Abstract
Aim
We aimed at estimating excess medical expenditures associated with major depressive disorder (MDD) among working-age adults diagnosed with diabetes, disaggregated by treatment mode: insulin-treated diabetes (ITDM) or non-insulin-treated diabetes (NITDM).
Methods
We analyzed data for over 500,000 individuals with diagnosed diabetes from the 2008 U.S. MarketScan claims database. We grouped diabetic patients first by treatment mode (ITDM or NITDM), then by MDD status (with or without MDD), and finally by whether those with MDD used antidepressant medication. We estimated annual mean excess outpatient, inpatient, prescription drug, and total expenditures using regression models, controlling for demographics, types of health coverage, and comorbidities.
Results
Among persons having ITDM, the estimated annual total mean expenditure for those with no MDD (the comparison group) was $19,625. For those with MDD, the expenditures were $12,406 (63%) larger if using antidepressant medication and $7322 (37%) larger if not using antidepressant medication. Among persons having NITDM, the corresponding estimated expenditure for the comparison group was $10,746, the excess expenditures were $10,432 (97%) larger if using antidepressant medication and $5579 (52%) larger if not using antidepressant medication, respectively. Inpatient excess expenditures were the largest of total excess expenditure for those with ITDM and MDD treated with antidepressant medication; for all others with diabetes and MDD, outpatient expenditures were the largest excess expenditure.
Conclusions
Among working-age adults with diabetes, MDD was associated with substantial excess medical expenditures. Implementing the effective interventions demonstrated in clinical trials and treatment guidelines recommended by professional organizations might reduce the economic burden of MDD in this population.
Keywords: Insulin, Depression, Insulin-treated diabetes, Medical costs, Antidepressant medication
1. Introduction
Major depressive disorder (MDD) among persons with diabetes is a large public health problem [1,2]. In 2006, an estimated 8.3% (age-adjusted) of U.S. adults (aged ≥18 years) with diagnosed diabetes had MDD [2]. The American Diabetes Association (ADA) recommends screening for depression among persons with diabetes and incorporating depression assessment and treatments into routine care as part of diabetes management [3].
Persons with diabetes and MDD use more health care services [4–8] and incur larger medical costs [8–10] than those without MDD. However, the medical cost of MDD among person with diabetes, which is critical to assessing the financial burden and economic benefit of interventions aimed at preventing and controlling MDD, is not fully understood. Previous studies on assessing the excess economic burdens of MDD were either restricted to persons aged 65+ [9] or had small sample sizes [10] or were simply descriptive in nature [8]. Furthermore, none of these studies examined whether costs associated with MDD and diabetes differed if stratified by diabetes treatment mode: insulin-treated diabetes (ITDM) vs. non-insulin-treated diabetes (NITDM). Previous studies also did not examine how those costs would differ if differentiated by whether or not persons with MDD were treated with antidepressant medication.
The excess medical expenditures of MDD among persons with diabetes are likely to differ by both diabetes treatment mode and antidepressant medication use. Diabetes management among persons with ITDM may be more complicated than among persons with NITDM. These persons need to closely monitor blood glucose and manage insulin use on a daily basis and are, perhaps, more vulnerable to diabetes-related depression [11–14], and have worsening depressive symptoms (among those with MDD) [15]. Because of the severity of depression, persons with ITDM may be vulnerable to self-monitoring their blood glucose less frequently than they should [16] and to subsequent diabetes complications [11,15]. Thus, excess costs are very likely to be influenced by the interaction between depression and diabetes treatment mode [17]. In terms of antidepressant medication use, those who were on medication might have more severe depression symptoms, thus they might incur larger costs than those who were not on antidepressant medication.
Our study’s objective was to estimate the excess medical expenditures associated with MDD, with or without antidepressant medication use, among working-age adults (aged 18–64 years) with diagnosed diabetes, differentiated by diabetes treatment mode: ITDM or NITDM.
2. Methods
2.1. Data source
We analyzed data from a large sample of persons with diabetes from across the United States using the 2008 MarketScan Commercial Claims and Encounters (CCE) Database (MarketScan Database, Thompson Medstat. Ann Arbor, MI). This database contains fully adjudicated and paid claims for over 30 million enrollees with employer-sponsored health plans, including claims for employees and their spouses and dependents. The CCE database includes patient-level data on inpatient, outpatient, and prescription drug claims from non-personally identifiable information that can be linked using encrypted enrollee information [18]. These claims include the amount paid by third-party payers and for the out-of-pocket expenses of patients.
There are two major types of health plans through which enrollees obtain services: fee-for-service (FFS) plans and capitated plans (some fully, some partially). FFS plans include preferred provider organization (PPO) plans, exclusive provider organization plans, point-of-service (POS) plans without capitation, consumer-directed health plans, and indemnity plans. Fully or partially capitated plans include health maintenance organization plans and POS plans with capitation [19]. This database has been used extensively in studies of medical expenditures of many medical conditions [8,20–22].
We restricted our sample to those who had employer-sponsored health coverage, were enrolled in an FFS plan between January 1 and December 31, 2008, and had prescription drug coverage. Persons enrolled in capitated plans were not included because their insurance claims often reflect only encounters instead of actual claims [19].
