Abstract
Meiotic progression in mammalian preovulatory follicles is controlled by the granulosa cells around the oocyte. Cyclic GMP (cGMP) generated in the granulosa cells diffuses through gap junctions into the oocyte, maintaining meiotic prophase arrest. Luteinizing hormone then acts on receptors in outer granulosa cells to rapidly decrease cGMP. This occurs by two complementary pathways: cGMP production is decreased by dephosphorylation and inactivation of the NPR2 guanylyl cyclase, and cGMP hydrolysis is increased by activation of the PDE5 phosphodiesterase. The cGMP decrease in the granulosa cells results in rapid cGMP diffusion out of the oocyte, initiating meiotic resumption. Additional, more slowly developing mechanisms involving paracrine signaling by extracellular peptides (C-type natriuretic peptide and EGF receptor ligands) maintain the low level of cGMP in the oocyte. These coordinated signaling pathways ensure a fail-safe system to prepare the oocyte for fertilization and reproductive success.
Keywords: oocyte meiosis, ovarian follicle, luteinizing hormone, intercellular communication, cyclic GMP, gap junctions
INTRODUCTION
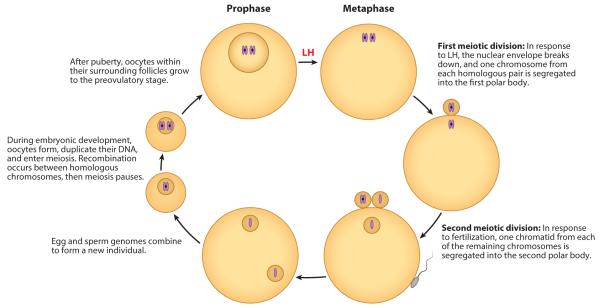
Meiosis, which reduces the number of homologous chromosomes from two to one, allows egg and sperm genomes to combine at fertilization. In mammalian oocytes, meiosis starts during embryogenesis and concludes at fertilization, months later in mice, and years later in humans (1). The oocyte’s DNA duplicates, and recombination occurs between homologous chromosomes (Figure 1). Meiosis then pauses at the early stage, which is characterized by an intact nuclear envelope and nucleolus as well as partially condensed chromatin. Oocytes remain in this state until after puberty, when during each reproductive cycle, follicles grow to the preovulatory stage and are then stimulated by luteinizing hormone (LH) from the pituitary, which acts on the outer granulosa cells to restart meiosis. LH signaling also causes ovulation, releasing the oocyte from its follicle such that it can enter the oviduct where fertilization occurs.
Figure 1.
Life cycle of a mammalian oocyte. The diagram places the prophase-to-metaphase transition in response to luteinizing hormone (LH) into the context of the overall meiotic cell cycle of the oocyte. One set of homologous chromosomes, each composed of two chromatids (purple), is shown.
This review discusses the remarkable regulatory system in mammalian preovulatory follicles that maintains meiotic prophase arrrest and how this system is reversed by LH to cause meiosis to resume. Both events, maintaining arrest and restarting meiosis, involve signaling from granulosa cells to the oocyte through gap junctions and the extracellular space. Signaling within the oocyte was reviewed elsewhere (1–5) and is considered only briefly here.
OVARIAN FOLLICLE STRUCTURE
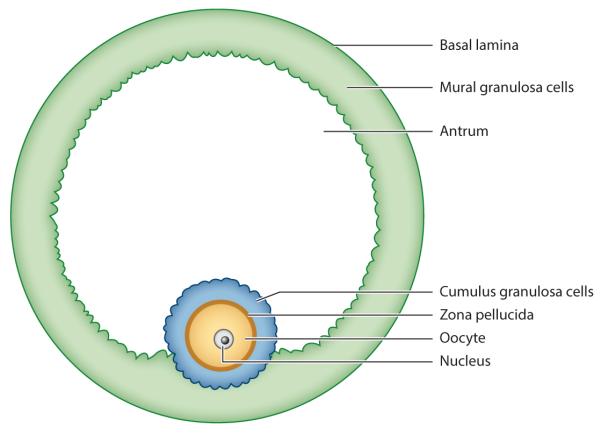
Ovaries contain follicles of various sizes. The smallest follicles, called primordial, consist of a single layer of granulosa cells around the oocyte. The largest follicles, called preovulatory or Graafian, consist of approximately 2–3 layers of inner granulosa cells, called cumulus cells, and approximately 5–10 outer layers of cells called mural granulosa cells (Figure 2). Gap junctions connect all of the granulosa cells in a functional syncytium, and the cumulus cells also form gap junctions with the oocyte (see 6). The cumulus cells are attached to one region of the mural layer, but elsewhere the two types of granulosa cells are separated by a space called the antrum, filled with follicular fluid. The cumulus cells form a pseudostratified epithelium, with cells from the first, second, and even third layers extending processes through the extracellular coat of the oocyte, the zona pellucida (7). These processes form gap junctions with the oocyte (8), comprised primarily of connexin 37 (6, 9, 10), although some contribution of connexin 43 from the cumulus cells is possible (11, 12). Elsewhere in the follicle, the gap junctions are composed of primarily connexin 43 (6, 9, 10). The localization of these connexins and some of the other signaling proteins that regulate meiotic arrest and resumption in preovulatory follicles is shown schematically in Figure 3.
Figure 2.
Tissue layers of a mammalian preovulatory follicle. The oocyte with its prophase-arrested nucleus is surrounded by 2–3 layers of cumulus granulosa cells, which are attached in one region to the 5–10 layers of mural granulosa cells. Elsewhere, a fluid-filled antrum separates the two types of granulosa cells.
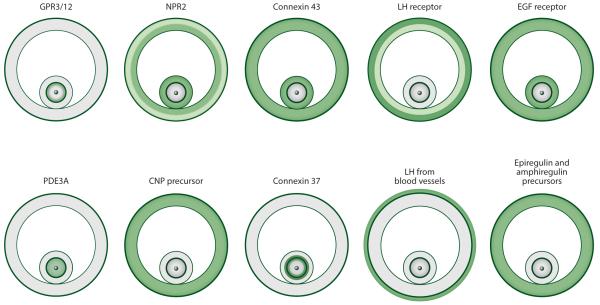
Figure 3.
Localization of some of the signaling proteins that regulate meiotic arrest and resumption in preovulatory follicles. Protein distribution is either determined directly, by ligand binding, immunofluorescence, or Western blotting; or it is inferred from mRNA distribution, by in situ hybridization, or from RT-qPCR. Green indicates the presence of the protein, and lighter green indicates a lesser amount of the protein. White indicates that the protein (or mRNA) was either not detected or detected at a level ≤10% of that elsewhere. Figure is based on data from the following references: CNP precursor (66); connexin 43 (9), connexin 37 (9), EGF receptor (99; LA Jaffe and JR Egbert, unpublished data); epiregulin and amphiregulin precursors (99); GPR3/12 (40, 46); LH from blood vessels (14); LH receptor (84); NPR2 (66, 70); and PDE3A (61, which used a previous nomenclature, PDE3B). Abbreviations: CNP, C-type natriuretic peptide; EGF, epidermal growth factor; LH, luteinizing hormone; NPR2, natriuretic peptide receptor 2; PDE3A, phosphodiesterase 3A.
The outer layers of mural granulosa cells form another pseudostratified epithelium, extending processes to the extracellular matrix forming the basal lamina (13, 14). These processes may facilitate communication with the theca cells and blood vessels outside of the basal lamina, although gap junctions do not form connections across the basal lamina. The theca cells initiate the production of steroids important for follicle development, and the blood vessels, along with their many other functions, deliver LH from the pituitary (Figure 3). We use the term follicle to include just the granulosa cells and oocyte, although it is sometimes used to include the theca as well. Figure 4 shows a photograph of a mouse preovulatory follicle (and a schematic diagram of its cellular structure is illustrated later in Figure 5).
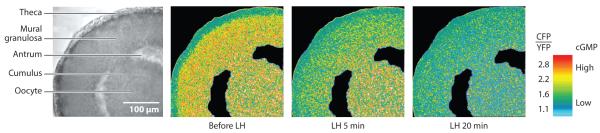
Figure 4.
LH-induced cGMP decreases in a mouse ovarian follicle from a transgenic mouse expressing the cGMP FRET sensor cGi500. A larger CFP/YFP emission ratio indicates higher cGMP. Ratios are color-coded: Yellow indicates high cGMP, and turquoise indicates low cGMP. Before LH perfusion, cGMP is high throughout the follicle but low in the theca cells. At 5 min after LH perfusion, cGMP has decreased in the mural cells but not in the cumulus cells or oocyte. At 20 min, cGMP has decreased throughout the follicle. Figure modified from Reference 71. Abbreviations: CFP, cyan fluorescent protein; cGMP, cyclic GMP; FRET, Förster resonance energy transfer; LH, Luteinizing hormone; YFP, yellow fluorescent protein.
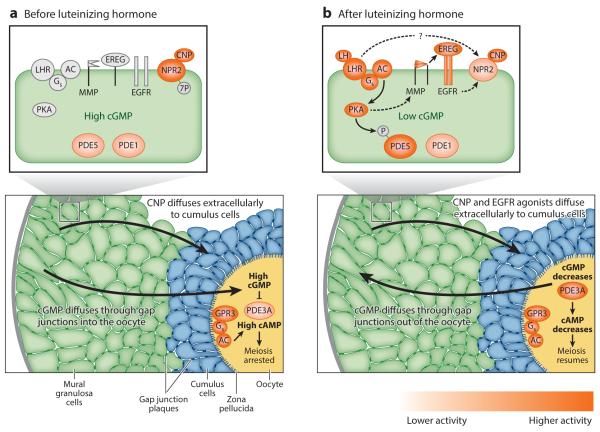
Figure 5.
Working model of signaling pathways that regulate meiotic arrest and resumption in preovulatory follicles. Panel a shows a follicle and an expanded view of a mural granulosa cell before LH exposure. Panel b depicts events occurring in response to LH. Some of the slower events are not shown, such as the decrease in CNP and the increase in mRNA encoding epiregulin and amphiregulin. Higher levels of enzymatic activity are depicted by darker shades of orange. Abbreviations: AC, adenylyl cyclase; CNP, C-type natriuretic peptide; EGFR, epidermal growth factor receptor; EREG, epiregulin (and amphiregulin); GPR3, G-protein receptor 3; Gs, Gs G protein; LH, luteinizing hormone; LHR, luteinizing hormone receptor; MMP, matrix metalloprotease; NPR2, natriuretic peptide receptor 2; PDE1, 3A, 5, phosphodiesterases; PKA, protein kinase A. Figure modified from Reference 71, with additional details about the phosphodiesterases from Reference 109. The cellular structures were drawn based on electron microscopic images of a mouse follicle from Valentina Baena and Mark Terasaki.
Among mammals, the size of the preovulatory follicle is proportional to the size of the animal, ranging in diameter from approximately 400 μm in a mouse to more than 10 cm in a rhinoceros (15). The diameter of a human preovulatory follicle is approximately 2 cm. This proportionality probably arises because larger animals need more estrogen, which comes from the follicle. The number of cell layers lining the basal lamina and surrounding the oocyte is similar across species; follicle size variation is due to differences in the size of the antrum. The diameter of the oocyte in preovulatory follicles varies little among different species, ranging from ~70 to ~120 μm (16).
The prophase-arrested oocyte contains a large nucleus, also known as a germinal vesicle, with a prominent nucleolus. The first obvious sign of meiotic resumption in response to LH is the breakdown of the nuclear envelope and disappearance of the nucleolus. In mice, this begins ~2–3 h after LH exposure, and the first meiotic division occurs at ~10–12 h (17). In larger animals, the time between LH receptor activation and nuclear envelope breakdown is longer (18), ~18 h in women, based on the limited information that is available (19).
