Abstract
Minimally invasive techniques were used for tracheostomy including small horizontal skin incision, limited soft tissue dissection and no suturing. A Retrospective analysis of case sheets of patients who underwent elective tracheostomy by the first and second authors at M S Ramaiah Hospitals in Bangalore between 1st May 2010 and 1st May 2015 was done to compare the result of elective conventional open surgical tracheostomy using midline vertical skin incision with minimally invasive tracheostomy using a short horizontal incision. No statistically significant difference in the peri and post operative complication rate was found. The patterns of intra and post operative complications reflected the choice of the surgical technique—the conventional technique had problems associated with wide dissection, whereas the minimally invasive technique had problems associated with limited exposure. Problems of wound gaping, emphysema and peristomal inflammation were reduced with minimally invasive technique with short horizontal skin incision although statistical difference could not be shown. There was also no statistically significant difference with either technique regards death and decannulation rates. Minimally invasive technique of elective open surgical tracheostomy was found to be as safe as conventional open surgical tracheostomy with midline vertical skin incision in the studied groups.
Keywords: Elective surgical tracheostomy, Horizontal versus vertical incision, Minimally invasive surgery
Introduction
There are a number of minimally invasive procedures performed by surgeons who are leaders in their respective fields. In the past few years, minimally invasive surgery has replaced the open conventional surgery as the gold standard for many procedures [1]. The concept of surgical invasiveness cannot be limited to the length or to the site of the skin incision. It must be extended to all structures dissected during the procedure [2]. Although there has been some work studying minimally invasive head and neck surgeries [3, 4], our search revealed little literature available regarding minimally invasive techniques being applied to open surgical tracheostomy [5, 6].
The conventional surgical tracheostomy is considered as the gold standard for securing the airway. Most of the minimally invasive approaches to tracheostomy have evolved into percutaneous tracheostomy techniques. There are several studies comparing percutaneous and open surgical tracheostomy techniques. Percutaneous tracheostomy is reported to have less peristomal infection and inflammation compared to open surgical tracheostomy [7, 8], probably due to utilization of smaller incision and minimal tissue dissection. Per operative difficulty and complications were minimally higher with percutaneous tracheostomy. The cost and requirement of specialized equipment are barriers to utilization of percutaneous techniques in our country [9]. Open surgical tracheostomy is preferred in patients with morbid obesity and those with difficult anatomy like short neck [10].
There are several described modifications of the surgical steps of elective adult surgical tracheostomy. The choice of the technique used depends on patient factors, surgeon training and preference [11, 12]. Among studies of the variations of technique, the horizontal vs vertical skin incisions have literature available. Although horizontal and vertical skin incisions have been described for surgical tracheostomy most surgeons consider that horizontal skin incisions are cosmetically superior to vertical incisions [13]. There are also variations in the length of the incisions used as described in standard literature [14]. The length of incisions used vary from 5 mm to 5 cm or even longer [5, 13, 14].
While performing elective tracheostomy in our institution, surgical tracheostomy with minimally invasive techniques and a short horizontal skin incision was applied by one of the authors while the other preferred a conventional approach with a vertical incision. Hence, we performed a retrospective analysis of the patient data and compared the per operative and post operative results.
Methods
A retrospective analysis of the available case sheets of adult patients who underwent elective tracheostomy by the first and second authors at M S Ramaiah Hospital and M S Ramaiah Memorial Hospital between 1st May 2010 and 1st May 2015 was done. Data was collected using a pre designed format and analysis was done with Libreoffice ver. 5.0.2.2 Spreadsheet using inbuilt statistical formulae at statistical level of significance of 0.05. Care was taken to maintain patient confidentiality.
Surgical Procedure
Conventional tracheostomy was performed with a midline vertical skin incision extending from 5 mm below the lower border of the cricoid till about 5 mm above the suprasternal notch. Midline blunt dissection was extended through the fascia and between the strap muscle fibres to reach the pretracheal fascia. Horizontal exposure as required up to the carotid sheath was achieved with retraction using Langenbeck retractors.
