Abstract
Endovascular particle embolization is a common procedure with a relatively safe profile. We report here four cases in which cranial nerves, skin and mucosal ischemic complications occurred with the use of hydrogel microspheres (250–500 µm in size). Given the compressibility and higher penetration potential of microsphere particles compared with polyvinyl alcohol particles of similar size, we suggest oversizing hydrogel microsphere particles for head and neck embolizations.
Keywords: Particles, embolization, ischemia, cranial nerve palsy, necrosis
Introduction
Endovascular particle embolization for head and neck tumors and epistaxis management1 is a safe, efficacious and well established procedure.2–8 Two categories of particles are commonly used: polyvinyl alcohol (PVA) (old generation, irregular shape) and hydrogel microsphere (new generation, spherical) particles. We report here ischemic complications that unexpectedly occurred at the level of cranial nerves, skin and mucosa during head and neck embolization procedures using microsphere particles and we review some of the particle characteristics that could explain these complications.
Methods and case reports
A retrospective review of four cases in which complications were noted was carried out, including a review of the medical charts, procedural notes and radiographic documents. The literature was reviewed by searching the following key terms on the Pubmed database: particles and embolization. We also conducted a review of our quality control database and looked up details of our head and neck embolization procedures.
Case 1
A 57-year-old man underwent endovascular embolization for epistaxis which was refractory to conservative management (bilateral endoscopic packing). Under general anesthesia, embolization of the bilateral distal internal maxillary and distal right facial arteries was achieved using Bead Block microsphere particles (size range 300–500 µm; BTG International Ltd., UK). The intervention successfully stopped the bleeding but the patient awoke with diplopia secondary to right trochlear nerve (cranial nerve IV) palsy (confirmed by ophthalmology). A brain magnetic resonance imaging prior to hospital discharge did not show any abnormality. The diplopia had resolved at 6-month follow-up.
Case 2
A 59-year-old man underwent, under general anesthesia, endovascular embolization for refractory epistaxis on day 3 following elective nasal septoplasty. Because the bleeding was predominantly coming from the right nostril we embolized first the right internal maxillary artery and the right facial artery using Bead Block microspheres (size range 300–500 µm). Only after this particle embolization the left external carotid artery was catheterized and active bleeding from a pseudoaneurysm on the sphenopalatine branch of the left internal maxillary artery was demonstrated. Following selective micro-catheterization, the pseudoaneurysm was embolized using histoacryl glue diluted at 25% without any visible distal glue migration or complication. The intervention successfully stopped the bleeding but the patient developed necrosis of the right nostril skin in the days following the procedure, which required surgical debridement by a plastic surgeon.
Case 3
A 49-year-old woman with a family history of Osler–Weber–Rendu syndrome presented with massive bilateral epistaxis requiring posterior nasal packing and endovascular embolization of the distal bilateral internal maxillary arteries using Bead Block microspheres (size range 300–500 µm). The patient remained intubated for 24 hours under critical care and the nasal packing was kept for 5 days. They were discharged on day 7 with no symptoms but returned on day 20 complaining of a constant foul smell in the mouth and nose. Examination revealed necrosis of the hard palate mucosa, exposure of the palatine bone and the presence of an oronasal fistula. The patient was started on antibiotics and was offered reconstructive surgery which they declined. The fistula was therefore treated with a buccal prosthesis by a stomatologist.
Case 4
A 21-year-old male patient with a one-year history of recurrent intermittent bilateral epistaxis leading to the diagnosis of juvenile angiofibroma of the right nasopharynx was admitted for elective preoperative embolization. The patient underwent endovascular particle embolization of the right internal maxillary artery with Embozene microspheres (250 µm; CeloNova Biosciences, San Antonio, TX, USA) under local anesthesia. Following the procedure, the patient developed diplopia with right and downward gaze, as well as pain and pressure sensation in the right eye. Examination by a neurologist showed right oculomotor nerve palsy (cranial nerve III). The patient underwent the planned endonasal endoscopic surgery after which vision further deteriorated as bilateral vertical diplopia developed secondary to orbital floor edema, for which a short course of corticosteroid was administered. Magnetic resonance brain imaging did not identify any ischemic cause of his initial cranial nerve III palsy. The patient was discharged home and returned for a 3-week follow-up with no visual symptoms.
