Abstract
Temporomandibular joint replacement (TJR) with alloplastic prosthesis has shown promising long-term results in end stage joint disorders. We present a case of young woman with painful ankylosis that where reconstructed with TJR, due to a complex mandibular fracture with dislocation of the left condyle into the middle cranial fossa two years earlier. At the age of 18 the subject underwent a total joint replacement with custom-made alloplastic TMJ prosthesis. To determine the bone response and remodeling activity around the prosthesis, a F18 PET/CT-scan was used. No sign of increased remodeling or pathology were seen in the imaging after the reconstruction. Four years postoperatively the subject reports no pain and excellent jaw function.
Keywords: temporomandibular joint (TMJ), trauma, dislocated condyle, middle cranial fossa, ankylosis, alloplastic prosthesis
Mandibular condyle fractures account for ∼30% of all mandibular fractures.1 2 A rare event is when the mandibular condyle penetrates and dislocates into the middle cranial fossa.3 4 5 6 The first reported case in the English literature, was described by Dingman and Grabb in 1963.7 The injury is more commonly seen in the pediatric population due to anatomical conditions.4 8 9 Fonseca showed that a small rounded condyle, as in younger individuals, have a greater potential to penetrate the, relatively thin glenoid fossa, than a full-grown condyle.9
Fractures of both the mandibular condyle and the glenoid fossa on the temporal bone can result in ankylosis of the temporomandibular joint (TMJ), although the etiology of the development of ankylosis is still unknown.10 Trauma is the main cause of TMJ ankylosis with infections, rheumatoid arthritis and psoriasis as other etiological factors.11 12
The optimal treatment for this condition is still debated as both surgical interventions such as gap arthroplasty, costochondral grafts and total joint reconstruction with alloplastic materials, and pharmaceutical methods has been proposed for treatment of traumatic TMJ ankylosis.12 13
Report of a Case
The subject, a 15-year-old girl, was reported to her local hospital following a severe trauma to the chin. She had fainted at home and hit her chin against the bathroom sink. Upon presentation to the emergency room the subject showed a lateral open bite with no sign of neurological deficit and underwent a computed tomography scan (CT). The examination revealed a mandibular symphysis fracture as well as a bilateral condyle fracture with displacement of the left condyle into to the middle cranial fossa (Fig. 1). The subject was then, after neurosurgical consultation, referred to the Department of Oral and Maxillofacial surgery, Uppsala university hospital. With the subject under general anesthesia, the symphysis fracture was reduced and fixated and a closed attempt to non-surgically reduce the dislocated and fractured left condyle was made. Mandibulomaxillary fixation (MMF) was postoperatively kept for two weeks. The postoperative period was uneventful with no neurological complications observed. After release of MMF, early mobilization and physiotherapy was introduced to reduce the risk of ankylosis. A second surgery was performed to remove the fixation plate at the site of the symphysis fracture to reduce the risk of growth disturbances. Follow-up was undertaken at the Oral and maxillofacial department of her local hospital.
Fig. 1.
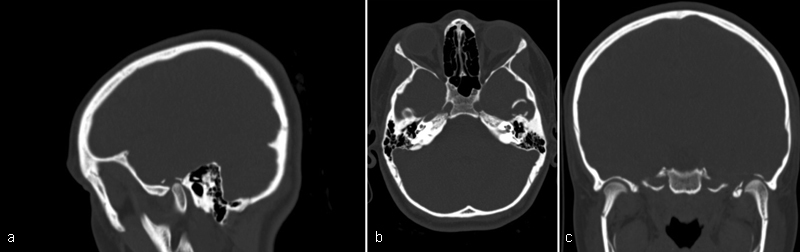
(a,b,c) Coronal, sagittal and axial view of CT-scan showing the left mandibular condyle dislocated into the middle cranial fossa.
The subject was initially free from symptoms but after two years started to notice reduced jaw function with restriction in maximal mouth opening and increasing constant pain from the left TMJ area. Three years after the first visit to the Department of Oral and Maxillofacial surgery in Uppsala, she was again referred back due to incipient painful (VAS 8) ankylosis of the left TMJ. The maximum opening of the jaw was 20 mm, with a deviation of the jaw to the left. A CT scan revealed a progressive ankylosis of the left TMJ (Fig. 2). At the age of 18, a total joint reconstruction (TJR) was decided upon using a custom-made alloplastic TMJ prosthesis (Biomet® Microfixation, Jacksonville, FL) on her left side.
