Abstract
The blood-brain barrier is a physical and physiological barrier that protects the brain from toxic substances within the bloodstream and helps maintain brain homeostasis. It also represents the main obstacle in the treatment of many diseases of the central nervous system. Among the different approaches employed to overcome this barrier, the use of nanoparticles as a tool to enhance delivery of therapeutic molecules to the brain is particularly promising. There is special interest in the use of magnetic nanoparticles, as their physical characteristics endow them with additional potentially useful properties. Following systemic administration, a magnetic field applied externally can mediate the capacity of magnetic nanoparticles to permeate the blood-brain barrier. Meanwhile, thermal energy released by magnetic nanoparticles under the influence of radiofrequency radiation can modulate blood-brain barrier integrity, increasing its permeability. In this review, we present the strategies that use magnetic nanoparticles, specifically iron oxide nanoparticles, to enhance drug delivery to the brain.
Keywords: magnetic nanoparticles, IONs, blood-brain barrier
1. Introduction
Despite the extremely large surface area of the 100 billion capillaries contained in the human brain (approximately 20 m2), the capacity of many substances to pass from blood to brain is low due to the existence of the blood-brain barrier (BBB). This barrier, no equivalent of which exists in circulation through other organs, consists of tightly interconnected endothelial cells that form the circumferential interior lining of the walls of the cerebral blood vessels. The brain capillary endothelial layer is morphologically distinct from the endothelial cells in the rest of the body due to the absence of fenestrations, reduced pinocytic activity and more extensive tight junctions [1]. The tight junctions of the BBB cause a much higher transendothelial electrical resistance (TEER) than that of other tissues, which reduces intercellular space and makes it less permeable with regard to aqueous-based paracellular transport. The tight junctions are composed of smaller subunits formed by proteins [2], which, in turn, are bound to the endothelial cells by other proteins. Moreover, the BBB is equipped with many proteins, such as P-glycoprotein (P-gp) and multidrug resistance protein (MRP), that act as efflux proteins. These proteins are ATP-dependent and pump many foreign substances out of cells, including many therapeutic agents.
The BBB prevents harmful substances from entering the brain. In this way, it protects against infiltration by bacteria, viruses and other foreign material [3], and, by extension, it precludes most molecules from entering the central nervous system (CNS). According to Pardridge [3], more than 98% of small molecules, including therapeutics, do not cross the BBB. Only some gases (O2 and CO2, for example) and some small lipophilic substances diffuse freely across the BBB (passive transport). Other substances, such as glucose and amino acids, which are crucial for neural functioning, are allowed to pass into the brain extracellular fluid by selective transport, that is, by receptor-mediated transport (RMT) or carrier-mediated transport (CMT). The movement of large peptides and proteins across the BBB is facilitated by RMT. The insulin receptor, the transferrin receptor, and the insulin-like growth factor receptor are examples of endogenous receptors located at the BBB.
CMT carries small molecules (Mw < 600 Da) as it delivers nutrients, vitamins, and hormones to the CNS. A third mechanism by which substances may cross the BBB is vesicular transport, which is facilitated by either receptor-mediated or adsorptive-mediated transcytosis, possibly induced by cationic proteins [4].
Effective treatment of most CNS diseases requires the delivery of therapeutic agents to the brain. For this, a drug must cross the BBB in pharmacologically significant amounts, and this is only possible if the drug has the following characteristics: (1) a molecular mass less than 400 to 500 Da; and (2) a high lipid solubility. In particular, this is the case for psychiatric drugs. Unfortunately, many drugs that could be useful for CNS disorders cannot be given because they do not cross the BBB. Numerous attempts have been made to achieve efficient delivery of drugs to the CNS; strategies employed are invasive or noninvasive [5] An invasive method would involve overcoming the physiological barrier of the BBB through temporary osmotic opening, intracerebral infusion or intracerebral implantation (e.g., drug loaded wafer) [6,7]. Transcranial delivery can only deliver drugs near the injection site and, moreover, is ineffective if a uniform distribution of the drug to the entire brain is required [6]. All the invasive procedures are associated with high risk [3,8]. Moreover, hyperosmolar or transcranial techniques are surgical procedures that are not amenable to daily use. A noninvasive method consists of chemical modification of drugs (i.e., conjugation of cell-penetrating peptides), inhibition of efflux transporters and delivery through endogenous transporters (i.e., carrier-mediated transport for glucose or amino acids). The above-mentioned methods offer improvements of treatment outcomes. However, these methods are also associated with side effects. Therefore, finding ways to administer drugs effectively and safely to the CNS is a formidable challenge.
Over the last decade, attention has focused on nanoparticles (NPs) as new drug delivery agents that can transport drugs across the BBB and increase their uptake in the brain [9]. The important advantages of NP-drug complexes over their corresponding free drugs are mainly due to prolonged blood circulation. Increasing the duration of the circulation of a drug in the blood increases its capacity to interact with specific transporters or receptors expressed on the luminal side of the BBB endothelial cells and, consequently, to cross the BBB. Another important advantage of any nanotechnological approach, compared with the administration of a free drug, is that the important requirement of reaching the CNS while producing few systemic effects can be achieved by supporting parts of the nanoscale complex.
Poly(butyl cyanoacrylate) (PBCA) NPs were the first NPs that were used for in vivo delivery of drugs to the brain. This polymer has the advantage of being extremely rapidly biodegraded. Various modifications have been employed to increase the efficacy of these NPs across the BBB. One of the most used modifications has been overcoating the NPs with a surfactant, the polysorbate 80. The first drug that was delivered to the brain using these NPs was the hexapeptide dalargin (sequence: YAGFLR); a leucine-enkephalin analogue with opioid activity that does not cross the BBB by itself [10,11]. Other drugs that, after incorporation in polysorbate 80-coated PBCA NPs, have been transported across the BBB are the dipeptide kytorphin, loperamide, tubocurarine, doxorubicin, tacrine, and rivastigmine, among others [12,13].
Among the possible BBB penetration routes available to NPs, RMT has been shown to be the most efficient transport mechanism. RMT takes place on the luminal side, after which the compound moves through the cytoplasm of the endothelial cell and is finally exocytosed into the brain capillary endothelium. This mechanism requires the surface of the NPs to be coated with endogenous ligands or peptidomimetic antibodies. Commonly used endogenous ligands are transferrin [14,15], lactoferrin [16,17], the low-density lipoprotein (LDL) receptor [13] and insulin [18].
In the context of using NPs to improve penetration of the BBB, magnetic nanoparticles (MNPs) are of special interest, since brain cells are quite sensitive to MNPs, compared to, say, liver and heart cells [19,20]. The responsiveness of MNPs to an external magnetic field is an important factor in facilitating uptake by brain cells. Moreover, the permeability of the BBB between adjacent endothelial cells (tight junctions) is known to increase in response to physiologically relevant temperature increases (38–39 °C) [21,22]. In this way, the moderate heat dissipated from MNPs under the effect of a low radiofrequency (RF) field can increase the permeability of the BBB without perturbing other brain cells.
In this paper, we review the use of MNPs, specifically of iron oxide nanoparticles (IONs), as an appealing strategy that facilitates crossing of the BBB in therapeutic or diagnostic applications.
2. Magnetic Nanoparticles
MNPs are currently used in various biomedical applications: as a contrast agent for magnetic resonance imaging (MRI) [23], to induce hyperthermia in tumor therapy [24], for cell labelling and cell separation [25], in targeted therapeutics [26], in magnetofection [27], etc. However, uses of MNPs in the brain have been somewhat limited, due in part to a 30–50 cm working distance requirement for humans and FDA limits on the magnetic field strength used on human subjects (8 T for adults, 4 T for children) [28].
