LETTER TO THE EDITOR
A single intravenous dose of ketamine, a N-methlyl D-aspartate receptor (NMDAR) full antagonist, produces robust and rapid anti-obsessional effects in obsessive-compulsive disorder (OCD),1, 2 but ketamine’s side effects, including dissociation and nausea, may limit clinical use.1, 3–5 Rapastinel (formerly GLYX-13), a putative NMDAR functional glycine-site partial agonist, has shown rapid anti-depressant activity without ketamine-like side effects,6 and may be a new therapeutic strategy for OCD. We conducted the first test of the tolerability and potential efficacy of rapastinel administration in OCD. Specifically, we explored the drug’s acute effects on obsessive-compulsive symptoms, depression and anxiety at 90 and 230 minutes post-infusion and at one week post-infusion.
Methods
With IRB approval, seven unmedicated OCD outpatients (aged 18–55) were recruited (March, 2014 – March, 2015) and provided written informed consent. Patients met criteria for OCD (both DSM-IV and DSM-5) with at least moderate symptoms (Yale-Brown Obsessive-Compulsive Scale [Y-BOCS7, 8] score ≥16). Exclusion criteria included severe depression (Hamilton Depression Rating Scale [17 item version] >25),9 current cognitive behavioral therapy, and other comorbid psychiatric or medical conditions that made participation unsafe.
Patients (n=7) received a single 3–5 minute IV push of rapastinel (dose=10 mg/kg). At baseline, 90, and 230 minutes post-infusion, patients self-rated the severity of their obsessions and compulsions (Y-BOCS Challenge Scale [YBOCCS],10 a 10 item self-report form that assesses OCD symptoms [i.e., time spent, degree of control, severity] [total score range 0–40] over the previous 60 minutes, facilitating symptom evaluation over shorter time intervals), anxiety (Beck Anxiety Inventory [BAI]11), and depression (Beck Depression Inventory [BDI]12). Side effects of dissociation,13 mania,14 and psychosis15 were assessed at baseline, 90, and 230 minutes post-infusion. At baseline and one week post-infusion, an independent evaluator, blind to study design, evaluated patients using the Y-BOCS, which appraises obsessive and compulsive symptoms over the prior week, and patients self-rated anxiety (BAI) and depression (BDI). Treatment response was defined a priori as ≥35% Y-BOCS reduction.16 Outcomes were analyzed using a non-parametric Wilcoxon signed-rank matched-pairs test (α = .05, two-tailed) without adjustment for multiple comparisons given the exploratory nature of this study.