Fig. 2.

(a,b) Coronal and sagittal view of CBCT-scan, showing fibrous ankylosis of the left mandibular condyle to the earlier fractured glenoid fossa.
Surgical Technique
The total joint reconstruction was performed with the subject under general anesthesia. Prophylactic antibiotic, Cloxacillin 2 g × 3, was administered intravenously. Through two surgical approaches, preauricular and retromandibular incisions, the mandibular condyle and ramus were exposed. The condylar head and fossa displayed substantial bone remodelling with adherences (Fig. 3). Resection of the condylar head and coronoid process was then performed with the custom-made cutting guides (Medical Modelling Inc., Golden, CO) in place using a piezo-electric micromovement bone osteotomies with inserts of a microsaw (Mectron Piezosurgery®, Blade OT7, Carasco, Italy) (Fig. 4). After establishing MMF with screws, the individualized templates were tried out and minor corrections were made to finally insert the custom-made fossa and ramus prosthesis (Fig. 5). Fixation of both parts was performed with specified screw lengths according to the pre-surgical virtual plan. After release of MMF the mandible was manipulated to ensure proper matching of the fossa and ramus components. A subdermal multilayer closure was accomplished with resorbable sutures and the skin was sutured with non-resorbable sutures. The external ear canal was inspected directly after closure with no signs of perforation.
Fig. 3.
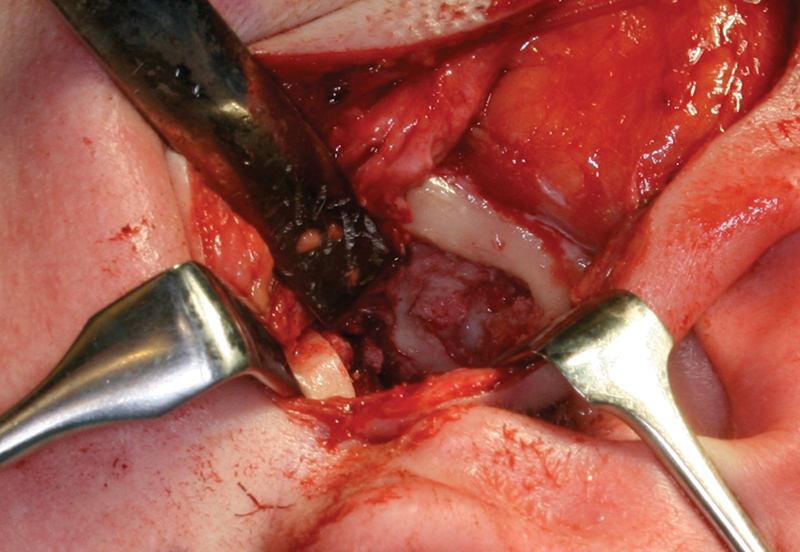
Temporomandibular fossa after resection of the ankylosed condyle.
Fig. 4.

Resected condylar head and coronoid process.
Fig. 5.
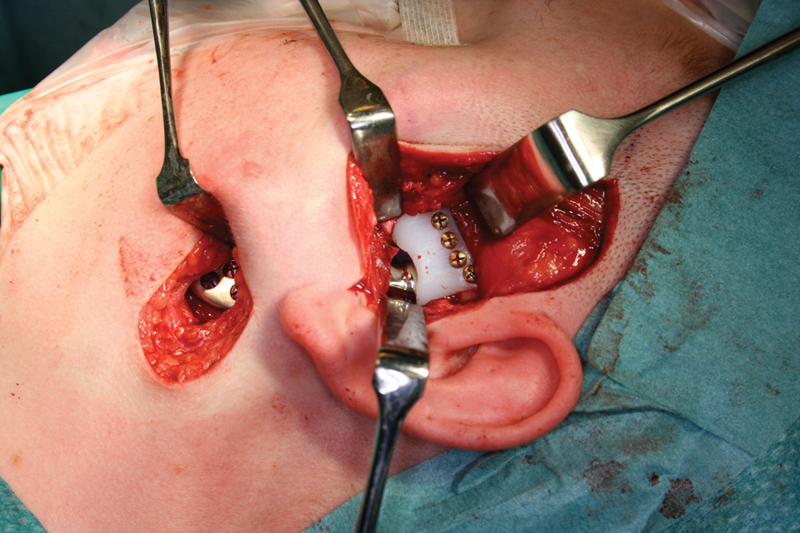
TMJ Prosthesis, ramus and fossa component, installed through the preauricular and retromandibular approaches.
