Abstract
The formation of a traumatic arteriovenous fistula (AVF) between the extracranial middle meningeal artery (MMA) and the pterygoid plexus (PP) is very rare, and understanding of this condition is limited. This paper reports the case of an 8-year-old who suffered minor injuries after a high fall four months prior to admission and showed good recovery after one month. However, the child gradually developed exophthalmos of the left eye and conjunctival redness one month prior to admission. Auscultation revealed an intracranial murmur near the left side of the face, in the temporal region. A digital subtraction angiography (DSA) showed rupture of the left extracranial MMA and an AVF between the MMA and the PP. The blood drained toward the cavernous sinus, resulting in retrograde blood flow into the ophthalmic vein and the cortical vein. The diagnosis was an AVF between the MMA and the PP, and a combination of coils and Onyx liquid embolic agent was employed to perform AVF embolization. Follow-up six months later indicated no recurrence of the AVF, and the patient showed good recovery with a normal-appearing left eye. The AVF in this case drained toward the cavernous sinus, and symptoms of increased intracranial venous system pressure were apparent, similar to those produced by fistulas between the internal carotid artery and the cavernous sinus. This condition is very rare, and the use of coils in combination with Onyx for AVF embolization is novel, warranting the reporting of the current case.
Keywords: Middle meningeal artery (MMA), pterygoid plexus (PP), arteriovenous fistula (AVF)
Introduction
The development of a traumatic arteriovenous fistula (AVF) between the middle meningeal artery (MMA) and the pterygoid plexus (PP) is very rare because the MMA and PP are well hidden in the temporal fossa and not easily injured.1,2 In rare cases, the MMA and the PP may become damaged, causing them to communicate with each other, which can result in the appearance of an AVF. An AVF between the MMA and the PP generally occurs following serious injury;3 however, it can also result from mild trauma. For example, the patient in the