During the first meiotic division, one set of chromosomes is discarded in a tiny cell called a polar body, leaving the other set in the oocyte (Figure 1). This division reduces the complement of chromosomes remaining in the oocyte from the diploid (2N) to the haploid (N) number. The remaining chromosomes assemble on the second meiotic spindle, but then meiosis pauses again. At this point, the oocyte (now also called an egg), is ovulated from the follicle and enters the oviduct. Meiosis remains arrested at second metaphase until fertilization causes separation of the chromatids and formation of a second polar body. This leaves one copy of each oocyte-derived gene in the egg, such that the egg genome can combine with the sperm genome to create a new individual.
MEIOTIC PROPHASE ARREST
Dependence of Prophase Arrest in the Preovulatory Follicle on the Mural Granulosa Cells
During the months or years before a follicle reaches the preovulatory stage, prophase arrest is maintained by the oocyte itself and does not rely on signals from the surrounding follicle. In part, this is thought to be due to limiting levels of cyclin-dependent kinase 1 (CDK1, CDC2), which is required for the progression from prophase to metaphase (20–23). When present in sufficient amounts and when activated by dephosphorylation and binding to its cyclin partner, CDK1 is proposed to cause nuclear envelope breakdown by controlling signaling pathways that trigger the disassembly of nuclear lamins (23) and nuclear pores (24). CDK1 activity also causes chromosomes to condense (25).
As the follicle grows to its full size and approaches the preovulatory stage, the oocyte increases its expression of CDK1 as well as other proteins needed to resume meiosis. Nevertheless, the oocyte remains arrested in prophase as long as it resides within the follicle. If the cumulusoocyte complex is removed from a preovulatory follicle, meiosis resumes spontaneously (26). This phenomenon is observed in all mammalian species examined, including humans (27). Within 1–2 h after the isolation of a mouse oocyte or cumulus-oocyte complex, the nuclear envelope breaks down, and meiosis proceeds to second metaphase. The ability of the isolated oocyte to resume meiosis develops gradually as the follicle grows (28).
Meiosis-inhibitory signals from the mural granulosa cells travel to the oocyte both through gap junctions and through the follicular fluid. Gap junction inhibitors such as carbenoxolone cause meiosis to resume in preovulatory follicles (6, 29–31), as do peptides or antibodies that specifically block either connexin 37 or connexin 43 (6, 31). These findings indicate that the transmission of the inhibitory signal from the mural granulosa cells to the oocyte requires gap junctions between the cumulus cells and oocyte (connexin 37), between mural granulosa cells, and between the mural and cumulus cells (connexin 43). Incubating isolated cumulus-enclosed oocytes in follicular fluid also partially inhibits meiotic resumption, indicating the presence of an extracellular inhibitor (32).
Dependence of Prophase Arrest in the Preovulatory Follicle on Cyclic AMP Produced in the Oocyte
Meiotic resumption in isolated oocytes can be suppressed by addition of a membrane permeant, hydrolysis-resistant form of 3′,5′-cyclic AMP (cAMP) (33), or a cAMP phosphodiesterase inhibitor (34). Thus, it was initially thought that meiotic arrest in the follicle might be due to cAMP diffusing from the granulosa cells into the oocyte (35). However, early studies also showed that the oocyte itself could produce cAMP (35). Testing these concepts became possible with the development of techniques for imaging and injecting the oocyte within the intact living follicle (36), allowing investigation of physiological functions that depend on intercellular signaling.
Evidence that the oocyte itself is an essential source of inhibitory cAMP came from experiments showing that inhibition of the Gs G protein in follicle-enclosed oocytes causes meiotic resumption. Gs, which stimulates adenylyl cyclase that converts ATP to cAMP, was inhibited by injection of a function-blocking antibody (36) or a dominant negative form of Gs (37). Because these proteins cannot pass through gap junctions into the granulosa cells, it can be concluded that the oocyte is the original source of cAMP. Furthermore, any cAMP that might enter the oocyte through gap junctions from granulosa cells is insufficient to maintain meiotic arrest. Injection of a Gs-inhibitory antibody and/or dominant negative Gs also causes meiotic resumption in oocytes of fish and frogs (37, 38) and humans (39), indicating that this mechanism is conserved among vertebrate oocytes.
The requirement of Gs for maintaining arrest also suggests that Gs is kept active via a trans-membrane G protein–coupled receptor present in the oocyte. Indeed, this receptor was identified from a list of the G-protein–coupled receptors in a mouse oocyte cDNA library (40). Of the ~1000 potential candidate receptors, only 15 were present in this particular oocyte library, and of these, two were known to activate Gs, the β-adrenergic receptor and the orphan receptor GPR3. This latter receptor was previously characterized as a constitutive activator of Gs (41). Because β-adrenergic agonists do not maintain meiotic arrest in isolated oocytes (LM Mehlmann, LA Jaffe, unpublished data), GPR3 was the prime suspect. Gpr3 mRNA is highly enriched in the mouse oocyte, with levels 10 times greater than detected in surrounding granulosa cells (40) (Figure 3).
Loss of function studies in mice established that GPR3 activates Gs and maintains meiotic arrest in the oocyte, as depicted in Figure 5. Oocytes isolated from Gpr3−/− mice exhibit a loss of Gs activity (42), and meiosis resumes spontaneously in preovulatory follicles of Gpr3−/− mice (40, 43). These phenotypes are rescued by injection of Gpr3 mRNA into follicle-enclosed oocytes (40, 42). Similar to the genetic knockout, knockdown of Gpr3 by siRNA injection into wild type follicle-enclosed oocytes initiates resumption of meiosis (44). GPR3 also maintains meiotic arrest in porcine oocytes (45). In rats, the corresponding and functional receptor is the closely related GPR12 (46). GPR3, but not GPR12, is present in human oocytes, but the function of GPR3 in maintaining meiotic arrest was not tested (39). To date, no endogenous agonists were definitively identified for GPR3 or GPR12, consistent with evidence that these receptors are constitutively active. The GPR3–Gs system produces cAMP in the oocyte by activating adenylyl cyclase AC3 (47).
Targets of cAMP in the Oocyte
Early studies showed that cAMP acts through protein kinase A (PKA) to maintain meiotic arrest (48). Through multiple steps, PKA maintains the CDK1 kinase in an inactive form (4). Although oocytes within preovulatory follicles have sufficient amounts of CDK1 to proceed to metaphase, they remain arrested in prophase, due primarily to phosphorylation of CDK1 on sites that inhibit its activity. PKA phosphorylates and activates the kinase WEE1B that then phosphorylates and inactivates CDK1 (49). PKA also phosphorylates the phosphatase CDC25B that dephosphorylates CDK1. Phosphorylated CDC25B is sequestered in the cytoplasm by the 14-3-3 protein and prevented from entering the nucleus (50, 51). By keeping CDC25B out of the nucleus, cAMP signaling maintains nuclear CDK1 in a phosphorylated and inactive state. In turn, nuclear envelope breakdown and chromosome condensation are unable to proceed. Thus, through the PKA-dependent activation of WEE1B and inhibition of CDC25B, high levels of oocyte cAMP help to limit CDK1 activity and meiotic arrest. Additional PKA substrates may be important as well; in Xenopus oocytes, the PKA substrate ARPP19 was recently identified as an essential regulator of CDK1 activity and meiotic resumption (52).
cAMP also suppresses cytoplasmic changes in the oocyte. These include the transformation of an interphase microtubule network into microtubule asters (53) and the development of mechanisms that release calcium from the endoplasmic reticulum (54) and prevent polyspermy (55). Similar to the progression of meiosis, these cytoplasmic responses are probably suppressed by inhibiting CDK1 kinase activity, although this hypothesis remains to be tested.
Dependence of Prophase Arrest in the Preovulatory Follicle on Cyclic GMP Produced in the Granulosa Cells
The finding that the oocyte is the source of inhibitory cAMP raises the question as to what role(s) granulosa cells play in maintaining prophase arrest. Earlier studies showed that cAMP in the mouse oocyte decreases when it is removed from the follicle (56–58), indicating that the granulosa cells participate in regulating oocyte cAMP. Several mechanisims have been considered to explain this observation.
The first mechanism proposes that granulosa cells synthesize and secrete an agonist that keeps GPR3 active in the oocyte, thus keeping Gs active and increasing cAMP. However, Gs activity fails to change when the oocyte is removed from the follicle (42). Another possibility is that additional cAMP enters the oocyte from the granulosa cells through gap junctions, adding to levels already being produced in the oocyte. Whether the concentration of free cAMP in the granulosa cells is high enough to provide a source of cAMP for diffusion into the oocyte is unknown. To test whether cAMP from the granulosa cells contributes to maintaining meiotic arrest, it would be informative to specifically lower cAMP in the granulosa cells and determine if this causes meiosis to resume. At present, it can only be concluded that cAMP diffusion from the granulosa cells into the oocyte is not sufficient to maintain meiotic arrest in the absence of GPR3/ Gs-mediated production of cAMP in the oocyte.
An alternative hypothesis, which ultimately proved to be correct, suggested that granulosa cells provide an inhibitor of cAMP phosphodiesterase activity, thus maintaing high cAMP levels in the oocyte. Another cyclic nucleotide, cGMP, was found to inhibit cAMP phosphodiesterase activity in oocyte lysates (59), and removing the oocyte from the follicle lowered cGMP in the oocyte (58). These findings were consistent with the hypothesis that cGMP from granulosa cells diffuses through gap junctions into the oocyte, where it inhibits cAMP hydrolysis and maintains meiotic arrest (58, 60). It was subsequently established that the predominant cAMP phosphodiesterase in the oocyte is PDE3A (61–63) (Figures 3 and 5), an enzyme that is competitively inhibited by cGMP (63, 64).
This hypothesis was tested by injecting follicle-enclosed oocytes with Förster resonance energy transfer (FRET) sensors for cAMP and cGMP, allowing quantitative measurements of cyclic nucleotide concentrations in a physiologically intact system (65). Injecting oocytes with a specific cGMP phosphodiesterase, PDE9, decreases cGMP and leads to resumption of meiosis. However, this effect could be blocked by milrinone, an inhibitor of PDE3A, supporting the conclusion that lowering cGMP caused meiosis to resume by relieving the inhibition of PDE3A. The concentration of cGMP in follicle-enclosed oocytes was measured to be ~900 nM, which is sufficient to competitively inhibit PDE3A at the ~700 nM cAMP level in the oocyte (63, 65). Based on the finding that inhibiting follicular gap junctions decreased cGMP in the oocyte and is accompanied by resumption of meiosis, it was concluded that this inhibitory cGMP comes from granulosa cells and enters the oocyte through gap junctions (65).
Production of cGMP in the Granulosa Cells by the NPR2 Guanylyl Cyclase
cGMP is produced in the granulosa cells by the guanylyl cyclase natriuretic peptide receptor 2 (NPR2, also called guanylyl cyclase B) (66). NPR2 mRNA and protein are present in both the mural granulosa cells and cumulus cells, but not in the oocyte or theca cells (66–69) (Figure 3). The concentration of Npr2 mRNA is nearly two times higher in the cumulus versus mural granulosa cells. Within mural cells, Npr2 levels are higher near the antrum, consistent with a report demonstrating that signals from the oocyte increase Npr2 (66). However, in terms of the total mass of NPR2 protein, ~97% of the NPR2 in the follicle resides in mural cells, correlating with the much larger volume of the mural compartment (70). By imaging follicles from mice expressing a global cGMP sensor, cGMP concentrations are seen to be uniform throughout mural granulosa cells, cumulus cells, and the oocyte; this results from cGMP diffusion through gap junctions (71) (Figures 4 and 5).
NPR2 is activated by the 22-amino acid C-type natriuretic peptide (CNP, also called NPPC) that is produced in mural granulosa cells and released into the extracellular space (Figure 3) (66). CNP diffuses in the follicular fluid and activates NPR2 in both cumulus and mural granulosa cells. Loss-of-function mutations in Npr2 or Nppc result in spontaneous meiotic resumption in preovulatory follicle-enclosed oocytes (66, 69, 72). Npr2-deficient follicles also contain less cGMP (72). As would be predicted, female Npr2 mutant mice are infertile (72). Human females with loss-of-function mutations in NPR2 are fertile when heterozygous, but the fertility of homozygous females has not been investigated (73).
