Abstract
Objectives
To examine the association between multisite musculoskeletal pain in adolescence and mental health disorders in young adulthood.
Design and setting
Data were obtained from a linkage between the Norwegian Patient Registry (2008–2012) and the Norwegian Arctic Adolescent Health Study, a school-based survey conducted among 10th grade students in North Norway (2003–2005).
Participants
In total, 3987 (68%) of all 5877 invited participants consented to the registry linkage.
Outcome measures
Mental healthcare use and disorders from age 18–20 to 23–25 years (5 years).
Methods
Musculoskeletal pain was measured by the number of musculoskeletal pain sites. Multivariable logistic regression was used to explore the association with later mental healthcare use and disorders.
Results
Multisite adolescent musculoskeletal pain was significantly associated with an increase in mental healthcare use and mental health disorders in young adulthood. The relationship was stronger for anxiety and mood disorders, in both genders. Overall, the association between musculoskeletal pain and later mental health problems was attenuated after controlling for adolescent psychosocial and mental health problems, not by physical or sedentary activity. This could be due to confounding or mediation. However, when examining different mental health disorders, we found musculoskeletal pain to be significantly associated with anxiety disorders, and showing a strong trend in mood disorders, when adjusted for the adolescent factors.
Conclusions
Physicians should be aware that multisite adolescent pain is associated with mental health problems in adolescence, and that these adolescents are at increased risk of mental health disorders in young adulthood. As youth troubled by mental health problems commonly present physical symptoms it is important to examine for psychosocial problems in order to offer early interventions.
Keywords: PSYCHIATRY, MENTAL HEALTH, PUBLIC HEALTH, EPIDEMIOLOGY
Strengths and limitations of this study.
The main strength of this study is the linkage of a large population-based study in adolescents (2003–2005) to the Norwegian Patient Registry (2008–2012).
This study linkage was used to explore the association between multisite musculoskeletal pain in adolescence and mental health disorders in young adulthood.
Psychosomatic problems are complex, and with only one cross-sectional study linked to the patient registry there might be other factors influencing the associations found in this study.
The adolescent population study relied on self-reports with the risk of information bias.
The Norwegian Patient Registry had few logical errors, but it was not possible to differentiate between primary and secondary diagnoses of mental health disorders.
Introduction
Musculoskeletal pains are prevalent in adolescents,1–3 with an increasing trend in recent decades.4 5 Pain problems in youth tend to persist into adulthood,6 7 and multisite pain is more associated with psychosocial problems than single-site pain is.2 3 8 9 Pain in adolescents has been shown to be associated with psychosocial and mental health problems in cross-sectional3 10 11 and longitudinal12–17 studies. Longitudinal studies in adolescents have shown overall a bidirectional relationship between pain and mental health problems.12–17 Except for the recent findings presented by Shanahan et al16 most of the studies are of a shorter timeframe18 and do not examine this relationship beyond adolescence.
Multiple physical symptoms are strongly associated with mental health disorders, especially mood and anxiety disorders, influencing the clinical picture of these disorders.11 19–22 Comorbid physical symptoms are a common way of presenting mental health problems in a clinical setting,20–22 and may be an important sign in the early detection of mental health problems.19 22 23 Shanahan et al16 found pain in children and adolescents to be predictive of mood and anxiety disorder in young adulthood, and youth with persistent pain were at increased risk of later mental health problems. Adolescents are generally a physically healthy group, and the influence of potential adolescent mediators on the relationship between adolescent pain and adult mental health problems needs to be examined further.16
Adolescence and young adulthood can be a challenging period and the age of mental illness onset.24 25 Chronic pain and mental health disorders are two major public health issues. They are costly to young people's2 26 27 and their families' quality of life,27 28 and to society.24 26 29 30 Therefore, early detection and interventions are of major importance. In order to investigate the relationship between adolescent musculoskeletal pain and mental health problems in young adulthood we linked the Norwegian Patient Registry31 section on specialised mental healthcare with a population-based study, the Norwegian Arctic Adolescents Health Study.32
The aim of this study was to investigate whether multisite musculoskeletal pain in adolescents was associated with mental health problems in young adulthood in an unselected community sample. Second, to determine the importance of musculoskeletal pain in relation to later mental healthcare use and mental health disorders, when adjusting for adolescent psychosocial factors. Third, we wanted to explore differences in the potential association between adolescent musculoskeletal pain and different mental health disorders.