One week after the TJR, maximal mouth opening was 30 mm and physical rehabilitation of the TMJ was initiated with TheraBite® Jaw Motion Rehabilitation System™ (Hörby, Sweden). The subject was on a normal diet without restrictions. The facial mimic was intact postoperatively. At her 6-week follow-up visit, she was eating normally, with a maximal mouth opening of 36 mm without pain. Four months postoperatively, she had gained another 4 mm up to a total of 40mm. At the 1-year follow-up after TJR, a CBCT-scan was performed and at the second year follow-up an F18 PET-CT with no signs of pathology (Figs. 6 and 7a, b) with the 40 mm mouth opening intact (Fig. 8). At 4-year follow up her mouth opening had increased to 44 mm. Epilepsy was diagnosed post surgery at her local hospital and medication was used for one year. It has now been discontinued for two years and the patient has since then been disease free.
Fig. 6.
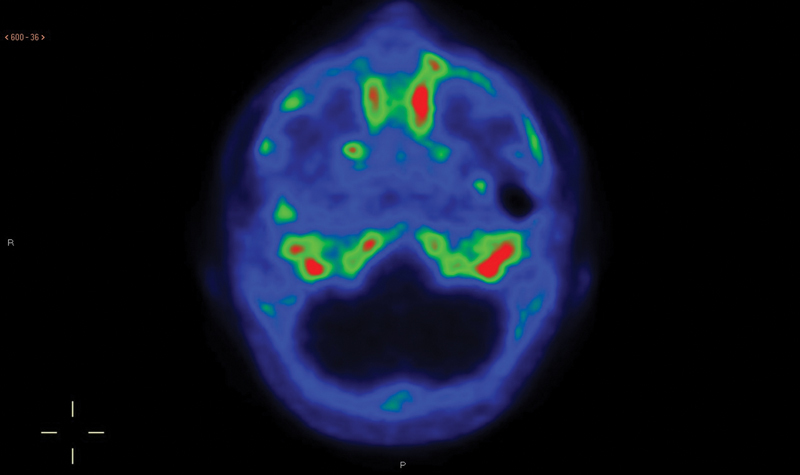
PET-CT with F18 to control the remodelling of the bone. No signs of recurrence of the ankylosis were seen. F18-PET-scan showing normal bone formation around the prosthetic materials and no signs of pathological conditions in terms of re-ankylosis.
Fig. 7.
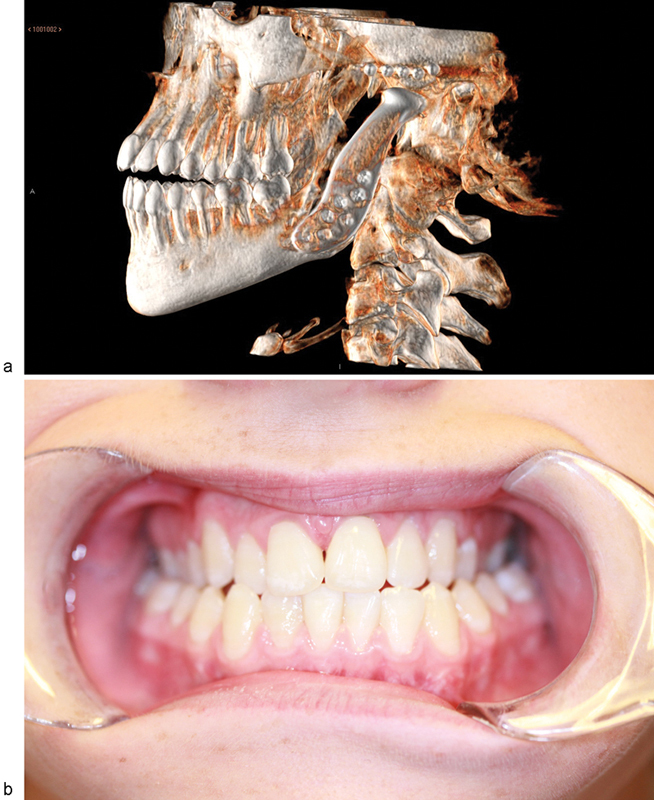
(a,b) 3D CT-reconstruction of the reconstructed TMJ. Nota bene: the fossa component is not radiopaque. The patient has had a stable bilateral cross bite since childhood, with no need for treatment.