Application of CNP (10–100 nM) to cumulus-oocyte complexes from mice (66, 74), pigs (75, 76), cows (77), and domestic cats (78) inhibits meiotic resumption. CNP does not inhibit meiotic resumption in isolated oocytes (66, 75, 76) because oocytes do not express NPR2 (66). A second peptide, porcine B-type natriuretic peptide (BNP), was also shown to activate NPR2 and inhibit meiotic resumption in porcine cumulus-oocyte complexes (76). Porcine BNP is unique in this regard because BNP of other species does not activate NPR2 (79). Meiotic inhibition by CNP (and porcine BNP) is consistent with early evidence that a small peptide (~2 kDa) in follicular fluid partially inhibits meiotic resumption in porcine cumulus-oocyte complexes (32).
The CNP concentration in follicular fluid isolated from human preovulatory follicles is ~100 nM (74), and the combined CNP and BNP concentration in porcine follicular fluid is ~130 nM (76). This concentration of CNP and BNP is similar to that required to maintain meiotic arrest in ~75% of porcine cumulus-oocyte complexes (76). However, when hamster cumulus-oocyte complexes are dislodged from the follicle wall, but remain within the follicular fluid, meiosis resumes (80). This suggests that sufficient cGMP levels are maintained in the cumulus-oocyte complex only if the complex is attached to mural cells. Likewise, when connexin 43 junctions are inhibited, meiosis resumes, illustrating the importance of gap junction–mediated signals from the mural cells (31). It is possible that local CNP concentrations are higher in the extracellular space between the multiple layers of mural granulosa cells, where CNP is produced, than in the follicular fluid surrounding the cumulus cells (see Figure 5). If so, the cGMP concentration in the oocyte could be maintained at a higher level if gap junctions between the mural cells and cumulus cells are intact.
Activity of the enzyme inosine monophosphate dehydrogenase (IMPDH) is also essential for maintaining meiotic arrest. Specific IMPDH inhibitors induce resumption of meiosis when injected into mice (81) or applied to CNP-arrested cumulus oocyte complexes (82). IMPDH catalyses the conversion of IMP to guanylyl substrates for NPR2 production of cGMP (82).
RELEASE OF MEIOTIC PROPHASE ARREST BY LUTEINIZING HORMONE
Signaling Across a Tissue
A long-standing mystery is how LH signals through its receptor in the outer granulosa cells and then remotely initiates resumption of meioisis in the oocyte that is located up to 10 cell layers away. Understanding of this long distance signaling in meiotic resumption might also shed light on hormonal signaling in other avascular tissues, such as the growth plate of developing bone (83). LH receptors are expressed almost exclusively in mural granulosa and in theca cells with little or no presence in cumulus cells or the oocyte (14, 84–90). In rat and mouse preovulatory follicles, LH receptors are enriched in the outer layers of mural granulosa cells (14, 84, 85, 87, 89, 91) (Figure 3). Although in most conditions LH receptors are also expressed in theca cells, they are absent in the theca cells of preovulatory follicles from gonadotropin-primed immature rats (84), and yet these follicles are able to resume meiosis following LH stimulation. Furthermore, in granulosa-oocyte complexes derived by culturing preantral follicles from which both the basal lamina and most of the theca cells are removed, LH signaling can also stimulate meiotic resumption (92). Collectively, these observations indicate that LH receptors in the granulosa cells rather than theca cells mediate meiotic resumption.
In fish and amphibians, LH receptors are located in the somatic cells surrounding the oocyte. However, in these vertebrate species, LH conveys the meiosis–inducing signal by release of a steroid that acts on the oocyte (93, 94). This has raised the question of whether a steroid-mediated process also restarts meiosis in mammalian follicles; however, published studies indicate that the answer is no (95).
Other mechanisms accounting for this long-distance signaling included the possibilities that LH signaling reduces endogenous GPR3 agonists or elevates GPR3 antagonists. Either one of these changes would decrease Gs activity in the oocyte, resulting in less cAMP production. However, Gs activity in the oocyte is unchanged by LH signaling (96). Likewise, inhibition of the Gi G protein by pertussis toxin fails to prevent meiotic resumption in the mouse oocyte (97), unlike results reported for starfish, where an agonist from the follicle cells (1-methyladenine in starfish) causes meiotic resumption by activating Gi in the oocyte (98).
Following the recognition that cGMP could inhibit cAMP hydrolysis in the oocyte, it was proposed that lowering oocyte cGMP could mediate LH signaling of meiotic resumption and that this could occur either by closing gap junctions or by decreasing cGMP in granulosa cells (60). As discussed below, the development of methods for measuring and manipulating cyclic nucleotide levels in individual compartments of live follicles has allowed testing of this hypothesis. These studies established that one important component of the signaling that reinitiates meiosis is a rapid decrease in cGMP in the outer granulosa cells where LH receptors are located. As a consequence, cGMP diffuses out of the oocyte down its concentration gradient (Figure 5).
Signaling to the interior of the follicle is also accomplished by slower processes involving changes in the amounts of peptides that are released by the mural cells and that diffuse through the extracellular space to act on the cumulus cells. In particular, as discussed below, LH signaling decreases the production of the NPR2 agonist CNP (74) and increases the production of epidermal growth factor receptor (EGFR) agonists, which act to lower cGMP (99). Regulation of gap junction permeability is yet another component in this complex system.
LH signaling begins with the activation of a G-protein–coupled receptor that is coupled primarily to Gs, thus increasing cAMP production by adenylyl cyclase in the granulosa cells (100). This seems paradoxical, as an increase in cAMP in the granulosa cells leads to a decrease in cAMP in the oocyte. We return to this paradox later but first discuss the cyclic nucleotide changes in the oocyte that result from LH signaling. We then discuss the intercellular signaling mechanisms in the follicle that accomplish these changes in the oocyte and finally consider how G-protein signaling in the outer layers of mural granulosa cells initiates these events.
The Luteinizing Hormone–Induced Decreases in cAMP and cGMP in Follicle-Enclosed Oocytes
The effects of LH on cAMP and cGMP in follicle-enclosed oocytes were initially measured by rapidly removing the oocytes from the follicles; immunoassays showed that LH causes a decrease in both cAMP (30, 56) and cGMP (101). Such measurements were complicated by the fall in cyclic nucleotides that results from oocyte isolation from the follicle, but nevertheless, LH-induced changes were detected. Later, when it became possible to microinject cyclic nucleotide FRET sensors into follicle-enclosed oocytes, avoiding the need to isolate the oocytes to make measurements, larger changes were seen (65). By 1 h after LH treatment, cAMP decreases from ~700 to ~100 nM, and cGMP decreases from ~900 nM to ~40 nM. Both cAMP and cGMP stay low in the oocyte for at least 5 h. Based on these measurements, the decrease in cGMP in the oocyte would increase PDE3A hydrolysis of cAMP by ~5 times, thus decreasing cAMP (63, 65).
The Luteinizing Hormone–Induced Decrease in cGMP in the Granulosa Cells
The LH-induced decrease in cGMP in the oocyte is accompanied by a decrease in cGMP in rat ovaries (102) and in isolated preovulatory follicles from mice, rats, and hamsters (63, 65, 101, 103), as measured by immunoassays. LH also causes cGMP to decrease in luteinized human granulosa cells (104). Although cGMP concentrations cannot be precisely determined from measurements of follicle cGMP content, due to a lack of precise information about cytosolic volume, estimated concentrations for mouse follicles are ~1–4 μM before LH application and ~100 nM at 1 h afterward (65, 71, 105). cGMP stays at a low level for at least 5 h (103–105). Considering the limitations of each method of measurement, these values from immunoassays of whole follicles are quite similar to the FRET measurements from follicle-enclosed oocytes, both before and after LH treatment.
Using mouse follicles that transgenically express a FRET sensor for cGMP and imaging with a confocal microscope, it was seen directly that prior to LH application, the concentration of cGMP is similar throughout the mural granulosa, cumulus cells, and oocyte (71). Time-lapse recordings of cGMP levels using follicles expressing the FRET sensor (Figure 4) showed that within 1 min of LH application, cGMP starts to decrease in the outer 25 μm of the follicle where LH receptors are located (71). Within this region, a plateau value is reached after ~10 min. In the cumulus cells, the cGMP decrease starts with a delay of ~5 min, and in the oocyte, it starts with a delay of ~7 min. By 20 min after LH application, the cGMP concentration is at a uniformly low level throughout the follicle. These results show that the LH-induced decrease in cGMP occurs first in the outer mural granulosa cells, then in the cumulus cells, and finally in the oocyte.
When gap junction permeability in the follicle is inhibited by carbenoxolone, cGMP stays high in both the mural granulosa cells and cumulus cells, where the NPR2 guanylyl cyclase is located. However in the oocyte, which lacks NPR2, cGMP decreases (71). In the presence of carbenoxolone, measurements at 20 min after LH application show a decrease in cGMP in the mural cells where the LH receptors are located, but not in the cumulus cells. However, by 2 h, cGMP decreases in the cumulus cells as well. These results support the conclusion that the initial LH-induced cGMP decrease in the cumulus cells is due to cGMP diffusion outward into the mural cells by way of gap junctions (Figure 5), but that later, cGMP is maintained at a low level in the cumulus cells due to gap junction-independent signaling.
The Luteinizing Hormone–Induced Decrease in Synthesis of cGMP by Natriuretic Peptide Receptor 2
Early studies investigating the LH-induced cGMP decrease in follicles explored the possibilities that either cGMP synthesis or cGMP hydrolysis was changed (106, 107). Although variable results were obtained at that time, it is now established that the rapid LH-induced cGMP decrease in the follicle results from both a decrease in cGMP synthesis by NPR2 (103, 108) and an increase in cGMP hydrolysis by the phosphodiesterase PDE5 (109) (Figure 5). These two changes are complementary. Whether LH also increases cGMP efflux was not investigated. This section discusses the decrease in NPR2 activity and its regulation by dephosphorylation of NPR2. The regulation of PDE5 is discussed in a subsequent section.
LH treatment of either mouse or rat follicles reduces NPR2 activity by ~50% by 20–30 min (103, 108). This rapid decrease in activity, as measured in the whole follicle, is indicative of a decrease in activity in the mural granulosa cells, as these account for ~95% of the follicle volume. Two to three hours later, NPR2 activity also decreases in the cumulus cells (108), most likely mediated by paracrine signaling by way of the EGFR, which is discussed in a later section.
The rapid decrease in NPR2 activity occurs without any change in the amount of the NPR2 protein or CNP, although CNP decreases later (103, 108). Instead, the activity decrease is caused by the dephosphorylation of seven juxtamembrane serines and threonines of NPR2 (70, 103). Inhibitor studies indicate that the responsible phosphatase is in the phosphoprotein phosphatase (PPP) family, and together with expression analysis, they point to PP1, PP2A, or PP6 as likely candidates for mediating LH-induced NPR2 dephosphorylation (103).
Because of direct effects on the oocyte, phosphatase inhibitors are not suitable for testing whether NPR2 dephosphorylation is required for LH-induced meiotic resumption. Instead, this question was addressed using mice in which the seven juxtamembrane serines and threonines of NPR2 were replaced with the phosphomimetic amino acid glutamate (NPR2-7E) (70). In these follicles, LH treatment does not reduce NPR2 activity, and the LH-induced decrease in cGMP is attenuated (70). As a result, meiotic resumption in NPR2-7E follicles is delayed by ~5 h (70).
However, meiotic resumption does eventually occur (70). This may be related to a slow decrease in gap junction permeability between the oocyte and cumulus cells, first detected at 5–6 h after LH receptor activation (110, 111), which could isolate the oocyte from the source of inhibitory cGMP. One cause of the permeability decrease could be the secretion of an extracellular matrix by cumulus cells that begins at ~6 h after LH activation and results in an apparent separation of these cells (111). Another likely contributor to the eventual resumption of meiosis is that the CNP content of the ovary decreases starting ~2 h after LH receptor activation (104, 108). This would decrease NPR2 activity and lower cGMP levels, even with the NPR2-7E mutation. By ~3 h, Npr2 transcripts decrease as well (68, 69).