Methods
Study design
The Norwegian Arctic Adolescent Health Study (NAAHS)32 was conducted among 10th graders (15–16 years old) in nearly all junior high schools (292 of 293) in the three northernmost counties in Norway, in 2003–2005. The questionnaires were administered in classroom settings by the project staff, and completed during two school hours. Students who were absent completed the questionnaire at a later date. There were no specific exclusion criteria in this study.
The participants from the NAAHS were linked to the Norwegian Patient Registry (NPR),31 a detailed registry from 2008 that includes personal identification of specialised healthcare usage and diagnosis. We used available data from specialised mental healthcare from 2008 to 2012 when the participants were 18–20 to 23–25 years of age.
Sample
In total, 4881 of 5877 (83%) invited students responded to the NAAHS, and 3987 (82%) consented to a future registry linkage, resulting in a 68% sample of all 10th grade students in Northern Norway. The registry sample consisted of 49.9% women and 9.2% indigenous Sami.
In order to explore the representativeness of the proportion of mental healthcare users in our sample (68% of the total population), the NPR calculated the total number of mental healthcare users in Northern Norway with the same age and registration period as the study sample. The total number of patients (n=850) was compared to the total population data from Statistics Norway public database (n=5715) to give and approximate cumulative prevalence of mental healthcare users in the total population, which we compared our sample to.
The Norwegian Arctic Adolescent Health Study
Physical factors
Musculoskeletal pain was measured by ‘yes/no’ answers to the question: “During the past 12 months have you often been troubled by pain in the head, neck/shoulder, arms/legs/knees, abdomen or back?” Abdominal pain was excluded due to the potential confusion with menstrual pain,3 resulting in 0–4 musculoskeletal pain sites.
Pain-related functional impairment was present if the participants reported reduced activity during leisure time due to pain (yes/no).
Physical activity was measured by the question: “How many hours per week do you spend on physical activity, to an extent that makes you sweat and/or out of breath?” Possible answers: 0, 1–4, 5–7 and ≥8 hours per week.33
Sedentary activity was measured by the question: “After school hours: How many hours per school day (Monday to Friday) do you spend in front of a TV, video and/or PC?” Possible answers: <1, 1–2, 3–5 or >5 hours.
Psychosocial supportive factors
Self-efficacy was measured by a five-item version (α=0.77) of the General perceived self-efficacy scale34 with higher scores indicating higher self-efficacy. Responses were scored on a four-point Likert scale from ‘completely wrong’ to ‘completely right’.
Parental involvement was measured by a four-item version of the Parental Involvement scale (α=0.78).3 35
Parental support (α=0.88) was measured by five statements on family attachment, being valued and taken seriously, and receiving help when needed.3
Peer support (α=0.84) was measured by four statements on peer attachment and support, being valued, and receiving help when needed.3
Parental involvement, parental and peer support were scored on a four-point Likert scale from ‘completely agree’ to ‘completely disagree’.
Psychosocial life stressor factors
School-related stress (α=0.66) was measured by the following four experiences: work pressure, pressure to succeed, concentration difficulties and understanding the teacher.3 Responses were scored on a three-point scale from ‘no’ to ‘yes, often’.
Adverse life events such as parental drug problems, bullying and assault were measured by 12 dichotomised questions previously described by Eckhoff and Kvernmo.3
Psychosocial mental health factors
Mental health was examined by anxiety/depression symptoms measured by the Hopkins Symptom Checklist 10-item version (HSCL-10).36 The HSCL-10 (α=0.87) measures symptoms in the previous week. Psychometrics has been validated among participants aged 16–24 years37 with a cut-off of 1.85 indicating a presence of emotional distress.
Help seeking
The use of a psychiatrist/psychologist during the previous year was dichotomised (yes/no) from the responses ‘no’, ‘1–3 times’ and ‘4 or more times’.
Sociodemographic factors
Parental education
Parents' highest education was obtained from Statistics Norway's education registry, registered when the participants were 15–16 years old. Parental education was categorised from ‘lower secondary’ (≤10th grade), ‘upper secondary’ (≤13th grade), ‘lower university degree’ (up to 5 years) to ‘higher university degree’ (5 years or more).38
Family income
Adolescents reported their family's economic situation compared to other families on a four-point scale from ‘not well off’ to ‘very well off’.
Sami ethnicity
Was measured by participants having one or more of the following factors: Sami parentage and Sami language competence in parents, grandparents and the participants, and Sami ethnic self-labelling.
