/occmed/44.5.239. [DOI] [PubMed] [Google Scholar]
- National Institute on Deafness and Other Communication Disorders. Fact sheet: work-related hearing loss. Washington, DC: Health and Human Services; 2008. [Google Scholar]
- National Institute for Occupational Safety and Health. Criteria for a recommended standard: occupational exposure to noise. Cincinnati: USDHHS, PHS, CDC, NIOSH; 1998. publication no. 98–126. [Google Scholar]
- Neitzel R, Seixas N, Goldman B, Daniell W. Contributions of non-occupational activities to total noise exposure of construction workers. Ann Occup Hyg. 2004a;48:463–73. doi: 10.1093/annhyg/meh041. [DOI] [PubMed] [Google Scholar]
- Neitzel R, Seixas N, Olson J, Daniell W, Goldman B. Nonoccupational noise: exposures associated with routine activities. J Acoust Soc Am. 2004b;115:237–245. doi: 10.1121/1.1615569. [DOI] [PubMed] [Google Scholar]
- O’Brien I, Wilson W, Bradley A. Nature of orchestral noise. J Acoust Soc Am. 2008;124:926–939. doi: 10.1121/1.2940589. [DOI] [PubMed] [Google Scholar]
- Occupational Safety and Health Administration. Occupational noise exposure; hearing conservation amendment. Occupational Safety and Health Administration, 29 CFR 1910.95. Federal Register. 1981;46:4078–4181. [Google Scholar]
- Portnuff C, Fligor B, Arehart K. Adolescent use of portable listening devices: A hazard to hearing?. Paper presented at Annual Conference of the National Hearing Conservation Association; February; Atlanta, GA. 2009. [Google Scholar]
- Reeb-Whitaker CK, Seixas NS, Sheppard L, Neitzel R. Accuracy of task recall for epidemiological exposure assessment to construction noise. Occup Environ Med. 2004;61:135–42. doi: 10.1136/oem.2002.000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CG, Breslin M, Roper RG. Sound levels from personal cassette players. Br J Audiol. 1987;21:273–78. doi: 10.3109/03005368709076419. [DOI] [PubMed] [Google Scholar]
- Roberts G. Noise impact from motor sport activities. Noise Control Engineering Journal. 1999;47:154–157. [Google Scholar]
- Ross B. Noise exposure of motorcyclists. Ann Occup Hyg. 1989;33:123–7. doi: 10.1093/annhyg/33.1.123. [DOI] [PubMed] [Google Scholar]
- Royster LH, Berger EH, Royster JD. Noise surveys and data analysis. In: Berger EH, Royster LH, Royster JB, Driscoll DP, Layne M, editors. The Noise Manual. 5. Fairfax: American Industrial Hygiene Association Press; 2000. pp. 165–244. [Google Scholar]
- Schmidt JH, Pedersen ER, Paarup HM, Christensen-Dalsgaard J, Andersen T, Poulsen T, Bælum J. Hearing loss in relation to sound exposure of professional symphony orchestra muscians. Ear Hear. 2014;35:448–60. doi: 10.1097/AUD.0000000000000029. [DOI] [PubMed] [Google Scholar]
- Schori TR, McGatha EA. A real-world assessment of noise exposure. Sound and Vibration. 1978;12:24–30. [Google Scholar]
- Seixas N. Final report: Noise and hearing damage in construction apprentices. University of Washington School of Public Health and Community Medicine, Department of Environmental and Occupational Health Sciences; 2004. [Google Scholar]
- Smith E, Burke D, Graf E. Cabin noise in light aircraft. Proceedings of 1975 IEEE Southeastern Region 3 Conference on Electricity and Expanding Technology; Charlotte, NC: IEEE; 1975. [Google Scholar]
- Smith P, Davis A, Ferguson M, Lutman M. The prevalence and type of social noise exposure in young adults in England. Noise Health. 2000;6:4–56. [PubMed] [Google Scholar]
- Stamper GC, Johnson TA. Auditory function in normal-hearing, noise-exposed human ears. Ear Hear. 2015;36:172–84. doi: 10.1097/AUD.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson M. Noise exposure characterization via task-based analysis. Proceedings of Hearing Conservation Conference III/XX; March; Cincinnati, OH. 1995. [Google Scholar]
- Stewart M, Meinke DK, Snyders JK, Howerton K. Shooting habits of youth recreational firearm users. Int J Audiol. 2014;53:S26–S34. doi: 10.3109/14992027.2013.857437. [DOI] [PubMed] [Google Scholar]
- Susi P, Goldberg M, Barnes P, Stafford E. The use of a task-based exposure assessment model (T-BEAM) for assessment of metal fume exposures during welding and thermal cutting. Appl Occup Environ Hyg. 2000;15:26–38. doi: 10.1080/104732200301827. [DOI] [PubMed] [Google Scholar]
- Suter A. Standards and Regulations. In: Berger EH, Royster LH, Royster JD, Driscoll DP, Layne M, editors. The Noise Manual. 5. Fairfax: American Industrial Hygiene Association Press; 2000. pp. 639–668. [Google Scholar]
- Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–193. doi: 10.1126/science.3287615. [DOI] [PubMed] [Google Scholar]
- Swets JA, Pickett RM. Evaluation of Diagnostic Systems: Methods from Signal Detection. New York: Academic; 1982. [Google Scholar]
- Thompson E, Berger EH, Hipskind N. Reporting 24-hour Leqs arising from the non-occupational noise exposed population in the 21st century. Poster presented at the 28th Annual Conference of the National Hearing Conservation Association; February; Dallas, TX. 2003. [Google Scholar]
- Tobias J. Cockpit noise intensity: Fifteen single-engine light aircraft. Aerosp Med. 1969;40:963–6. [PubMed] [Google Scholar]
- U.S. Office of Noise Abatement and Control. Protective noise levels: Condensed version of EPA levels document. Springfield, VA: Environmental Protection Agency; 1978. [Google Scholar]
- Ward WD, Royster JD, Royster LH. Auditory and non-auditory effects of noise. In: Berger EH, Royster LH, Royster JD, Driscoll DP, Layne M, editors. The Noise Manual. 5. Fairfax: American Industrial Hygiene Association Press; 2000. pp. 123–148. [Google Scholar]
- Williams W. Noise exposure levels from personal stereo use. Int J Audiol. 2005;44:231–236. doi: 10.1080/14992020500057673. [DOI] [PubMed] [Google Scholar]
- Worthington D, Siegel J, Wilber L, Faber B, Dunckley K, Garstecki D, Dhar S. Comparing two methods to measure preferred listening levels of personal listening devices. J Acoust Soc Am. 2009;125:3733–3741. doi: 10.1121/1.3125798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yassi A, Pollock N, Tran N, Cheang M. Risks to hearing from a rock concert. Can Fam Physician. 1993;39:1045–50. [PMC free article] [PubMed] [Google Scholar]
- Zheng D, Cai X, Song H, Chen T. Study on personal noise exposure in China. Applied Acoustics. 1996;48:59–70. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.