Although NPR2 dephosphorylation is required for the normal time course of meiotic resumption, NPR2-7E female mice are fertile (70). This indicates that despite the delay in meiotic resumption, there appears to be time for completion of the first meiotic division prior to fertilization. However, it is unknown whether the mutations cause subfertility.
How activation of the LH receptor leads to NPR2 dephosphorylation and inactivation is poorly understood. One question is whether these mechanisms involve the activation of a phosphatase or the inhibition of a kinase (or both). LH signaling, via PKA, phosphorylates and activates a regulatory subunit of the PP2A phosphatase in rat granulosa cells (112), indicating that PKA activation of PP2A could be a factor leading to NPR2 dephosphorylation. EGFR signaling, discussed below, also contributes to LH-induced NPR2 dephosphorylation, based on the finding that EGFR agonist-induced nuclear envelope breakdown is delayed in NPR2-7E mice (70).
The Luteinizing Hormone–Induced Increase in Hydrolysis of cGMP by Phosphodiesterase 5
Although the rapid LH-induced decrease in NPR2 guanylyl cyclase activity does not occur when NPR2 dephosphorylation is prevented, a partial decrease in cGMP, insufficient to trigger meiotic resumption, still occurs (70, 103). These findings suggest that LH signaling might also increase the activity of a cGMP phosphodiesterase.
Several cGMP-hydrolyzing phosphodiesterases are expressed in granulosa cells of mice and rats (109). Among these, PDE5 is of particular interest because its activity is increased by phosphorylation by PKA (113, 114), and LH signaling activates PKA (115). Indeed, PDE5 in rat follicles is phosphorylated within 10 min of LH treatment and remains phosphorylated for at least 4 h (109). As a result, LH treatment increases the cGMP-hydrolytic activity of PDE5 by ~70%. These events are dependent on PKA activity but independent of EGFR kinase activity (109), which as discussed below, increases in response to LH signaling. The phosphorylation and activation of PDE5 would act, along with the dephosphorylation and inactivation of NPR2, to lower follicle cGMP levels in response to LH (109) (Figure 5).
PDE1A, a phosphodiesterase that is activated by Ca2+/calmodulin, is also expressed in rat and mouse granulosa cells (109), but whether PDE1A activity is increased by LH is unknown. If LH signaling increases cytosolic free Ca2+, an increase in PDE1A activity would follow. Increases in cytosolic Ca2+ are detected when LH is applied to isolated porcine granulosa cells (116), and EGFR agonists, which increase in response to LH, cause Ca2+ to increase in mouse cumulus cells (117). However, it is unknown if LH signaling causes Ca2+ to increase in intact follicles.
cGMP phosphodiesterase activity is required to achieve the low cGMP levels that trigger meiotic resumption (63). However, there are some differences between species in the particular phosphodiesterases that are required. PDE5 inhibitors delay LH-induced meiotic resumption in mouse follicles by several hours (63), indicating that PDE5 activity is responsible for most of the cGMP decrease. In contrast, in rat follicles, both PDE1 and PDE5 must be inhibited to maximally inhibit meiotic resumption. However, it is unknown whether the contribution of PDE1 stems from its steady-state activity in the granulosa cells or whether LH increases its activity by increasing free Ca2+.
Contribution of the Decrease in C-Type Natriuretic Peptide to the Luteinizing Hormone–Induced cGMP Decrease and Meiotic Resumption
A slower response to LH that contributes to maintaining cGMP at low levels is a decrease in the NPR2 small peptide agonist CNP. This decrease was measured in mouse ovaries (74, 104, 108), rat follicles (103), and human and porcine follicular fluid (74, 76). In mouse ovaries, the decrease is not seen until 2 h after LH receptor stimulation, when CNP content has decreased to about half of its initial value (104, 108). Thus, the fall in CNP is too slow to account for the rapid decrease in cGMP in the follicle (71) but could be important for maintaining cGMP at a low level at later times.
CNP would diffuse through the extracellular space of the follicle, such that a fall in CNP production in the mural cells would result in a fall in CNP not only around the mural cells but also around the cumulus cells (Figure 5). At 36 h after LH receptor activation in porcine follicles, at which time most oocytes have undergone nuclear envelope breakdown, the concentration of CNP plus BNP has decreased to ~20 nM (76). When incubated with 20 nM CNP or BNP, ~50% of isolated cumulus-oocyte complexes resume meiosis, versus ~25% at the ~130 nM concentration before LH exposure (76). This finding indicates that the decrease in CNP (and BNP) is sufficient to contribute to the decrease in cGMP in response to LH.
The LH-induced decrease in CNP peptide levels is associated with decreased Nppc transcripts encoding the precursor protein of CNP (74, 104); signaling pathways leading to the decrease in Nppc are not well understood, although EGFR activation appears sufficient but not essential (104). The LH-induced decrease in CNP is also independent of the natriuretic peptide clearance receptor NPR3 (118).
Contribution of Epidermal Growth Factor Receptor Activation to the Luteinizing Hormone–Induced cGMP Decrease and Meiotic Resumption
An important component of the signaling pathway by which LH decreases cGMP in the follicle is the activation of the EGFR by its endogenous agonists epiregulin and amphiregulin. In ovaries of mice (99), rats (119, 120), pigs (121), and humans (122), epiregulin and/or amphiregulin increase in response to LH. These peptides are produced in the mural granulosa cells (99) and act on EGFRs that are located in mural granulosa and cumulus cells but not in the oocyte (99) (Figure 3). Binding to the EGFR causes dimerization and an increase in intrinsic protein-tyrosine kinase activity, resulting in autophosphorylation (123). EGFR phosphorylation in mouse follicles increases within 15 min after LH application and continues to increase over the next 3 h (99, 104, 124).
Activating EGFR in follicles decreases cGMP (63, 71, 104, 105), which is seen first in the mural cells and then in the cumulus cells and oocyte (71). In different studies, EGFR activation by epiregulin and/or amphiregulin completely or partially recapitulates the LH-induced cGMP decrease. Moreover, inhibiting EGFR kinase activity attenuates the LH-induced cGMP decrease, although the extent of attenuation reported is variable (63, 71, 104, 105, 125).
Activating EGFR in cumulus-oocyte complexes also decreases cGMP in both cumulus cells and oocytes from mice (117) and pigs (121). This supports the concept that endogenous EGFR agonists are released in response to LH receptor activation in the mural granulosa cells and then diffuse through the extracellular space to decrease cGMP in the cumulus cells (Figure 5). Because gap junctions directly connect cumulus cells to the oocyte, the EGFR-induced cGMP decrease in cumulus cells also decreases cGMP in the oocyte. EGFR agonists also act to decrease cGMP in the mural granulosa cells (71), contributing to the decrease in oocyte cGMP through the series of gap junctions connecting these compartments.
Application of EGFR agonists epiregulin and/or amphiregulin to mouse or rat follicles (99, 105, 120, 126), or to pig cumulus-oocyte complexes incubated in CNP (121), causes meiotic resumption. Correspondingly, the use of pharmacological inhibitors of EGFR signaling that target receptor kinase activity or block protein processing of epiregulin and/or amphiregulin delays LH-induced meiotic resumption by at least 4–6 h in mouse follicles (99, 104, 105, 125); some of these follicles eventually resume meiosis (105). Similar findings are also reported for rat follicles (120, 127) and human and pig cumulus-oocyte complexes (121, 122). Thus, in all mammalian species tested, EGFR signaling is a critical mediator of LH signaling.
Mutant mice with minimal EGFR kinase activity also show delayed meiotic resumption in response to LH receptor stimulation (125, 128). However, most oocytes in these mutant mice do eventually resume meiosis, as indicated by the finding that their fertility is only slighly impaired (125, 128) or normal (129, 130). One such mutant line has highly reduced fertility, but nonovarian effects may contribute to this phenotype (128). The lack of a major effect on fertility in Egfr mutant mice is presumably due to functionally redundant parallel signaling pathways that provide a fail-safe system for ensuring meiotic resumption.
How LH signaling stimulates EGFR phosphorylation and activation is incompletely understood. Matrix metalloproteases, which release epiregulin and amphiregulin from their precursor proteins, are required, indicating that the activation of the EGFR occurs by an increase in these endogenous agonists (120, 124). Within 1 h, LH signaling increases transcript levels that encode epiregulin and amphiregulin precursor proteins (99). However, because EGFR phosphorylation increases within 15 min of LH receptor activation (104), it is likely that LH signaling also stimulates the cleavage of epiregulin and amphiregulin from preexisting precursor proteins (Figure 5).
Elevating cAMP with forskolin mimics the LH-induced stimulation of EGFR phosphorylation, and the PKA inhibitor H89 partially inhibits EGFR phosphorylation, supporting a role for PKA in part of the signaling pathway (124). PKA stimulates MAP kinase activity (131), which is required for part of the increase in EGFR agonist mRNAs (132). It is unknown how LH signaling might stimulate matrix metalloproteases or other pathways that activate the EGFR.
How EGFR activity decreases cGMP is also incompletely understood. As discussed above, it contributes to the pathway leading to NPR2 dephosphorylation (70) but not PDE5 phosphorylation (109) (Figure 5). Because EGFR activation can elevate Ca2+ in cumulus cells (117), it may also stimulate hydrolysis of cGMP by PDE1.
Luteinizing Hormone Regulation of Gap Junctions in the Follicle
As mentioned above, on a timescale of hours, LH signaling reduces gap junction permeability between the oocyte and cumulus cells by mechanisms that are not certain but may be related to physical separation of the cumulus cells, associated with the secretion of an extracellular matrix between them (110, 111). There are also incompletely understood changes in gap junction structure in the follicle, as detected by freeze fracture electron microscopy (133, 134).
On a more rapid time scale, LH signaling partially inhibits the permeability of the connexin 43 junctions between the granulosa cells; this decrease is due to phosphorylation of connexin 43 by MAP kinase (6, 135). Permeability decreases by 30 min after LH application, reaches a minimum at 1 h, and returns to the original level by 5 h (6, 71). The permeability decrease was detected by use of fluorescent tracers; whether permeability to cGMP and/or cAMP also decreases was not examined. Gap junction permeability between the cumulus cells and oocyte, which is mediated by connexin 37, does not decrease during this period (6).
The function of the decrease in gap junction permeability between the granulosa cells is unknown. It is not necessary for causing meiotic resumption in response to LH, which still occurs with a normal time course when the permeability decrease is prevented by inhibiting connexin 43 phosphorylation by inhibiting MAP kinase (6). Likewise, the gap junction permeability decrease is not sufficient to cause meiotic resumption under conditions in which NPR2 dephosphorylation is prevented (70). If connexin 43 phosphorylation caused a selective decrease in cAMP versus cGMP permeability, this could be beneficial, as discussed below.
Initiation of Luteinizing Hormone Signaling by G Protein Activation, cAMP Elevation, and Protein Kinase A Activation in the Mural Granulosa Cells
In this section, we consider the earliest events in LH signaling and how these initiate the pathways described above. LH signaling begins with the activation of its G-protein–coupled receptor in the mural granulosa cells. The duration of LH signaling is extended by internalization of the receptors after LH binding, such that signaling continues even in the absence of extracellular LH (127, 136). The LH receptor can activate multiple G proteins (137, 138), but most of its effects on meiotic resumption appear to be due to the activation of Gs.
Gs activation in the mural granulosa cells increases cAMP production by adenylyl cyclase (139, 140). This results in an elevation of cAMP in the follicle, as measured by immunoassays (56, 128, 139, 141, 142), and specifically in the mural granulosa cells, as detected with a FRET sensor (136). cAMP also increases in the cumulus cells, based on immunoassays of isolated cumulus-oocyte complexes, but this was not seen until ~1.5 h after LH application (56). FRET sensor measurements suggest that the cAMP increase in the cumulus cells might occur earlier, but this is uncertain because of the large region of measurement that extended beyond the 2–3 layers of cumulus cells (136).