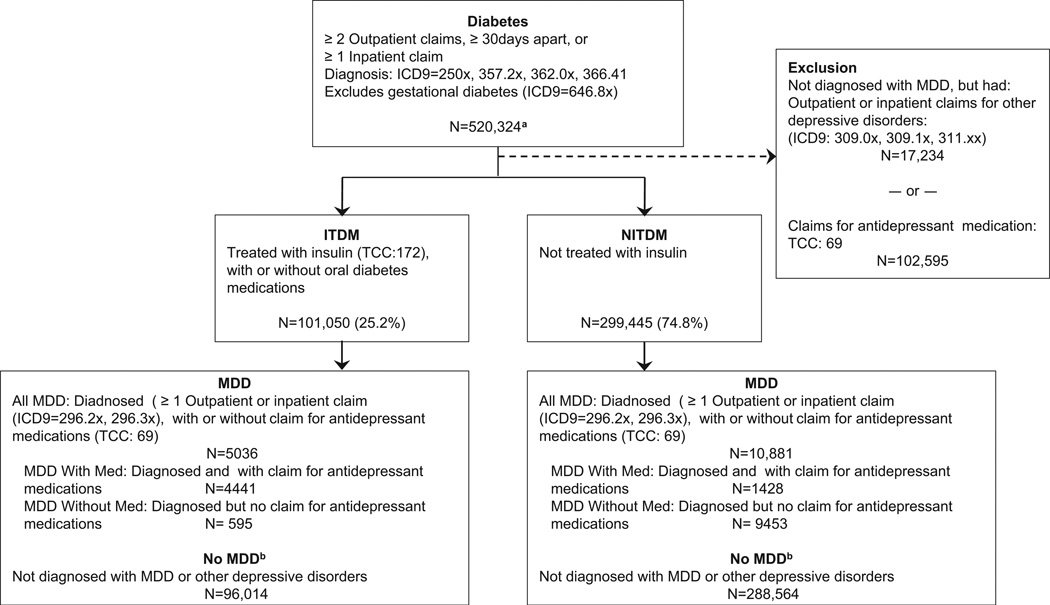
2.2. Identifying persons with diagnosed diabetes
The study sample consisted of working-age adults with diagnosed diabetes, excluding women diagnosed with gestational diabetes (International Statistical Classification of Diseases and Related Health Problems, Ninth Edition [ICD-9] code: 648.8x), based on inpatient or outpatient claims. The study included persons with diabetes who had at least two outpatient encounters, a minimum of 30 days apart, in which diabetes was a primary or secondary diagnosis (ICD-9 codes: 250x, 357.2x, 362.0x, 366.41), or at least one inpatient admission with diabetes as a primary or secondary diagnosis (n = 520,324) (Fig. 1) [23]. We required at least two outpatient encounters to exclude those who may have been misdiagnosed as having diabetes at the first encounter.
Fig. 1.
Criteria used to identify persons with diabetes, diabetes treatment type, major depressive disorder (MDD). ITDM, insulin-treated diabetes mellitus; NITDM, non-insulin-treated diabetes mellitus. aAfter accounting for those excluded the total number persons with diagnosed diabetes in the analytical sample is 400,495. b“No MDD” is reference (comparison) group.
Because our study focused on assessing the financial burden on persons with diagnosed diabetes and comorbid MDD (defined below), our comparison groups were composed of persons diagnosed with diabetes but not with MDD. We excluded from our comparison group: (1) those who had depressive disorders other than MDD (ICD-9: 309.0x, 309.1x, 311.xx) in their outpatient or inpatient claims; and (2) those who had no diagnosis codes for MDD in their outpatient or inpatient claims but had claims for antidepressant medications (Fig. 1). With these exclusions, our analytical sample consisted of 400,495 persons diagnosed with diabetes.
Persons with ITDM (n = 101,050) were identified as those having diabetes and were prescribed insulin; this diagnosis is identified by the Therapeutic Class Code (TCC) 172 from prescription claim data. Persons with NITDM (n = 299,445) were identified as those having diabetes but not taking insulin (Fig. 1).
2.3. Identifying persons with MDD
Under each of the diabetes treatment modes, we identified persons with MDD as either the primary or a secondary diagnosis in their inpatient or outpatient claims by the ICD-9 codes 296.2x or 296.3x [9]. We further grouped those diagnosed with MDD as either: (1) those treated with antidepressant medication (MDD with Med), identified by the TCC 69 in their prescription claims (n = 13,894; ITDM: 4441; NITDM: 9453), or (2) those not treated with antidepressant medication (MDD without Med: n = 2023; ITDM: 595; NITDM: 1428) (Fig. 1).
2.4. Statistical analysis
The outcome variables of interest included the annual per-person medical expenditures from outpatient claims, inpatient claims (including inpatient medications), or prescription drugs, as well as total medical expenditures, including patients’ out-of-pocket expenses. We estimated the excess annual per-person medical expenditures in total and by component for two subpopulations: those with ITDM and those with NITDM. For each of the four outcomes, we fit a model to estimate the excess medical expenditures associated with MDD separately: for those treated with antidepressant medication and for those with not treated with antidepressant medication. The exposure variables included three categories: (1) having MDD and treated with antidepressant medications; (2) having MDD and not treated with antidepressant medications; and (3) not having MDD (the comparison group). Covariates in the models included demographic variables (age and sex); geographical variables (census region: Midwest, South, West, or Northeast), and area of residence (inside or outside of a metropolitan statistical area); type of health benefit plan (PPO or not a PPO); comorbidities; and interaction terms between MDD and covariates.