Fig. 8.

Mouth opening 4 month postoperatively with 40mm maximal opening.
Discussion
Dislocation of the mandibular condyle to the mid-cranial fossa is a rare event, with 66 cases, the present case included, reported in the literature.4 5 14 15 16 17 18 19 20 21 22 23 Rosa et al reported 55 cases using Medline and PubMed search engines between 1960 and 2005. Between 2005 and 2014, 11 new cases were reported according to our PubMed search. The majority of the patients were female with a 2:1 ratio. To our knowledge, this case is the first involving reconstruction with an alloplastic TMJ prosthesis.
As for all trauma to the TMJ, early mobilization is of great importance to prevent the development of ankylosis. In only three cases of all of the above, ankylosis is described as a late complication to the initial trauma after two to five years of follow-up.24 Although the pathogenesis of TMJ ankylosis is not fully understood, prevention may be undertaken such as active jaw opening exercises. Some authors recommend fat grafts when performing TMJ reconstruction, to reduce dead space and serving as a physical barrier between the condyle and fossa. The scientific evidence for this procedure is however debated.11 25 In the present case, early jaw exercise was the only prevention of reankylosis introduced after the TMJ reconstruction.
In the present case, the subject was placed in MMF for two weeks and then mobilized, as recommended, according to a suggested management protocol.26 Despite this, three years after the trauma the subject developed ankylosis of the affected TMJ. This was confirmed by a CBCT-scan two years after the trauma (Fig. 3).
To analyze the metabolic bone response to the prosthetic implant, we used fluoride-positron emission CT (F18 PET/CT) which earlier has shown promising results in studies of un-cemented stems following total hip arthroplasty (THA).27 A PET/CT-scan with F18, as presented in this report, may function as a new modality illustrating the bone remodelling activity of osteoblasts and thus function as a control modality in the event of re-ankylosis. However, in this case there were no signs of pathological activity after total joint reconstruction.
Total joint reconstruction with alloplastic prosthesis is a well-known treatment in end stage TMJ disorders. Promising results have shown that reconstructive procedures with TMJ prosthesis are a stable and functional treatment with good prognosis.
TMJ ankylosis after dislocation of the condyle into the cranial fossa is a demanding condition. Different treatments have been suggested, but in our opinion, the alloplastic prosthesis may be the preferred treatment of post-traumatic TMJ ankylosis. The use of a polyethylene mandibular fossa and a Co/Cr condyle and ramus part, with a titanium plasma sprayed surface connecting to the mandibular bone, is according to orthopaedic principles.
The lifespan of a joint replacement is dependent on factors such as anatomical conditions, functional loading, stability, materials and design. In comparison with total hip arthroplasties, using the same biomaterials, the 15-year survival rate in the Nordic countries is between 84–88% years.28 The functional load of biting forces is significantly lower and the design of the TMJ prosthesis is different which makes the comparison inadequate in some aspects, such as material fatigue and wear. Long-term results of TMJ prosthesis durability are increasing and show promising data and jaw function and quality of life.29 30
Conclusion
Dislocation of the mandibular condyle into the middle cranial fossa is a rare event with few cases reported in the literature. Our subject sustained a progressive and painful ankylosis of her left condyle and fossa three years after her initial trauma. The ankylosis was resolved by an intervention including resection of the dislocated mandibular condyle and TJR, with a custom made alloplastic prosthesis for the fossa and condyle. F18 PET/CT-scan was used for investigating a normal bone remodelling and resulted in no signs of pathology two years postoperatively. A normalization regarding pain and function was established and the patient displayed good function with 44 mm mouth opening four years post-operatively.