Discussion
We hereby describe four cases of complications that are believed to be ischemic with transient cranial nerve palsies and skin and mucosal necrosis after head and neck particle embolization. These events occurred in a period during which a shortage of our usual PVA particles triggered the use of microsphere particles with which we had no previous experience. Prior to our use of microspheres (July 2013), a total of 243 head and neck embolization procedures were performed at our institution between January 2004 and June 2013 with no complications recorded in our morbidity mortality reports which could be related to particles. In contrast, we performed 38 head and neck embolizations between July 2013 and December 2014. It is during this time that the four complications described occurred, leading us to review the charts and try to understand what was wrong.
Those complications were unexpected by us because the size of the chosen particles was larger than the normal arterioles vascularizing cranial nerves (between 100 and 300 µm),9 skin or mucosal capillaries, and because of our extensive experience with head and neck embolization procedures using PVA particles without any ischemic complications. Ischemia in such locations using large size PVA particles is considered unlikely to occur owing to the small size of the capillary blood supply and the extent of collateralization (e.g. the microvascular bed of the nasal cavity). In cases of embolization for epistaxis management, for example, thrombosis occurs6 safely with blood flow reduction while distal necrosis is rarely seen.
Two types of embolization particles are available to the neuro-interventionist: PVA and hydrogel microsphere particles.
PVA particles have been used for endovascular embolization for over 30 years.10,11 PVA particles are ellipsoid and irregular in shape (Figure 1); they behave like a sponge and swell when suspended in contrast medium.12 They were initially ‘homemade’13 but later became available in commercially prepared dry form supplied in several ranges of particle size. Early reports of clinical complications14,15 and death16 in head and neck applications were thought to be related to impurity in particle size12 (with smaller size particles infiltrated in PVA preparations). Manufacturers have since improved the sieving process and the uniformity of now commercially available products was demonstrated by Derdeyn et al.12 The safety profile of this embolization agent since its industrial refinement is reflected in the literature4–6,17 and translated to daily routine in neuro-interventional practice. Morbid complications (stroke, loss of vision, cranial nerve paresis, necrosis of the parotid gland and soft tissue necrosis including nasal ala, buccal mucosa, hard palate and facial skin)18 are the most feared complications but they remain rare occurrences as reviewed by Sadri et al.19 They are thought to occur secondary to particle embolization to the internal carotid artery territories via internal/external carotid arterial anastomoses. Inadvertent embolization and forceful embolization with reflux into proximal non-desired vessels account for most complications described with PVA. The frequency of minor complications (mild facial, jaw or nasal pain, headache, eyelid edema and transient ischemic attack) has been shown to be proportional to the number of vessels embolized.17
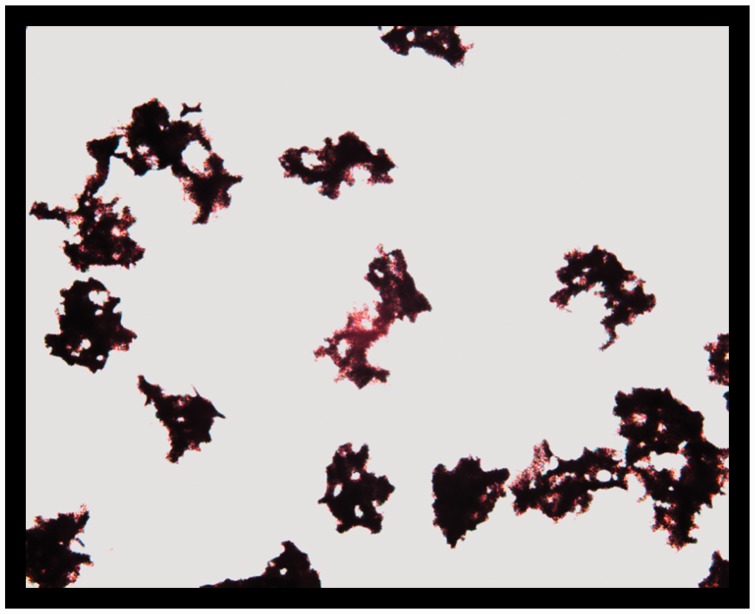
Figure 1.
Optic microscope 250–355 microns PVA particles (Contour; Boston Scientific).