Mental healthcare registry
Mental healthcare users consisted of participants found in the specialised psychiatric patient registry, including use of public psychiatric healthcare and private specialists. We constructed an ordinal variable of ‘not a patient’, ‘outpatient only’ and ‘inpatient’.
The number of outpatient contacts and inpatient admissions, and the sum of all outpatient treatment hours and inpatient treatment days were calculated.
Mental health disorders
Each participant's primary and secondary diagnoses were organised according to the main chapters in the International Classification of Diseases 10th Revision (ICD-10).39 We used a classical model for psychiatric diagnoses to achieve theoretically constructed groups of reasonable size. We recorded whether the participants had received a diagnosis from any of the five diagnostic groups: substance use disorders (F10–19), psychotic (F20–29), mood (F30–39), anxiety (F40–49), developmental and behavioural disorders (F50–98), and undiagnosed. We included both primary and secondary diagnoses due to an evident difference in diagnostic coding practice, making it difficult to pick out the primary disorder in patients with several diagnoses. Patients with two or more diagnoses from the ICD-10 main chapters were: two=102, three=42, four=32 and five diagnostic chapters=22.
Data analysis
The means of the explanatory factors were examined in the registry sample, the original NAAHS sample3 and in the participants not accepting the registry linkage (non-registry sample). We found no significant difference between the registry sample and the non-registry sample (n=894) except for a slightly lower mean of adverse life events in the non-registry sample (see online supplementary table S1). The non-registry sample was not worse off. χ2 Tests and one-way ANOVA were used for the univariate analyses. Anxiety/depression (HSCL-10) was handled continuously in the multivariable analyses.
bmjopen-2016-012035supp_table.pdf (54KB, pdf)
Initially we examined the prediction of later mental healthcare by ordinal and multinomial regression. However, we found no linearity between the constructed ordinal groups. The main statistical difference was between the users and non-users of mental healthcare, and not between the user groups (outpatient only vs inpatients). We therefore present multivariable logistic regression results on mental healthcare users versus no mental healthcare users.
Hierarchical logistic regression was used for the multivariable analysis for later mental healthcare use (table 3). In step 1 the sociodemographic factors (model 1), physical factors (model 2: musculoskeletal pain, adjusted for sedentary and physical activity) and psychosocial factors (model 3, 4 and 5) were analysed grouped together in models based on their respective characteristic groups. Factors that were not statistically significant, at a predefined cut-off of p<0.05, were not included in the next steps in order to simplify the models. In step 2, the significant sociodemographic factors from model 1 were added as adjustments for musculoskeletal pain alongside physical activity (model 6). The significant psychosocial factors from step 1 were analysed together in model 7. In the final model, the significant psychosocial factors from the second step (model 7) were added to the adjustment of adolescent musculoskeletal pain.
Table 3.
The association between adolescent musculoskeletal pain and mental healthcare use* in young adulthood, adjusted for adolescent sociodemographic, physical and psychosocial factors (Final model: n=3302)
| Mental healthcare use in young adulthood | ||
|---|---|---|
| Adolescent factors | n | OR (95% CI)/R2 |
| Step 1: | ||
| Model 1—sociodemographic: | 3583 | R2=0.026 |
| Female gender | 1.47 (1.21 to 1.79)p<0.001 | |
| Sami | 0.86 (0.61 to 1.20)p=0.372 | |