References
- 1.Lee K H. Epidemiology of mandibular fractures in a tertiary trauma centre. Emerg Med J. 2008;25(9):565–568. doi: 10.1136/emj.2007.055236. [DOI] [PubMed] [Google Scholar]
- 2.de Matos F P, Arnez M F, Sverzut C E, Trivellato A E. A retrospective study of mandibular fracture in a 40-month period. Int J Oral Maxillofac Surg. 2010;39(1):10–15. doi: 10.1016/j.ijom.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Bu S S, Jin S L, Yin L. Superolateral dislocation of the intact mandibular condyle into the temporal fossa: review of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(2):185–189. doi: 10.1016/j.tripleo.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 4.Cillo J E, Sinn D P, Ellis E III. Traumatic dislocation of the mandibular condyle into the middle cranial fossa treated with immediate reconstruction: a case report. J Oral Maxillofac Surg. 2005;63(6):859–865. doi: 10.1016/j.joms.2005.02.029. [DOI] [PubMed] [Google Scholar]
- 5.Harstall R, Gratz K W, Zwahlen R A. Mandibular condyle dislocation into the middle cranial fossa: a case report and review of literature. J Trauma. 2005;59(6):1495–1503. doi: 10.1097/01.ta.0000199241.49446.80. [DOI] [PubMed] [Google Scholar]
- 6.He Y, Zhang Y, Li Z L, An J G, Yi Z Q, Bao S D. Treatment of traumatic dislocation of the mandibular condyle into the cranial fossa: development of a probable treatment algorithm. Int J Oral Maxillofac Surg. 2015;44(7):864–870. doi: 10.1016/j.ijom.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 7.Dingman R O, Grabb W C. Mandibular laterognathism. Plast Reconstr Surg. 1963;31:563–575. doi: 10.1097/00006534-196306000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Gladwell M, Viozzi C. Temporal bone fractures: a review for the oral and maxillofacial surgeon. J Oral Maxillofac Surg. 2008;66(3):513–522. doi: 10.1016/j.joms.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 9.da Fonseca G D. Experimental study on fractures of the mandibular condylar process (mandibular condylar process fractures) Int J Oral Surg. 1974;3(3):89–101. doi: 10.1016/s0300-9785(74)80040-2. [DOI] [PubMed] [Google Scholar]
- 10.He D, Ellis E III, Zhang Y. Etiology of temporomandibular joint ankylosis secondary to condylar fractures: the role of concomitant mandibular fractures. J Oral Maxillofac Surg. 2008;66(1):77–84. doi: 10.1016/j.joms.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Yan Y B, Liang S X, Shen J, Zhang J C, Zhang Y. Current concepts in the pathogenesis of traumatic temporomandibular joint ankylosis. Head Face Med. 2014;10:35. doi: 10.1186/1746-160X-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jayavelu P, Shrutha S P, Vinit G B. Temperomandibular joint ankylosis in children. J Pharm Bioallied Sci. 2014;6 01:S178–S181. doi: 10.4103/0975-7406.137450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ebrahimi A, Ashford B G. Advances in temporomandibular joint reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2010;18(4):255–260. doi: 10.1097/MOO.0b013e32833af88c. [DOI] [PubMed] [Google Scholar]
- 14.Ohura N, Ichioka S, Sudo T, Nakagawa M, Kumaido K, Nakatsuka T. Dislocation of the bilateral mandibular condyle into the middle cranial fossa: review of the literature and clinical experience. J Oral Maxillofac Surg. 2006;64(7):1165–1172. doi: 10.1016/j.joms.2006.03.043. [DOI] [PubMed] [Google Scholar]
- 15.Clauser L, Tieghi R, Polito J, Galiè M. Dislocation of the mandibular condyle into the middle cranial fossa. J Craniofac Surg. 2006;17(3):590–594. doi: 10.1097/00001665-200605000-00036. [DOI] [PubMed] [Google Scholar]