Hydrogel microspheres, developed in the mid-1980s,20 are effective endovascular embolization agents as a result of their hydrophilic nature, high swelling ability, non-toxicity and non-biodegradable properties among others.21 They are slippery and compressible when in suspension, making them ideal for injections through microcatheters.22 They are commercially available in a pre-mixed form offering several ranges of well calibrated particle size.23 At the time of their commercial introduction, the provided sizes were chosen theoretically to match the size ranges of arterioles detectable by angiography and accessible to selective catheterization. Three commonly used US Food and Drug Administration approved brands – Embosphere, Bead Block and Embozene (Figure 2) – share the following properties: a compressible microsphere made of an acrylic core (trisacryl, acrylamido-PVA and polymethylmethacrylate, respectively) and a hydrophilic coating (a water-insoluble polymer connected in a three-dimensional framework, or hydrogel).23–27 The safety of microspheres in head applications was reported in a prospective case series of 55 patients compared with a historical control, in which large size 400 µm calibrated Embozene microspheres were associated with no intracranial hemorrhage following meningioma embolization, conferring to them a safety profile unlike any previously published safety data.28 Although fragmentation was not observed following suspension and manipulation of microsphere particles, they were shown to be easily deformed by a needle or indented by other particles.29 Compressibility along with lack of aggregation and smooth hydrophilic surfaces are likely to be the basis for the ease of injectability and lack of hub accumulation and catheter occlusions seen with microspheres. On the other hand, as a result also of their compressibility, they penetrate into small caliber arterioles and travel more distally than PVA particles of the same size as demonstrated in animal experiments of pig rete embolization.29 Compared with 200–300 µm PVA particles which aggregated at the proximal rete, embolization using similar size microsphere hydrogel particles (100–300 µm Embosphere) lead to complete packing of the rete (average arteriolar diameter 173.3 µm) and embolization of microspheres to the brain.29 In addition, initial experience with microspheres reported a discrepancy of 400 µm on average between the initially chosen particle size with which an operator started the embolization procedure and the final (larger) size which was required for efficacious occlusion.30 Several clinical trials and prospective case series for the use of microsphere particles in vascular interventional radiology are available in the literature,25,27,31–35 but large case series or reports of major morbidity related to microsphere particle embolization for head and neck applications such as epistaxis have not been published.
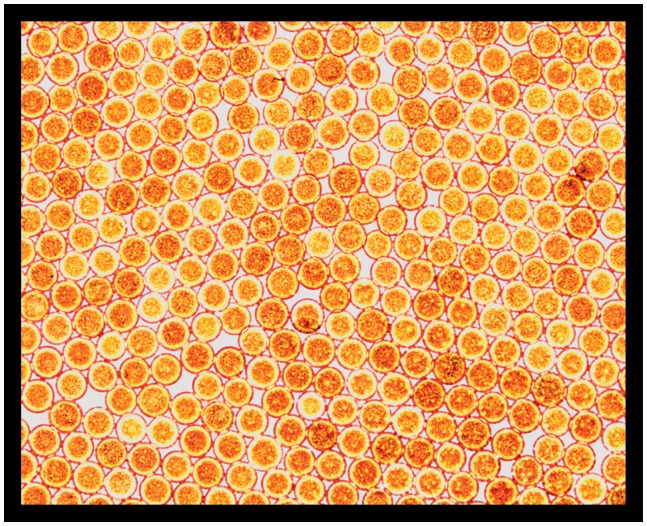
Figure 2.
Optic microscope 250 microns Embozene (CeloNova Biosciences).
We believe that we undersized the microsphere particles chosen for our embolization procedures. We invite readers to consider oversizing their microsphere particles for head and neck embolization and not to apply their experience with PVA particle sizing to the sizing routine of microspheres. The limitation to our recommendation is the retrospective nature of the case report.
In case 2, because the bleeding was apparently coming from the right side we started the embolization on the right side. We only discovered that the bleeding was due to a pseudoaneurysm on the left sphenopalatine artery when we injected the left external carotid artery. This pinpoints the importance of doing a bilateral diagnostic angiogram for epistaxis. Glue was used for the pseudoaneurysm occlusion but the ischemic complication occurred on the right side where only particles were injected.
In case 3, we acknowledge that the prolonged packing may have enhanced ischemia.
Nevertheless, all four events, feared and well known by neuro-interventionists but not seen before in our institution, occurred in a short period of time corresponding to the change in particles. We thus believe in a causality effect. This, to our knowledge, is the first report of complications with head and neck hydrogel microsphere particle embolization procedures leading to ischemia at the level of small arterioles and capillary beds. From our side, we decided to revert back to PVA particles when they became available again.