Results
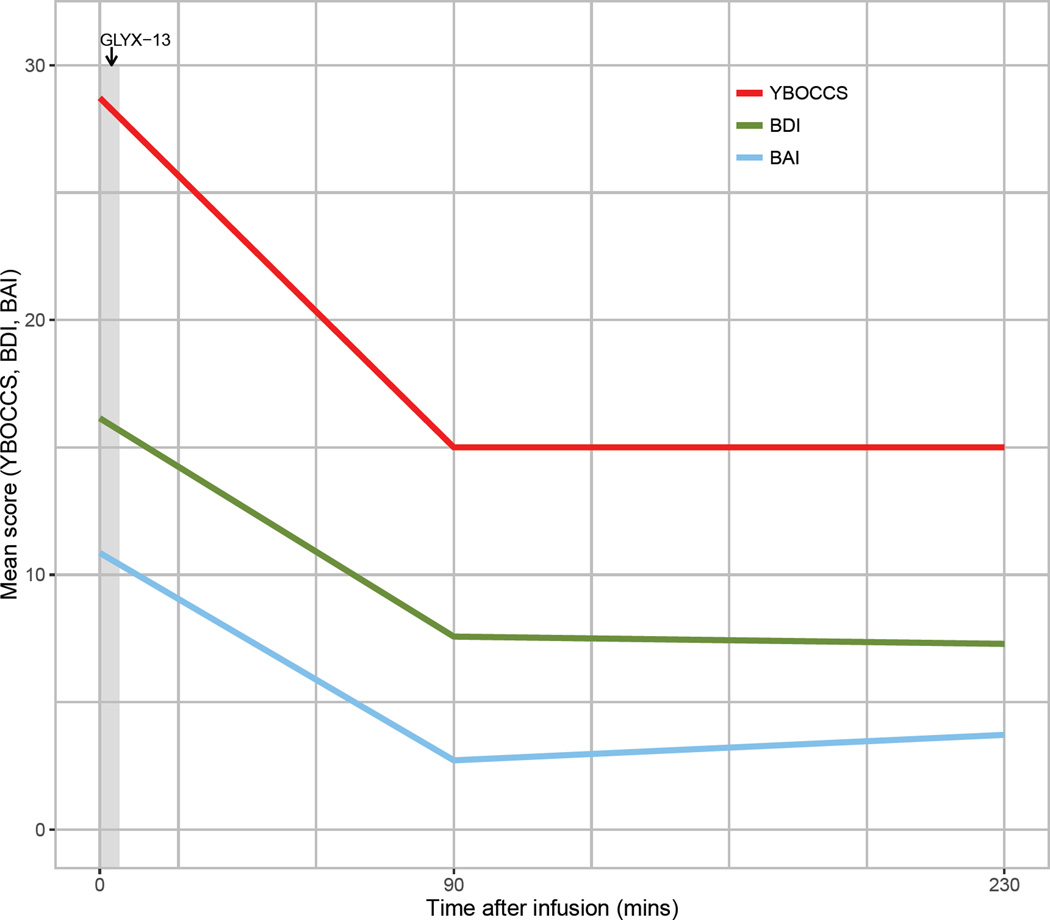
All seven patients who received rapastinel completed the infusion. Patients had severe OCD symptoms: mean Y-BOCS score at baseline was 28.9 (SD = 4.4), with mean duration of illness of 24.9 years (SD = 10.6 years). The mean number of prior adequate serotonin reuptake inhibitor (SRI) trials was 3.4 (SD = 2.8, median = 3, with range 0–7). In our sample, 86% received at least one adequate trial of an SRI, 29% failed at least one prior adequate trial of antipsychotic augmentation, and 57% failed at least one prior adequate trial of cognitive behavior therapy with exposure and response prevention. Three of the seven OCD subjects (43%) had no other psychiatric comorbidity. Two subjects (29%) met criteria for comorbid generalized anxiety disorder. Two (29%) met criteria for comorbid major depression, with baseline HDRS scores of 11 (mild) and 14 (moderate). Compared to baseline, YBOCCS, BAI, and BDI scores were significantly lower at 90 and 230 minutes post-infusion (all p values < .05; Figure 1 and Supplementary Figure 1; the percentage decrease in YBOCCS from baseline to 230 minutes post infusion was 46.4%). OCD severity, as measured by the Y-BOCS, was not significantly decreased (p = .20) from baseline to one week post-infusion, nor was BDI (p = .20), although BAI was significantly decreased (p = .02). No patient met the treatment response criterion (≥35% Y-BOCS reduction) at one week post-infusion (mean Y-BOCS score was 28.9 [SD = 4.4] at baseline and 26.0 [SD = 5.4] at one week post infusion). One individual with mild comorbid depression had further reduction in HDRS score from 11 (at baseline) to 1 (at 230 min), with a slight increase to 7 (by one week post rapastinel infusion).
Figure 1. Obsessive-compulsive, Depression, and Anxiety Severity Mean Scores at baseline, 90, and 230 minutes after a Single Infusion of Rapastinel (N=7).
At baseline, 90, and 230 minutes post infusion (rapastinel 10mg/kg), patients self-rated the severity of their obsessions and compulsions (YBOCCS [range 0–40]), anxiety (BAI [range 0–63]), and depression (BDI [range 0–63]). For the 90 and 230 minute assessments, patients were instructed to rate their symptoms over the past 60 minutes for all three measures. Means scores are plotted for each assessment measure.
Abbreviation: YBOCCS = Yale-Brown Obsessive Compulsive Challenge Scale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory.