The LH-induced increase in cAMP in the mural granulosa cells contrasts with the decrease in cAMP in the oocyte. How this transpires is poorly understood, as it might be expected that cAMP would diffuse from the granulosa cells into the oocyte. Both the connexin 43 junctions between the granulosa cells and the connexin 37 junctions at the oocyte surface are permeable to cGMP (71), but some types of gap junctions are more permeable to cGMP than cAMP (143). Connexin 43 junctions are highly permeable to cAMP (144, 145), but cAMP permeability was not investigated for connexin 37. If connexin 37 had low cAMP permeability, this could explain why the granulosa cell cAMP increase is not transmitted to the oocyte. If phosphorylation of connexin 43 selectively lowered cAMP permeability (but not cGMP permeability) between the granulosa cells, that could also contribute to preventing cAMP diffusion into the oocyte. In addition, cAMP phosphodiesterase activity may restrict the elevation of cAMP in the granulosa cells from spreading into the oocyte.
Transiently elevating cAMP by treating follicles with forskolin to activate adenylyl cyclase (127, 141), or elevating cAMP in the granulosa cells with an inhibitor of the cAMP phosphodiesterase PDE4 (61, 136), causes meiotic resumption. The forskolin-induced cAMP increase activates PKA (112, 115), which phosphorylates and activates PDE5 to the same extent as LH stimulation (109) (Figure 5). Forskolin treatment also inactivates NPR2 ( JR Egbert, JW Robinson, LR Potter, LA Jaffe, unpublished data). These experiments indicate that elevation of cAMP in the granulosa cells is the primary stimulus that initiates the events that restart meiosis.
Another indirect consequence of PKA activation is the phosphorylation of the EGFR, as indicated by evidence that EGFR phosphorylation is stimulated by forskolin, and LH-induced EGFR phosphorylation is reduced by inhibiting PKA (124) (Figure 5). It is unknown how PKA causes EGFR phosphorylation; it may stimulate the matrix metalloproteases that cleave epiregulin and amphiregulin from their precursors (Figure 5), and/or it may stimulate transcription of the precursors. As discussed above, activation of the EGFR is a component of the pathway by which LH signaling dephosphorylates and inactivates NPR2, which is essential for the normal progression of meiosis. Thus PKA activation is a regulator of multiple pathways by which LH signaling triggers meiotic resumption.
SUMMARY AND FUTURE ISSUES
Mammalian oocytes become arrested in meiotic prophase before birth, and remain arrested as they develop within a follicle that is ultimately comprised of approximately 10 layers of granulosa cells. Meiotic resumption is triggered by the mid-cycle surge in luteinizing hormone that acts on the outermost granulosa cells, but how this signal is transduced to the oocyte has only recently become clear. Diffusion of cyclic GMP from the granulosa cells to the oocyte through gap junctions maintains meiotic arrest in the later stages of development. Through many redundant and thus fail-safe processes over different time scales, luteinizing hormone decreases cGMP levels in the granulosa cells and oocyte, which coordinates the timing of meiotic resumption with ovulation and fertilization to ensure reproductive success. Understanding these long-distance signaling mechanisms that control oocyte meiosis might also shed light on signaling in other physiological systems.
Although much has been discovered, many questions remain. Some of these outstanding questions are summarized below.
How does LH signaling cause NPR2 dephosphorylation? What kinase phosphorylates NPR2, and is it inhibited by LH signaling? Does LH signaling activate a phosphatase that dephosphorylates NPR2?
Does LH signaling increase Ca2+ and activate PDE1 in the granulosa cells?
How does LH signaling decrease the concentration of CNP?
Does LH signaling activate a matrix metalloprotease that releases amphiregulin and epiregulin from their precursors? Does LH signaling also activate the EGFR through an intracellular pathway?
How does EGFR signaling lead to NPR2 dephosphorylation? Does EGFR activation decrease cGMP by other mechanisms as well?
Are connexin 37 gap junctions more permeable to cGMP than cAMP? Does connexin 43 phosphorylation reduce cGMP and/or cAMP permeability?
Are there other pathways that participate in the fail-safe mechanisms that promote the timely resumption of meiosis in mammals, such as the positive stimuli acting in frogs and starfish?
Do other avascular tissues, such as the growth plate of developing bone, use similar mechanisms for intercellular communication?
ACKNOWLEDGMENTS
We thank Lisa Mehlmann, Rachael Norris, and Leia Shuhaibar for their contributions to the research from our laboratory that is described here. We also thank John Eppig, Slava Nikolaev, Lincoln Potter, Melina Schuh, Mary Hunzicker-Dunn, Gail Mandel, and Mark Terasaki for many thought-provoking discussions and for their comments on the manuscript, and Holly Ingraham for her insightful suggestions. Research in our laboratory is supported by a grant from the National Institute of Child Health and Human Development (R37HD014939).
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- 1.Eppig JJ, Viveiros MM, Marin-Bivens C, De La Fuente R. Regulation of mammalian oocyte maturation. In: Leung PCK, Adashi EY, editors. The Ovary. 2nd ed Elsevier/Academic; San Diego, CA: 2004. pp. 113–29. [Google Scholar]
- 2.Conti M, Hsieh M, Zamah AM, Oh JS. Novel signaling mechanisms during oocyte maturation and ovulation. Mol. Cell. Endocrinol. 2012;356:65–73. doi: 10.1016/j.mce.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clift D, Schuh M. Restarting life: fertilization and the transition from meiosis to mitosis. Nat. Rev. Mol. Cell Biol. 2013;14:549–62. doi: 10.1038/nrm3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holt JE, Lane SIR, Jones KT. The control of meiotic maturation in mammalian oocytes. Curr. Top. Dev. Biol. 2013;102:207–26. doi: 10.1016/B978-0-12-416024-8.00007-6. [DOI] [PubMed] [Google Scholar]
- 5.Adhikari D, Liu K. The regulation of maturation promoting factor during prophase I arrest and meiotic entry in mammalian oocytes. Mol. Cell. Endocrinol. 2014;382:480–87. doi: 10.1016/j.mce.2013.07.027. [DOI] [PubMed] [Google Scholar]
- 6.Norris RP, Freudzon M, Mehlmann LM, Cowan AE, Simon AM, et al. Luteinizing hormone causes MAPK-dependent phosphorylation and closure of Cx43 gap junctions in mouse ovarian follicles: one of two paths to meiotic resumption. Development. 2008;135:3229–38. doi: 10.1242/dev.025494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson E, Wilkinson RF, Lee G, Meller S. A correlative microscopical analysis of differentiating ovarian follicles of mammals. J. Morphol. 1978;156:339–66. doi: 10.1002/jmor.1051560303. [DOI] [PubMed] [Google Scholar]
- 8.Anderson E, Albertini DF. Gap junctions between the oocyte and companion follicle cells in the mammalian ovary. J. Cell Biol. 1976;71:680–86. doi: 10.1083/jcb.71.2.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simon AM, Goodenough DA, Li E, Paul DL. Female infertility in mice lacking connexin 37. Nature. 1997;385:525–29. doi: 10.1038/385525a0. [DOI] [PubMed] [Google Scholar]
- 10.Li TY, Colley D, Barr KJ, Yee S-P, Kidder GM. Rescue of oogenesis in Cx37-null mutant mice by oocyte-specific replacement with Cx43. J. Cell Sci. 2007;120:4117–25. doi: 10.1242/jcs.03488. [DOI] [PubMed] [Google Scholar]
- 11.Gittens JE, Kidder GM. Differential contributions of connexin37 and connexin43 to oogenesis revealed in chimeric reaggregated mouse ovaries. J. Cell Sci. 2005;118:5071–78. doi: 10.1242/jcs.02624. [DOI] [PubMed] [Google Scholar]
- 12.Simon AM, Chen H, Jackson CL. Cx37 and Cx43 localize to zona pellucida in mouse ovarian follicles. Cell Commun. Adhes. 2006;13:61–77. doi: 10.1080/15419060600631748. [DOI] [PubMed] [Google Scholar]
- 13.Lipner H, Cross NL. Morphology of the membrana granulosa of the ovarian follicle. Endocrinology. 1968;82:638–41. doi: 10.1210/endo-82-3-638. [DOI] [PubMed] [Google Scholar]
- 14.Amsterdam A, Koch Y, Lieberman ME, Linder HR. Distribution of binding sites for human chorionic gonadotropin in the preovulatory follicle of the rat. J. Cell. Biol. 1975;67:894–900. doi: 10.1083/jcb.67.3.894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bächler M, Menshykau D, De Geyter C, Iber D. Species-specific differences in follicular antral sizes result from diffusion-based limitations on the thickness of the granulosa cell layer. Mol. Hum. Reprod. 2014;20:208–21. doi: 10.1093/molehr/gat078. [DOI] [PubMed] [Google Scholar]
- 16.Griffin J, Emery BR, Huang I, Peterson CM, Carrell DT. Comparative analysis of follicle morphology and oocyte diameter in four mammalian species (mouse, hamster, pig, and human) J. Exp. Clin. Assist. Reprod. 2006;3:2. doi: 10.1186/1743-1050-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edwards RG, Gates AH. Timing of the stages of the maturation divisions, ovulation, fertilization and the first cleavage of eggs of adult mice treated with gonadotrophins. J. Endocrinol. 1959;18:292–304. doi: 10.1677/joe.0.0180292. [DOI] [PubMed] [Google Scholar]
- 18.Motlík J, Fulka J. Breakdown of the germinal vesicle in pig oocytes in vivo and in vitro. J. Exp. Zool. 1976;198:155–62. doi: 10.1002/jez.1401980205. [DOI] [PubMed] [Google Scholar]
- 19.Seibel MM, Smith DM, Levesque L, Borten M, Taymor ML. The temporal relationship between the luteinizing hormone surge and human oocyte maturation. Am. J. Obstet. Gynecol. 1982;142:568–72. doi: 10.1016/0002-9378(82)90763-3. [DOI] [PubMed] [Google Scholar]
- 20.Chesnel F, Eppig JJ. Synthesis and accumulation of p34cdc2 and cyclin B in mouse oocytes during acquisition of competence to resume meiosis. Mol. Reprod. Dev. 1995;40:503–8. doi: 10.1002/mrd.1080400414. [DOI] [PubMed] [Google Scholar]
- 21.de Vantéry C, Stutz A, Vassalli JD, Schorderet-Slatkine S. Acquisition of meiotic competence in growing mouse oocytes is controlled at both translational and posttranslational levels. Dev. Biol. 1997;187:43–54. doi: 10.1006/dbio.1997.8599. [DOI] [PubMed] [Google Scholar]
- 22.Nishimura T, Shimaoka T, Kano K, Naito K. Insufficient amount of Cdc2 and continuous activation of Wee1 B are the cause of meiotic failure in porcine growing oocytes. J. Reprod. Dev. 2009;55:553–57. doi: 10.1262/jrd.09-072a. [DOI] [PubMed] [Google Scholar]
- 23.Adhikari D, Zheng W, Shen Y, Gorre N, Ning Y, et al. Cdk1, but not Cdk2, is the sole Cdk that is essential and sufficient to drive resumption of meiosis in mouse oocytes. Hum. Mol. Genet. 2012;21:2476–84. doi: 10.1093/hmg/dds061. [DOI] [PubMed] [Google Scholar]