All materials present some extent of magnetism; the extent varies depending on their atomic structure and the temperature. The magnetic properties arise from the electrons circulating around atomic nuclei, from the electrons spinning on their axes and from the rotating positively charged atomic nuclei. Nuclei and electrons constitute magnetic dipoles, also called magnetons. Altogether, these effects may cancel out such that a given type of atom may not be a net magnetic dipole. If they do not fully cancel out, however, the atom is a permanent magnetic dipole. This is the case of iron atoms. The strength of a magnetic dipole is called the magnetic moment and may be thought as the quantity that determines the torque it will experience in an external magnetic field. Materials with stable magnetic properties are called ferromagnets. If the magnetic properties only exist in the presence of an external magnetic field, the material is a paramagnet. A ferromagnet becomes a paramagnet above a certain temperature called the Curie temperature (TC): the temperature at which there is a change in the direction of the intrinsic magnetic moments.
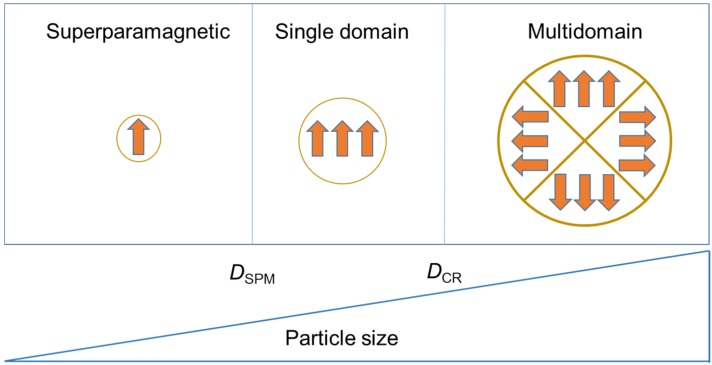
Fundamental changes occur in magnetic materials when their physical size is reduced. In ferromagnetic materials, magnetons are associated within groups called domains. A magnetic domain is a volume of material in which all the magnetons remain aligned in the same direction by exchanging forces (Figure 1). The reduction of the size of a ferromagnetic material below a critical value, the so-called critical diameter DCR, becomes the material in a single domain. The value of DCR is typically a few tens of nanometres and depends on the material. A single domain particle presents all the spins aligned in the same direction. If the size is further reduced, below the superparamagnetic diameter, DSPM, the ferromagnetic material is transformed into a superparamagnetic one. In this case, the magnetic properties are only evident in the presence of an external magnetic field. As for DCR, the value of DSPM depends on the material.
Figure 1.
Magnetic regimes of ferromagnetic materials as a function of their size (superparamagnetic, single domain, multidomain).
IONs are a subtype of MNPs that are highly magnetizable and have a core of iron oxide particles composed of magnetite (Fe3O4) or maghemite (γ-Fe2O3). This core exerts a low level of toxicity as it gradually degrades to Fe3+ in the body and is integrated into the iron stores of the body, which are used for metabolic processes and eventually eliminated from the body.
To date, a variety of synthetic methods, such as co-precipitation, thermal decomposition, hydrothermal and solvothermal syntheses, sol–gel synthesis, microemulsion, ultrasound irradiation and biological synthesis, have been used to produce IONs. The methods of synthesis can be divided into aqueous and non-aqueous routes. Aqueous approaches are characterized by their low cost and sustainability; however, there is a generic challenge in directly obtaining water-soluble monodisperse superparamagnetic IONs (SPIONs) with no size selection. Non-aqueous routes generally yield SPIONs that only dissolve in non-polar solvents [29]. The most usual and straightforward method for synthesizing SPIONs is the co-precipitation of Fe2+ and Fe3+ aqueous salt solutions by the addition of a base. Control of the size, shape and composition of SPIONs depends on the type of salts used, the Fe2+ to Fe3+ ratio, and the pH and ionic strength of the media [30]. A major advantage of the properties of SPIONs is that they are only magnetized in the presence of a magnetic field. A magnet can therefore be used to direct the delivery of the SPIONs to a given target zone [31]. Under the influence of the magnetic field, the SPIONs are moved toward the magnet and concentrate near its location.
One of the first studies that related SPIONs with the permeability of the BBB was by Rousseau et al. [32]. As MNPs cannot cross the BBB, it was opened by intracarotid injection of mannitol. The study showed that SPIONs crossed the BBB 12 h after mannitol injection, at a time when brain permeability for molecules had returned to normal. Recently, Sun et al. [33] found that two formulations of SPIONs were unable to permeate a monolayer of bEnd.3 cells. Only after disrupting the tight junctions with d-mannitol did the flux of SPIONs across the cells increase.
Owing to their inability to cross the BBB, studies with MNPs are in general based on three kinds of strategies. In the first, SPIONs are modified with functional ligands that target specific receptors in brain cells (examples of these ligands are antibodies, peptides and proteins) (Figure 2). In the second, an external magnetic field is applied to direct the movement of a SPION-encapsulated cargo to the brain [34]. Finally, the third strategy consists of applying a regulated RF field to the MNPs to produce heat and thereby transiently and locally open the BBB. Strategies that are specific to MNPs are the second and the third; both use physical principles derived from the magnetic properties of this kind of material: the magnetic force and heat generated by the particles under the influence of external electromagnetic radiation. Broadly speaking, the first strategy is no different from that adopted with other NPs to which a specific ligand is attached to the particle surface. However, this strategy can be combined with the second when an external magnet reinforces the vectorization achieved with the ligands.
Figure 2.
After disrupting the blood-brain barrier (BBB), nanoparticles (NPs) can accumulate at the tumor site. Receptor-mediated endocytosis of the functionalized NPs by cells overexpressing a receptor can retain NPs inside the tumor.
The transmembrane glycoprotein NMB (GPNMB) is a protein that in humans presents two isoforms: the isoform a, which has 572 amino acids, and the isoform b, which has 560 amino acids. GMPB promotes breast tumor growth and metastasis, and its expression in tumor ephitelium correlates with poor prognosis in breast cancer patients. GPNMB is expressed in various cell types, including malanocytes, osteoclasts, osteoblasts, and dendritic cells. Moreover, GPNMB is overexpressed in various cancer types (i.e., its overexpression is associated with glioma) [35]. GPNMB showed more than a 10-fold increase in the induction of protein expression compared to normal brain samples in cases of glioblastoma multiforme, the highest-grade glioma. Patients with glioblastoma multiforme have an average survival time of only around one year after diagnosis [36]. Thus, the overexpression of GPNMB is a promising target for immunotherapy for glioblastoma multiforme.