Conclusion
Hydrogel microspheres are efficacious embolization agents which have recently gained ground in head and neck applications. In our limited experience, their use was associated with cranial nerve ischemia as well as skin and mucosal necrosis, probably due to the relatively small size of the particles used (250–500 µm). As a result of their compressibility and penetration potential in arterioles smaller than their stated size range, it is suggested to oversize microsphere particles for head and neck embolization and not to compare microsphere size choice with that of PVA.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Dubel GJ, Ahn SH, Soares GM. Transcatheter embolization in the management of epistaxis. Semin Intervent Radiol 2013; 30: 249–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quisling RG, Mickle JP, Ballinger W. Small particle polyvinyl alcohol embolization of cranial lesions with minimal arteriolar-capillary barriers. Surg Neurol 1986; 25: 243–252. [DOI] [PubMed] [Google Scholar]
- 3.Wehrli M, Lieberherr U, Valavanis A. Superselective embolization for intractable epistaxis: experiences with 19 patients. Clin Otolaryngol Allied Sci 1988; 13: 415–420. [DOI] [PubMed] [Google Scholar]
- 4.Elden L, Montanera W, Terbrugge K, et al. Angiographic embolization for the treatment of epistaxis: a review of 108 cases. Otolaryngol Head Neck Surg 1994; 111: 44–50. [DOI] [PubMed] [Google Scholar]
- 5.Moreau S, De Rugy MG, Babin E, et al. Supraselective embolization in intractable epistaxis: review of 45 cases. The Laryngoscope 1998; 108: 887–888. [DOI] [PubMed] [Google Scholar]
- 6.Tseng EY, Narducci CA, Willing SJ, et al. Angiographic embolization for epistaxis: a review of 114 cases. The Laryngoscope 1998; 108: 615–619. [DOI] [PubMed] [Google Scholar]
- 7.Ricci G, Molini E, Hamam M, et al. Treatment of severe epistaxis by superselective embolization: a review of 22 cases. Rev Laryngol Otol Rhinol (Bord) 2004; 125: 247–251. [PubMed] [Google Scholar]
- 8.Andersen PJ, Kjeldsen AD, Nepper-Rasmussen J. Selective embolization in the treatment of intractable epistaxis. Acta Otolaryngol 2005; 125: 293–297. [DOI] [PubMed] [Google Scholar]
- 9.Ozanne A, Pereira V, Krings T, et al. Arterial vascularization of the cranial nerves. Neuroimag Clin North Am 2008; 18: 431–439, xii. [DOI] [PubMed] [Google Scholar]
- 10.Tadavarthy SM, Moller JH, Amplatz K. Polyvinyl alcohol (Ivalon) – a new embolic material. Am J Roentgenol Radium Ther Nucl Med 1975; 125: 609–616. [DOI] [PubMed] [Google Scholar]
- 11.Sokoloff J, Wickbom I, McDonald D, et al. Therapeutic percutaneous embolization in intractable epistaxis. Radiology 1974; 111: 285–287. [DOI] [PubMed] [Google Scholar]
- 12.Derdeyn CP, Moran CJ, Cross DT, et al. Polyvinyl alcohol particle size and suspension characteristics. AJNR Am J Neuroradiol 1995; 16: 1335–1343. [PMC free article] [PubMed] [Google Scholar]
- 13.Berenstein A, Graeb DA. Convenient preparation of ready-to-use particles in polyvinyl alcohol foam suspension for embolization. Radiology 1982; 145: 846. [DOI] [PubMed] [Google Scholar]
- 14.Handa J, Nakasu S, Matsuda I. Facial nerve palsy following therapeutic embolization. Surg Neurol 1980; 14: 377–380. [PubMed] [Google Scholar]
- 15.Lasjaunias P. Nasopharyngeal angiofibromas: hazards of embolization. Radiology 1980; 136: 119–123. [DOI] [PubMed] [Google Scholar]
- 16.Repa I, Moradian GP, Dehner LP, et al. Mortalities associated with use of a commercial suspension of polyvinyl alcohol. Radiology 1989; 170: 395–399. [DOI] [PubMed] [Google Scholar]
- 17.Gottumukkala R, Kadkhodayan Y, Moran CJ, et al. Impact of vessel choice on outcomes of polyvinyl alcohol embolization for intractable idiopathic epistaxis. J Vasc Interv Radiol 2013; 24: 234–239. [DOI] [PubMed] [Google Scholar]
- 18.Yilmaz M, Mamanov M, Yener M, et al. Acute ischemia of the parotid gland and auricle following embolization for epistaxis. The Laryngoscope 2013; 123: 366–368. [DOI] [PubMed] [Google Scholar]
- 19.Sadri M, Midwinter K, Ahmed A, et al. Assessment of safety and efficacy of arterial embolisation in the management of intractable epistaxis. Eur Arch Otorhinolaryngol 2006; 263: 560–566. [DOI] [PubMed] [Google Scholar]