We controlled for the 15 major comorbidities as defined in Deyo et al.’s paper [24], including myocardial infarction, congestive heart failure, peripheral vascular disease, cerebro-vascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, mild liver disease, hemiplegia, renal disease, any malignancy (including leukemia and lymphoma), moderate or severe liver disease, metastatic tumor, and AIDS. We included each condition as a separate variable instead of combining them into a comorbidity index because the effects of comorbidities can vary and our large sample made this possible. We also tested for the interactions of MDD with age, sex, and each of the comorbidities. Only those interaction terms for which p < 0.05 were retained.
We used a two-part model to estimate inpatient expenditures because a large proportion of individuals had no inpatient admissions and, for those with admissions, expenditures were positively skewed [25]. In the first part of the two-part model, we used logistic regression to estimate the probability that a person with diabetes would have inpatient expenditures, and in the second part, we used a generalized linear model with log link and gamma distribution to estimate the inpatient expenditures for those who had such expenditures. Only the second part of the two-part model was needed to estimate medical expenditures on outpatient care and prescription drugs, because all patients in our sample had outpatient or prescription medical expenses [26]. For the total expenditures and for each component of expenditure, we estimated annual medical expenditures for persons with both diabetes and MDD (with or without antidepressant medication use) and for those with diabetes alone. We did this for each individual by multiplying the parameter expenditure estimates from these two models, keeping the value of all other variables as is and setting the MDD indicator variable to ‘1’ or ‘0’ separately. The mean differences among the counterfactual options resulted in the estimated mean excess medical expenditure associated with MDD.
We used 1000 nonparametric bootstrap replications to calculate the standard errors of estimated excess expenditures. All expenses are in 2008 U.S. dollars. All statistical analyses were conducted using Stata v. 11.
3. Results
3.1. Characteristics of the study sample
Among persons with diabetes in our sample, 25% were treated with insulin (Fig. 1). Descriptive statistics for the variables used in the models, designated by diabetes treatment mode and MDD status, appear in Table 1. Regardless of diabetes treatment mode, those with MDD were more likely to be female, reside in metropolitan statistical areas, or reside in the Midwest, but were less likely to reside in the South census region than those without MDD. Those with ITDM and MDD treated with antidepressant medication were slightly older and those with NITDM and MDD or those with ITDM not treated with antidepressant medication were slightly younger than their counterparts who did not have MDD. Among all persons with diabetes, the proportion of persons diagnosed with comorbidities was significantly larger for those with MDD treated with antidepressant medication than for those without MDD.
Table 1.
Characteristics of adults aged 18–64 years with diabetes differentiated by diabetes treatment mode and major depressive disorder (MDD) status.
| Variables | ITDM (n = 101,050) | NITDM (n = 299,445) | ||||
|---|---|---|---|---|---|---|
| MDD w/Med |
MDD w/out Med |
No MDD |
MDD w/Med |
MDD w/out Med |
No MDD |
|
| Age, years (mean) | 50.8**, δδ | 48.3**,δδ | 49.9 | 52.2** | 51.3** | 53.1 |
| Gender (female = 1), % | 62.9**,δδ | 57.0**,δδ | 41.8 | 65.0** | 55.5** | 41.0 |
| Census region, % | ||||||
| Northeast | 9.8 | 10.1 | 9.2 | 9.5 | 10.9 | 9.4 |
| Midwest | 38.0** | 39.0** | 32.4 | 35.6** | 34.5** | 30.7 |
| South | 39.9**,δ | 35.8**,δ | 46.2 | 41.5** | 38.1** | 47.9 |
| West | 12.3δ | 15.1*,δ | 12.1 | 13.4**,δδ | 16.6**,δδ | 12.0 |
| Residence (% metro) | 83.8**,δ | 85.5**,δ | 81.1 | 85.3** | 86.5** | 80.3 |
| Health plan (% non-PPO) | 26.9**,δ | 31.4**,δ | 25.1 | 25.5δ | 28.3**,δ | 24.4 |
| a Comorbidity, % | ||||||
| Myocardial infarction | 3.8** | 3.0 | 2.2 | 2.1** | 1.7 | 1.4 |
| Congestive heart failure | 8.7** | 7.4** | 4.8 | 3.6** | 3.4** | 2.1 |
| Peripheral vascular disease | 5.3** | 5.0* | 3.5 | 2.6** | 3.3** | 2.1 |
| Cerebrovascular disease | 11.2**,δδ | 7.4**,δδ | 4.8 | 7.0** | 6.5** | 3.5 |
| Dementia | 0.9** | 0.2 | 0.1 | 0.5** | 0.6** | 0.1 |
| Chronic pulmonary disease | 19.2**,δ | 15.0**,δ | 8.6 | 17.7** | 16.7** | 7.8 |
| Rheumatic disease | 3.0**,δ | 1.2δ | 1.3 | 3.0**,δ | 2.1**,δ | 1.2 |
| Peptic ulcer disease | 1.5** | 1.3** | 0.5 | 1.3** | 1.2** | 0.5 |
| Mild liver disease | 1.9** | 2.4** | 0.9 | 0.9** | 0.8* | 0.5 |
| Hemiplegia | 1.1** | 0.8* | 0.3 | 0.6** | 0.6** | 0.2 |
| Renal disease | 9.4** | 10.8** | 7.6 | 3.7** | 4.1** | 2.6 |
| Any malignancy | 5.8** | 6.2 | 4.7 | 6.4** | 6.0 | 4.9 |
| Moderate/severe liver disease | 1.1** | 1.0* | 0.4 | 0.3* | 0.4* | 0.2 |
| Metastatic tumor | 1.0* | 1.0 | 0.7 | 0.7** | 0.8 | 0.5 |
| AIDS | 0.5** | 0.2 | 0.2 | 0.3**,δ | 0.6**,δ | 0.1 |
% Metro: percentage living in Metropolitan Statistical Area, based on employee zip code (reference = not in metro area); % Non-PPO: percentage not having health care coverage through a PPO (Preferred Provider Organization); MDD w/Med: persons with MDD treated with antidepressant medication; MDD w/out Med: persons with MDD not treated with antidepressant medication; No MDD: persons w/out MDD (comparison group).