With the minimally invasive procedure, small horizontal skin incision about the same width as the trachea (about 25–30 mm) was placed midway between the lower border of the cricoid and the suprasternal notch (Fig. 1: showing a short horizontal incision with strap muscle retraction with retractors). Sharp dissection was extended till the superficial cervical fascia and blunt dissection was thereafter used in the midline. Vertical dissection was limited to the width of the extended tips of a mosquito artery foreceps—about 2 cm in length. Strap muscles were retracted with Langenbeck retractors.
Fig. 1.

Tracheal stoma through short horizontal incision
With both techniques, the thyroid isthmus was dissected from the trachea and retracted superiorly with a blunt cricoid hook and tracheotomy was completed with a horizontal inter cartilaginous incision placed approximately between 2nd and 4th tracheal rings. An appropriately sized portex blue line tracheostomy tube was used in all cases which was later secured to the skin with sutures. Haemostasis was achieved with pressure and monopolar diathermy where required.
The conventional technique required two to three skin sutures to close the incision around the tube. With the minimally invasive method, the tube fit snugly into the skin wound without surrounding skin gaping, and no skin sutures were used.
Prior to planned decannulation, a trial of capping was given with a fenestrated or small sized tube and where possible fibre-optic laryngoscopy was done. Decannulation was done in the OPD or ward followed by skin strapping with adhesive tape.
Results
Records of eighty-seven patients were found and analysed. Fifty-three patients had undergone surgical tracheostomy by conventional technique (CT); and thirty-four by minimally invasive (MT) as described above.
There were 67 male and 20 female patients: a male: female ratio of 3.35:1. Male: female ratio for CT group was 4.89:1, and for the MT group was 2.1:1. There was no significant difference in the gender distribution of both groups (Χ2 = 2.77, P = 0.096).
There was significant difference in the age distribution of the two groups (t = 4.03, P = 0.0003144). However, the mean difference in age was 6.06 years with mean age of CT group being 55.64 years and MT group being 51.97 years.
There was a significant difference in the weight distribution of the participants of the two groups (t = 2.85, P = 0.0074), with the patients of the CT group being heavier (mean wt = 66.49 kg) than the MT group (mean wt = 58.76 kg).
Twelve participants (22.6 %) in the CT group were documented by the surgeon to have a short neck, whereas three (8.8 %) in the MT group were documented to have a short neck; there was no statistically significant difference (X2 = 2.77, P = 0.096).
Eleven participants (20.8) in the CT group were documented to have a coagulation disorder (INR > 1.4), whereas three in the MT group (8.8 %) were documented to have a coagulation problem; there was no statistically significant difference (X2 = 2.18, P = 0.139).
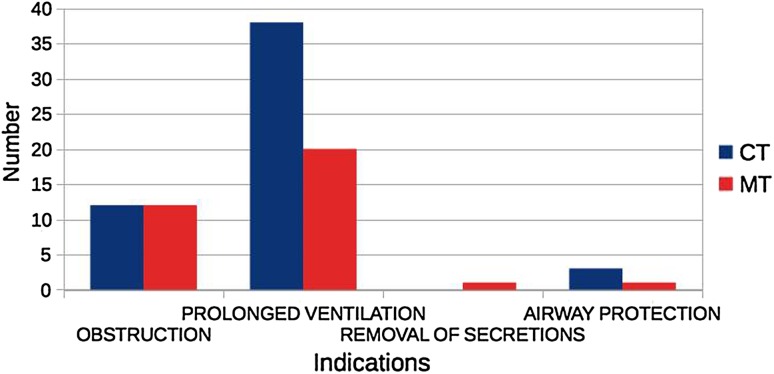
There was no statistical significance in the indications for the tracheostomy (X2 = 3.61, P = 0.306) (Fig. 2: Shows the prevalence of indications for tracheostomy for each group). The commonest indication was for prolonged ventilatory therapy followed by obstruction of the upper airway.
Fig. 2.