Another receptor that is also a promising marker for malignant gliomas is the epidermal growth factor receptor (EGFR). Several mutant forms of this receptor have been reported; EGFRvIII is the most common. In contrast to other EGFRs, the mutant form EGFRvIII is tumor-specific; it is not expressed in normal tissues. Hadjipanayis et al. [37] reported the possibility of targeting glioma cells with IONs conjugated to an antibody that selectively binds to EGFRvIII. Those authors demonstrated the accumulation of NPs inside the tumor after convection-enhanced delivery with subsequent inhibition of GBM. However, that approach has limited clinical relevance due to the local application of NPs. Furthermore, the specific antibodies only targeted a subpopulation of EGFRvIII-positive cells; they did not affect subsets of tumor cells with wild-type EGFR or other mutant receptor forms. Thus, the application of epidermal growth factor (EGF), which is one of several natural ligands for EGFR, could help cover all of the subsets of tumor cells that express wild-type EGFR, as well as its mutant forms. Several studies have showed the utility of targeting tumors in various models via the conjugation of EGF to NPs [38,39]. Shevtsov et al. [40] demonstrated the possibility of targeting EGFR-overexpressing brain tumors via MNPs conjugated to EGF in a C6 glioma model. In the same cellular model, Kievit et al. studied targeted gene delivery in a xenograft mouse model using NPs labelled with chlorotoxin (CTX) [41]. The nanovector they developed consisted of an ION core, coated with a copolymer of chitosan, PEG, and polyethylenimine (PEI). DNA-encoding green fluorescent protein (GFP) was bound to the NPs, and CTX was then attached using a short PEG linker. NPs without CTX were also prepared as a control. Mice bearing C6 xenograft tumors were injected via an intravenous (IV) route with the DNA-bound NPs. NP accumulation at the tumor site was monitored using MRI and analysed by histology, and GFP gene expression was monitored through Xenogen IVIS fluorescence imaging and confocal fluorescence microscopy. Interestingly, the CTX did not affect the accumulation of NPs at the tumor site, but it specifically enhanced their uptake into cancer cells as evidenced by higher gene expression. These results indicated that this targeted gene delivery system could potentially improve treatment outcomes of gene therapy for glioma and other deadly cancers.
As indicated above, lactoferrin can intervene in receptor-mediated transcytosis [42]. In this way, lactoferrin was covalently conjugated to PEG-coated SPIONs, and the efficacy of these conjugates at crossing the BBB was evaluated in an in vitro model based on primary porcine brain capillary endothelial cells (PBCECs) [43]. The results revealed that the lactoferrin-SPIONs exhibited an enhanced capacity to cross the BBB compared to the PEG-SPIONs. In good agreement with the in vitro results, further in vivo animal experiments showed a similar tendency. Other ligands that have been used to trigger receptor-mediated transcytosis are ferritin [44] and transferrin [44,45,46].
3. SPIONs Modified with Penetrating Peptides that Help to Penetrate Brain Cells
Cell-penetrating peptides are short peptides (generally not exceeding 30 residues) that have the capacity to ubiquitously cross cellular membranes, with very limited associated toxicity, without the need for chiral recognition by specific receptors [47].
The BBB-penetrating peptide, angiopep-2 (ANG, sequence: TFFYGGRGKRNNFKTEEY), was conjugated onto the surface of Pluronic F127-modified water-dispersible poly(acrylic acid)-bound iron oxide (PF127-PAAIO). The ANG-PF127-PAAIO complex showed a better feasibility than PF127-PAAIO in U87 cells (negligible cell cytotoxicity, better cellular uptake, and higher T2-weighted image enhancement) [48]. Using an ex vivo BBB model, those authors showed that it was more permeable to ANG-PF127-PAAIO, and therefore this complex was more able to bypass the BBB. This is because ANG-PF127-PAAIO has dual targeting capacity due to its recognition of the LDL receptor-related protein, which is overexpressed in both BBB and glioblastoma cells and the clathrin-mediated receptor on the U87 surface.
Another penetrating peptide is the trans-activator of transcription (Tat) protein derived from the human immunodeficiency virus (HIV) (sequence: YGRKKRRQRRR). The HIV-1 Tat peptide interacts with tight junction proteins and adhesion molecules. Such interaction results in an enhancement of the BBB permeability [49]. In this way, when Tat was used to functionalize magnetic liposomes (MLPs), the permeability of the BBB enhanced in comparison with non-functionalized MLPs when a magnetic field was applied. Moreover, MLPs accumulate significantly at a spinal cord injury site [50].
Recently, Ausciaux et al. [51] prepared ultra-small SPIONs functionalized with peptides that present an affinity for β-amyloid peptide independently of its state of aggregation. Their results have demonstrated that a SPION coupled to a cyclic heptapeptide (sequence: c-IPLPFYN-c) is capable of crossing the BBB of NMRI mice without any facilitating strategy. Around the same time, Cheng et al. [52] demonstrated that curcumin (Cur) can naturally bind to the surface of SPIONs, and that the particles showed low cytotoxicity and exhibited BBB penetration potential in an in vitro monolayer cell permeability test. In vivo, the particles can penetrate the BBB of both the Tg2576 Alzheimer’s disease (AD) model and non-transgenic mice. Cur-SPIONs bind to amyloid plaques in mouse brains, as shown by multiple detection methods. T2* ex vivo MRI revealed more dark spots in transgenic mice than in controls, and an important number of the detected dark spots were aligned with amyloid plaques on immunohistochemically dyed sections matched with magnetic resonance images. Techniques such as iron staining, fluorescence or immunohistochemistry showed co-localization of SPIONs and Cur on amyloid plaques. Therefore, Cur-SPIONs are novel NPs with potential use for visualizing amyloid plaques in AD patients. Further in vivo MRI tests in AD mice models is required to further elucidate the potential of Cur-SPIONs for early diagnosis of AD.
4. Transport of MNPs through Brain Cells by the Effect of an External Magnet
The magnetic force experienced by a magnetic particle in an applied magnetic field is given by the following equation:
| (1) |
where is the magnetic moment of the particle, calculated using the equation:
| (2) |
where, in turn, ρ is the particle density, V is the volume of magnetic material in the particle, and is the magnetization of the particle. According to Equation (2), the magnetic force experienced by a particle is proportional to ~r3; it increases with the size of the MNP. Therefore, high magnetization and a large size are necessary to ensure a strong attractive force. However, the size of the MNPs should remain small enough for them to be within the superparamagnetism regime.
4.1. In Vitro Studies
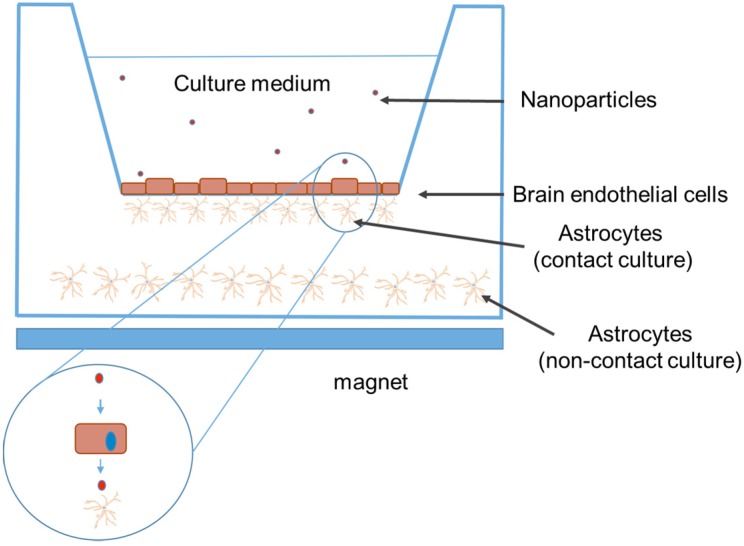
The capacity of any drug to pass through the BBB in vitro is checked in a cellular model (the BBB model). This model consists of 2-compartment wells in a culture plate with the upper compartment separated from the lower by a membrane with a pore diameter of 3 μm (Transwell™, Corning, MA, USA). On the upper side of a 24-well cell culture insert (surface area 0.3 cm2), endothelial cells grow to confluency, while a confluent layer of human astrocytes grow on the underside (Figure 3). The integrity of a monolayer of cells can be checked by TEER measurements of tight junctions. An average TEER value of 150 to 200 Ω/cm2 of cell culture insert is consistent with the formation of the BBB.
Figure 3.