p < 0.05: Statistical difference (one-tailed) in mean expenditures between MDD w/Med and No MDD, or between MDD w/out Med and No MDD.
p < 0.01: Statistical difference (one-tailed) in mean expenditures between MDD w/Med and No MDD, or between MDD w/out Med and No MDD.
p < 0.05: statistical difference (one-tailed) in mean expenditures between MDD w/Med and MDD w/out Med.
p < 0.01: statistical difference (one-tailed) in mean expenditures between MDD w/Med and MDD w/out Med.
Comorbidities were as defined in Deyo et al. [24].
Among persons having ITDM, those with MDD and on antidepressant medication were more likely to be older, female, reside in the South, and to have cerebrovascular, chronic pulmonary, and rheumatic diseases, but less likely to reside in the West, reside in metropolitan statistical areas, or be enrolled in non-PPO health plans than were those with MDD but not on antidepressant medication. Among persons having NITDM, those with MDD and on medication were less likely to reside in the West, be enrolled in non-PPO health plans, or have diagnosed AIDS, but were more like to have rheumatic disease than those with MDD but not on antidepressant medication.
3.2. Unadjusted medical expenditures
Table 2 presents the unadjusted mean annual medical expenditures by MDD status and antidepressant medication use for persons diagnosed with diabetes, by treatment mode. Among persons having ITDM, the total expenditure and each of its three components were all significantly larger if a person had MDD, regardless of antidepressant medication use, compared with a person without MDD. All expenditures, except inpatient expenditures, were also significantly larger for those who used antidepressant medication compared with those who did not use it. However, of the three expenditure components, expenditures on inpatient care were highest for persons who had MDD and treated with antidepressant medication, but expenditures on outpatient care were highest if not treated with antidepressant medication.
Table 2.
Per capita unadjusted mean medical expenditures among adults aged 18–64 years, differentiated by diabetes treatment mode and major depressive disorder (MDD) status.
| Diabetes treatment mode | MDD Status | n | Expenditures (2008 $) | |||
|---|---|---|---|---|---|---|
| Outpatient | Inpatient | Prescription drugs | Total | |||
| ITDM (n = 101,050) | MDD w/Med | 4441 | 14,512 | 15,384 | 9122 | 39,018 |
| MDD w/out Med | 595 | 13,431 | 11,162 | 5683 | 30,276 | |
| No MDD | 96,014 | 7986 | 5338 | 5069 | 18,393 | |
| NITDM (n = 299,445) | MDD w/Med | 9453 | 10,877 | 7556 | 6313 | 24,747 |
| MDD w/out Med | 1428 | 9229 | 6407 | 3321 | 18,957 | |
| No MDD | 288,564 | 5003 | 2625 | 2656 | 10,284 | |
ITDM, insulin-treated diabetes mellitus; NITDM, non-insulin-treated diabetes mellitus.
MDD w/Med: persons with MDD treated with antidepressant medication; MDD w/out Med: persons with MDD not treated with antidepressant medication.
Difference in mean expenditures between MDD w/Med and no MDD, between MDD w/out Med and no MDD were all statistically different (p < 0.01, one tailed).
Difference in mean expenditures for outpatient, prescription drugs and total expenditures between MDD w/Med and MDD w/out Med (except for inpatient expenses; not significant at 5%) were statistically different (p < 0.01).
Difference in mean expenditures between ITDM and NITDM means were statistically different for all corresponding categories (p < 0.01).
Among NITDM patients, the total expenditure and each of its three components for those with MDD were significantly larger than that for those without MDD, independent of antidepressant medication use. These expenditures for those with MDD who used antidepressant medication were significantly larger than those for persons with MDD who did not. Of the three expenditure components, expenditure on outpatient care was the largest component, regardless of antidepressant medication use.