- 16.Rosa V L, Guimarães A S, Marie S K. Intrusion of the mandibular condyle into the middle cranial fossa: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(1):e4–e7. doi: 10.1016/j.tripleo.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 17.Magge S N Chen H I Heuer G G Carrasco L R Storm P B; Department of Neurosurgery. Dislocation of the mandible into the middle cranial fossa. Case report J Neurosurg 2007107(1, Suppl)75–78. [DOI] [PubMed] [Google Scholar]
- 18.Taglialatela Scafati C, Aliberti F, Scotto di Clemente S, Taglialatela Scafati S, Facciuto E, Cinalli G. Dislocation of a fractured mandibular condyle into the middle cranial fossa: a case treated by an extracranial approach. Childs Nerv Syst. 2008;24(9):1067–1070. doi: 10.1007/s00381-008-0659-8. [DOI] [PubMed] [Google Scholar]
- 19.Lloyd T E, Sivarajasingam V. An unusual cranial dislocation of the mandibular condyle. Br J Oral Maxillofac Surg. 2010;48(3):176–177. doi: 10.1016/j.bjoms.2009.08.031. [DOI] [PubMed] [Google Scholar]
- 20.Struewer J, Kiriazidis I, Figiel J, Dukatz T, Frangen T, Ziring E. Dislocation of the mandibular condyle into the middle cranial fossa causing an epidural haematoma. J Craniomaxillofac Surg. 2012;40(5):396–399. doi: 10.1016/j.jcms.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Man C, Zhu S S, Chen S, Jiang L, Hu J. Dislocation of the intact mandibular condyle into the middle cranial fossa: a case report. Int J Oral Maxillofac Surg. 2011;40(1):118–120. doi: 10.1016/j.ijom.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 22.Oberman B, Setabutr D, Goldenberg D. Traumatic dislocation of intact mandibular condyle into middle cranial fossa. Am J Otolaryngol. 2014;35(2):251–253. doi: 10.1016/j.amjoto.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Zhang S, Wu J, Xu B, Shi J, Shen S G, Gui H. Features and management of intracranial mandibular condyle dislocation after trauma. Cranio. 2014;32(1):63–67. doi: 10.1179/0886963413Z.0000000007. [DOI] [PubMed] [Google Scholar]
- 24.van der Linden W J. Dislocation of the mandibular condyle into the middle cranial fossa: report of a case with 5 year CT follow-up. Int J Oral Maxillofac Surg. 2003;32(2):215–218. doi: 10.1054/ijom.2002.0319. [DOI] [PubMed] [Google Scholar]
- 25.Wolford L M Morales-Ryan C A Morales P G Cassano D S Autologous fat grafts placed around temporomandibular joint total joint prostheses to prevent heterotopic bone formation Proc (Bayl Univ Med Cent) 2008213248–254. (Bayl Univ Med Cent) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koretsch L J, Brook A L, Kader A, Eisig S B. Traumatic dislocation of the mandibular condyle into the middle cranial fossa: report of a case, review of the literature, and a proposal management protocol. J Oral Maxillofac Surg. 2001;59(1):88–94. doi: 10.1053/joms.2001.19301. [DOI] [PubMed] [Google Scholar]
- 27.Ullmark G, Nilsson O, Maripuu E, Sörensen J. Analysis of bone mineralization on uncemented femoral stems by [18F]-fluoride-PET: a randomized clinical study of 16 hips in 8 patients. Acta Orthop. 2013;84(2):138–144. doi: 10.3109/17453674.2013.786632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mäkelä K T, Matilainen M, Pulkkinen P. et al. Countrywise results of total hip replacement. An analysis of 438,733 hips based on the Nordic Arthroplasty Register Association database. Acta Orthop. 2014;85(2):107–116. doi: 10.3109/17453674.2014.893498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolford L M, Mercuri L G, Schneiderman E D, Movahed R, Allen W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg. 2015;73(5):952–960. doi: 10.1016/j.joms.2014.10.032. [DOI] [PubMed] [Google Scholar]
- 30.Mercuri L G, Edibam N R, Giobbie-Hurder A. Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg. 2007;65(6):1140–1148. doi: 10.1016/j.joms.2006.10.006. [DOI] [PubMed] [Google Scholar]