- 24.Lénárt P, Rabut G, Daigle N, Hand AR, Terasaki M, Ellenberg J. Nuclear envelope breakdown in starfish oocytes proceeds by partial NPC disassembly followed by a rapidly spreading fenestration of nuclear membranes. J. Cell Biol. 2003;160:1055–68. doi: 10.1083/jcb.200211076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abe S, Nagasaka K, Hirayama Y, Kozuka-Hata H, Oyama M, et al. The initial phase of chromosome condensation requires Cdk1-mediated phosphorylation of the CAP-D3 subunit of condensin II. Genes Dev. 2011;25:863–74. doi: 10.1101/gad.2016411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pincus G, Enzmann EV. The comparative behavior of mammalian eggs in vivo and in vitro. J. Exp. Med. 1935;62:665–75. doi: 10.1084/jem.62.5.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Edwards RG. Maturation in vitro of mouse, sheep, cow, pig, rhesus monkey and human ovarian oocytes. Nature. 1965;208:349–51. doi: 10.1038/208349a0. [DOI] [PubMed] [Google Scholar]
- 28.Erickson GF, Sorensen RA. In vitro maturation of mouse oocytes isolated from late, middle, and pre-antral Graafian follicles. J. Exp. Zool. 1974;190:123–27. doi: 10.1002/jez.1401900112. [DOI] [PubMed] [Google Scholar]
- 29.Piontkewitz Y, Dekel N. Heptanol, an alkanol that blocks gap junctions, induces oocyte maturation. Endocr. J. 1993;1:365–72. [Google Scholar]
- 30.Sela-Abramovich S, Edry I, Galiani D, Nevo N, Dekel N. Disruption of gap junctional communication within the ovarian follicle induces oocyte maturation. Endocrinology. 2006;147:2280–86. doi: 10.1210/en.2005-1011. [DOI] [PubMed] [Google Scholar]
- 31.Richard S, Baltz JM. Prophase I arrest of mouse oocytes mediated by natriuretic peptide precursor C requires GJA1 (connexin-43) and GJA4 (connexin-37) gap junctions in the antral follicle and cumulusoocyte complex. Biol. Reprod. 2014;90(6):137. doi: 10.1095/biolreprod.114.118505. [DOI] [PubMed] [Google Scholar]
- 32.Tsafriri A, Pomerantz SH, Channing CP. Inhibition of oocyte maturation by porcine follicular fluid: partial characterization of the inhibitor. Biol. Reprod. 1976;14:511–16. doi: 10.1095/biolreprod14.5.511. [DOI] [PubMed] [Google Scholar]
- 33.Cho WK, Stern S, Biggers JD. Inhibitory effect of dibutyryl cAMP on mouse oocyte maturation in vitro. J. Exp. Zool. 1974;187:383–86. doi: 10.1002/jez.1401870307. [DOI] [PubMed] [Google Scholar]
- 34.Magnusson C, Hillensjö T. Inhibition of maturation and metabolism in rat oocytes by cyclic AMP. J. Exp. Zool. 1977;201:139–47. doi: 10.1002/jez.1402010117. [DOI] [PubMed] [Google Scholar]
- 35.Bornslaeger EA, Schultz RM. Adenylate cyclase in zona-free mouse oocytes. Exp. Cell Res. 1985;156:277–81. doi: 10.1016/0014-4827(85)90282-4. [DOI] [PubMed] [Google Scholar]
- 36.Mehlmann LM, Jones TLZ, Jaffe LA. Meiotic arrest in the mouse follicle maintained by a Gs protein in the oocyte. Science. 2002;297:1343–45. doi: 10.1126/science.1073978. [DOI] [PubMed] [Google Scholar]
- 37.Kalinowski RR, Berlot CH, Jones TLZ, Ross LF, Jaffe LA, Mehlmann LM. Maintenance of meiotic prophase arrest in vertebrate oocytes by a Gs protein-mediated pathway. Dev. Biol. 2004;267:1–13. doi: 10.1016/j.ydbio.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Gallo CJ, Hand AR, Jones TLZ, Jaffe LA. Stimulation of Xenopus oocyte maturation by inhibition of the G-protein alpha S subunit, a component of the plasma membrane and yolk platelet membranes. J. Cell Biol. 1995;130:275–84. doi: 10.1083/jcb.130.2.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DiLuigi A, Weitzman VN, Pace MC, Siano LJ, Maier D, Mehlmann LM. Meiotic arrest in human oocytes is maintained by a Gs signaling pathway. Biol. Reprod. 2008;78:667–72. doi: 10.1095/biolreprod.107.066019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehlmann LM, Saeki Y, Tanaka S, Brennan TJ, Evsikov AV, et al. The Gs-linked receptor GPR3 maintains meiotic arrest in mammalian oocytes. Science. 2004;306:1947–50. doi: 10.1126/science.1103974. [DOI] [PubMed] [Google Scholar]
- 41.Eggerickx D, Denef J-F, Labbe O, Hayashi Y, Refetoff S, et al. Molecular cloning of an orphan G-protein-coupled receptor that constitutively activates adenylate cyclase. Biochem. J. 1995;309:837–43. doi: 10.1042/bj3090837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Freudzon L, Norris RP, Hand AR, Tanaka S, Saeki Y, et al. Regulation of meiotic prophase arrest in mouse oocytes by GPR3, a constitutive activator of the Gs G protein. J. Cell Biol. 2005;171:255–65. doi: 10.1083/jcb.200506194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ledent C, Demeestere I, Blum D, Petermans J, Hamalainen T, et al. Premature ovarian aging in mice deficient for Gpr3. PNAS. 2005;102:8922–26. doi: 10.1073/pnas.0503840102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mehlmann LM. Oocyte-specific expression of Gpr3 is required for the maintenance of meiotic arrest in mouse oocytes. Dev. Biol. 2005;288:397–404. doi: 10.1016/j.ydbio.2005.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang C-R, Wei Y, Qi S-T, Chen L, Zhang Q-H, et al. The G protein coupled receptor 3 is involved in cAMP and cGMP signaling and maintenance of meiotic arrest in porcine oocytes. PLOS ONE. 2012;7:e38807. doi: 10.1371/journal.pone.0038807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hinckley M, Vaccari S, Horner K, Chen R, Conti M. The G-protein-coupled receptors GPR3 and GPR12 are involved in cAMP signaling and maintenance of meiotic arrest in rodent oocytes. Dev. Biol. 2005;287:249–61. doi: 10.1016/j.ydbio.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 47.Horner K, Livera G, Hinckley M, Trinh K, Storm D, Conti M. Rodent oocytes express an active adenylyl cyclase required for meiotic arrest. Dev. Biol. 2003;258:385–96. doi: 10.1016/s0012-1606(03)00134-9. [DOI] [PubMed] [Google Scholar]
- 48.Bornslaeger EA, Mattei P, Schultz RM. Involvement of cAMP-dependent protein kinase and protein phosphorylation in regulation of mouse oocyte maturation. Dev. Biol. 1986;114:453–62. doi: 10.1016/0012-1606(86)90209-5. [DOI] [PubMed] [Google Scholar]
- 49.Han SJ, Chen R, Paronetto MP, Conti M. Wee1B is an oocyte-specific kinase involved in the control of meiotic arrest in the mouse. Curr. Biol. 2005;15:1670–76. doi: 10.1016/j.cub.2005.07.056. [DOI] [PubMed] [Google Scholar]
- 50.Duckworth BC, Weaver JS, Ruderman JV. G2 arrest in Xenopus oocytes depends on phosphorylation of cdc25 by protein kinase A. PNAS. 2002;99:16794–99. doi: 10.1073/pnas.222661299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pirino G, Wescott MP, Donovan PJ. Protein kinase A regulates resumption of meiosis by phosphorylation of Cdc25B in mammalian oocytes. Cell Cycle. 2009;8:665–70. doi: 10.4161/cc.8.4.7846. [DOI] [PubMed] [Google Scholar]
- 52.Dupré A, Daldello EM, Nairn AC, Jessus C, Haccard O. Phosphorylation of ARPP19 by protein kinase A prevents meiosis resumption in Xenopus oocytes. Nat. Commun. 2014;5:3318. doi: 10.1038/ncomms4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schuh M, Ellenberg J. Self-organization of MTOCs replaces centrosome function during acentrosomal spindle assembly in live mouse oocytes. Cell. 2007;130:484–98. doi: 10.1016/j.cell.2007.06.025. [DOI] [PubMed] [Google Scholar]
- 54.Mehlmann LM, Kline D. Regulation of intracellular calcium in the mouse egg: calcium release in response to sperm or inositol trisphosphate is enhanced after meiotic maturation. Biol. Reprod. 1994;51:1088–98. doi: 10.1095/biolreprod51.6.1088. [DOI] [PubMed] [Google Scholar]
- 55.Kryzak CA, Moraine MM, Kyle DD, Lee HJ, Cubenas-Potts C, et al. Prophase I mouse oocytes are deficient in the ability to respond to fertilization by decreasing membrane receptivity to sperm and establishing a membrane block to polyspermy. Biol. Reprod. 2013;89:44. doi: 10.1095/biolreprod.113.110221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schultz RM, Montgomery RR, Belanoff JR. Regulation of mouse oocyte meiotic maturation: Implication of a decrease in oocyte cAMP and protein dephosphorylation in commitment to resume meiosis. Dev. Biol. 1983;97:264–73. doi: 10.1016/0012-1606(83)90085-4. [DOI] [PubMed] [Google Scholar]
- 57.Vivarelli E, Conti M, DeFelici M, Siracusa G. Meiotic resumption and intracellular cAMP levels in mouse oocytes treated with compounds which act on cAMP metabolism. Cell Differ. 1983;12:271–76. doi: 10.1016/0045-6039(83)90023-4. [DOI] [PubMed] [Google Scholar]
- 58.Törnell J, Billig H, Hillensjö T. Resumption of rat oocyte meiosis is paralleled by a decrease in guanosine 3′, 5′-cyclic monophosphate (cGMP) and is inhibited by microinjection of cGMP. Acta. Physiol. Scand. 1990;139:511–17. doi: 10.1111/j.1748-1716.1990.tb08953.x. [DOI] [PubMed] [Google Scholar]
- 59.Bornslaeger EA, Mattei P, Schultz RM. Regulation of mouse oocyte maturation: involvement of cyclic AMP phosphodiesterase and calmodulin. Dev. Biol. 1984;105:488–99. doi: 10.1016/0012-1606(84)90306-3. [DOI] [PubMed] [Google Scholar]
- 60.Törnell J, Billig H, Hillensjö T. Regulation of oocyte maturation by changes in ovarian levels of cyclic nucleotides. Human. Reprod. 1991;6:411–22. doi: 10.1093/oxfordjournals.humrep.a137351. [DOI] [PubMed] [Google Scholar]
- 61.Tsafriri A, Chun S-Y, Zhang R, Hsueh AJW, Conti M. Oocyte maturation involves compartmentalization and opposing changes of cAMP levels in follicular somatic and germ cells: studies using selective phosphodiesterase inhibitors. Dev. Biol. 1996;178:393–402. doi: 10.1006/dbio.1996.0226. [DOI] [PubMed] [Google Scholar]
- 62.Masciarelli S, Horner K, Liu C, Park SH, Hinckley M, et al. Cyclic nucleotide phosphodiesterase 3A-deficient mice as a model of female infertility. J. Clin. Investig. 2004;114:196–205. doi: 10.1172/JCI21804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vaccari S, Weeks JL, Hsieh M, Menniti FS, Conti M. Cyclic GMP signaling is involved in the LH-dependent meiotic maturation of mouse oocytes. Biol. Reprod. 2009;81:595–604. doi: 10.1095/biolreprod.109.077768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bender AT, Beavo JA. Cyclic nucleotide phosphodiesterases: molecular regulation to clinical use. Pharmacol. Rev. 2006;58:488–520. doi: 10.1124/pr.58.3.5. [DOI] [PubMed] [Google Scholar]
- 65.Norris RP, Ratzan WJ, Freudzon M, Mehlmann LM, Krall J, et al. Cyclic GMP from the surrounding somatic cells regulates cyclic AMP and meiosis in the mouse oocyte. Development. 2009;136:1869–78. doi: 10.1242/dev.035238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang M, Su Y-Q, Sugiura K, Xia G, Eppig JJ. Granulosa cell ligand NPPC and its receptor NPR2 maintain meiotic arrest in mouse oocytes. Science. 2010;330:366–69. doi: 10.1126/science.1193573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jankowski M, Reis AM, Mukaddam-Daher S, Dam T-V, Farookhi R, Gutkowska J. C-type natriuretic peptide and the guanylyl cyclase receptors in the rat ovary are modulated by the estrous cycle. Biol. Reprod. 1997;56:59–66. doi: 10.1095/biolreprod56.1.59. [DOI] [PubMed] [Google Scholar]