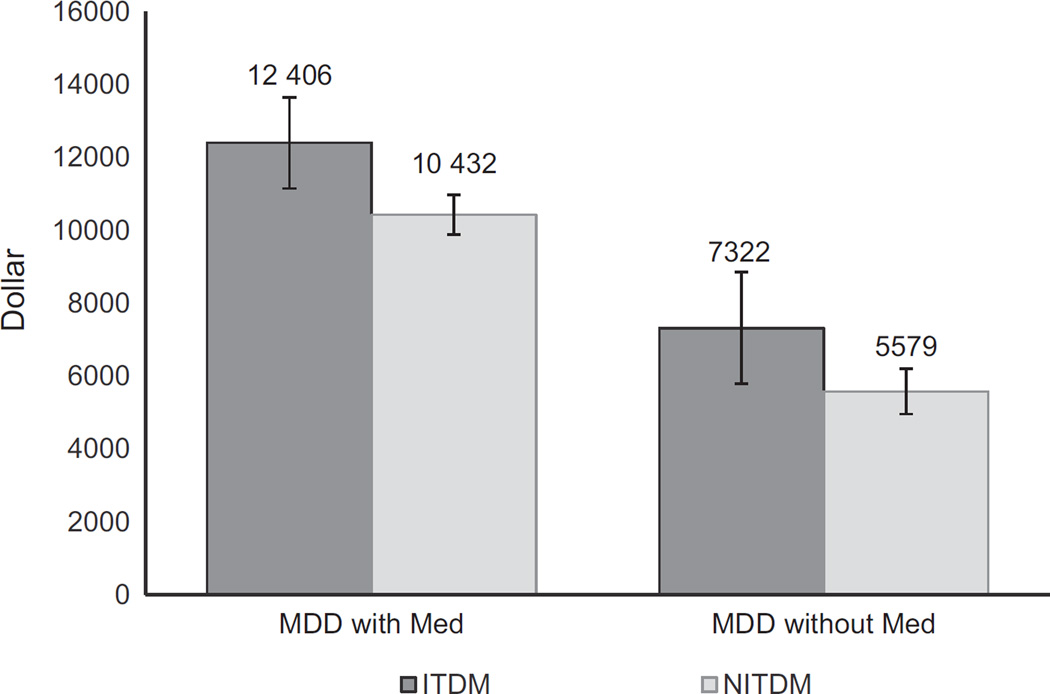
3.3. Estimated excess total medical expenditures
Among persons having ITDM, the estimated mean annual total medical expenditure was $12,406 ($32,031 vs. $19,625; p < 0.01) or 63% larger if the person was diagnosed with MDD and used antidepressant medication compared with person not diagnosed with MDD. This estimated expenditure was $7322 ($26,947 vs. $19,625, p < 0.01) or 37% larger if person was diagnosed with MDD, but did not use antidepressant medication (Fig. 2). Among persons having NITDM and MDD, the estimated mean annual total excess medical expenditure was $10,432 ($21,178 vs. $10,746; p < 0.01) or 97% larger if their MDD was treated with antidepressant medication, but was $5579 ($16,325 vs. $10,746; p < 0.01) or 52% larger if not prescribed antidepressant medication (Fig. 2).
Fig. 2.
Estimated mean excess annual total medical expenditure associated with major depressive disorder (MDD), differentiated by antidepressant medication use for persons with ITDM and NITDM, 2008. ITDM, insulin-treated diabetes mellitus; NITDM, non-insulin-treated diabetes mellitus; MDD w/Med, persons with MDD treated with antidepressant medication; MDD w/out Med, persons with MDD not treated with antidepressant medication. Error bars show the bootstrap standard errors with 1000 replications.
The excess mean annual total medical expenditures for MDD among diabetes patients differed by both diabetes treatment mode and antidepressant medication use. For example, the average excess medical expenditure for a person having ITDM and MDD treated with antidepressant medication was $5084 or 69% larger than for a person with ITDM and MDD not on antidepressant medication. The corresponding excess expenditure was $4853 or 87% larger for a person having NITDM and MDD treated with antidepressant medication than for a person with NITDM and MDD not on antidepressant medication.
3.4. Components of estimated excess total medical expenditures
The estimated and excess annual medical expenditures on outpatient care, inpatient care, and prescription drug use appear in Table 3. Among persons having ITDM, of the total excess medical expenditure for those who were diagnosed with MDD and treated with antidepressant medication, excess expenses for inpatient health care accounted for the largest proportion ($5456; 44%) followed by prescription drugs ($3628; 29%) and outpatient health care ($3321; 27%). But, among those who did not use antidepressant medication, excess expenses for outpatient care accounted for the largest proportion of excess total medical expenditures ($3908; 53%), followed by inpatient care ($2945; 40%), and prescription drugs ($469; 7%).
Table 3.
Mean and excess annual estimated medical expenditures (2008 $) for persons with diagnosed major depressive disorder (MDD), with or without antidepressant medication among adults (18–64 years) with diabetes, by treatment mode, 2008.
| Expenditures/ MDD status |
ITDM (n = 101,050) | NITDM (n = 299,445) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SEa | Excess mean | SEa | Ratiob | Mean | SEa | Excess mean | SEa | Ratiob | |
| Outpatient care | ||||||||||
| MDD w/Med | 12,240 | 189 | 3321 | 191 | 1.37 | 9185 | 116 | 3805 | 117 | 1.71 |
| MDD w/out Med | 12,828 | 482 | 3908 | 481 | 1.44 | 8169 | 200 | 2789 | 199 | 1.52 |
| No MDD | 8919 | 33 | – | – | 1.00 | 5380 | 20 | – | – | 1.00 |
| Inpatient care | ||||||||||
| MDD w/Med | 11,067 | 1414 | 5456 | 1345 | 1.97 | 6036 | 595 | 3340 | 574 | 2.24 |
| MDD w/out Med | 8556 | 1405 | 2945 | 2395 | 1.52 | 4810 | 1187 | 2114 | 1183 | 1.78 |
| No MDD | 5611 | 206 | – | – | 1.00 | 2696 | 80 | – | – | 1.00 |
| Prescription drugs | ||||||||||
| MDD w/Med | 8723 | 110 | 3628 | 111 | 1.71 | 5957 | 65 | 3287 | 66 | 2.23 |
| MDD w/out Med | 5563 | 183 | 469 | 183 | 1.09 | 3346 | 123 | 676 | 123 | 1.25 |
| No MDD | 5094 | 15 | – | – | 1.00 | 2670 | 6 | – | – | 1.00 |
ITDM, insulin-treated diabetes mellitus; NITDM, non-insulin-treated diabetes mellitus.