Indications for tracheostomy
There was not much difference in the mean operative time (22.87 min for CT and 22 min for MT group).
Three patients in each group (CT = 5.5 %, MT = 8.1 %) were documented to have intra operative complications, the difference was not statistically significant. (X2 = 0.32, P = 0.57). With the MT group, the complications were difficult insertion and false tract passage in 2 patients, and bleeding while insertion of the tube in 1 patient. With the CT Group, one patient had pneumothorax, one had bleeding from the thyroid isthmus and one had difficulty in tube insertion.
Ten patients in the CT group (18.87 %) and three (8.82 %) in the MT group were documented to have early post operative complications (<48 h). The difference was not statistically significant (X2 = 1.64, P = 0.2). Of the ten patients in the CT group, two patients had tracheostomy tube block, four had minimal peristomal bleed controlled by pressure and four had peristomal surgical emphysema which responded to conservative management. In the MT group, one patient had peristomal surgical emphysema, one had peristomal minimal bleed and one had neck cellulitis—all of which responded to conservative management.
Four patients in the CT group (7.5 %) and five (14.7 %) in the MT group had late complications (>48 h)—the difference was statistically insignificant (X2 = 1.14, P = 0.28). The complications of the CT group were skin gaping, stoma necrosis, stoma infection and granulation. The complications of the MT group were one each of tube block, delayed onset surgical emphysema, peristomal skin radionecrosis, pneumonia and peristomal infection.
At the time of data collection, 18 (33.96 %) participants in the CT group and 9 (26.5 %) participants in the MT group were dead. The difference between the groups was not significant (X2 = 0.54, P = 0.46).
Among the survivors, we could decannulate 10 (28.5 %) in the CT group and 11 (44 %) in the SH group. The difference was not statistically significant (X2 = 0.95, P = 0.33). The remaining participants either continued with tracheostomy or did not follow up.
Discussion
The group which had undergone conventional tracheostomy had a statistically significant higher mean age (mean difference of about 6 years)—however only adults were included in the study and paediatric tracheostomies which require significant modification of technique were not included. Hence, there is no variation of technique due to age of the patients.
There was significant difference in the mean weight—the mean difference being about 7.75 kg more in the CT group. It is possible that technical difficulties were increased due to thick neck and obesity in the group which underwent conventional tracheostomy compared to the minimally invasive group. It is also possible that there might have been a surgeon selection bias towards conventional method when the patient was obese. This problem is difficult to avoid as the selection of surgical techniques is highly individualized, and the advantages of better exposure with conventional technique may possibly guide the surgeon to choose this technique in the situation of morbid obesity; the principle of ‘primum non nocere’ may lead the surgeon towards conventional tracheostomy in these difficult situations. Documentation of body mass index and neck circumference may permit better statistical result.
There was no statistical difference in the preoperative documentation of short neck and coagulation disorder in both groups, and both techniques could be applied in these groups. However, better analysis could be obtained in these technically difficult cases as more number of surgeries are performed in such individuals.
In this study, indications for tracheostomy were grouped into four viz. airway obstruction, prolonged ventilation, retained secretion and protection from aspiration. The most relevant indication was taken into consideration when more than one was applicable. There was no variation of surgical technique or selection of tube size based on the indication. Hence there is no possibility of selection bias based on indication.
Since the study is focused on elective surgical tracheostomy, the majority of surgeries were performed in the operating theatre on intubated or sedated patients under anaesthetist’s care. Separate analysis for local versus general anaesthesia has not been performed. There was no variation of technique for tracheostomies performed under local or general anaesthesia. Hence, preference of anaesthesia was unlikely to affect the result.
There was no significant change in the mean operative time for both the techniques. The minimally invasive technique was possibly about a minute faster than the conventional technique. Whereas the conventional surgical method possibly reduces tube insertion time, the minimally invasive technique probably reduces time spent on skin suturing and tissue dissection.