- 68.Zhang M, Su Y-Q, Sugiura K, Wigglesworth K, Xia G, Eppig JJ. Estradiol promotes and maintains cumulus cell expression of natriuretic peptide receptor 2 (NPR2) and meiotic arrest in mouse oocytes in vitro. Endocrinology. 2011;152:4377–85. doi: 10.1210/en.2011-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tsuji T, Kiyosu C, Akiyama K, Kunieda T. CNP/NPR2 signaling maintains oocyte meiotic arrest in early antral follicles and is suppressed by EGFR-mediated signaling in preovulatory follicles. Mol. Reprod. Dev. 2012;79:795–802. doi: 10.1002/mrd.22114. [DOI] [PubMed] [Google Scholar]
- 70.Shuhaibar LC, Egbert JR, Edmund AB, Uliasz TF, Dickey DM, et al. Dephosphorylation of juxtamembrane serines and threonines of the NPR2 guanylyl cyclase is required for rapid resumption of oocyte meiosis in response to luteinizing hormone. Dev. Biol. 2016;409:194–201. doi: 10.1016/j.ydbio.2015.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shuhaibar LC, Egbert JR, Norris RP, Lampe PD, Nikolaev VO, et al. Intercellular signaling via cyclic GMP diffusion through gap junctions in the mouse ovarian follicle. PNAS. 2015;112:5527–32. doi: 10.1073/pnas.1423598112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Geister KA, Brinkmeier ML, Hsieh M, Faust SM, Karolyi IJ, et al. A novel loss-of-function mutation in Npr2 clarifies primary role in female reproduction and reveals a potential therapy for acromesomelic dysplasia, Maroteaux type. Hum. Mol. Genet. 2013;22:345–57. doi: 10.1093/hmg/dds432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Khan S, Ali RH, Abbasi S, Nawaz M, Muhammad N, Ahmad W. Novel mutations in natriuretic peptide receptor-2 gene underlie acromesomelic dysplasia, type maroteaux. BMC Med. Genet. 2012;13:44. doi: 10.1186/1471-2350-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kawamura K, Cheng Y, Kawamura N, Takae S, Okada A, et al. Pre-ovulatory LH/hCG surge decreases C-type natriuretic peptide secretion by ovarian granulosa cells to promote meiotic resumption of pre-ovulatory oocytes. Hum. Reprod. 2011;26:3094–101. doi: 10.1093/humrep/der282. [DOI] [PubMed] [Google Scholar]
- 75.Hiradate Y, Hoshino Y, Tanemura K, Sato E. C-type natriuretic peptide inhibits porcine oocyte meiotic resumption. Zygote. 2014;22:372–77. doi: 10.1017/S0967199412000615. [DOI] [PubMed] [Google Scholar]
- 76.Zhang W, Yang Y, Liu W, Chen Q, Wang H, et al. Brain natriuretic peptide and C-type natriuretic peptide maintain porcine oocyte meiotic arrest. J. Cell. Physiol. 2015;230:71–81. doi: 10.1002/jcp.24682. [DOI] [PubMed] [Google Scholar]
- 77.Franciosi F, Coticchio G, Lodde V, Tessaro I, Modina SC, et al. Natriuretic peptide precursor C delays meiotic resumption and sustains gap junction-mediated communication in bovine cumulus-enclosed oocytes. Biol. Reprod. 2014;91(3):61, 1–9. doi: 10.1095/biolreprod.114.118869. [DOI] [PubMed] [Google Scholar]
- 78.Zhong Y, Lin J, Liu X, Hou J, Zhang Y, Zhao X. C-type natriuretic peptide maintains domestic cat oocytes in meiotic arrest. Reprod. Fert. Develop. 2016;28:1553–59. doi: 10.1071/RD14425. [DOI] [PubMed] [Google Scholar]
- 79.Potter LR. Regulation and therapeutic targeting of peptide-activated receptor guanylyl cyclases. Pharmacol. Ther. 2011;130:71–82. doi: 10.1016/j.pharmthera.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Racowsky C, Baldwin KV. In vitro and in vivo studies reveal that hamster oocyte meiotic arrest is maintained only transiently by follicular fluid, but persistently by membrana/cumulus granulosa cell contact. Dev. Biol. 1989;134:297–306. doi: 10.1016/0012-1606(89)90102-4. [DOI] [PubMed] [Google Scholar]
- 81.Downs SM, Eppig JJ. Induction of mouse oocyte maturation in vivo by perturbants of purine metabolism. Biol. Reprod. 1987;36:431–37. doi: 10.1095/biolreprod36.2.431. [DOI] [PubMed] [Google Scholar]
- 82.Wigglesworth K, Lee K-B, O’Brien MJ, Peng J, Matzuk MM, Eppig JJ. Bidirectional communication between oocytes and ovarian follicular somatic cells is required for meiotic arrest of mammalian oocytes. PNAS. 2013;110:E3723–29. doi: 10.1073/pnas.1314829110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kozhemyakina E, Lassar AB, Zelzer E. A pathway to bone: signaling molecules and transcription factors involved in chondrocyte development and maturation. Development. 2015;142:817–31. doi: 10.1242/dev.105536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bortolussi M, Marini G, Dal Lago A. Autoradiographic study of the distribution of LH(HCG) receptors in the ovary of untreated and gonadotrophin-primed immature rats. Cell Tissue Res. 1977;183:329–42. doi: 10.1007/BF00220640. [DOI] [PubMed] [Google Scholar]
- 85.Bortolussi M, Marini G, Reolon ML. A histochemical study of binding of 125I-HCG to the rat ovary throughout the estrus cycle. Cell Tissue Res. 1979;197:213–26. doi: 10.1007/BF00233915. [DOI] [PubMed] [Google Scholar]
- 86.Channing CP, Bae I-H, Stone SL, Anderson LD, Edelson S, Fowler SC. Porcine granulosa and cumulus cell properties. LH/hCG receptors, ability to secrete progesterone and ability to respond to LH. Mol. Cell. Endocrinol. 1981;22:359–70. doi: 10.1016/0303-7207(81)90044-7. [DOI] [PubMed] [Google Scholar]
- 87.Wang X, Greenwald GS. Hypophysectomy of the cyclic mouse. II. Effects of follicle-stimulating hormone (FSH) and luteinizing hormone on folliculogenesis, FSH and human chorionic gonadotropin receptors, and steroidogenesis. Biol. Reprod. 1993;48:595–605. doi: 10.1095/biolreprod48.3.595. [DOI] [PubMed] [Google Scholar]
- 88.Eppig JJ, Wigglesworth K, Pendola F, Hirao Y. Murine oocytes suppress expression of luteinizing hormone receptor messenger ribonucleic acid by granulosa cells. Biol. Reprod. 1997;56:976–84. doi: 10.1095/biolreprod56.4.976. [DOI] [PubMed] [Google Scholar]
- 89.Eppig JJ, Wigglesworth K, Pendola F. The mammalian oocyte orchestrates the rate of ovarian follicular development. PNAS. 2002;99:2890–94. doi: 10.1073/pnas.052658699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jeppesen JV, Kristensen SG, Nielsen ME, Humaidan P, Dal Canto M, et al. LH-receptor gene expression in human granulosa and cumulus cells from antral and preovulatory follicles. J. Clin. Endocrinol. Metab. 2012;97:E1524–31. doi: 10.1210/jc.2012-1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Richards JS, Midgley AR. Protein hormone action: a key to understanding ovarian follicular and luteal cell development. Biol. Reprod. 1976;14:82–94. doi: 10.1095/biolreprod14.1.82. [DOI] [PubMed] [Google Scholar]
- 92.Eppig JJ. Maintenance of meiotic arrest and the induction of oocyte maturation in mouse oocytegranulosa cell complexes developed in vitro from preantral follicles. Biol. Reprod. 1991;45:824–30. doi: 10.1095/biolreprod45.6.824. [DOI] [PubMed] [Google Scholar]
- 93.Nagahama Y, Yamashita M. Regulation of oocyte maturation in fish. Dev. Growth Differ. 2008;50(Suppl. 1):S195–219. doi: 10.1111/j.1440-169X.2008.01019.x. [DOI] [PubMed] [Google Scholar]
- 94.Haccard O, Dupré A, Liere P, Pianos A, Eychenne B, et al. Naturally occurring steroids in Xenopus oocyte during meiotic maturation. Unexpected presence and role of steroid sulfates. Mol. Cell. Endocrinol. 2012;362:110–19. doi: 10.1016/j.mce.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 95.Tsafriri A, Motola S. Are steroids dispensable for meiotic resumption in mammals? Trends Endocrinol. Metab. 2007;18:321–27. doi: 10.1016/j.tem.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 96.Norris RP, Freudzon L, Freudzon M, Hand AR, Mehlmann LM, Jaffe LA. A Gs-linked receptor maintains meiotic arrest in mouse oocytes, but luteinizing hormone does not cause meiotic resumption by terminating receptor-Gs signaling. Dev. Biol. 2007;310:240–49. doi: 10.1016/j.ydbio.2007.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mehlmann LM, Kalinowski RR, Ross LF, Parlow AF, Hewlett EL, Jaffe LA. Meiotic resumption in response to luteinizing hormone is independent of a Gi family G protein or calcium in the mouse oocyte. Dev. Biol. 2006;299:345–55. doi: 10.1016/j.ydbio.2006.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shilling F, Chiba K, Hoshi M, Kishimoto T, Jaffe LA. Pertussis toxin inhibits 1-methyladenine-induced maturation in starfish oocytes. Dev. Biol. 1989;133:605–8. doi: 10.1016/0012-1606(89)90063-8. [DOI] [PubMed] [Google Scholar]
- 99.Park JY, Su YQ, Ariga M, Law E, Jin SL, Conti M. EGF-like growth factors as mediators of LH action in the ovulatory follicle. Science. 2004;303:682–84. doi: 10.1126/science.1092463. [DOI] [PubMed] [Google Scholar]
- 100.Hunzicker-Dunn M, Mayo K. Gonadotropin signaling in the ovary. In: Plant TM, Zeleznik AJ, editors. Knobil and Neill’s Physiology of Reproduction. 4th ed Academic; San Diego, CA: 2015. pp. 895–945. [Google Scholar]
- 101.Hubbard CJ. Cyclic AMP changes in the component cells of Graafian follicles: possible influences on maturation in the follicle-enclosed oocytes of hamsters. Dev. Biol. 1986;118:343–51. doi: 10.1016/0012-1606(86)90003-5. [DOI] [PubMed] [Google Scholar]
- 102.Ratner A. Effects of follicle stimulating hormone and luteinizing hormone upon cyclic AMP and cyclic GMP levels in rat ovaries in vitro. Endocrinology. 1976;99:1496–500. doi: 10.1210/endo-99-6-1496. [DOI] [PubMed] [Google Scholar]
- 103.Egbert JR, Shuhaibar LC, Edmund AB, Van Helden DA, Robinson JW, et al. Dephosphorylation and inactivation of the NPR2 guanylyl cyclase in the granulosa cells contributes to the LH-induced cGMP decrease that causes resumption of meiosis in rat oocytes. Development. 2014;141:3594–604. doi: 10.1242/dev.112219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liu X, Xie F, Zamah AM, Cao B, Conti M. Multiple pathways mediate luteinizing hormone regulation of cGMP signaling in the mouse ovarian follicle. Biol. Reprod. 2014;91(1):9, 1–11. doi: 10.1095/biolreprod.113.116814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Norris RP, Freudzon M, Nikolaev VO, Jaffe LA. Epidermal growth factor receptor kinase activity is required for gap junction closure and for part of the decrease in ovarian follicle cGMP in response to LH. Reproduction. 2010;140:655–62. doi: 10.1530/REP-10-0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Patwardhan VV, Lanthier A. Cyclic GMP phosphodiesterase and guanylate cyclase activities in rabbit ovaries and the effect of in-vivo stimulation with LH. J. Endocrinol. 1984;101:305–10. doi: 10.1677/joe.0.1010305. [DOI] [PubMed] [Google Scholar]