MDD: major depressive disorder; MDD w/Med: persons with MDD treated with antidepressant medication; MDD w/out Med: persons with MDD not treated with antidepressant medication; No MDD: persons without MDD (comparison group).
SE: standard errors (nonparametric bootstrap using 1,000 replications).
Ratio: component specific relative expenditures: ratio of estimated expenditures for the MDD group relative to No MDD group.
Among persons having NITDM and diagnosed with MDD and treated with antidepressant medication, unlike among those having ITDM, of the excess total medical expenditure, excess expenditures on outpatient care accounted for the largest proportion ($3805; 36%), followed by inpatient care ($3340; 32%), and prescription drugs ($3287; 32%). The similar pattern of component-wise estimated excess expenditures was observed among those with NITDM diagnosed with MDD not treated with antidepressant medication, (outpatient care ($2789; 50%), inpatient care ($2114; 38%), and prescription drug ($676; 12%). These excess expenditures were similar in proportion to that observed among those with ITDM and MDD not treated with antidepressant medication.
4. Discussion
Using a large administrative claims database with data from all regions of the United States, our study provides the most updated estimate for excess medical expenditures associated with MDD, among working-age adults with diagnosed diabetes. We also improved on previous estimates of excess medical expenditures associated with MDD among persons with diabetes by controlling for multiple covariates and comorbidities. In addition, we showed that excess medical expenditures associated with MDD differed by diabetes treatment mode: ITDM or NITDM and antidepressant medication use.
Our study results were consistent with previous studies in terms of showing that MDD was associated with substantial excess medical expenditures among persons with diabetes [8– 10]. Our estimated excess expenditures associated with MDD, with or without antidepressant medication use, both for persons having ITDM and NITDM were, however, larger in absolute amount than those obtained by Simon et al. [10]. Their estimate of annual medical expenditures for persons with diabetes and MDD was $4482 larger than for persons with diabetes not having MDD. A number of factors may have contributed to the difference between Simon et al.’s and our estimates. While Simon et al. used data from a group-managed care organization, which estimated medical costs based on a budget-based cost accounting approach, we used claims data from persons with FFS health plans. Medical expenditures for persons with FFS insurance tend to be larger than those with managed care health plans [27]. However, the estimated excess medical expenditure as measured in percentage term (70%) from the Simon et al. study were within the range of our estimates for those with MDD, whether or not treated with antidepressant medication, among those with ITDM or NITDM (37% to 97% larger).
Le et al. [8] reported an estimated of $8470 for the total excess expenditure associated with MDD among persons with diabetes, which was lower than our estimated excess costs for persons with MDD with medication, but higher than our estimated excess expenditure for persons with MDD but not on medication. The difference in estimated excess expenditures between Le et al. and our study could be, in part, due to differences in the sample characteristics in terms of types of health plans enrollees had. Data from Le et al. came from persons aged ≥ 18 years enrolled in both employer-sponsored private insurance plans and in Medicare supplemental plans. The study sample from Le at al. also included persons enrolled in capitated plans, which tend to have lower reimbursement rates than FFS plans and often have incomplete reporting of claims [19,27].
In contrast, Finkelstein et al., using 1997 Medicare claims data, estimated the excess medical cost for MDD among persons with diabetes, aged ≥65 years, in the United States as $15,002 (2.4 times larger than among persons with diabetes without MDD) [9]. Apart from different study populations, the Finkelstein et al. study did not control for comorbid conditions, which could have impacted the estimated excess costs associated with MDD, particularly in the case of comorbidities associated with diabetes. In our study, average excess total medical expenditures would be 62–66% larger among persons with ITDM and MDD, and 39–55% larger among persons with NITDM and MDD, if we did not control for comorbidities and other covariates (Tables 2 and 3).
Inpatient care, outpatient care, and medication expenditures all contributed to the excess total medical expenditures from MDD, with or without antidepressant medication use. In general, a person with MDD would have a higher medical expenditure because of additional spending from two sources: care associated with treating MDD itself and induced care associated with treating non-MDD related commodities. Le et al. [8] reported that, among persons with diabetes, those with MDD had nearly twice as many annualized mean total outpatient visits as those without (37.6 vs. 19.9 visits/year). The outpatient care uses were even larger for diabetes-related and other causes. Simon et al. and Vamos et al. showed that persons with diabetes and MDD, compared with those without MDD, had larger diabetes related and other causes related outpatient and inpatient costs because the formers were more likely to be hospitalized and had a longer length of hospital stay [7,10].
We also found that, except for outpatient care for persons with ITDM, excess medical expenditures associated with MDD among those on antidepressant medication were higher than that not on antidepressant medication for all cost components. The higher medication expenditures for those who were on antidepressant medication could be due to a higher expenditure on both antidepressant and non-antidepressant medications [8]. The larger excess inpatient expenditures for those who were on antidepressant medication could be due to greater level of severity of depression, which could lead to a more frequent inpatient visit and a longer hospital stay when admitted. This warrants a future research examining the reasons for it using a longitudinal data.
The higher estimated outpatient costs among those with ITDM who were not on antidepressant medication compared to those using medication among person with MDD (Table 3) was unexpected. One plausible explanation for this could be that, for some patients with a well-control MDD, medication could reduce the need for outpatient visits. In addition, ITDM patients with MDD who are treated antidepressant medication have more severe symptoms [8] and have more comorbidities than those who are not on antidepressant medication. Additional outpatient visits associated with treating non-MDD related comorbidities could decrease the need for outpatient visits associated with treating MDD. A future research is needed to verify these hypotheses.