Cellular model for checking the passage of drugs or NPs across the BBB. The Transwell filter consists of a porous membrane support submerged in a culture medium. Two different Transwell co-culture modes exist: non-contact and contact culture. In non-contact culture, the cells (for instance, brain endothelial cells and astrocytes) are co-cultured in two different compartments (insert membrane in well). In contact culture, astrocytes are first seeded onto the abluminal side of the inverted Transwell filter, and after adhering, the filter is flipped back, and the astrocytes are cultured for 2 days. At the end of the second day, brain cells are seeded onto the luminal side of the Transwell filter and co-cultured with astrocytes for an additional 3–4 days. The number of NPs is determined in both compartments. Superparamagnetic IONs (SPIONs) are depicted as red dots. The passage through the BBB model can be mediated by the effect of a magnet located underneath the plate.
HIV-1 seems to be harboured in the brain, as pointed out by the presence of considerable quantities of unintegrated viral DNA in the brain of HIV-infected individuals [53]. The inability of antiretroviral therapy to cross the BBB provokes the prevalence of a number of CNS disorders collectively known as neuroAIDS [54]. Several studies report monocyte/macrophage-based nanocarrier drug delivery systems for delivering antiretrovirals to the brain [55,56]. This approach uses the capacity of phagocytes to cross the BBB. Likewise, Jain et al. reported that monocytes/neutrophils mediated delivery of Arg-Gly-Asp (RGD)-anchored MLPs to the brain [57]. Saiyed et al. reported that MNPs encapsulated in liposomes are captured by monocytes and moved through an in vitro BBB model by an external magnet without modifying the TEER values [58].
To understand the cellular uptake of MNPs (polystyrene nanospheres with trapped MNPs), Kong et al. [59] imaged human brain endothelial cells (D3) treated with MNPs and studied them using atomic force microscopy. This technique demonstrated that the MNPs were internalized by the cells, suggesting that trans-cellular trafficking may be the mechanism by which the MNPs cross the BBB. That study supported a model for the use of external magnets to regulate the distribution of MNPs in in vivo models where delivery through an intact BBB is advantageous. Moreover, the study concluded that the uptake of MNPs into the brain does not seem to need any major disruption of the endothelial barrier or modification of BBB integrity.
Thomsen et al. studied the capacity of fluorescent IONs to pass through human brain capillary endothelial cells facilitated by an external magnet [60]. The MNPs consisted of a magnetite core surrounded by a lipophilic fluorescent dye covered by a hydrophilic polysaccharide matrix of starch made up of α-d-glucose units. The BBB model was a monoculture of cells in inserts in 12-well Transwell membrane culture plates that contained astrocytes. A ferrite block magnet was placed underneath the culture plates. IONs passed into and through a cellular monolayer and reached the astrocytes cultured at the bottom of the chamber in a manner that was significantly enhanced by the use of an external magnet. This passage happened in a concentration-dependent manner. The magnetic force did not alter the integrity of the endothelial monolayer, nor was cell viability altered by the IONs or by the magnetic force dragging the NPs through the cells. When IONs were added to the luminal side of BBB model, they were found in astrocytes co-cultured at a distance on the abluminal side, pointing out that the particles were transported through the barrier and capturated by the astrocytes.
In another study, MLs were used as nanoparticulate systems to study the passage through the BBB. MLs with transferrin were applied to an in vitro BBB transmigration study in the presence or absence of an external magnetic force. Compared to magnetic force- or transferrin receptor-mediated transportation alone, the combination of the two resulted in synergistic 50%–100% increased transmigration, without affecting BBB integrity [61].
4.2. In Vivo Studies
MLPs show a preference for blood monocytes/neutrophils, and this results in the incorporation of magnetism into these cells, which subsequently become magnetized cells that can respond to a magnetic field [62]. In this way, Jain et al. showed that RGD-coated MLPs encapsulating diclofenac imparted magnetic properties to monocytes/neutrophils; and, due to their trend to migrate exclusively towards inflammatory sites, under the direction of an external magnetic field, the drug could be actively targeted to any poorly accessible site such as the brain [57].
Magnetic therapy using MNPs increased the survival of glioma-bearing rats by intensifying the brain concentration of paclitaxel [63]. Chertok et al. observed that intravascularly administered NPs were passively delivered to a brain tumor even in the absence of a magnetic field. A magnetic force of 0.4 T increased the concentration of starch-coated SPIONs (which accumulated approximately fivefold in a rat brain tumor than the concentration found in non-targeted (no magnetic force applied) brain tumors) [64]. Those authors observed the presence of SPIONs injected via an IV route in the brain parenchyma of normal rat brain tissue. Thus, a possible application of SPIONs for drug delivery appears to be valid, not only for BCECs, but also for neurons and glial cells located far down inside the brain, as SPIONs moving through BCECs are likely to be taken up by these cells too. This approach was improved by the administration of the NPs via a non-occluded carotid artery. This route increased the passive exposure of tumor vasculature to the NPs [65,66]. The main potential advantage of intra-arterial (IA) administration over the IV way is that the vasculature of the tissue perfused by the injected artery acquire a higher plasma concentration during the first passage through the circulation. However, IA administration in conjunction with magnetic targeting can also have a serious pitfall: The artery exposed to a magnetic field can become mechanically occluded due to NP aggregation. The extent of NP aggregation at arterial flow rates depends on the magnetic field topography and strength [67]. Therefore, the magnetic field was reduced at the carotid injection site to achieve desirable tumor retention of NPs while avoiding undesirable arterial aggregation.
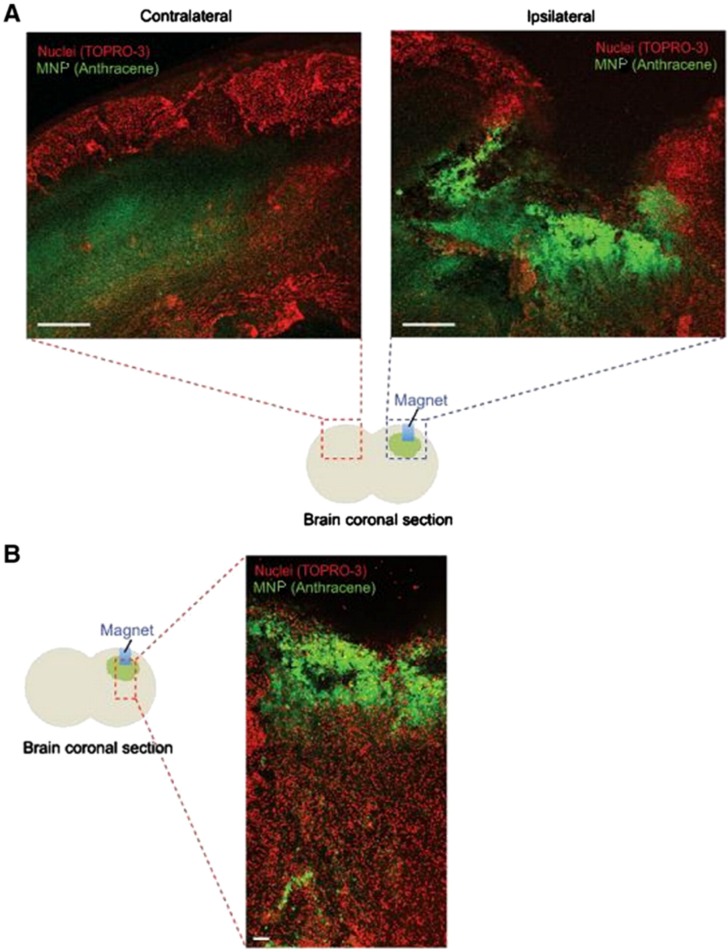
Kong et al. [59] demonstrated that MNPs can cross the normal BBB when subjected to an external magnetic field. In that study, polystyrene nanospheres that encapsulate MNPs (100 nm size) and contain a fluorophore were injected into mice. In the absence of an applied magnetic field, no preferential accumulation of the MNPs within the brain was observed. To assess how MNPs respond to an external magnetic field applied locally, a Nd-Fe-B magnet was implanted in the right hemisphere of the cerebral cortex of the mice. One week post-implantation, MNPs were delivered systemically by IV injection. After obtaining brain sections, these were laser-imaged using scanning confocal microscopy to track their distribution in the brain. In the presence of the magnetic field, the number of MNPs was higher in the ipsilateral hemisphere where the magnet was implanted in comparison to the contralateral hemisphere (Figure 4A). Within the ipsilateral hemisphere, higher MNP accumulation was observed in the cortex near the magnet, whereas areas farther from the magnet exhibited lower accumulation (Figure 4B). To avoid potential tissue damage caused by the implantation of the magnet in the brain, the authors assessed whether the distribution of MNPs could be modified by the application of a non-invasive, external magnetic field (~1 T), which was applied by placing a Nd-Fe-B magnet near the head of the mice. The number of MNPs accumulated after systemic delivery was increased ~25-fold compared to control with no-magnet.