current case report did not appear to experience skull fracture or intracranial hemorrhage after a high fall; however, an AVF appeared between the MMA and the PP three months after the fall. Because the PP tends to drain into the external carotid veins, craniocerebral injury symptoms are absent in most cases, and drainage into the intracranial venous system can occur in rare cases,4 such as in the case in this report. In addition to presenting a case report, this work reviews the potential options for treating an AVF between the MMA and PP and broadens understanding of the condition.
Case report
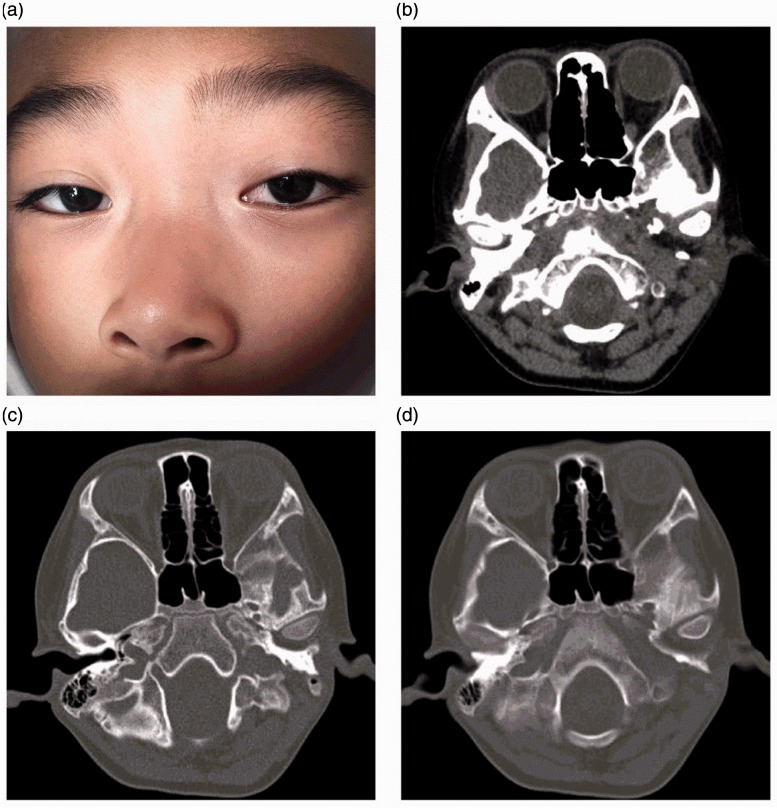
An 8-year-old boy was admitted for exophthalmos of the left eye with redness and swelling accompanied by an intracranial murmur for one month. The boy accidentally suffered a fourth-floor fall while playing four months prior to admission, and a tree prevented him from landing on the ground. He had a pulmonary contusion, fractured ribs, subluxation of the cervical vertebrae, splenic and renal contusions, and head and facial soft tissue contusions; however, all of these symptoms were mild. The patient showed good recovery by one month after the accident. However, during the one month prior to admission, the patient’s left eyeball began to gradually protrude, accompanied by slight redness and swelling in the eyeball. However, there was no diplopia. Additionally, a murmur consistent with the heartbeat could be heard at rest. Physical examination showed mild protrusion of the left eyeball, conjunctival congestion, free movement of the eyeball in each direction, and normal binocular vision. A murmur consistent with the heartbeat could be heard in the left temporal region and anterior left ear on auscultation. There were no other positive signs associated with the nervous system. The exophthalmos and conjunctival congestion were as shown in Figure 1a. Soft tissue computed tomography (CT) of the eye showed protrusion of the left eyeball, but no findings behind the eyeball, as shown in Figure 1b. Skull base CT showed no evidence of skull fracture, as shown in Figure 1c and d. Based on the exophthalmos, conjunctival congestion and intracranial murmur, a traumatic fistula between the internal carotid artery and the carotid cavernous sinus was considered. Whole-brain digital subtraction angiography (DSA) was used to obtain a definite clinical diagnosis.