The larger excess medical expenditures for persons with ITDM and MDD, compared to those for persons with NITDM and MDD, were mainly attributable to excess inpatient expenditures. Persons with ITDM are more vulnerable to depression and their depression is more severe than persons with NITDM [15]. This interaction of insulin treatment and depression could result in persons on insulin treatment being more likely to be hospitalized and to stay in the hospital longer for the depression treatment [11–13,15]. Future research is needed to examine how insulin treatment impacts depression treatment in this population. The large difference in excess medical expenditures associated MDD between persons with ITDM and NITDM implies future studies in assessing excess economic or health burdens of depression among persons with diabetes should differentiate patients by diabetes treatment mode.
We found that cost consequences of co-occurrence of MDD among persons with diabetes were substantial. Persons with diabetes are more likely to be depressed and find it harder to manage their diabetes and diabetes-related complications after they develop depression. The ADA recommends depression assessment and treatments into routine diabetes care [3]. Randomized clinical trials have demonstrated that the integrated management of type 2 diabetes and depression could improve both medication adherence and symptoms of diabetes and depression [28], and screening and enhanced treatment regimens for depression could lead to not only better health outcomes but also cost savings compared to “usual care” [29–31]. Implementing ADA recommendations and effective interventions demonstrated in the clinical trials could reduce the excess financial burden of MDD among persons with diabetes.
Our study had several limitations. First, the claims data we used were based on persons with diagnosed diabetes who had employer-sponsored health insurance with FFS health plans. Therefore, our results may not be generalizable to persons who are uninsured or who have undiagnosed diabetes. Second, we identified MDD through claims directly attributed to MDD-related services, which means that those with undiagnosed MDD were not included; 3% of adults with diabetes were estimated to have undiagnosed MDD [32]. Persons with undiagnosed MDD may have less severe symptoms than those diagnosed with MDD but larger expenditures than those without depression. Third, we excluded patients who had claims for antidepressant medications but were not diagnosed with MDD. They might have been receiving treatment for MDD, but had not been formally diagnosed [8]. Fourth, the sensitivity and specificity of the use of ICD-9 codes to identify persons with MDD are unknown. Fifth, our study focused on excess direct medical expenditures due to MDD, so indirect costs (e.g., premature mortality, productivity loss, disability, and nonmedical costs) were not considered. Sixth, because of the cross sectional data, the long-run impacts on expenditure of antidepressant medication use were not assessed. Finally, covariates such as race/ethnicity, income, and length of time since diagnoses of diabetes might have been important, but information on these variables was not available in the MarketScan database.
5. Conclusions
Our findings show that MDD is associated with substantial excess medical expenditures among adults with diagnosed diabetes. This excess expenditure is much larger for persons with ITDM than those with NITDM. Similarly, among those with MDD, the excess expenditures are much larger for persons on antidepressant medication than for those who are not on antidepressant medication. Implementing recommended treatment practice by professional organizations and the effective interventions demonstrated in the clinical trials might reduce the economic burden of MDD in this population.
Acknowledgments
The authors would like to thank Tony Pearson-Clarke at the U.S. Centers for Disease Control and Prevention for his editorial help.
Financial disclosure
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Footnotes
Contributors
SS contributed to study concept, design, data analysis and interpretation, and to drafting of the manuscript; PZ contributed to the study concept, design and data interpretation; and RL TT, DC, and LB contributed to data interpretation.
Conflict of interest
The authors report no conflicts of interest.
references
- 1.Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010;87(3):302–312. doi: 10.1016/j.diabres.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 2.Li C, Ford ES, Strine TW, Mokdad AH. Prevalence of depression among U.S. adults with diabetes: findings from the 2006 behavioral risk factor surveillance system. Diabetes Care. 2008;31(1):105–107. doi: 10.2337/dc07-1154. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care. 2012;35(Suppl 1):S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Das-Munshi J, Stewart R, Ismail K, Bebbington PE, Jenkins R, Prince MJ. Diabetes, common mental disorders, and disability: findings from the UK National Psychiatric Morbidity Survey. Psychosom Med. 2007;69(6):543–550. doi: 10.1097/PSY.0b013e3180cc3062. [DOI] [PubMed] [Google Scholar]
- 5.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25(3):464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 6.Subramaniam M, Sum CF, Pek E, Stahl D, Verma S, Liow PH, et al. Comorbid depression and increased health care utilisation in individuals with diabetes. Gen Hosp Psychiatry. 2009;31(3):220–224. doi: 10.1016/j.genhosppsych.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Vamos EP, Mucsi I, Keszei A, Kopp MS, Novak M. Comorbid depression is associated with increased healthcare utilization and lost productivity in persons with diabetes: a large nationally representative Hungarian population survey. Psychosom Med. 2009;71(5):501–507. doi: 10.1097/PSY.0b013e3181a5a7ad. [DOI] [PubMed] [Google Scholar]