Figure 4.
Magnetically vectored magnetic nanoparticles (MNPs) accumulate in the brain. (A) A small magnet was implanted in the right hemisphere of the brains of mice by stereotactic injection. (Blue represents the inserted magnet and green shade represents MNPs in cartoon). One week after implantation, MNPs were administered by IV injection. Confocal analysis demonstrated accumulation of the MNPs in the ipsilateral hemisphere, whereas a background level of MNPs was found in the contralateral hemisphere. Scale bar: 500 μm. (B) Confocal analysis of coronal sections of brain demonstrated enrichment of the MNPs near the magnet. Scale bar: 100 μm. Reproduced with permission of [59]. Copyright Elsevier Science, 2012.
MLPs have been used to target gliomas in vivo. In this way, Marie et al. [68] subjected these NPs to selective magnetic sorting to target glioma multiforme. Such targeting was assessed in vivo on gliomas orthopically implanted in mice. A magnetic field gradient of 190 T m −1 originated by an external 0.4 T permanent magnet located on the head of the animals effectively concentrated the MLPs in the malignant neoplasm next to the healthy brain. In vivo tracking of the MLPs in the brain was performed by quantitative MRI. Electron spin resonance spectroscopy was employed to calculate the iron oxide delivered to healthy parenchyma and tumor tissue ex vivo. Histological analysis using confocal fluorescence microscopy confirmed the significant boost in the accumulation of MLPs in the cancerous tissue up to the intracellular level. Electron transmission microscopy revealed that MLPs were effectively internalized by endothelial and glioblastoma cells. Moreover, MLPs preserved their structures.
IONs can also be encapsulated in bolaamphiphiles—amphiphilic molecules consisting of two hydrophilic headgroups linked by a hydrophobic chain. Philosof-Mazor et al. [69] studied the cell uptake of such vesicles in murine brain microvessel endothelial cells (bEnd.3 cells). They found that association of the SPIONs with the vesicles enhanced cell internalization, even in the absence of a magnetic field.
5. Increase of BBB Permeability by Magnetic Heating of Nanoparticles
MNPs present magnetic anisotropy, that is, there is a directional dependence of a material’s magnetic properties. Because of the magnetic anisotropy, the magnetic moment of a magnetic particle usually has only two stable orientations antiparallel to each other, separated by an energy barrier. The energy barrier in the simplest of cases it has uniaxial form and is given by ΔE = KV, where K is the anisotropy energy density and V is the particle volume. In superparamagnetic particles, ΔE is comparable to the thermal energy (kBT, where kB is the Boltzmann constant and T the absolute temperature) and the direction of magnetization fluctuates randomly.
The application of an external alternating magnetic field (AMF) to MNPs leads to the production of energy, in the form of heat, if the magnetic field reorients the magnetic moments of the MNPs. Such an effect can be exploited to use MNPs as mediators in magnetic hyperthermia. For multidomain ferro- or ferri-magnetic materials, the production of heat is due to hysteresis losses. Since large particles of such materials contain several sub-domains, each of them has a definite magnetization direction. When the domains are exposed to a magnetic field, those domains with magnetization direction along the magnetic field axis grow, and the other ones become smaller. In single domain particles (superparamagnetic NPs) the heating is not due to hysteresis losses because such materials do not present domain walls. In this case, the external magnetic field affords energy and helps magnetic moments to rotate in overcoming the energy barrier. This energy is vanished when the particle moment relaxes to its equilibrium orientation (Néel relaxation). This fact is characterised by the Néel relaxation time tN,
| (3) |
where typical values for t0 are between 10−9 and 10−10 s.
For both types of particles, heating can also be due to the rotational Brownian motion within a liquid in which the particles are dispersed. This rotational movement creates frictional losses to the environment (Brown relaxation). Theoretically, in superparamagnetic NPs, Néel relaxation predominates over Brown relaxation, while, for larger sizes and low viscosity media, Brown relaxation is the main rotation mechanism. In the general case, both mechanisms are present, but the faster relaxation mechanism is prevailing and an effective relaxation time, τR, can be defined as:
| (4) |
where τB is the Brown relaxation time.
At high AMF frequencies, the heat generated by the MNPs is enough to produce temperatures above 42 °C. At low frequencies, the heat should open up the BBB junctions. In order to make this a clinically viable technique, it is first essential to show that the opening of the BBB is local and entirely reversible.
Tabatabaei et al. [70,71] examined BBB permeability in rats in the presence of moderate heat dissipated via magnetic heating of MNPs by a low RF field. To verify BBB integrity, before the administration of the MNPs through the external carotid artery, fluorescent Evans blue dye was injected into the tail vein. Observation of brain samples using a 7 T magnetic resonance scanner and an epifluorescent microscope indicated a substantial but reversible opening of the BBB where hyperthermia was induced.
Dan et al. [72] used two types of SPIONs, cross-linked nanoassemblies loaded with IONs and conventional SPIONs, to study the effects of AMF-induced hyperthermia on SPION permeability and flux across the BBB. They used two in vitro modes (bEnd.3 and Madin-Darby canine kidney II cells) in Transwells™ under normothermic, conventional hyperthermic, and AMF-induced hyperthermic conditions. Their results showed that the flux across BBB models was low under normothermic condition, while AMF-induced hyperthermia for 0.5 h enhanced cross-linked-SPION cell association/uptake and flux in the absence of cell death. In contrast, SPIONs agglomerated in a cell culture medium and were taken up by, but did not flux through, the bEnd.3 BBB model. The AMF-induced hyperthermia enhanced the BBB association/uptake and permeability of cross-linked-SPIONs more effectively than conventional hyperthermia via other mechanisms in addition to the elevated temperature around the IONs. Cross-linked-SPIONs activated by an AMF produced quantifiable, controllable hyperthermia in a defined area, as required for clinical applications. In conclusion, AMF-induced hyperthermia is an approach that could potentially deliver SPIONs across the BBB with low toxicity for therapeutic and diagnostic CNS applications.
6. Conclusions
NPs are useful vehicles which can facilitate passage across the BBB. Three strategies can be adopted to enable the use of IONs for this purpose: modification of the IONs with functional ligands that target specific receptors of the brain cells; the use of an external magnetic field to direct the movement of the particles to the brain; and, finally, the application of an RF field to the IONs, which will generate enough thermal energy to transiently and locally open up the BBB. The last two strategies make use of two physical properties: magnetic force and the energy generated by the movement of particles. This third strategy, in particular, opens up a new avenue in the search for a local drug delivery mechanism to treat CNS disorders.