Rapstinel was well tolerated. Of note, in contrast to participant reports in a prior study of IV ketamine in OCD,1 participants did not report adverse events (e.g., dizziness, nausea, vomiting, or headache). Assessments of dissociation, mania, and psychosis were not significantly changed from baseline.
Conclusions/Discussion
The findings suggest that rapastinel is well tolerated in unmedicated OCD patients, as it is in patients with depression.6 Specifically, rapastinel did not increase psychotomimetic effects following dosing in this sample of OCD patients, unlike ketamine in prior studies.1, 3–5 In this small open-label sample, rapastinel had acute effects on obsessions and compulsions, anxiety and depression. However, rapastinel did not have significant effects on OCD symptoms one week post-infusion. To have clinical utility, glutamate modulators should refine molecular targets for rapid and sustained action while minimizing side effects. Mechanistic preclinical data suggests drugs like rapastinel17 and ketamine’s metabolite hydroxynorketamine1,8 that act on AMPA receptor modulation pathways may be promising therapeutic strategies.
Supplementary Material
At baseline, 90, and 230 minutes post-infusion (rapastinel 10mg/kg), patients self-rated the severity of their: a) obsessions and compulsions (YBOCCS [range 0–40]), b) anxiety (BAI [range 0–63]), and c) depression (BDI [range 0–63]). For the 90 and 230 minute assessments, patients were instructed to rate their symptoms over the past 60 minutes for all three measures. Box plots illustrate the first quartile (bottom of box), third quartile (top of box), median (dark line), mean score (red circle), and maximum and minimum (lines extending vertically from the boxes), except for outliers (black circle).
Abbreviation: YBOCCS = Yale-Brown Obsessive Compulsive Challenge Scale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory.
Acknowledgments
The authors thank the individuals who generously donated their time to participate in this research study.
Funding support: This study was supported by the Brain and Behavior Research Foundation/NARSAD Ellen Schapiro and Gerald Axelbaum Investigator Award (Dr. Rodriguez), the National Institutes of Mental Health (K23MH092434 [Dr. Rodriguez], K24MH09155 [Dr. Simpson]), the New York Presbyterian Youth Anxiety Center (NYP-YAC), and the New York State Psychiatric Institute (NYSPI). Rapastinel (formerly GLYX-13) study drug was supplied by Naurex (since drug donation, Naurex has been acquired by Allergan).
Dr. Rodriguez received rapastinel for the present study at no cost, and she was reimbursed for travel and time to present findings to Allergan after the letter was submitted for publication; she reports no additional financial relationships relevant to the subject of this letter. Dr. Simpson received royalties from Cambridge University Press and UpToDate, Inc. Dr. Moskal was founder and owned stock in Naurex and Dr. Burch was an employee at Naurex when rapastinel was donated for the current study.
Role of the Sponsor: NARSAD, NYP-YAC, NIMH, and NYSPI had no role in the design, analysis, interpretation or publication of this study. Naurex supplied study materials (rapastinel at no cost) and Naurex staff participated in the outline of the study but had no role in study selection or interpretation of the data. Although staff at Allergan reviewed the manuscript, final approval for the decision to submit the manuscript was the sole decision of the authors.
Footnotes
Previous Presentation: None
Financial Disclosures: Drs. Kalanthroff, Shen, Jo, Filippou, and Ms. Zwerling, report no additional financial or other relationships relevant to the subject of this manuscript. Dr. Rodriguez received rapastinel for the present study at no cost, and she was reimbursed for travel and time to present findings to Allergan after the letter was submitted for publication; she reports no additional financial relationships relevant to the subject of this letter. Dr. Simpson received royalties from Cambridge University Press and UpToDate, Inc. Dr. Moskal was founder and owned stock in Naurex and Dr. Burch was an employee at Naurex when rapastinel was donated for the current study.