While there was no difference in the prevalence of intra operative complications, the complications associated with minimally invasive method were mostly due to difficulty in insertion of the tracheostomy tube; whereas, the intraoperative complications with the conventional technique were problems associated with wide dissection—such as bleeding and pneumothorax.
Although there was no statistically measurable difference, the early post operative complications were more with conventional tracheostomy (18.87 vs 8.82 %). The complications with the conventional technique were probably related to wide dissection—mainly peristomal bleeding and surgical emphysema.
The late complications with the conventional technique were related to peristomal wound healing—like skin gaping, stoma necrosis—and were also probably related to wider dissection; whereas the late complications with minimally invasive technique were fewer but with a tendency towards infection being the common problem. However, no statistically significant difference could be calculated.
Percutaneous tracheostomy has been reported to reduce peristomal and skin inflammation and provide better tracheostomal result [7, 8]. Percutaneous tracheostomy has also been reported to give better cosmetic healing of the skin compared with conventional open surgical tracheostomy [15, 16]. As minimally invasive open surgical tracheostomy also reduces peristomal problems, and combines with it the advantages of surgical tracheostomy, it may provide an effective middle ground between these two techniques. Comparison between percutaneous techniques and minimally invasive technique is required.
Although there was a 31.03 % mortality among the study group during the study period, there was no statistically significant difference between the two groups. There was also a 35 % decannulation rate among the survivors with no significant differences between the groups. It is likely that the choice of surgical technique did not impact decannulation or death rates.
Although we did not analyse the cosmetic appearance of the scar following decannulation in this study, we observed that minimally invasive tracheostomy with short horizontal skin incision usually healed with a small horizontal linear scar without significant puckering or irregularity (Fig. 3: Post decannulation photograph shows a hyperpigmented small horizontal scar).
Fig. 3.

Early post decannulation scar
We did not analyse intratracheal scarring in this study, but we anticipate no differences since the same intercartilaginous tracheal wall incision was used as a tracheotomy technique in both groups.
These statistics correspond with the reported data from other studies [17]. Hence there is correlation of the result with that obtained at other centres with experience in open surgical tracheostomy.
The procedure of minimally invasive tracheostomy described in this paper was performed with standard surgical tracheostomy instruments and tracheostomy tubes. Hence, the need for additional equipment, training, experience or cost are not barriers for the adoption of this technique.
The study design was a retrospective observational study. All available records of the patients who underwent elective open surgical tracheostomy by the first and second authors during the study period were analysed. Therefore, there is a possibility of statistical bias due to the non random nature of sampling. In addition, errors of available documentation could not be identified. As widely known, better statistical utility can be obtained by performing an appropriately blinded randomized controlled prospective trial.
Conclusion
Although the group which underwent conventional tracheostomy was older and heavier than the group for which minimally invasive approach was used, we feel that there is unlikely to be a bias in the result obtained. The patterns of intra and post operative complications reflected the choice of the surgical technique—the conventional technique had problems associated with wide dissection like bleeding, surgical emphysema and wound gaping, whereas the minimally invasive technique had problems associated with limited exposure for manipulation like difficulty of passage of the tube and false tract. Problems of wound gaping, emphysema and peristomal inflammation were reduced with minimally invasive technique with short horizontal skin incision although statistical difference could not be shown. There was no difference with either technique regards death and decannulation rates. Minimally invasive technique of elective open surgical tracheostomy was found to be as safe as conventional open surgical tracheostomy with midline vertical skin incision in the studied groups. With increasing experience with minimally invasive tracheostomy, it is hoped to further enhance the safety of the procedure and improve the statistical data with regards to high risk groups like obese, patients with neck restriction, elderly and those with bleeding tendency.
Compliance with Ethical Standards
Conflict of interest
Rajiv Ranganath Sanji, Chandrakiran Channegowda and Sanjay B. Patil authors declare that they have no conflicts of interest.
Ethical Approval
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Dash AK, Meher D, Patro S, et al. Benign thyroid lesions: small incision hemithyroidectomy is a cosmetic alternative. Natl J Otorhinolaryngol Head Neck Surg. 2014;2(11):21–22. [Google Scholar]
- 2.Henry J. Minimally invasive thyroid and parathyroid surgery is not a question of length of the incision. Langenbecks Arch Surg. 2008;393:621–626. doi: 10.1007/s00423-008-0406-3. [DOI] [PubMed] [Google Scholar]
- 3.Terris DJ, Seybt MW. Classification system for minimally invasive thyroid surgery. ORL. 2008;70:287–291. doi: 10.1159/000149830. [DOI] [PubMed] [Google Scholar]
- 4.Consorti F, Milazzo F, Notarangelo M, et al. Factors influencing the length of the incision and the operating time for total thyroidectomy. BMC Surg. 2012;12:15. doi: 10.1186/1471-2482-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng K-H, Chen C-H, Ho C, et al. A fast method of surgical tracheostomy: a preliminary result of minimally invasive tracheostomy. Arch Clin Exp Surg. 2015;4:36–40. doi: 10.5455/aces.20140324123308. [DOI] [Google Scholar]
- 6.Goldman RK. Minimally invasive surgery. Bedside tracheostomy and gastrostomy. Crit Care Clin. 2000;16:113–130. doi: 10.1016/S0749-0704(05)70100-7. [DOI] [PubMed] [Google Scholar]
- 7.Putensen C, Theuerkauf N, Guenther U, et al. Percutaneous and surgical tracheostomy in critically ill adult patients: a meta-analysis. Crit Care. 2014;18:544. doi: 10.1186/s13054-014-0544-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Delaney A, Bagshaw SM, Nalos M. Percutaneous dilatational tracheostomy versus surgical tracheostomy in critically ill patients: a systematic review and meta-analysis. Crit Care. 2006;10:R55. doi: 10.1186/cc4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravi Kumar A, Mohanty KS, Senthil MG. Comparative study of percutaneous dilatational tracheostomy and conventional tracheostomy in the intensive care unit. Indian J Otolaryngol Head Neck Surg. 2005;57:202–206. doi: 10.1007/BF03008014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El Solh AA, Jaafar W. A comparative study of the complications of surgical tracheostomy in morbidly obese critically ill patients. Crit Care. 2007;11:R3. doi: 10.1186/cc5147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marullo L, Izzo G, Orsini A, et al. Clinical features as discriminating factors in the choice of tracheostomy techniques. BMC Surg. 2013;13:A28. doi: 10.1186/1471-2482-13-S1-A28. [DOI] [Google Scholar]
- 12.Pelosi P, Severgnini P. Tracheostomy must be individualized! Crit Care Lond. 2004;8:322–324. doi: 10.1186/cc2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pracy P (2008) Tracheostomy. In: Browning GG, Gleeson M, Burton MJ (eds) Scott brown’s otorhinolaryngology, Head and neck surgery, 7th Edn. Hodder Arnold, UK, pp 2295–2298
- 14.Bovie MJ, Afifi MS (2010) Tracheostomy procedure. In: CCNS DLM PhD, APN, FCCP DMSA MD, FCCM (eds) Tracheostomies: the complete guide, 1st edn. Springer Publishing Company, Berlin, pp 25–37
- 15.Dulguerov P, Gysin C, Perneger TV, Chevrolet J-C. Percutaneous or surgical tracheostomy: a meta-analysis. Crit Care Med. 1999;27(8):1617–1625. doi: 10.1097/00003246-199908000-00041. [DOI] [PubMed] [Google Scholar]
- 16.Dulguerov P, Gysin C. Is surgical tracheostomy really superior to percutaneous tracheostomy? Crit Care Med. 2000;28:3370–3371. doi: 10.1097/00003246-200009000-00056. [DOI] [Google Scholar]
- 17.Gilyoma JM, Balumuka DD, Chalya PL. Ten-year experiences with tracheostomy at a University teaching hospital in Northwestern Tanzania: a retrospective review of 214 cases. World J Emerg Surg. 2011;6:38. doi: 10.1186/1749-7922-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]