Acknowledgments
J.E. and M.A.B. are grateful to the Spanish Ministerio de Economía y Competitividad (MINECO) for financial support of the project MAT2012-36270-C04-03.
Author Contributions
The manuscript was written through the contributions of all of the authors. All authors have approved the final version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Silva G.A. Nanotechnology approaches to crossing the blood-brian barrier and drug delivery to the CNS. BMC Neurosci. 2008;9 doi: 10.1186/1471-2202-9-S3-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu L., Zhang H., Wu Y. Dendrimer advances for the central nervous system delivery of therapeutics. ACS Chem. Neurosci. 2014;5:2–13. doi: 10.1021/cn400182z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pardridge W.M. The blood-brain barrier: Bottleneck in brain drug development. NeuroRx. 2005;2:3–14. doi: 10.1602/neurorx.2.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abbott N.J., Ronnback L., Hansson E. Astrocyte-endothelial interactions at the blood-brain barrier. Nat. Rev. Neurosci. 2006;7:41–53. doi: 10.1038/nrn1824. [DOI] [PubMed] [Google Scholar]
- 5.Dilnawaz F., Sahoo S.K. Therapeutic approaches of magnetic nanoparticles for the central nervous system. Drug Discov. Today. 2015;20:1256–1263. doi: 10.1016/j.drudis.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Pathirana W., Gunasekera S.M., Constantine G.R., Perera S., Perera B.M., Kamaladiwela R. Brain targeted transcranial administration of diazepam and shortening of sleep latency in healthy human volunteers. Indian J. Pharm. Sci. 2011;73:497–503. doi: 10.4103/0250-474X.98985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blanchette M., Michaud K., Fortin D. A new method of quantitatively assessing the opening of the blood-brain barrier in murine animal models. J. Neurosci. Methods. 2012;207:125–129. doi: 10.1016/j.jneumeth.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Lossinsky A.S., Vorbrodt A.W., Wisniewski H.M. Scanning and transmission electron microscopic studies of microvascular pathology in the osmotically impaired blood-brain barrier. J. Neurocytol. 1995;24:795–806. doi: 10.1007/BF01191215. [DOI] [PubMed] [Google Scholar]
- 9.Kreuter J. Nanoparticulate systems for brain delivery of drugs. Adv. Drug Deliv. Rev. 2001;47:65–81. doi: 10.1016/S0169-409X(00)00122-8. [DOI] [PubMed] [Google Scholar]
- 10.Kreuter J., Alyautdin R.N., Kharkevich D.A., Ivanov A.A. Passage of peptides through the blood-brain barrier with colloidal polymer particles (nanoparticles) Brain Res. 1994;674:171–174. doi: 10.1016/0006-8993(95)00023-J. [DOI] [PubMed] [Google Scholar]
- 11.Alyautdin R., Gothier D., Petrov V., Kharkevich D., Kreuter J. Analgesic activity of the hexapeptide dalargin adsorbed on the surface of polysorbate 80-coated poly(butyl cyanoacrylate) nanoparticles. Eur. J. Pharm. Biopharm. 1995;41:44–48. [Google Scholar]
- 12.Wilson B. Brain targeting PBCA nanoparticles and the blood-brain barrier. Nanomedicine. 2009;4:499–502. doi: 10.2217/nnm.09.29. [DOI] [PubMed] [Google Scholar]
- 13.Kreuter J. Drug delivery to the central nervous system by polymeric nanoparticles: What do we know? Adv. Drug Deliv. Rev. 2014;71:2–14. doi: 10.1016/j.addr.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Hall W.A. Transferrin receptor on glioblastoma multiforme. J. Neurosurg. 1991;74:313–314. doi: 10.3171/jns.1991.74.2.0313a. [DOI] [PubMed] [Google Scholar]
- 15.Eavarone D.A., Yu X., Bellamkonda R.V. Targeted drug delivery to C6 glioma by transferrin-coupled liposomes. J. Biomed. Mater. Res. 2000;51:10–14. doi: 10.1002/(SICI)1097-4636(200007)51:1<10::AID-JBM2>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 16.Huang R.Q., Ke W.L., Qu Y.H., Zhu J.H., Pei Y.Y., Jiang C. Characterization of lactoferrin receptor in brain endothelial capillary cells and mouse brain. J. Biomed. Sci. 2007;14:121–128. doi: 10.1007/s11373-006-9121-7. [DOI] [PubMed] [Google Scholar]
- 17.Hu K., Li J., Shen Y., Lu W., Gao X., Zhang Q., Jiang X. Lactoferrin-conjugated PEG-PLA nanoparticles with improved brain delivery: In vitro and in vivo evaluations. J. Control. Release. 2009;134:55–61. doi: 10.1016/j.jconrel.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 18.Shilo M., Motiei M., Hana P., Popovtzer R. Transport of nanoparticles through the blood-brain barrier for imaging and therapeutic applications. Nanoscale. 2014;6:2146–2152. doi: 10.1039/C3NR04878K. [DOI] [PubMed] [Google Scholar]
- 19.Laurent S., Burtea C., Thirifays C., Hafeli U.O., Mahmoudi M. Crucial ignored parameters on nanotoxicology: The importance of toxicity assay modifications and “cell vision”. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0029997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahmoudi M., Laurent S., Shokrgozar M.A., Hosseinkhani M. Toxicity evaluations of superparamagnetic iron oxide nanoparticles: Cell “vision” versus physicochemical properties of nanoparticles. ACS Nano. 2011;5:7263–7276. doi: 10.1021/nn2021088. [DOI] [PubMed] [Google Scholar]
- 21.Dokladny K., Moseley P.L., Ma T.Y. Physiologically relevant increase in temperature causes an increase in intestinal epithelial tight junction permeability. Am. J. Physiol. Gastrointest. Liver Physiol. 2006;290:G204–G212. doi: 10.1152/ajpgi.00401.2005. [DOI] [PubMed] [Google Scholar]
- 22.Kiyatkin E.A., Sharma H.S. Permeability of the blood-brain barrier depends on brain temperature. Neuroscience. 2009;161:926–939. doi: 10.1016/j.neuroscience.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Estelrich J., Sanchez-Martin M.J., Busquets M.A. Nanoparticles in magnetic resonance imaging: From simple to dual contrast agents. Int. J. Nanomed. 2015;10:1727–1741. doi: 10.2147/IJN.S76501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzales-Weimuller M., Zeisberger M., Krishnan M. Size-dependant heating rates of iron oxide nanoparticles for magnetic fluid hyperthermia. J. Magn. Magn. Mater. 2009;321:1947–1950. doi: 10.1016/j.jmmm.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilhelm C., Gazeau F. Universal cell labelling with anionic magnetic nanoparticles. Biomaterials. 2008;29:3161–3174. doi: 10.1016/j.biomaterials.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 26.Estelrich J., Escribano E., Queralt J., Busquets M.A. Iron oxide nanoparticles for magnetically-guided and magnetically-responsive drug delivery. Int. J. Mol. Sci. 2015;16:8070–8101. doi: 10.3390/ijms16048070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scherer F., Anton M., Schillinger U., Henke J., Bergemann C., Kruger A., Gansbacher B., Plank C. Magnetofection: Enhancing and targeting gene delivery by magnetic force in vitro and in vivo. Gene Ther. 2002;9:102–109. doi: 10.1038/sj.gt.3301624. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro B., Dormer K., Rutel I.B. A Two-Magnet System to Push Therapeutic Nanoparticles. AIP Conf. Proc. 2010;1311:77–88. doi: 10.1063/1.3530064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wui W., Wu Z., Yu T., Jiang C., Kim W.-S. Recent progress on magnetic iron oxide nanoparticles: Synthesis, surface functional strategies and biomedical applications. Sci. Technol. Adv. Mater. 2015;16 doi: 10.1088/1468-6996/16/2/023501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gupta A.K., Gupta M. Synthesis and surface engineering of iron oxide nanoparticles for biomedical applications. Biomaterials. 2005;26:3995–4021. doi: 10.1016/j.biomaterials.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 31.Garcia-Jimeno S., Escribano E., Queralt J., Estelrich J. External magnetic field-induced selective biodistribution of magnetoliposomes in mice. Nanoscale Res. Lett. 2012;7 doi: 10.1186/1556-276X-7-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rousseau V., Denizot B., Pouliquen D., Jallet P., le Jeune J.J. Investigation of blood-brain barrier permeability to magnetite-dextran nanoparticles (MD3) after osmotic disruption in rats. Magma. 1997;5:213–222. doi: 10.1007/BF02594584. [DOI] [PubMed] [Google Scholar]
- 33.Sun Z., Worden M., Wroczynskyj Y., Yathindranath V., van Lierop J., Hegmann T., Miller D.W. Magnetic field enhanced convective diffusion of iron oxide nanoparticles in an osmotically disrupted cell culture model of the blood-brain barrier. Int. J. Nanomed. 2014;9:3013–3026. doi: 10.2147/IJN.S62260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh D., McMillan J.M., Kabanov A.V., Sokolsky-Papkov M., Gendelman H.E. Bench-to-bedside translation of magnetic nanoparticles. Nanomedicine. 2014;9:501–516. doi: 10.2217/nnm.14.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maric G., Annis M.G., Dong Z., Rose A.A., Ng S., Perkins D., MacDonald P.A., Ouellet V., Russo C., Siegel P.M. GPNMB cooperates with neuropilin-1 to promote mammary tumor grwth and engages integrin α5β1 for efficient breast cancer metastasis. Oncogene. 2015;34:5494–5504. doi: 10.1038/onc.2015.8. [DOI] [PubMed] [Google Scholar]
- 36.Szulzewsky F., Pelz A., Feng X., Synowitz M., Markovic D., Langmann T., Holtman I.R., Wang X., Eggen B.J., Boddeke H.W., et al. Glioma associated microglia/macrophages display an expression profile different from M1 and M2 polarisation and highly express Gpnmb and Spp1. PLoS ONE. 2015;10:e0116644. doi: 10.1371/journal.pone.0116644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hadjipanayis C.G., Machaidze R., Kaluzova M., Wang L., Schuette A.J., Chen H., Wu X., Mao H. Egfrviii antibody-conjugated iron oxide nanoparticles for magnetic resonance imaging-guided convection-enhanced delivery and targeted therapy of glioblastoma. Cancer Res. 2010;70:6303–6312. doi: 10.1158/0008-5472.CAN-10-1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mamot C., Drummond D.C., Greiser U., Hong K., Kirpotin D.B., Marks J.D., Park J.W. Epidermal growth factor receptor (EGFR)-targeted immunoliposomes mediate specific and efficient drug delivery to EGFR- and EGFRvIII-overexpressing tumor cells. Cancer Res. 2003;63:3154–3161. [PubMed] [Google Scholar]
- 39.Kim I.Y., Kang Y.S., Lee D.S., Park H.J., Choi E.K., Oh Y.K., Son H.J., Kim J.S. Antitumor activity of EGFR targeted pH-sensitive immunoliposomes encapsulating gemcitabine in A549 xenograft nude mice. J. Control. Release. 2009;140:55–60. doi: 10.1016/j.jconrel.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 40.Shevtsov M.A., Nikolaev B.P., Yakovleva L.Y., Marchenko Y.Y., Dobrodumov A.V., Mikhrina A.L., Martynova M.G., Bystrova O.A., Yakovenko I.V., Ischenko A.M. Superparamagnetic iron oxide nanoparticles conjugated with epidermal growth factor (SPION-EGF) for targeting brain tumors. Int. J. Nanomed. 2014;9:273–287. doi: 10.2147/IJN.S55118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kievit F.M., Veiseh O., Fang C., Bhattarai N., Lee D., Ellenbogen R.G., Zhang M. Chlorotoxin labeled magnetic nanovectors for targeted gene delivery to glioma. ACS Nano. 2010;4:4587–4594. doi: 10.1021/nn1008512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fillebeen C., Descamps L., Dehouck M.P., Fenart L., Benaissa M., Spik G., Cecchelli R., Pierce A. Receptor-mediated transcytosis of lactoferrin through the blood-brain barrier. J. Biol. Chem. 1999;274:7011–7017. doi: 10.1074/jbc.274.11.7011. [DOI] [PubMed] [Google Scholar]
- 43.Qiao R., Jia Q., Huwel S., Xia R., Liu T., Gao F., Galla H.J., Gao M. Receptor-mediated delivery of magnetic nanoparticles across the blood-brain barrier. ACS Nano. 2012;6:3304–3310. doi: 10.1021/nn300240p. [DOI] [PubMed] [Google Scholar]
- 44.Yan F., Wang Y., He S., Ku S., Gu W., Ye L. Transferrin-conjugated, fluorescein-loaded magnetic nanoparticles for targeted delivery across the blood-brain barrier. J. Mater. Sci. Mater. Med. 2013;24:2371–2379. doi: 10.1007/s10856-013-4993-3. [DOI] [PubMed] [Google Scholar]
- 45.Chang J., Jallouli Y., Kroubi M., Yuan X.B., Feng W., Kang C.S., Pu P.Y., Betbeder D. Characterization of endocytosis of transferrin-coated PLGA nanoparticles by the blood-brain barrier. Int. J. Pharm. 2009;379:285–292. doi: 10.1016/j.ijpharm.2009.04.035. [DOI] [PubMed] [Google Scholar]
- 46.Cui Y., Xu Q., Chow P.K., Wang D., Wang C.H. Transferrin-conjugated magnetic silica PLGA nanoparticles loaded with doxorubicin and paclitaxel for brain glioma treatment. Biomaterials. 2013;34:8511–8520. doi: 10.1016/j.biomaterials.2013.07.075. [DOI] [PubMed] [Google Scholar]
- 47.Bechara C., Sagan S. Cell-penetrating peptides: 20 years later, where do we stand? FEBS Lett. 2013;587:1693–1702. doi: 10.1016/j.febslet.2013.04.031. [DOI] [PubMed] [Google Scholar]
- 48.Chen G.-J., Su Y.-Z., Hsu C., Lo Y.-L., Huang S.-J., Ke J.-H., Kuo Y.-C., Wang L.-F. Angiopep-pluronic F127-conjugated superparamagnetic iron oxide nanoparticles as nanotheranostic agents for BBB targeting. J. Mater. Chem. B. 2014;2:5666–5675. doi: 10.1039/C4TB00543K. [DOI] [PubMed] [Google Scholar]
- 49.Gandhi N., Saiyed Z.M., Napuri J., Samikkannu T., Reddy P.V., Agudelo M., Khatavkar P., Saxena S.K., Nair M.P. Interactive role of human immunodeficiency virus type 1 (HIV-1) clade-specific TAT protein and cocaine in blood-brain barrier dysfunction: Implications for HIV-1-associated neurocognitive disorder. J. Neurovirol. 2010;16:294–305. doi: 10.3109/13550284.2010.499891. [DOI] [PubMed] [Google Scholar]
- 50.Wang H., Zhang S., Liao Z., Wang C., Liu Y., Feng S., Jiang X., Chang J. PEGlated magnetic polymeric liposome anchored with TAT for delivery of drugs across the blood-spinal cord barrier. Biomaterials. 2010;31:6589–6596. doi: 10.1016/j.biomaterials.2010.04.057. [DOI] [PubMed] [Google Scholar]