- 8.Le TK, Curtis B, Kahle-Wrobleski K, Johnston J, Haldane D, Melfi C. Treatment patterns and resource use among patients with comorbid diabetes mellitus and major depressive disorder. J Med Econ. 2011;14(4):440–447. doi: 10.3111/13696998.2011.588507. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein EA, Bray JW, Chen H, Larson MJ, Miller K, Tompkins C, et al. Prevalence and costs of major depression among elderly claimants with diabetes. Diabetes Care. 2003;26(2):415–420. doi: 10.2337/diacare.26.2.415. [DOI] [PubMed] [Google Scholar]
- 10.Simon GE, Katon WJ, Lin EHB, Ludman E, VonKorff M, Ciechanowski P, et al. Diabetes complications and depression as predictors of health service costs. Gen Hosp Psychiatry. 2005;27(5):344–351. doi: 10.1016/j.genhosppsych.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, et al. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33(2):264–269. doi: 10.2337/dc09-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Groot M, Jacobson AM, Samson JA, Welch G. Glycemic control and major depression in patients with type 1 and type 2 diabetes mellitus. J Psychosom Res. 1999;46(5):425–435. doi: 10.1016/s0022-3999(99)00014-8. [DOI] [PubMed] [Google Scholar]
- 13.Manarte LF, Dias S, Gois C, Boavida JM. Independent factors associated with depression in type 1 diabetes mellitus. Acta Diabetol. 2010;47(3):201–207. doi: 10.1007/s00592-009-0110-y. [DOI] [PubMed] [Google Scholar]
- 14.Makine C, Karsidag C, Kadioglu P, Ilkova H, Karsidag K, Skovlund SE, et al. Symptoms of depression and diabetes-specific emotional distress are associated with a negative appraisal of insulin therapy in insulin-naive patients with Type 2 diabetes mellitus. A study from the European Depression in Diabetes [EDID] Research Consortium. Diabet Med. 2009;26(1):28–33. doi: 10.1111/j.1464-5491.2008.02606.x. [DOI] [PubMed] [Google Scholar]
- 15.Aikens JE, Perkins DW, Lipton B, Piette JD. Longitudinal analysis of depressive symptoms and glycemic control in type 2 diabetes. Diabetes Care. 2009;32(7):1177–1181. doi: 10.2337/dc09-0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gonzalez JS, Safren SA, Cagliero E, Wexler DJ, Delahanty L, Wittenberg E, et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007;30(9):2222–2227. doi: 10.2337/dc07-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hutter N, Schnurr A, Baumeister H. Healthcare costs in patients with diabetes mellitus and comorbid mental disorders—a systematic review. Diabetologia. 2010;53(12):2470–2479. doi: 10.1007/s00125-010-1873-y. [DOI] [PubMed] [Google Scholar]
- 18.Hensen LG, Chang S. White paper. Ann Arbor, MI: Thompson Reuters; 2010. Health research rata for the real world: The Thompson Reuters Marketscan Databases; pp. 1–28. [Google Scholar]
- 19.Thomson Medstat. MarketScan (R) Research Databases User Guide and Database Dictionary: Commercial Claims and Encounters Medicare Supplemental and COB. 2005. Ann Arbor, MI: Thomson Medstat; [Google Scholar]
- 20.Shrestha SS, Zhang P, Albright A, Imperatore G. Medical expenditures associated with diabetes among privately insured U.S. youth in 2007. Diabetes Care. 2011;34(5):1097–1101. doi: 10.2337/dc10-2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gibson TB, Jing Y, Smith Carls G, Kim E, Bagalman JE, Burton WN, et al. Cost burden of treatment resistance in patients with depression. Am J Manag Care. 2010;16(5):370–377. [PubMed] [Google Scholar]
- 22.Hellinger FJ, Encinosa WE. The cost and incidence of prescribing errors among privately insured HIV patients. Pharmacoeconomics. 2010;28(1):23–34. doi: 10.2165/11313810-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 23.Cohen FJ, Neslusan CA, Conklin JE, Song X. Recent antihyperglycemic prescribing trends for US privately insured patients with type 2 diabetes. Diabetes Care. 2003;26(6):1847–1851. doi: 10.2337/diacare.26.6.1847. [DOI] [PubMed] [Google Scholar]
- 24.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 25.Diehr P, Yanez D, Ash A, Hornbrook M, Lin DY. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–144. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- 26.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 27.Cutler DM, McClellan M, Newhouse JP. How does managed care do it? Rand J Econ. 2000;31(3):526–548. [PubMed] [Google Scholar]
- 28.Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Annals of Family Medicine. 2012;10:15–22. doi: 10.1370/afm.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Katon W, Unutzer J, Fan MY, Williams JW, Jr, Schoenbaum M, Lin EH, et al. Cost-effectiveness and net benefit of enhanced treatment of depression for older adults with diabetes and depression. Diabetes Care. 2006;29(2):265–270. doi: 10.2337/diacare.29.02.06.dc05-1572. [DOI] [PubMed] [Google Scholar]
- 30.Katon WJ, Russo JE, Von Korff M, Lin EHB, Ludman E, Ciechanowski PS. Long-term effects on medical costs of improving depression outcomes in patients with depression and diabetes. Diabetes Care. 2008;31(6):1155–1159. doi: 10.2337/dc08-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Simon GE, Katon WJ, Lin EHB, Rutter C, Manning WG, Von Korff M, et al. Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Arch Gen Psychiatry. 2007;64(1):65–72. doi: 10.1001/archpsyc.64.1.65. [DOI] [PubMed] [Google Scholar]
- 32.Li C, Ford ES, Zhao G, Ahluwalia IB, Pearson WS, Mokdad AH. Prevalence and correlates of undiagnosed depression among U.S. adults with diabetes: the Behavioral Risk Factor Surveillance System, 2006. Diabetes Res Clin Pract. 2009;83(2):268–279. doi: 10.1016/j.diabres.2008.11.006. [DOI] [PubMed] [Google Scholar]