- 107.Patwardhan VV, Lanthier A. Ovarian cyclic GMP concentration and guanylate cyclase and cyclic GMP phosphodiesterase activities in proestrous rat after treatment with LH. Horm. Metabol. Res. 1987;19:136–37. doi: 10.1055/s-2007-1011760. [DOI] [PubMed] [Google Scholar]
- 108.Robinson JW, Zhang M, Shuhaibar LC, Norris RP, Geerts A, et al. Luteinizing hormone reduces the activity of the NPR2 guanylyl cyclase in mouse ovarian follicles, contributing to the cyclic GMP decrease that promotes resumption of meiosis in oocytes. Dev. Biol. 2012;366:308–16. doi: 10.1016/j.ydbio.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Egbert JR, Uliasz TF, Shuhaibar LC, Geerts A, Wunder F, et al. Luteinizing hormone causes phosphorylation and activation of the cyclic GMP phosphodiesterase PDE5 in rat ovarian follicles, contributing, together with PDE1 activity, to the resumption of meiosis. Biol. Reprod. 2016;94:110, 1–11. doi: 10.1095/biolreprod.115.135897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gilula NB, Epstein ML, Beers WH. Cell-to-cell communication and ovulation. A study of the cumulus-oocyte complex. J. Cell Biol. 1978;78:58–75. doi: 10.1083/jcb.78.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Eppig JJ. The relationship between cumulus cell-oocyte coupling, oocyte meiotic maturation, and cumulus expansion. Dev. Biol. 1982;89:268–72. doi: 10.1016/0012-1606(82)90314-1. [DOI] [PubMed] [Google Scholar]
- 112.Flynn MP, Maizels ET, Karlsson AB, McAvoy T, Ahn J-H, et al. Luteinizing hormone receptor activation in ovarian granulosa cells promotes protein kinase A-dependent dephosphorylation of microtubule-associated protein 2D. Mol. Endocrinol. 2008;22:1695–710. doi: 10.1210/me.2007-0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Corbin JD, Turko IV, Beasley A, Francis SH. Phosphorylation of phosphodiesterase-5 by cyclic nucleotide-dependent protein kinase alters its catalytic and allosteric cGMP-binding activities. Eur. J. Biochem. 2000;267:2760–67. doi: 10.1046/j.1432-1327.2000.01297.x. [DOI] [PubMed] [Google Scholar]
- 114.Rybalkin SD, Rybalkina IG, Feil R, Hofmann F, Beavo JA. Regulation of cGMP-specific phosphodiesterase (PDE5) phosphorylation in smooth muscle cells. J. Biol. Chem. 2002;277:3310–17. doi: 10.1074/jbc.M106562200. [DOI] [PubMed] [Google Scholar]
- 115.Hunzicker-Dunn M. Selective activation of rabbit ovarian protein kinase isozymes in rabbit ovarian follicles and corpora lutea. J. Biol. Chem. 1981;256:12185–93. [PubMed] [Google Scholar]
- 116.Flores JA, Aguirre C, Sharma OP, Veldhuis JD. Luteinizing hormone (LH) stimulates both intra-cellular calcium ion ([Ca2+]i) mobilization and transmembrane cation influx in single ovarian (granulosa) cells: Recruitment as a cellular mechanism of LH-[Ca2+]i dose response. Endocrinology. 1998;139:3606–12. doi: 10.1210/endo.139.8.6162. [DOI] [PubMed] [Google Scholar]
- 117.Wang Y, Kong N, Li N, Hao X, Wei K, et al. Epidermal growth factor receptor signaling-dependent calcium elevation in cumulus cells is required for NPR2 inhibition and meiotic resumption in mouse oocytes. Endocrinology. 2013;154:3401–9. doi: 10.1210/en.2013-1133. [DOI] [PubMed] [Google Scholar]
- 118.Lee K-B, Zhang M, Sugiura K, Wigglesworth K, Uliasz T, et al. Hormonal coordination of natriuretic peptide type C and natriuretic peptide receptor 3 expression in mouse granulosa cells. Biol. Reprod. 2013;88:42, 1–9. doi: 10.1095/biolreprod.112.104810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sekiguchi T, Mizutani T, Yamada K, Kajitani T, Yazawa T, et al. Expression of epiregulin and amphiregulin in the rat ovary. J. Mol. Endocrinol. 2004;33:281–91. doi: 10.1677/jme.0.0330281. [DOI] [PubMed] [Google Scholar]
- 120.Ashkenazi H, Cao X, Motola S, Popliker M, Conti M, Tsafriri A. Epidermal growth factor family members: endogenous mediators of the ovulatory response. Endocrinology. 2005;146:77–84. doi: 10.1210/en.2004-0588. [DOI] [PubMed] [Google Scholar]
- 121.Zhang W, Chen Q, Yang Y, Liu W, Zhang M, et al. Epidermal growth factor-network signaling mediates luteinizing hormone regulation of BNP and CNP and their receptor NPR2 during porcine oocyte meiotic resumption. Mol. Reprod. Dev. 2014;81:1030–41. doi: 10.1002/mrd.22424. [DOI] [PubMed] [Google Scholar]
- 122.Zamah AM, Hsieh M, Chen J, Vigne JL, Rosen MP, et al. Human oocyte maturation is dependent on LH-stimulated accumulation of the epidermal growth factor-like growth factor, amphiregulin. Hum. Reprod. 2010;25:2569–78. doi: 10.1093/humrep/deq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kovacs E, Zorn JA, Huang Y, Barros T, Kuriyan J. A structural perspective on the regulation of the epidermal growth factor receptor. Annu. Rev. Biochem. 2015;84:739–64. doi: 10.1146/annurev-biochem-060614-034402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Panigone S, Hsieh M, Fu M, Persani L, Conti M. LH signaling in preovulatory follicles involves early activation of the EGFR pathway. Mol. Endocrinol. 2008;22:924–36. doi: 10.1210/me.2007-0246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hsieh M, Thao K, Conti M. Genetic dissection of epidermal growth factor receptor signaling during luteinizing hormone-induced oocyte maturation. PLOS ONE. 2011;6:e21574. doi: 10.1371/journal.pone.0021574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dekel N, Sherizly I. Epidermal growth factor induces maturation of rat follicle-enclosed oocytes. Endocrinology. 1985;116:406–9. doi: 10.1210/endo-116-1-406. [DOI] [PubMed] [Google Scholar]
- 127.Reizel Y, Elbaz J, Dekel N. Sustained activity of the EGF receptor is an absolute requisite for LH-induced oocyte maturation and cumulus expansion. Mol. Endocrinol. 2010;24:402–11. doi: 10.1210/me.2009-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hsieh M, Lee D, Panigone S, Horner K, Chen R, et al. Luteinizing hormone-dependent activation of the epidermal growth factor network is essential for ovulation. Mol. Cell. Biol. 2007;27:1914–24. doi: 10.1128/MCB.01919-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Du X, Tabeta K, Hoebe K, Liu H, Mann N, et al. Velvet, a dominant Egfr mutation that causes wavy hair and defective eyelid development in mice. Genetics. 2004;166:331–40. doi: 10.1534/genetics.166.1.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Andric N, Thomas M, Ascoli M. Transactivation of the epidermal growth factor receptor is involved in the lutropin receptor-mediated down-regulation of ovarian aromatase expression in vivo. Mol. Endocrinol. 2010;24:552–60. doi: 10.1210/me.2009-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Salvador LM, Maizels E, Hales DB, Miyamoto E, Yamamoto H, Hunzicker-Dunn M. Acute signaling by the LH receptor is independent of protein kinase C activation. Endocrinology. 2002;143:2986–94. doi: 10.1210/endo.143.8.8976. [DOI] [PubMed] [Google Scholar]
- 132.Fan H-Y, Liu Z, Shimada M, Sterneck E, Johnson PF, et al. MAPK3/1 (ERK1/2) in ovarian granulosa cells are essential for female fertility. Science. 2009;324:938–41. doi: 10.1126/science.1171396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Larsen WJ, Wert SE, Brunner GD. A dramatic loss of cumulus cell gap junctions is correlated with germinal vesicle breakdown in rat oocytes. Dev. Biol. 1986;113:517–21. doi: 10.1016/0012-1606(86)90187-9. [DOI] [PubMed] [Google Scholar]
- 134.Larsen WJ, Wert SE, Brunner GD. Differential modulation of rat follicle cell gap junction populations at ovulation. Dev. Biol. 1987;122:61–71. doi: 10.1016/0012-1606(87)90332-0. [DOI] [PubMed] [Google Scholar]
- 135.Sela-Abramovich S, Chorev E, Galiani D, Dekel N. Mitogen-activated protein kinase mediates luteinizing hormone-induced breakdown of communication and oocyte maturation in rat ovarian follicles. Endocrinology. 2005;146:1236–44. doi: 10.1210/en.2004-1006. [DOI] [PubMed] [Google Scholar]
- 136.Lyga S, Volpe S, Werthmann RC, Götz K, Sungkaworn T, et al. Persistent cAMP signaling by internalized LH receptors in ovarian follicles. Endocrinology. 2016;157:1613–21. doi: 10.1210/en.2015-1945. [DOI] [PubMed] [Google Scholar]
- 137.Herrlich A, Kühn B, Grosse R, Schmid A, Schultz G, Gudermann T. Involvement of Gs and Gi proteins in dual coupling of the luteinizing hormone receptor to adenylyl cyclase and phospholipase C. J. Biol. Chem. 1996;271:16764–72. doi: 10.1074/jbc.271.28.16764. [DOI] [PubMed] [Google Scholar]
- 138.Rajagopalan-Gupta RM, Lamm MLG, Mukherjee S, Rasenick MM, Hunzicker-Dunn M. Luteinizing hormone/choriogonadotropin receptor-mediated activation of heterotrimeric guanine nucleotide binding proteins in ovarian follicular membranes. Endocrinology. 1998;139:4547–55. doi: 10.1210/endo.139.11.6302. [DOI] [PubMed] [Google Scholar]
- 139.Tsafriri A, Lindner HR, Zor U, Lamprecht SA. In-vitro induction of meiotic division in follicle-enclosed rat oocytes by LH, cyclic AMP and prostaglandin E2. J. Reprod. Fert. 1972;31:39–50. doi: 10.1530/jrf.0.0310039. [DOI] [PubMed] [Google Scholar]
- 140.Hunzicker-Dunn M. Rabbit follicular adenylyl cyclase activity. I. Conditions of assay and gonadotropin sensitivity in granulosa cells and follicle shells. Biol. Reprod. 1981;24:267–78. doi: 10.1095/biolreprod24.2.267. [DOI] [PubMed] [Google Scholar]
- 141.Hashimoto N, Kishimoto T, Nagahama Y. Induction and inhibition of meiotic maturation in follicle-enclosed mouse oocytes by forskolin. Develop. Growth Differ. 1985;27:709–16. doi: 10.1111/j.1440-169X.1985.00709.x. [DOI] [PubMed] [Google Scholar]
- 142.Rodriguez KF, Couse JF, Jayes FL, Hamilton KJ, Burns KA, et al. Insufficient luteinizing hormone-induced intracellular signaling disrupts ovulation in preovulatory follicles lacking estrogen receptor-β. Endocrinology. 2010;151:2826–34. doi: 10.1210/en.2009-1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bevans CG, Kordel M, Rhee SK, Harris AL. Isoform composition of connexin channels determines selectivity among second messengers and uncharged molecules. J. Biol. Chem. 1998;273:2808–16. doi: 10.1074/jbc.273.5.2808. [DOI] [PubMed] [Google Scholar]
- 144.Ponsioen B, van Zeijl L, Moolenaar WH, Jalink K. Direct measurement of cyclic AMP diffusion and signaling through connexin43 gap junctional channels. Exp. Cell. Res. 2007;313:415–23. doi: 10.1016/j.yexcr.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 145.Kanaporis G, Mese G, Valiuniene L, White TW, Brink PR, Valiunas V. Gap junction channels exhibit connexin-specific permeability to cyclic nucleotides. J. Gen. Physiol. 2008;131:293–305. doi: 10.1085/jgp.200709934. [DOI] [PMC free article] [PubMed] [Google Scholar]