- 51.Ansciaux E., Burtea C., Laurent S., Crombez D., Nonclerc D., Vander Elst L., Muller R.N. In vitro and in vivo characterization of several functionalized ultrasmall particles of iron oxide, vectorized against amyloid plaques and potentially able to cross the blood-brain barrier: Toward earlier diagnosis of alzheimer's disease by molecular imaging. Contrast Media Mol. Imaging. 2015;10:211–224. doi: 10.1002/cmmi.1626. [DOI] [PubMed] [Google Scholar]
- 52.Cheng K.K., Chan P.S., Fan S., Kwan S.M., Yeung K.L., Wang Y.X., Chow A.H., Wu E.X., Baum L. Curcumin-conjugated magnetic nanoparticles for detecting amyloid plaques in Alzheimer’s disease mice using magnetic resonance imaging (MRI) Biomaterials. 2015;44:155–172. doi: 10.1016/j.biomaterials.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 53.Pang S., Koyanagi Y., Miles S., Wiley C., Vinters H.V., Chen I.S. High levels of unintegrated HIV-1 DNA in brain tissue of AIDS dementia patients. Nature. 1990;343:85–89. doi: 10.1038/343085a0. [DOI] [PubMed] [Google Scholar]
- 54.Spencer D.C., Price R.W. Human immunodeficiency virus and the central nervous system. Annu. Rev. Microbiol. 1992;46:655–693. doi: 10.1146/annurev.mi.46.100192.003255. [DOI] [PubMed] [Google Scholar]
- 55.Dou H., Destache C.J., Morehead J.R., Mosley R.L., Boska M.D., Kingsley J., Gorantla S., Poluektova L., Nelson J.A., Chaubal M., et al. Development of a macrophage-based nanoparticle platform for antiretroviral drug delivery. Blood. 2006;108:2827–2835. doi: 10.1182/blood-2006-03-012534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dou H., Grotepas C.B., McMillan J.M., Destache C.J., Chaubal M., Werling J., Kipp J., Rabinow B., Gendelman H.E. Macrophage delivery of nanoformulated antiretroviral drug to the brain in a murine model of neuroaids. J. Immunol. 2009;183:661–669. doi: 10.4049/jimmunol.0900274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jain S., Mishra V., Singh P., Dubey P.K., Saraf D.K., Vyas S.P. RGD-anchored magnetic liposomes for monocytes/neutrophils-mediated brain targeting. Int. J. Pharm. 2003;261:43–55. doi: 10.1016/S0378-5173(03)00269-2. [DOI] [PubMed] [Google Scholar]
- 58.Saiyed Z.M., Gandhi N.H., Nair M.P. Magnetic nanoformulation of azidothymidine 5′-triphosphate for targeted delivery across the blood-brain barrier. Int. J. Nanomed. 2010;5:157–166. doi: 10.2147/ijn.s8905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kong S.D., Lee J., Ramachandran S., Eliceiri B.P., Shubayev V.I., Lal R., Jin S. Magnetic targeting of nanoparticles across the intact blood-brain barrier. J. Control. Release. 2012;164:49–57. doi: 10.1016/j.jconrel.2012.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thomsen L.B., Linemann T., Pondman K.M., Lichota J., Kim K.S., Pieters R.J., Visser G.M., Moos T. Uptake and transport of superparamagnetic iron oxide nanoparticles through human brain capillary endothelial cells. ACS Chem. Neurosci. 2013;4:1352–1360. doi: 10.1021/cn400093z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ding H., Sagar V., Agudelo M., Pilakka-Kanthikeel S., Atluri V.S., Raymond A., Samikkannu T., Nair M.P. Enhanced blood-brain barrier transmigration using a novel transferrin embedded fluorescent magneto-liposome nanoformulation. Nanotechnology. 2014;25:055101. doi: 10.1088/0957-4484/25/5/055101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ranney D.F., Huffaker H.H. Magnetic microspheres for the targeted controlled release of drugs and diagnostic agents. Ann. N. Y. Acad. Sci. 1987;507:104–119. doi: 10.1111/j.1749-6632.1987.tb45795.x. [DOI] [PubMed] [Google Scholar]
- 63.Zhao M., Liang C., Li A., Chang J., Wang H., Yan R., Zhang J., Tai J. Magnetic paclitaxel nanoparticles inhibit glioma growth and improve the survival of rats bearing glioma xenografts. Anticancer Res. 2010;30:2217–2223. [PubMed] [Google Scholar]
- 64.Chertok B., Moffat B.A., David A.E., Yu F., Bergemann C., Ross B.D., Yang V.C. Iron oxide nanoparticles as a drug delivery vehicle for mri monitored magnetic targeting of brain tumors. Biomaterials. 2008;29:487–496. doi: 10.1016/j.biomaterials.2007.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chertok B., David A.E., Yang V.C. Polyethyleneimine-modified iron oxide nanoparticles for brain tumor drug delivery using magnetic targeting and intracarotid administration. Biomaterials. 2010;31:6317–6324. doi: 10.1016/j.biomaterials.2010.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chertok B., David A.E., Yang V.C. Brain tumor targeting of magnetic nanoparticles for potential drug delivery: Effect of administration route and magnetic field topography. J. Control. Release. 2011;155:393–399. doi: 10.1016/j.jconrel.2011.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Driscoll C.F., Morris R.M., Senyei A.E., Widder K.J., Heller G.S. Magnetic targeting of microspheres in blood flow. Microvasc. Res. 1984;27:353–369. doi: 10.1016/0026-2862(84)90065-7. [DOI] [PubMed] [Google Scholar]
- 68.Marie H., Lemaire L., Franconi F., Lajnef S., Frapart I.-M., Nicolas V., Frébourg G., Trichet M., Ménager C., Lessieur S. Superparamagnetic liposomes for MRI monitoring and external magnetic field-induced selective targeting of malignant brain tumors. Adv. Funct. Mater. 2015;25:1258–1269. doi: 10.1002/adfm.201402289. [DOI] [Google Scholar]
- 69.Philosof-Mazor L., Dakwar G.R., Popov M., Kolusheva S., Shames A., Linder C., Greenberg S., Heldman E., Stepensky D., Jelinek R. Bolaamphiphilic vesicles encapsulating iron oxide nanoparticles: New vehicles for magnetically targeted drug delivery. Int. J. Pharm. 2013;450:241–249. doi: 10.1016/j.ijpharm.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 70.Tabatabaei S.N., Duchemin S., Girouard H., Martel S. Towards MR-navigable nanorobotic carriers for drug delivery into the brain; Proceedings of the 2012 IEEE International Conference on Robotics and Automation (ICRA); Saint Paul, MN, USA. 14–18 May 2012; pp. 727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tabatabaei S.N., Girouard H., Carret A.S., Martel S. Remote control of the permeability of the blood-brain barrier by magnetic heating of nanoparticles: A proof of concept for brain drug delivery. J. Control. Release. 2015;206:49–57. doi: 10.1016/j.jconrel.2015.02.027. [DOI] [PubMed] [Google Scholar]
- 72.Dan M., Bae Y., Pittman T.A., Yokel R.A. Alternating magnetic field-induced hyperthermia increases iron oxide nanoparticle cell association/uptake and flux in blood-brain barrier models. Pharm. Res. 2015;32:1615–1625. doi: 10.1007/s11095-014-1561-6. [DOI] [PMC free article] [PubMed] [Google Scholar]