Figure 1.
Preoperative facial image and head computed tomography (CT) images. (a) The child’s facial image indicates mild redness and swelling of the left eyeball with exophthalmos. (b) A CT scan at the level of the left eyeball indicates exophthalmos, and no abnormal findings were observed at the posterior eyeball. (c) and (d) A skull base CT shows no fracture of the skull base.
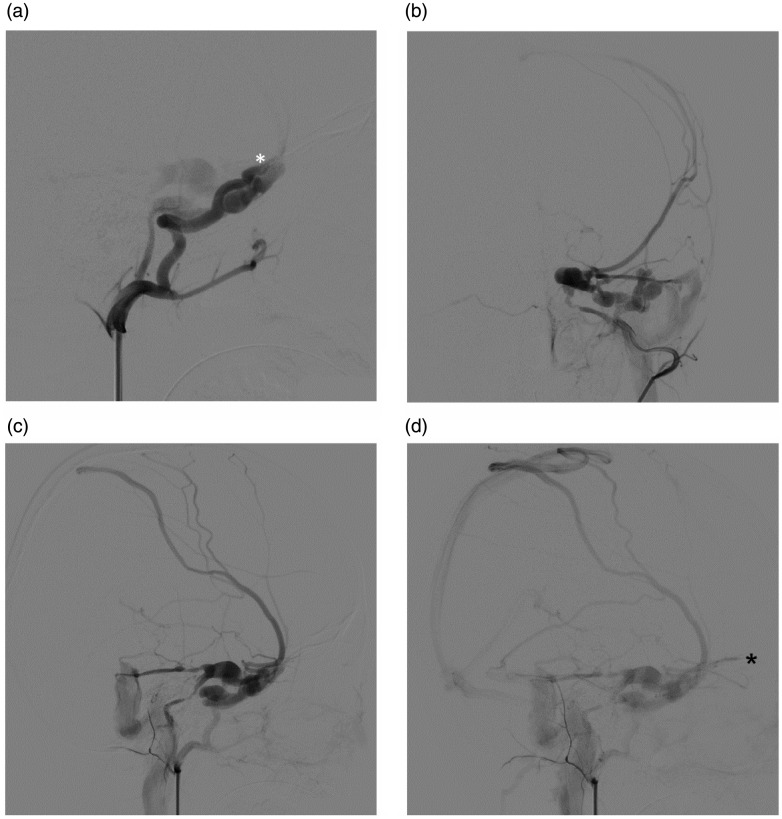
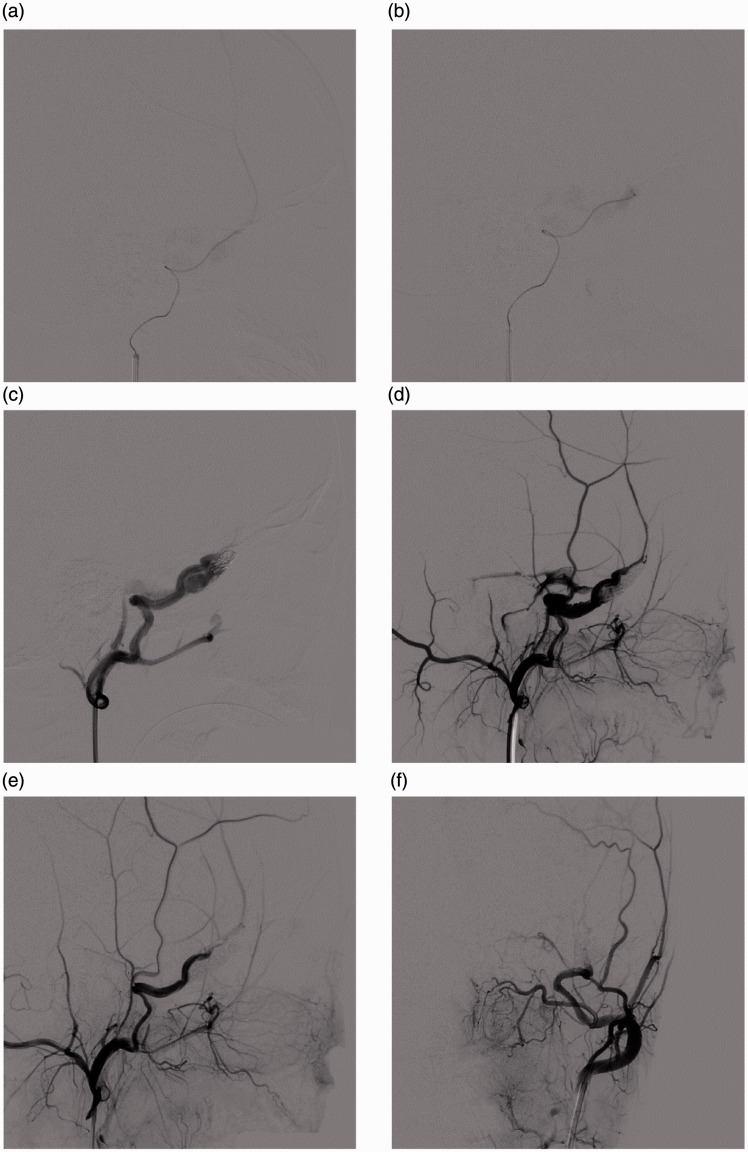
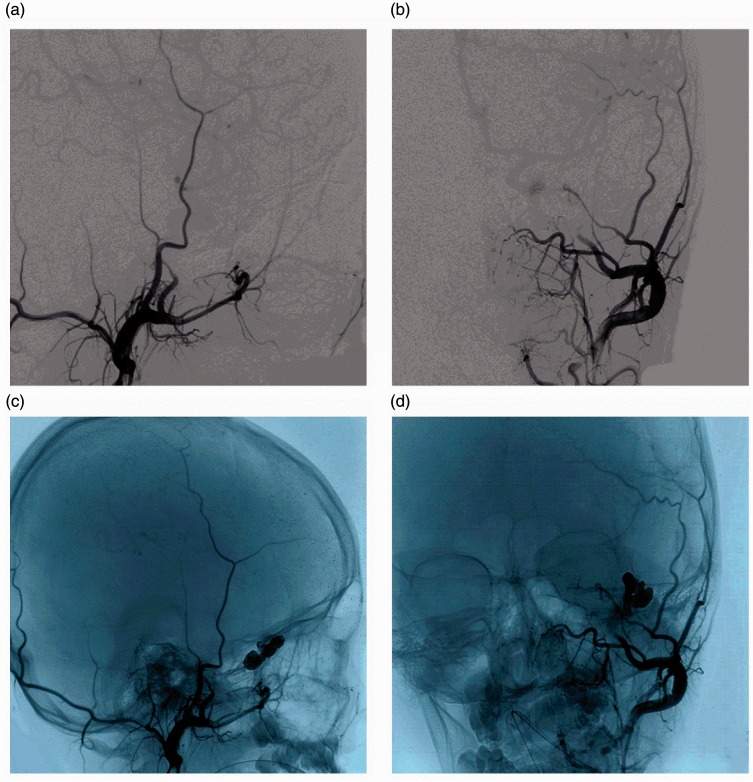
During the DSA examination, the left external carotid artery showed an AVF in the extracranial MMA. The blood flowed upward through the PP, into the cavernous sinus and then into the superior petrosal sinus and the interior petrosal sinus. The blood flowed into the sphenoparietal sinus and the superior sagittal sinus through the sylvian fissure vein and the upper anastomotic vein. A later DSA showed retrograde blood flow into the ophthalmic vein. The DSA images are shown in Figure 2. The definite diagnosis was an AVF between the MMA and the PP, and AVF embolization was proposed. At first, an Echelon-10 microcatheter was used to cross the fistula orifice using a Sycro-14 microguidewire, and the result showed the distal MMA. Then, the microcatheter was introduced into the fistula orifice. A coil was used for embolization of the fistula orifice. Three coils were used to fill the AVF, and imaging was used to confirm that the coils had occupied the fistula orifice. Then, Onyx was injected until the AVF completely disappeared. The treatment process is shown in Figure 3. The patient showed good recovery after the operation, and the intracranial murmur disappeared. The left eyeball returned to normal by six months after the operation, and follow-up DSA showed no recurrence of the AVF, although the proximal end of the MMA was blocked and the distal end was not developed. The follow-up DSA images are shown in Figure 4.
Figure 2.
Preoperative DSA images. (a) Lateral external carotid artery angiography indicates AVF, with the blood supply artery being the MMA. The white star indicates the fistula orifice, and blood can be observed flowing through the PP. (b) AP external carotid artery angiography indicates AVF drainage through the PP into the cavernous sinus. (c) Lateral external carotid artery angiography indicates that blood flow from the cavernous sinus goes to the superior petrosal sinus and the interior petrosal sinus. The blood then flows into the sphenoparietal sinus and the superior sagittal sinus through the lateral vein and the superior anastomotic vein. (d) Later, lateral left external carotid artery angiography showed the retrograde flow of blood into the ophthalmic vein. The star indicates the ophthalmic vein. DSA: digital subtraction angiography. AVF: arteriovenous fistula; MMA: middle meningeal artery; PP: pterygoid plexus; AP: anteroposterior.
Figure 3.
DSA images following treatment. (a) The microcatheter crossed the fistula orifice, and the angiography clearly shows the MMA; (b) The microcatheter was introduced into the fistula orifice, and the angiography shows the PP. (c) Lateral external carotid artery angiography indicates embolization with coils in the fistula orifice. (d) After the coil embolization, Onyx gel was injected to fill the AVF. (e) and (f) AP and lateral angiography at the end of the embolization indicates the disappearance of the AVF and the re-development of the distal end of the MMA. DSA: digital subtraction angiography; MMA: middle meningeal artery; PP: pterygoid plexus; AVF: arteriovenous fistula; AP: anteroposterior.
Figure 4.
DSA images taken six months postoperatively. (a) and (b) AP and lateral left external carotid artery angiography indicates no recurrence of the AVF, but occlusion at the proximal end of the MMA is apparent, and the distal end is not developed. (c) and (d) The non-silhouetted image shows the coils and the Onyx embolized in the AVF. DSA: digital subtraction angiography; AP: anteroposterior; AVF: arteriovenous fistula; MMA: middle meningeal artery.
Discussion
The formation of a traumatic AVF between the MMA and the adjacent venous structures is uncommon; these venous structures include the accompanying middle meningeal vein, the diploic vein, the cavernous sinus, the sphenoparietal sinus, the greater petrosal dural venous sinuses, and the cortical vein.5–8 Traumatic AVFs often occur in the area where the MMA passes through the basal foramen spinosum and in the area near the MMA groove in the medial skull. The angioarchitecture of AVFs in the MMA is complex. In 1981, Freckmann et al. classified AVFs in the MMA into six types based on venous drainage in angiography: I. drainage into the PP via the middle meningeal veins, characterized by the meningeal vessels adopting a train track-like appearance; II. drainage into the superior sagittal sinus via the sphenoparietal sinus or the other meningeal veins; III. drainage into the cavernous sinus via the sphenoparietal sinus; IV. drainage into the cavernous sinus/basilar plexus via the middle meningeal veins and the superior petrosal sinus; V. drainage via the diploic veins; and VI. drainage into the superior sagittal sinus via a bridging vein (e.g. the cortical vein).7 Freckmann et al. comprehensively discussed the various types of traumatic AVFs that can affect the MMA, but these AVFs are limited to the intracranial MMA. AVFs in the extracranial MMA, especially an AVF formed between the MMA and the PP, were not described. This is probably because AVFs between the MMA and the PP are rare or often neglected because of few intracranial symptoms. The current report discusses a rare case of an AVF between the MMA and the PP and aims to help increase understanding of traumatic AVFs in the MMA.
It is not easy for an extracranial AVF to form between the MMA and PP because of the anatomical features of these structures. The extracranial MMA is an important branch of the maxillary artery. The maxillary artery branches out to the MMA from the deep surface of the neck near the mandible to the temporal fossa. The extracranial MMA is surrounded by two auriculotemporal nerves between the sphenomandibular ligament and the lateral pterygoid muscle, and it enters the skull cavity upward through the foramen spinosum to form the intracranial MMA.1,2 The PP is also located in the temporal fossa, forming the venous plexus between the medial pterygoid, the extraocular muscles and the temporalis, surrounding the maxillary artery and the initiating area of its branches, including the extracranial MMA.9,10 Because the extracranial MMA and the PP are adjacent, it is possible for an AVF to form between them; however, the extracranial MMA and the PP are hidden in the temporal fossa and surrounded by soft tissues such as muscles and are therefore not easily damaged, making the formation of an AVF between the MMA and the PP very rare. AVFs in the intracranial MMA are typically caused by skull fracture, which causes avulsion of the MMA; this can result in communication with peripheral veins, leading to the formation of an AVF.11 The extracranial MMA and the PP are located in the temporal fossa, and skull base fractures typically do not injure these structures. However, the current case had special circumstances. The patient fell from the fourth floor, and he encountered a tree that prevented him from landing on the ground. The patient sustained facial abrasions and exhibited nose bleeding, and deformation of the maxillofacial bone was considered because the patient landed on his face. Extraction of the MMA and the PP resulted in avulsions of these structures, causing an AVF to form. A skull base CT scan failed to identify a fracture line, which supported the assumption that skull deformation ruptured the MMA and the PP. Deformation without fracture could have occurred because the patient is a child, and a child’s skull has better elasticity than the skull of an adult.12
If an AVF develops between the MMA and the PP, distal ischemia symptoms would not appear because of the large amount of collateral circulation in the MMA, and the appearance of clinical symptoms would mainly depend on the appearance of reversed drainage flow due to the increased venous pressure.13 Under normal circumstances, the PP guides the veins accompanying the maxillary artery branch into the maxillary vein, which flows back to the retromandibular vein. The PP connects with the facial vein through the inferior ophthalmic vein and the deep facial vein and connects with the cavernous sinus through a vein in the rete foraminis ovalis and the foramen lacerum.14 After an AVF forms between the MMA and the PP, it is possible that the arterial blood could drain via the external carotid vein after entering the PP, leading to an absence of intracranial symptoms. However, this case is special in that symptoms of a cavernous sinus fistula (CCF) in the internal carotid artery appeared after the AVF formed. This is likely because after the AVF the blood drained into the cavernous sinus via the foramen rotundum and the foramen ovale venous plexus, leading to similar symptoms as those produced by a CCF, which may have been associated with the reduced pressure in the cavernous sinus.15 In this case, the AVF drained into the cavernous sinus via the PP, leading to the superior and inferior petrosal sinus. The AVF also drained into the sylvian fissure vein toward the sagittal sinus through the sphenoid sinus; drainage to the ophthalmic vein was visible at the later DSA stage, producing ocular symptoms. Therefore, this case of an AVF between the MMA and the PP is descriptive of a high-flow direct fistula; as such, a murmur could be heard in the temporal region and on the left side of the face on auscultation. A high-flow AVF with reverse flow of the ocular vein and drainage of the cortex vein must be treated to prevent vein rupture and hemorrhage.16
For such a case of a traumatic AVF between the MMA and the PP, occlusion of the orifice of the AVF should be considered to prevent the abnormal flow of blood from the MMA into the PP. This treatment strategy may make the venous pressure in the cavernous sinus recover to normal, which would in turn cause the clinical symptoms to disappear. A ruptured MMA may not be retained because of the substantial difficulty associated with such retention and the rich collateral circulation at the distal end of the meningea. The simple application of coils to block the fistula orifice could be considered, but this may be challenging. In this study, a combination of coils and Onyx was adopted for embolization because coils can provide the support, while Onyx fills the hollows in coils. Coils combined with Onyx have been widely applied to treat large aneurysms, arteriovenous malformations and CCFs.17–20 The present case of AVF was located in the extracranial region, so the treatment was relatively safe. Embolization of the AVF with coils and Onyx was a satisfactory treatment option. The migration of Onyx must be considered when using this treatment option for AVF. To avoid this outcome, Onyx should be injected at both a fast and a slow rate, and the carotid artery should be compressed if necessary to prevent Onyx from flowing into the drainage vein too quickly. The treatment should be designed to avoid the excessive reflux of Onyx into the distal end of the MMA and into a dangerous anastomosis, which could produce symptoms of cranial nerve palsy.13
The development of a traumatic AVF between the MMA and the PP is very rare. When searching PubMed, only one similar case was found in a report by Ko and Kim from 2014. The 24-year-old patient in that study suffered an epidural hematoma after severe trauma and underwent removal of the hematoma. The patient experienced pulsatile tinnitus 25 days later. DSA identified an AVF between the MMA and the PP accompanied by a pseudoaneurysm in the MMA. The patient was treated by occlusion of the proximal end of the MMA with coils, and satisfactory results were achieved.3 The case reported by Ko and Kim differed from the case reported in the present study. First, the cases had different injury severities: Ko and Kim’s case resulted from severe head trauma, skull fracture and epidural hematoma, which are more likely to cause damage to the extracranial MMA, whereas there was no evidence of skull fracture or traumatic brain injury in the current case. This lack of fracture may be because the patient in the current study was a child, and children’s skulls have substantial elasticity, which could lead to avulsion of the MMA and PP, creating an AVF between them. Secondly, the clinical manifestations of the two patients differed. Ko and Kim’s case did not show drainage into the cavernous sinus, and the only symptom was pulsatile tinnitus. Furthermore, different treatment strategies were applied. Ko and Kim used coils to embolize the patient’s AVF in the MMA. Although satisfactory results could eventually be achieved with this strategy, the appearance of reversed blood flow in the MMA following treatment could lead to the recurrence of the AVF. Thus, this method does not provide as comprehensive of a solution as the use of coils combined with Onyx.
In summary, although rare, an AVF can form between the MMA and the PP, even in cases where trauma is not severe. The clinical manifestations of this condition mainly depend on the venous drainage pathways. Most drainage from the PP flows toward the external carotid vein and does not involve the intracranial venous system. In rare cases (e.g. in this case), blood may also drain into the cavernous sinus, which can cause similar clinical manifestations as those produced by a CCF, which should therefore be ruled out. The treatment for an AVF between the MMA and the PP should include thorough occlusion of the fistula orifice, for which the combination of coils and Onyx may be a suitable option.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Kornieieva M, Hadidy A, Zhuravlova I. Variability of the middle meningeal artery subject to the shape of skull. J Neurol Surg B Skull Base 2015; 76: 451–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chmielewski P, Skrzat J, Walocha J. Clinical importance of the middle meningeal artery. Folia Med Cracov 2013; 53: 41–46. [PubMed] [Google Scholar]
- 3.Ko JH, Kim YJ. Traumatic pseudoaneurysm of the middle meningeal artery with an arteriovenous fistula on a non-fractured site. Interv Neuroradiol 2014; 20: 352–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.San Millan Ruiz D, Oka M, Fasel JH, et al. Transvenous embolization of a dural arteriovenous fistula of the laterocavernous sinus through the pterygoid plexus. Neuroradiology 2007; 49: 665–668. [DOI] [PubMed] [Google Scholar]
- 5.Unterhofer C, Chemelli A, Waldenberger P, et al. Traumatic fistula between the middle meningeal artery and the sphenoparietal sinus. Acta Neurochir (Wien) 2009; 151: 1301–1304. [DOI] [PubMed] [Google Scholar]
- 6.Iakovlev SB. An arteriosinusal anastomosis between the middle meningeal artery and the cavernous sinus. Its surgical treatment using the balloon catheter [article in Russian]. Zh Vopr Neirokhir Im N N Burdenko 1997, pp. 31–33. [PubMed] [Google Scholar]
- 7.Freckmann N, Sartor K, Herrmann HD. Traumatic arteriovenous fistulae of the middle meningeal artery and neighbouring veins or dural sinuses. Acta Neurochir (Wien) 1981; 55: 273–281. [DOI] [PubMed] [Google Scholar]
- 8.Bitoh S, Hasegawa H, Fujiwara M, et al. Traumatic arteriovenous fistula between the middle meningeal artery and cortical vein. Surg Neurol 1980; 14: 355–358. [PubMed] [Google Scholar]
- 9.Joo W, Funaki T, Yoshioka F, et al. Microsurgical anatomy of the infratemporal fossa. Clin Anat 2013; 26: 455–469. [DOI] [PubMed] [Google Scholar]
- 10.Jahan R, Gobin YP, Glenn B, et al. Transvenous embolization of a dural arteriovenous fistula of the cavernous sinus through the contralateral pterygoid plexus. Neuroradiology 1998; 40: 189–193. [DOI] [PubMed] [Google Scholar]
- 11.Vassilyadi M, Mehrotra N, Shamji MF, et al. Pediatric traumatic dural arteriovenous fistula. Can J Neurol Sci 2009; 36: 751–756. [DOI] [PubMed] [Google Scholar]
- 12.Massenburg BB, Sanati-Mehrizy P, Taub PJ. Surgical treatment of pediatric craniofacial fractures: A national perspective. J Craniofac Surg 2015; 26: 2375–2380. [DOI] [PubMed] [Google Scholar]
- 13.Geibprasert S, Pongpech S, Armstrong D, et al. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: Vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol 2009; 30: 1459–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watanabe K, Kakeda S, Watanabe R, et al. Normal flow signal of the pterygoid plexus on 3T MRA in patients without DAVF of the cavernous sinus. AJNR Am J Neuroradiol 2013; 34: 1232–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zanaty M, Chalouhi N, Tjoumakaris SI, et al. Endovascular treatment of carotid-cavernous fistulas. Neurosurg Clin N Am 2014; 25: 551–563. [DOI] [PubMed] [Google Scholar]
- 16.Thomas AJ, Chua M, Fusco M, et al. Proposal of venous drainage-based classification system for carotid cavernous fistulae with validity assessment in a multicenter cohort. Neurosurgery 2015; 77: 380–385; discussion 385. [DOI] [PubMed] [Google Scholar]
- 17.John S, Jaffari N, Lu M, et al. Spontaneous vertebral arteriovenous fistula causing cervical myelopathy and acute ischemic strokes treated by endovascular balloon-assisted coiling and Onyx embolization. J Clin Neurosci 2014; 21: 167–170. [DOI] [PubMed] [Google Scholar]
- 18.Fang YB, Li Q, Yang PF, et al. Application of endovascular coiling and subsequent Onyx 34 embolization in anterior communicating artery aneurysms with adjacent hematoma. Clin Neurol Neurosurg 2014; 123: 40–44. [DOI] [PubMed] [Google Scholar]
- 19.Joshi KC, Singh D, Tandon MS. Intrafistula pressure measurement in traumatic carotid cavernous fistulas—key to increasing safety and effectiveness of endovascular coiling. Acta Neurochir (Wien) 2014; 156: 1695–1700. [DOI] [PubMed] [Google Scholar]
- 20.Gao X, Liang G, Li Z, et al. Transarterial coil-augmented Onyx embolization for brain arteriovenous malformation. Technique and experience in 22 consecutive patients. Interv Neuroradiol 2014; 20: 83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]