- 20.Horak D, Svec F, Kalal J, et al. Hydrogels in endovascular embolization. I. Spherical particles of poly(2-hydroxyethyl methacrylate) and their medico-biological properties. Biomaterials 1986; 7: 188–192. [DOI] [PubMed] [Google Scholar]
- 21.Jayakrishnan A, Thanoo BC, Rathinam K, et al. Preparation and evaluation of radiopaque hydrogel microspheres based on PHEMA/iothalamic acid and PHEMA/iopanoic acid as particulate emboli. J Biomed Mater Res 1990; 24: 993–1004. [DOI] [PubMed] [Google Scholar]
- 22.Rao VR, Ravimandalam K, Jayakrishnan A, et al. Hydrolysed microspheres from cross-linked polymethyl methacrylate (Hydrogel). A new embolic material for interventional neuroradiology. J Neuroradiol 1991; 18: 61–69. [PubMed] [Google Scholar]
- 23.Laurent A, Beaujeux R, Wassef M, et al. Trisacryl gelatin microspheres for therapeutic embolization, I: development and in vitro evaluation. AJNR Am J Neuroradiol 1996; 17: 533–540. [PMC free article] [PubMed] [Google Scholar]
- 24.Laurent A. Microspheres and nonspherical particles for embolization. Tech Vasc Interv Radiol 2007; 10: 248–256. [DOI] [PubMed] [Google Scholar]
- 25.Kroencke TJ, Scheurig C, Lampmann LE, et al. Acrylamido polyvinyl alcohol microspheres for uterine artery embolization: 12-month clinical and MR imaging results. J Vasc Interv Radiol 2008; 19: 47–57. [DOI] [PubMed] [Google Scholar]
- 26.Stampfl S, Stampfl U, Bellemann N, et al. Biocompatibility and recanalization characteristics of hydrogel microspheres with polyzene-F as polymer coating. Cardiovasc Intervent Radiol 2008; 31: 799–806. [DOI] [PubMed] [Google Scholar]
- 27.Bonomo G, Pedicini V, Monfardini L, et al. Bland embolization in patients with unresectable hepatocellular carcinoma using precise, tightly size-calibrated, anti-inflammatory microparticles: first clinical experience and one-year follow-up. Cardiovasc Intervent Radiol 2010; 33: 552–559. [DOI] [PubMed] [Google Scholar]
- 28.Sluzewski M, van Rooij WJ, Lohle PN, et al. Embolization of meningiomas: comparison of safety between calibrated microspheres and polyvinyl-alcohol particles as embolic agents. AJNR Am J Neuroradiol 2013; 34: 727–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Derdeyn CP, Graves VB, Salamat MS, et al. Collagen-coated acrylic microspheres for embolotherapy: in vivo and in vitro characteristics. AJNR Am J Neuroradiol 1997; 18: 647–653. [PMC free article] [PubMed] [Google Scholar]
- 30.Beaujeux R, Laurent A, Wassef M, et al. Trisacryl gelatin microspheres for therapeutic embolization, II: preliminary clinical evaluation in tumors and arteriovenous malformations. AJNR Am J Neuroradiol 1996; 17: 541–548. [PMC free article] [PubMed] [Google Scholar]
- 31.Spies JB, Allison S, Flick P, et al. Polyvinyl alcohol particles and tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: results of a randomized comparative study. J Vasc Interv Radiol 2004; 15: 793–800. [DOI] [PubMed] [Google Scholar]
- 32.Bilhim T, Pisco JM, Duarte M, et al. Polyvinyl alcohol particle size for uterine artery embolization: a prospective randomized study of initial use of 350–500 mum particles versus initial use of 500–700 mum particles. J Vasc Interv Radiol 2011; 22: 21–27. [DOI] [PubMed] [Google Scholar]
- 33.Worthington-Kirsch RL, Siskin GP, Hegener P, et al. Comparison of the efficacy of the embolic agents acrylamido polyvinyl alcohol microspheres and tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: a prospective randomized controlled trial. Cardiovasc Intervent Radiol 2011; 34: 493–501. [DOI] [PubMed] [Google Scholar]
- 34.Yu SC, Lok I, Ho SS, et al. Comparison of clinical outcomes of tris-acryl microspheres versus polyvinyl alcohol microspheres for uterine artery embolization for leiomyomas: results of a randomized trial. J Vasc Interv Radiol 2011; 22: 1229–1235. [DOI] [PubMed] [Google Scholar]
- 35.Shlansky-Goldberg RD, Rosen MA, Mondschein JI, et al. Comparison of polyvinyl alcohol microspheres and tris-acryl gelatin microspheres for uterine fibroid embolization: results of a single-center randomized study. J Vasc Interv Radiol 2014; 25: 823–832. [DOI] [PubMed] [Google Scholar]