REFERENCES
- 1.Rodriguez CI, Kegeles LS, Levinson A, et al. Randomized controlled crossover trial of ketamine in obsessive-compulsive disorder: proof-of-concept. Neuropsychopharmacology. 2013 Nov;38(12):2475–2483. doi: 10.1038/npp.2013.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez CI, Wheaton M, Zwerling J, et al. Can exposure-based CBT extend the effects of intravenous ketamine in obsessive-compulsive disorder? an open-label trial. J Clin Psychiatry. 2016 Mar;77(3):408–409. doi: 10.4088/JCP.15l10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez CI, Kegeles LS, Flood P, Simpson HB. Rapid resolution of obsessions after an infusion of intravenous ketamine in a patient with treatment-resistant obsessive-compulsive disorder. J Clin Psychiatry. 2011 Apr;72(4):567–569. doi: 10.4088/JCP.10l06653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bloch MH, Wasylink S, Landeros-Weisenberger A, et al. Effects of ketamine in treatment-refractory obsessive-compulsive disorder. Biol Psychiatry. 2012 Dec 1;72(11):964–970. doi: 10.1016/j.biopsych.2012.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niciu MJ, Grunschel BD, Corlett PR, Pittenger C, Bloch MH. Two cases of delayed-onset suicidal ideation, dysphoria and anxiety after ketamine infusion in patients with obsessive-compulsive disorder and a history of major depressive disorder. J Psychopharmacol. 2013 Jul;27(7):651–654. doi: 10.1177/0269881113486718. [DOI] [PubMed] [Google Scholar]
- 6.Moskal JR, Burch R, Burgdorf JS, et al. GLYX-13, an NMDA receptor glycine site functional partial agonist enhances cognition and produces antidepressant effects without the psychotomimetic side effects of NMDA receptor antagonists. Expert opinion on investigational drugs. 2014 Feb;23(2):243–254. doi: 10.1517/13543784.2014.852536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989 Nov;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 8.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989 Nov;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodman WK, Price LH, Woods SW, Charney DS. Pharmacological challenges in obsessive compulsive disorder. In: Zohar J, Insel T, Rasmussen S, editors. The Psycho-biology of Obsessive Compulsive Disorder. NY: Springer Pub. Co; 1991. p. 183. [Google Scholar]
- 11.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;(4):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 13.Bremner JD, Krystal JH, Putnam FW, Southwick SM, Marmar C, DS C. Measurement of dissociative states with the Clinician-Administered Dissociative States Scale (CADSS) J Trauma Stress. 1998;11:125–136. doi: 10.1023/A:1024465317902. [DOI] [PubMed] [Google Scholar]
- 14.Young RC, Biggs JT, Ziegler VE, Meyer DA. Young Mania Rating Scale. The British Journal of Psychiatry. 1978;133:429. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 15.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychology Reports. 1962;10:799–812. [Google Scholar]
- 16.Tolin DF, Abramowitz JS, Diefenbach GJ. Defining response in clinical trials for obsessive-compulsive disorder: a signal detection analysis of the Yale-Brown obsessive compulsive scale. J Clin Psychiatry. 2005 Dec;66(12):1549–1557. doi: 10.4088/jcp.v66n1209. [DOI] [PubMed] [Google Scholar]
- 17.Burgdorf J, Zhang XL, Nicholson KL, et al. GLYX-13, a NMDA receptor glycine-site functional partial agonist, induces antidepressant-like effects without ketamine-like side effects. Neuropsychopharmacology. 2013 Apr;38(5):729–742. doi: 10.1038/npp.2012.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zanos P, Moaddel R, Morris PJ, et al. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature. 2016 May 4; doi: 10.1038/nature17998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
At baseline, 90, and 230 minutes post-infusion (rapastinel 10mg/kg), patients self-rated the severity of their: a) obsessions and compulsions (YBOCCS [range 0–40]), b) anxiety (BAI [range 0–63]), and c) depression (BDI [range 0–63]). For the 90 and 230 minute assessments, patients were instructed to rate their symptoms over the past 60 minutes for all three measures. Box plots illustrate the first quartile (bottom of box), third quartile (top of box), median (dark line), mean score (red circle), and maximum and minimum (lines extending vertically from the boxes), except for outliers (black circle).
Abbreviation: YBOCCS = Yale-Brown Obsessive Compulsive Challenge Scale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory.