Supplemental Digital Content is Available in the Text.
Key Words: adherence, antiretroviral, HIV, homeless, housing stability, meta-analysis
Abstract
Background:
Previous research has produced inconsistent evidence of an association between housing stability and medication adherence among HIV-positive individuals in antiretroviral therapy.
Objective:
We conducted a meta-analysis of the housing–adherence relationship based on a comprehensive search of observational studies in the PubMed, Embase, and Cochrane databases (January 2000–January 2016). Ten qualifying studies were identified representing 10,556 individuals.
Methods:
A random-effects model was used to estimate the overall effect size and 95% confidence interval (CI). Robustness of the estimate was determined by sensitivity analysis. Heterogeneity was assessed by meta-regression analysis, subgroup analysis, and quality effects estimation. Publication bias was evaluated with a funnel plot and the Egger and Begg tests.
Results:
The summary effect for the association between housing stability and medication adherence was positive and significant (standardized mean difference = 0.15, 95% CI: 0.02 to 0.29). The association was slightly larger in the quality effects analysis (standardized mean difference = 0.20, 95% CI: 0.01 to 0.39). Sensitivity analysis disclosed that the association was robust at the P = 0.09 level. Results of the subgroup and meta-regression analyses were nonsignificant. Publication bias was not detected.
Conclusion:
Antiretroviral medication adherence is an increasing function of housing stability, but the magnitude of the effect is small. The finding challenges the view that unstable housing is incompatible with adherence and questions the potential benefit of deferring antiretroviral therapy initiation until the patient's housing circumstances are improved.
INTRODUCTION
Poor adherence to antiretroviral therapy (ART) among HIV-positive patients has been associated with incomplete viral suppression, the emergence of drug-resistant variants, and progression to AIDS.1 For economically vulnerable patients, efforts to adhere at high levels must compete with other survival needs, such as access to food and shelter.2 Arguably, patients who experience homelessness may be particularly disadvantaged with respect to adherence,3 facing a myriad of interrelated challenges including social isolation, substance use, mental illness, mistrust of the health care system, and inconsistent provider–patient relationships4—all of which affect access to services, health trajectories, and outcomes.5 Over the past 15 years, a body of observational research has investigated the relationship between housing stability and ART adherence. The findings have been inconsistent. Some studies have found a positive association between housing stability and adherence,6–10 whereas others have failed to reject the null hypothesis.11–15 We set out to synthesize the evidence of these studies. Our aims were 4-fold: to evaluate the methodological rigor of the individual studies, analyze the heterogeneity of effects across studies, compute a quantitative estimate of the overall association, and provide a test of the null with more power than is provided by the separate studies alone. In short, the present meta-analysis is designed to examine and test as precisely as possible the relationship between housing stability and ART adherence among people living with HIV (PLWH).
MATERIALS AND METHODS
Eligibility Criteria
Eligibility for inclusion in the meta-analysis was limited to observational studies which met all the following criteria:
the study population was adult PLWH who had a current ARV prescription and were engaged in ART;
the study classified each patient's housing status into one of several categories ordered in terms of greater or lesser housing stability—eg, living on the streets, in a car, or in a shelter vs. living in a single-room occupancy hotel or motel; doubling up with different people (couch surfing) vs. residing in an own or shared apartment or house;
the study measured the level of antiretroviral medication adherence—ie, taking medication as prescribed—for each patient. The instruments for measuring adherence differed across studies; and
the results of the statistical test of association between housing stability and adherence level were reported in adequate detail—eg, point estimate and standard error.
To reduce confounding and measurement error, we took a conservative approach to study selection. We excluded studies in which the measure of housing stability was entirely subjective (eg, are you worried about having a place to stay?), merged with another construct (eg, food–housing insecurity), or not time-specific (eg, were you ever homeless?). We also excluded studies in which the measure of adherence was merged with eligibility for therapy (eg, individuals who were eligible for but did not receive therapy were coded as not adherent) or discontinuation of therapy (eg, treatment discontinuation was coded as not adherent). Likewise, we excluded studies that limited their inquiry to a specific type of nonadherence (eg, sale or trade of ARV pills). Finally, to reduce heterogeneity due to international differences, we restricted our literature search to studies conducted in the United States, recognizing that the price for this restriction is a loss in generalizability. Our aim in this meta-analysis was a clear, direct, and focused test of the housing–adherence hypothesis.
Search Strategy
Systematic literature searches were conducted by a medical librarian, using PubMed (from 1947 through January 2016), Embase (from 1973 through January 2016), and Cochrane Central Register of Controlled Trials (from 1991 through January 2016), limiting the publication date between January 1, 2000, to January 31, 2016. For all databases, both controlled vocabulary and text word searches were performed. Manual searches of references from retrieved articles, major journals in the field, and gray literature (eg, abstracts and posters from scientific proceedings) were also performed to identify any additional relevant articles possibly missed by online indexes. We also contacted experts in the field to identify additional literature.
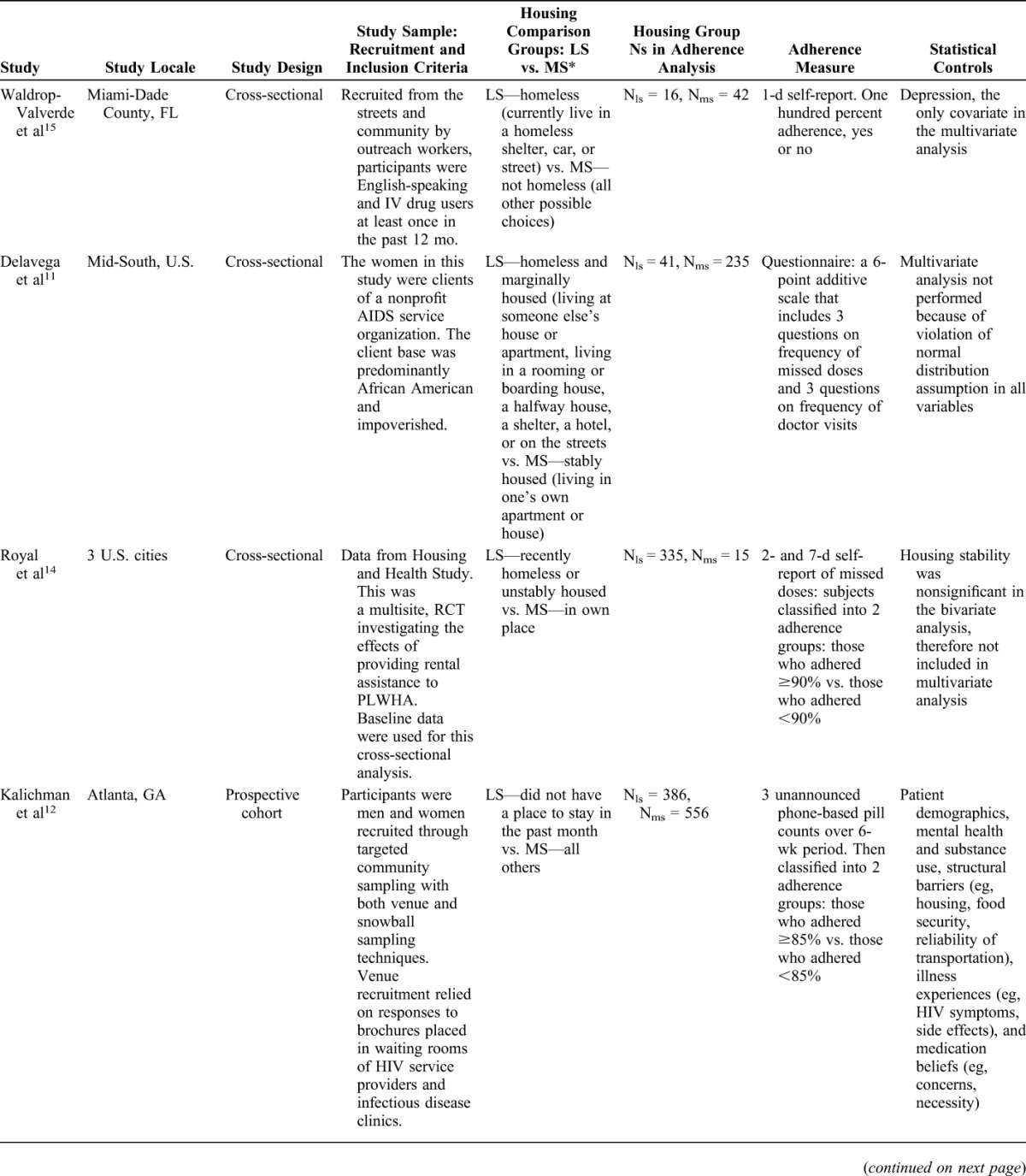
After the removal of 43 duplicates, the PubMed–Embase–Cochrane searches uncovered 164 articles. After screening the titles and abstracts, 85 articles were excluded, as they were not observational studies (eg, reviews, editorials, essays, and case reports) or studies conducted in the United States. The full text of 79 articles were collected and read. Of these, 61 did not analyze an association between housing and adherence among HIV+ individuals. Based on an evaluation by 2 of the authors, 10 studies did not meet the inclusion criteria, 8 met all the criteria, and an additional 2 studies were found through manual searches. Two of the authors conducted data extraction and quality assessment (QA) coding; there were no disagreements. A study selection flowchart (Figure S1), data extraction form (Table S1), and QA coding form (Table S2) are included in the Supplemental Digital Content, http://links.lww.com/QAI/A936. Table 1 lists the main characteristics of the 10 studies included in the meta-analysis.
TABLE 1.
Characteristics of Studies Included in the Meta-Analysis
Quality Assessment
A QA was conducted for each included study. The QA protocol evaluated each study on 6 domains:
research design: longitudinal vs. cross-sectional;
study locale: multisite vs. single site;
sample size in each housing comparison group;
operational definition of housing stability;
operational definition of medication adherence; and
statistical controls for potential confounders.
Each domain was judged on a quality continuum with 2 levels (higher and lower), as follows. Longitudinal research designs were rated “higher” as were multisite designs. The approach to sample size considered the N in each housing comparison group; a study population with ≥50 persons in each housing group was rated “higher.” The measure of housing stability in a study was rated “higher” if it used a clear and replicable operational definition for both comparators and did not use an undifferentiated residual category for one of the comparators (eg, all others were categorized as nonhomeless). A rating of “higher” for adherence required objective measurement (eg, medication event monitoring system caps, pharmacy refill data, and unannounced pill counts). We rated the adequacy of statistical controls “higher” if the study included a multivariate analysis that adjusted for other determinants of adherence (eg, food insecurity, depression, and substance abuse).
As most of the studies addressed several research questions, the housing–adherence question was not the main focus of each study. That was a limiting consideration in our choice of QA domains relative to the published methodological standards and guidelines for observational studies (eg, we did not include a domain for the prespecification of hypotheses).16 Also, the cutoff criteria separating “higher” from “lower” quality were, to some extent, unavoidably arbitrary for the sample size, housing, and adherence domains. We chose stringent criteria to frame a decisive test of the null hypothesis in the QA meta-regression analysis. In raising the bar, it should be emphasized that a “lower” rating on any 1 domain did not signify an overall weakness of a study. The QA relied on the full set of domains.
It is noteworthy that none of the studies scored “lower” or “higher” on every domain. Five of the 10 studies scored “higher” on 1 or 2 domains (Chen, Royal, Surratt, Waldrop-Valverde, and Delavega), and 5 studies scored higher on 3 or 4 domains (Berg, Kidder, Moss, Kalichman, and Johnson). Based on the sum of domains scored “higher,” each study was assigned a value from 1 to 4 on the QA scale. The scale served as an independent variable in the subgroup and meta-regression analysis. The ratings for each study (Table S3) are included in the Supplemental Digital Content, http://links.lww.com/QAI/A936.
Statistical Analysis
The outcome variable, adherence, was measured as a continuous variable in 4 of the primary articles (Berg, Moss, Surratt, and Delavega) and as a dichotomous variable in 6 articles (Johnson, Waldrop-Valverde, Kidder, Royal, Chen, and Kalichman). If a study reported multiple measures, we selected the result of the authors' primary adjusted model or the estimates with the greatest degree of adjustment for confounding. To meta-analyze studies that measured outcome in different ways, it was necessary to standardize the results of the studies to a uniform scale.17 We followed the usual convention in meta-analysis and converted the effect size reported in each primary article to a standardized mean difference (SMD).18 An SMD of 1.0 indicates that the mean values of 2 groups differ by 1 SD; an SMD of 0.5 indicates that the 2 groups' mean values differ by half an SD, and so on. For our specific area of inquiry, ie, estimating the association between housing stability and ART adherence, we considered the Cohen rule of thumb appropriate for interpreting the magnitude of the SMD effect size as follows: small = 0.20, medium = 0.50, and large = 0.80.19
To estimate pooled effects and confidence intervals (95% CIs), we used a random-effects model because of the anticipated heterogeneity due to study design differences. We conducted a sensitivity analysis by omitting each study in sequence to test the robustness of association. We also estimated the effect of housing stability on adherence with a quality effects model that incorporated QA scores into the weighting scheme of the meta-analysis to give higher quality studies proportionately more weight in the overall effect size. Meta-regression were performed to further investigate the effects of study quality on effect size and to test for a secular trend in the data. Additional investigations into possible sources of heterogeneity were conducted with subgroup analysis. To assess statistical heterogeneity beyond chance, we used the χ2 and I2 tests. Publication bias was assessed with a funnel plot and the Egger and Begg tests. Two-sided P values were presented, and significance was set at P < 0.05, except for the tests of homogeneity of effects where significance was set more conservatively at P < 0.10. We used MetaXL 5.2 for the quality effects model (Epigear International, Queensland, Australia). All other statistical analyses were performed using STATA 14.1 (StataCorp, College Station, TX).
RESULTS
Association Between Housing Stability and ART Adherence
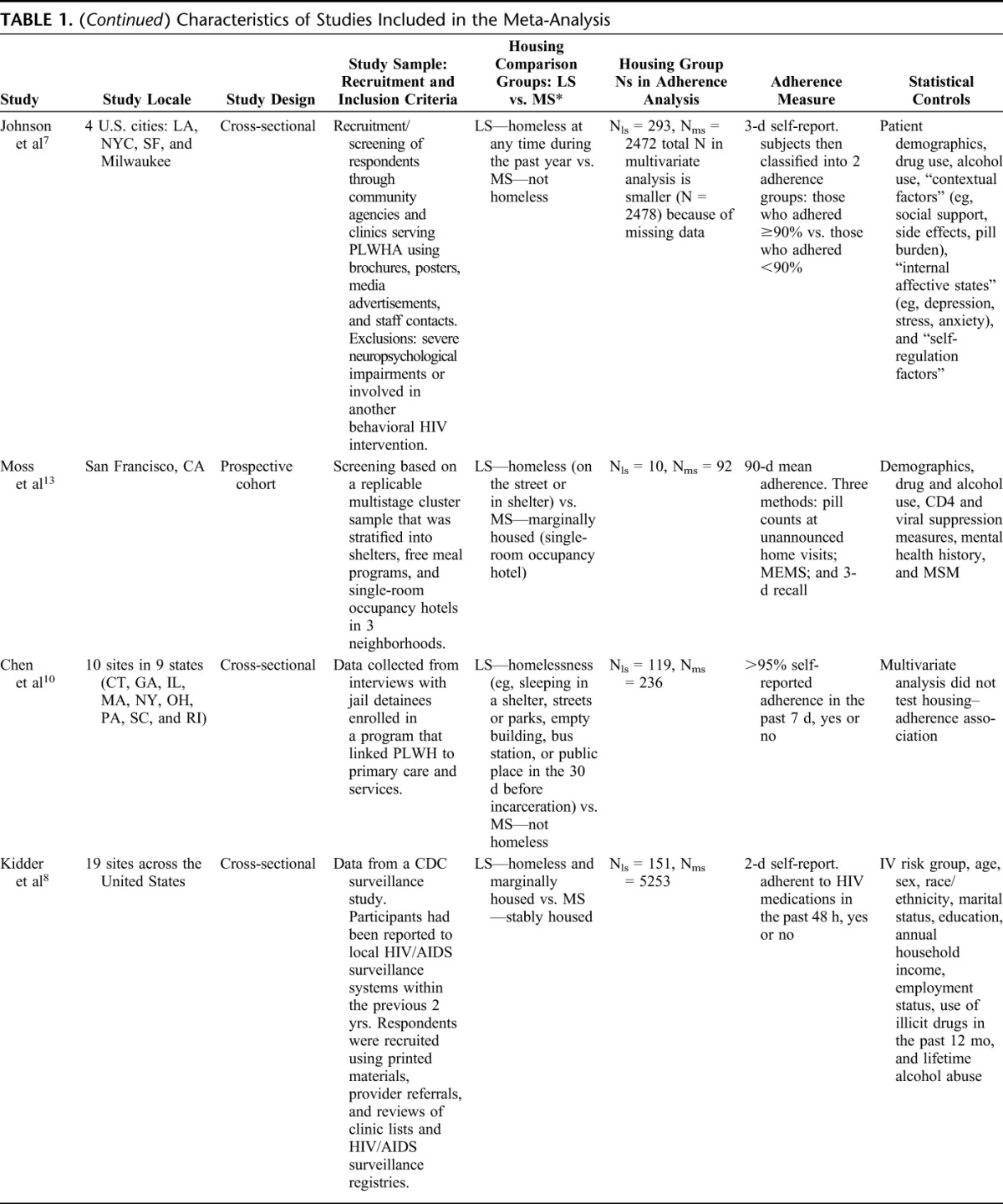
Ten studies, representing a total study population of 10,556 individuals, were included in the meta-analysis. Five studies showed a positive association, 5 showed no association, and none showed a negative association. Effect size heterogeneity was readily observable (Fig. 1) and statistically significant (I2 = 64%, P < 0.01). Of those studies reporting a positive association, the effect sizes ranged from small (Johnson: SMD = 0.13, 95% CI: 0.01 to 0.25) to medium (Berg: SMD = 0.57, 95% CI: 0.18 to 0.97). In the meta-analysis, the overall effect was positive (SMD = 0.15, 95% CI: 0.02 to 0.29).
FIGURE 1.
Forest plot of 10 observational studies examining the effect of housing stability on antiretroviral adherence among HIV-positive patients in treatment. The x-axis unit of measure is SMD. An SMD of 1.0 indicates that mean adherence for the housing comparison groups differ by 1 SD. Symbols: the size of the square boxes represent the relative weights of the primary studies in the meta-analysis. The dot in the center of a box indicates the point estimate of effect size, and the lines extending from the left and right of the box depict the 95% CI. The diamond represents the overall effect. The center of a diamond indicates the point estimate of effect size, and the width of a diamond is the precision of the estimate. ES, effect size.
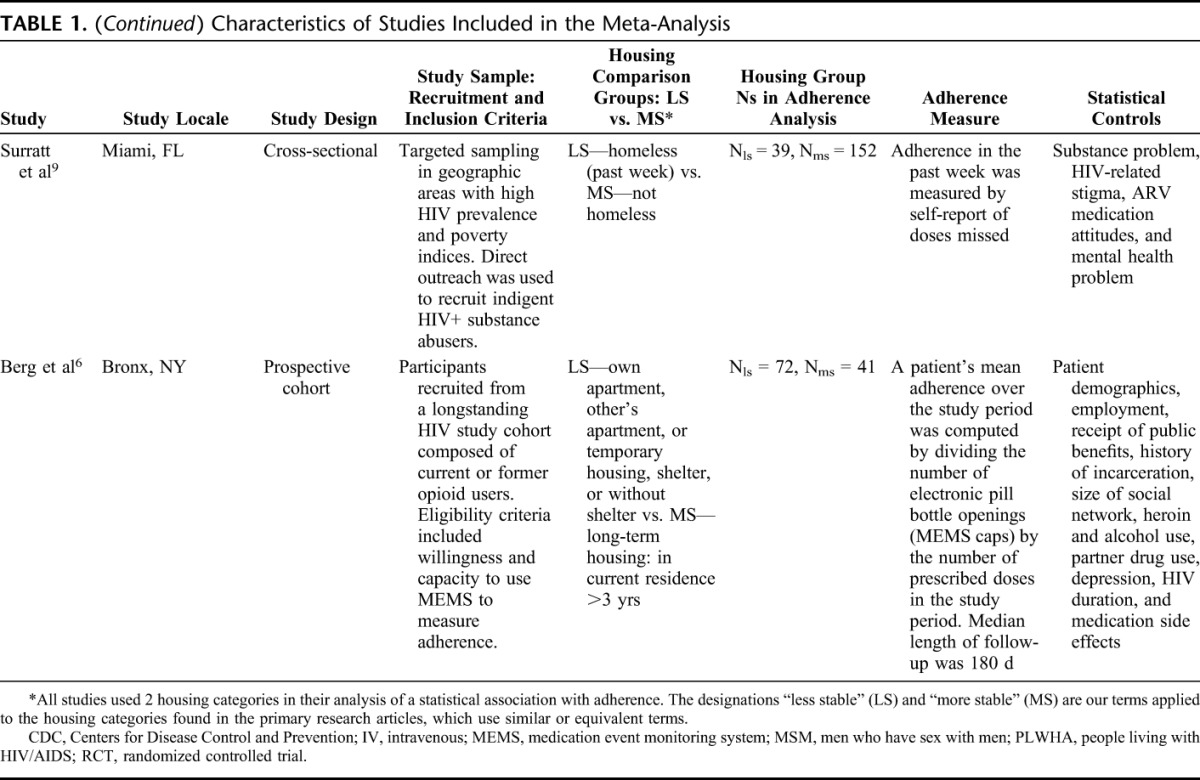
Sensitivity Analysis
To test the robustness of our findings, we performed a sensitivity analysis excluding each of the 10 studies in turn. This analysis showed that the pooled SMDs were similar in magnitude (Fig. 2). No outliers were present. However, one study, Kidder, was found to be especially influential, in part because it had the largest N among the studies reporting a positive association between housing and adherence. Exclusion of this study slightly decreased the size and lower bound of the pooled estimate (SMD = 0.13, 95% CI: −0.02 to 0.29), indicating that the association between housing and adherence was robust at the P = 0.09 level. Exclusion of the Kidder study did not affect heterogeneity (I2 = 63%, P < 0.01).
FIGURE 2.
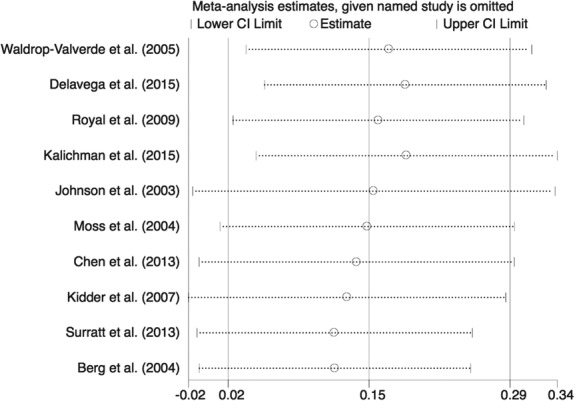
Sensitivity analysis of 10 observational studies examining the effect of housing stability on antiretroviral adherence among HIV-positive patients in treatment. The x-axis unit of measure is SMD. An SMD of 1.0 indicates that mean adherence for the housing comparison groups differ by 1 SD. Symbols: a circle represents the estimate of the summary effect size when that study is omitted from the meta-analysis. The dotted lines extending from the left and right of a circle depict the 95% CI.
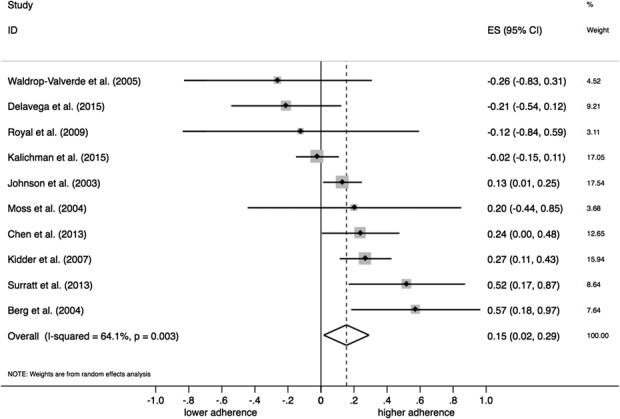
Subgroup, Meta-Regression, and Quality Effects Analysis
In a further investigation of heterogeneity, we conducted a QA subgroup analysis. Figure 3 displays the SMD and CI for each of the 10 studies grouped by numerical value on the QA scale along with the subgroup estimates. The test for differences across subgroups was not significant (P = 0.84). Similarly, the meta-regression analysis of the association between QA scale and SMDs revealed that the slope coefficient, although positive, was not significant (slope = 0.05, 95% CI: −0.11 to 0.21). We also estimated the overall effect using the quality effects statistical model. The model incorporates QA scores into the weighting scheme of the meta-analysis to give higher quality studies proportionately more weight in the overall effect size.20,21 The SMD was slightly larger in this analysis (SMD = 0.20, 95% CI: 0.01 to 0.39).
FIGURE 3.
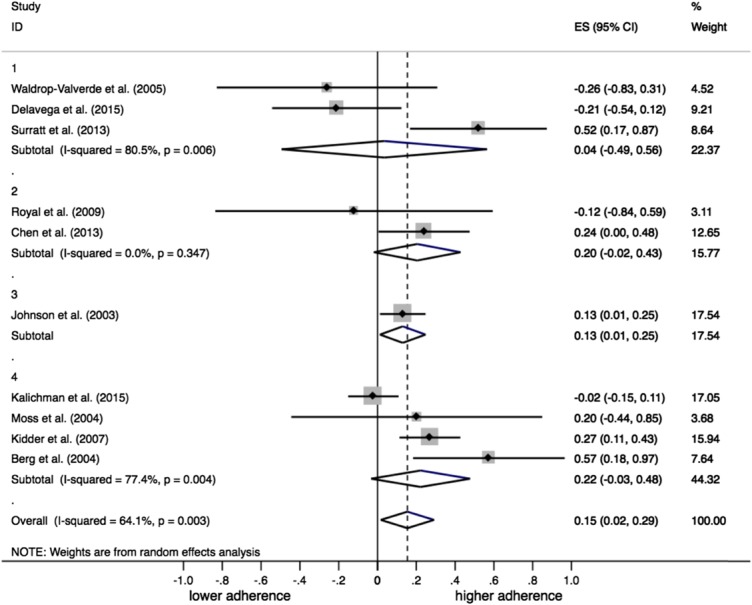
Subgroup analysis comparing effect size and 95% confidence limits by Quality Assessment scale. Values on the QA scale range from 1 (lowest quality) to 4 (highest quality). The x-axis unit of measure is SMD. An SMD of 1.0 indicates that mean adherence for the housing comparison groups differ by 1 SD. Symbols: the size of the square boxes represents the relative weights of the primary studies in the meta-analysis. The dot in the center of a box indicates the point estimate of effect size, and the lines extending from the left and right of the box depict the 95% CI. The diamonds represent the subgroup summary effects and the overall effect. The center of a diamond indicates the point estimate of effect size, and the width of a diamond is the precision of the estimate. ES, effect size.
Subgroup analysis was also used to examine whether differences in the operational definition of housing stability would account for part of the heterogeneity in the size of effects on adherence. We divided the 10 studies into 4 categories according to the definitions used in the housing comparisons. The test for differences across subgroups was not significant (P = 0.13). The subgroup analysis forest plot (Figure S3) is included in the Supplemental Digital Content, http://links.lww.com/QAI/A936.
Finally, we tested for a secular trend in the SMDs on the theory that patients' pill burden was substantial in the earlier years of our study period compared with the single-tablet regimens more common in the later years,22 and that the change would be reflected in a weaker association between housing and adherence over time. The meta-regression estimate for this association was not significant (slope = −0.01, 95% CI: −0.05 to 0.03).
Publication Bias
Visual inspection of the funnel plot (Figure S2 in the Supplemental Digital Content, http://links.lww.com/QAI/A936) did not show any obvious asymmetry. There was also no indication of publication bias as suggested by the Begg test (P = 0.66) and Egger test (P = 0.77).
DISCUSSION
This is the first meta-analysis to examine the effects of housing stability on adherence to ART among PLWH. Our results suggest an increased risk of nonadherence in patients living on the streets or in transient housing compared with those in more stable arrangements, but the magnitude of the effect is small. Previous literature reviews, by contrast, have concluded that there is a strong association between housing and adherence,23–25 but these conclusions did not rest on the rigorous statistical methods of meta-analysis. Our study fills that gap. In combining the primary studies into a single data set representing 10,556 individuals, we have computed a more precise estimate of the overall effect and conducted a more powerful test of the null, relative to less formal methods.
Our study has a number of important strengths and limitations. First, across the 10 observational studies, the dispersion of effect sizes was not overlarge, a finding which supports the logic of our strict eligibility criteria. The specific reasons for the heterogeneity remain unaccounted for. However, our investigations into possible sources of bias provide assurances that the individual studies are comparable—ie, address the same question with similar explanatory and outcome measures. Using the full complement of meta-analytic tools, we found no secular trend in the data, association of effect size with measurement approach to housing stability, or publication bias. Adjusting for the quality of the primary articles, the housing–adherence association was just slightly larger in the quality effects model.
Second, most of the studies relied on purposive sampling methods. Participants were recruited from clinical sites, social service agencies, and targeted community outreach, using brochures, posters, media advertisements, staff contacts, referrals, clinic lists, and snowball methods. Other participants were obtained through ongoing cohort studies, Centers for Disease Control and Prevention and local public health surveillance systems, and jail detainee screenings (Table 1). Although it is impossible to establish that the samples combined in the meta-analysis are statistically representative of the population of HIV-positive individuals engaged in ARV therapy in the United States, where good lists were unavailable, the primary studies chose sensible alternatives to probability sampling and, in the aggregate, they cover a broad spectrum of housing statuses.
Third, there is currently no “gold standard” of measurement for either housing stability or medication adherence.26,27 In each of the primary studies, the operational definition of housing stability had just 2 categories. Although the definitions had face validity, it is possible that with more highly developed instruments housing might have explained a larger percentage of the adherence variance and provided a more detailed understanding of the housing–adherence relationship. Regarding measuring ART adherence, 3 of the 10 primary studies used objective measures (microelectronic monitors and unannounced pill counts) and 7 relied exclusively on self-report instruments. The concurrent and predictive validity of self-report instruments have been well established. Still, field testing has shown that question wording and response options may not be consistently understood or applied by all respondents.28 In addition, self-reported adherence measures are susceptible to recall and social desirability bias.29
Fourth, our meta-analysis combined primary studies that differed in research design (eg, longitudinal and cross-sectional designs, multisite and single site, large samples and small). Because variability in the study design is to be expected in any meta-analysis and is present to a greater degree when the primary studies are observational rather than randomized controlled trials, our results should be interpreted cautiously. Likewise, it is necessary to acknowledge the limitations of the primary literature and the need for more exacting research designs. We suggest that future research would benefit from appropriately powered, prospective cohort studies with longer follow-up periods. To closely map changes in housing and adherence over time, plans should include more fine-grained measures of housing status and objective measures of adherence.
Previous research has shown that at each stage in the continuum of HIV care, stable housing makes a difference,23,24 with the largest effects probably found in the earlier stages.25 For those in care and in ARV therapy, the evidence of this study indicates that patients with stable housing tend to adhere better than those without, but the difference is small. The finding challenges the view that unstable housing is incompatible with adherence and questions the potential benefit of deferring ART initiation until the patient's housing circumstances are improved. The treatment guidelines of the U.S. Department of Health and Human Services30 urge clinicians to address areas known to impair adherence—homelessness and unstable housing, among them—before (and after) the initiation of therapy. Given the results of the meta-analysis, the recommendation that ties ART readiness to housing should be reconsidered.
ACKNOWLEDGMENTS
The authors wish to thank Aurelia Minuti, MLS, Head of Reference and Educational Services, D. Samuel Gottesman Library, Albert Einstein College of Medicine, for her generous assistance in conducting the literature searches.
Footnotes
Presented at the 11th International Conference on HIV Treatment and Prevention Adherence, May 9–11, 2016, Fort Lauderdale, FL.
The authors have no funding or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Bangsberg DR. Preventing HIV antiretroviral resistance through better monitoring of treatment adherence. J Infect Dis. 2008;197(suppl 3):S272–S278. [DOI] [PubMed] [Google Scholar]
- 2.Saghayam SL, Wanke C. The impact of nutritional status and nutrition supplementation on outcomes along the HIV treatment cascade in the resource-limited setting. Curr Opin HIV AIDS. 2015;10:472–476. [DOI] [PubMed] [Google Scholar]
- 3.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an international association of physicians in AIDS Care Panel. Ann Intern Med. 2012;156:817–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aidala AA, Sumartojo E. Why housing? AIDS Behav. 2007;11:S1–S6. [DOI] [PubMed] [Google Scholar]
- 6.Berg KM, Demas PA, Howard AA, et al. Gender differences in factors associated with adherence to antiretroviral therapy. J Gen Inter Med. 2004;19:1111–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson MO, Catz SL, Remien RH, et al. Theory-guided, empirically supported avenues for intervention on HIV medication nonadherence: findings from the healthy living project. AIDS Patient care and STDS. 2003;17:645–656. [DOI] [PubMed] [Google Scholar]
- 8.Kidder DP, Wolitski RJ, Campsmith ML, et al. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97:2238–2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Surratt HL, Kurtz SP, O'Grady CE. Serious Mental Illness and Treatment Adherence Among Vulnerable HIV-Positive Women. Poster Presented at: the 5th World Congress on Women’s Mental Health; March 4–7, 2013; Lima, Peru.
- 10.Chen NE, Meyer JP, Avery AK, et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS Behav. 2013;17:2654–2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delavega E, Lennon-Dearing R. Differences in housing, health, and well-being among HIV-positive women living in poverty. Soc Work Public Health. 2015;30:294–311. [DOI] [PubMed] [Google Scholar]
- 12.Kalichman S, Kalichman MO, Cherry C. Medication beliefs and structural barriers to treatment adherence among people living with HIV infection. Psychol Health. 2016;31:383–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moss AR, Hahn JA, Perry S, et al. Adherence to highly active antiretroviral therapy in the homeless population in San Francisco: a prospective study. Clin Infect Dis. 2004;39:1190–1198. [DOI] [PubMed] [Google Scholar]
- 14.Royal SW, Kidder DP, Patrabansh S, et al. Factors associated with adherence to highly active antiretroviral therapy in homeless or unstably housed adults living with HIV. AIDS Care. 2009;21:448–455. [DOI] [PubMed] [Google Scholar]
- 15.Waldrop-Valverde D, Valverde E. Homelessness and psychological distress as contributors to antiretroviral nonadherence in HIV-positive injecting drug users. AIDS Patient Care and STDS. 2005;19:326–334. [DOI] [PubMed] [Google Scholar]
- 16.Morton SC, Costlow MR, Graff JS, et al. Standards and guidelines for observational studies: quality is in the eye of the beholder. J Clin Epidemiol. 2016;71:3–10. [DOI] [PubMed] [Google Scholar]
- 17.Whitehead A, Bailey A, Elbourne D. Combining summaries of binary outcomes with those of continuous outcomes in a meta-analysis. J Biopharm Stat. 1999;9:1–16. [DOI] [PubMed] [Google Scholar]
- 18.Hedges LV. Statistical considerations. In: Cooper H, Hedges LV, eds. The Handbook of Research Synthesis. New York, NY: Russell Sage Foundation, 1994. [Google Scholar]
- 19.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. [DOI] [PubMed] [Google Scholar]
- 20.Doi SAR, Thalib L. A quality-effects model for meta-analysis. Epidemiology. 2008;19:94–100. [DOI] [PubMed] [Google Scholar]
- 21.Doi SAR, Barendregt JJ, Khan S, et al. Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp Clin Trials. 2015;45:123–129. [DOI] [PubMed] [Google Scholar]
- 22.Bangsberg DR, Ragland K, Monk A, et al. A single tablet regimen is associated with higher adherence and viral suppression than multiple tablet regimens in HIV+ homeless and marginally housed people. AIDS. 2010;24:2835–2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aidala AA, Wilson MG, Shubert V, et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health. 2016;106:e1–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leaver CA, Bargh G, Dunn JR, et al. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6 suppl):85–100. [DOI] [PubMed] [Google Scholar]
- 25.Milloy MJ, Marshall BDL, Montaner J, et al. Housing status and the health of people living with HIV/AIDS. Curr HIV/AIDS Rep. 2012;9:364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frederick TJ, Chwalek Michal, Hughes Jean, et al. How stable is stable? Defining and measuring housing stability. J Community Psychol. 2014; 42:964–979. [Google Scholar]
- 27.Chesney MA. The elusive gold standard. Future perspectives for HIV adherence assessment and intervention. J Acquir Immune Defic Syndr. 2006;43(suppl 1):S149–S155. [DOI] [PubMed] [Google Scholar]
- 28.Wilson IB, Fowler FJ, Cosenza CA, et al. Cognitive and field Testing of a new set of medication adherence self-report items for HIV care. AIDS Behav. 2014;18:2349–2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams AB, Amico KR, Bova C, et al. A proposal for quality standards for measuring medication adherence in research. AIDS Behav. 2013;17:284–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services; Available at http://www.aidsinfo.nih.gov/ContentFiles/Adul-%20tandAdolescentGL.pdf. Accessed September 14, 2016. [Google Scholar]