| Higher parental education | 0.89 (0.78 to 1.00)p=0.051 | |
| Family income | 0.68 (0.59 to 0.78)p<0.001 | |
| Model 2—physical: | 3602 | R2=0.041 |
| Musculoskeletal pain | 1.27 (1.18 to 1.37)p<0.001 | |
| Sedentary activity | 0.99 (0.89 to 1.11)p=0.909 | |
| Physical activity | 0.72 (0.64 to 0.80)p<0.001 | |
| Psychosocial factors: | ||
| Model 3—supportive: | 3790 | R2=0.037 |
| Self-efficacy | 0.91 (0.88 to 0.94)p<0.001 | |
| Parental involvement | 1.02 (0.98 to 1.07)p=0.320 | |
| Parental support | 1.07 (1.04 to 1.11)p<0.001 | |
| Peer support | 1.05 (0.99 to 1.09)p=0.053 | |
| Model 4—life stressors: | 3703 | R2=0.046 |
| School-related stress | 1.18 (1.12 to 1.24)p<0.001 | |
| Adverse life events | 1.14 (1.08 to 1.20)p<0.001 | |
| Model 5—mental health: | 3876 | R2=0.060 |
| Anxiety/depression | 2.51 (2.15 to 2.93)p<0.001 | |
| Step 2: | ||
| Model 6 (1+2)—sociodemographic and physical: | 3572 | R2=0.058 |
| Female gender | 1.25 (1.02 to 1.53)p=0.036 | |
| Family income | 0.68 (0.59 to 0.79)p<0.001 | |
| Musculoskeletal pain | 1.24 (1.15 to 1.34)p<0.001 | |
| Physical activity | 0.75 (0.67 to 0.84)p<0.001 | |
| Model 7 (3+4+5)—psychosocial: | 3578 | R2=0.066 |
| Self-efficacy | 0.96 (0.92 to 0.99)p=0.026 | |
| Parental support | 1.02 (0.99 to 1.06)p=0.182 | |
| School-related stress | 1.10 (1.04 to 1.17)p=0.001 | |
| Adverse life events | 1.07 (1.01 to 1.13)p=0.029 | |
| Anxiety/depression | 1.64 (1.33 to 2.02)p<0.001 | |
| Step 3/final model† (model 6+7): | 3302 | R2=0.081 |
| Female gender | 1.01 (0.80 to 1.27)p=0.965 | |
| Family income | 0.76 (0.65 to 0.90)p=0.001 | |
| Musculoskeletal pain | 1.05 (0.96 to 1.15)p=0.329 | |
| Physical activity | 0.79 (0.69 to 0.89)p<0.001 | |
| Self-efficacy | 0.98 (0.94 to 1.02)p=0.326 | |
| School-related stress | 1.07 (1.01 to 1.14)p=0.024 | |
| Adverse life events | 1.06 (0.99 to 1.13)p=0.055 | |
| Anxiety/depression | 1.63 (1.29 to 2.07)p<0.001 | |
Statistical analyses: hierarchical logistic regression.
*Patient data from the Norwegian Patient Registry.
†Bonferroni adjusted significance level 0.0063 for the final model.
Hierarchical logistic regression was used for the multivariable analyses on the diagnostic groups of mental health disorders (table 4), following the same model building approach as described above. However, only the significant factors from step 1 in the mental healthcare use model were examined in order to simplify the models. In addition, musculoskeletal pain, physical activity and the sociodemographic factors were included in the final model regardless of whether they were found insignificant in step 1 and 2 (model 1, 2 and 6), while insignificant psychosocial factors from model 7 were excluded.
Table 4.
The association between adolescent musculoskeletal pain and mental health disorders* in young adulthood, adjusted for adolescent sociodemographic, physical and psychosocial factors (Final model: n=3464)
| Mood n=165 |
Anxiety n=201 |
Developmental and behavioural n=130 |
Undiagnosed n=129 | ||
|---|---|---|---|---|---|
| Adolescent factors | n | OR (95% CI)/R2 | |||
| Step 1: | |||||
| Model 1—sociodemographic: | 3918 | R2=0.032 | R2=0.034 | R2=0.024 | R2=0.002 |
| Female gender | 1.88 (1.35 to 2.61)p<0.001 | 2.04 (1.50 to 2.77)p<0.001 | 1.74 (1.20 to 2.53)p=0.003 | 1.12 (0.78 to 1.60)p=0.546 | |
| Family income | 0.60 (0.47 to 0.75)p<0.001 | 0.63 (0.51 to 0.78)p<0.001 | 0.62 (0.48 to 0.80)p<0.001 | 0.84 (0.64 to 1.09)p=0.190 | |
| Model 2—physical: | 3618 | R2=0.062 | R2=0.043 | R2=0.022 | R2=0.008 |
| Musculoskeletal pain | 1.36 (1.20 to 1.54)p<0.001 | 1.43 (1.28 to 1.61)p<0.001 | 1.29 (1.12 to 1.49)p<0.001 | 1.14 (0.98 to 1.31)p=0.084 | |
| Physical activity | 0.54 (0.44 to 0.67)p<0.001 | 0.75 (0.63 to 0.90)p=0.001 | 0.78 (0.63 to 0.97)p=0.022 | 0.81 (0.65 to 1.00)p=0.051 | |
| Psychosocial factors: | |||||
| Model 3 –supportive: | 3892 | R2=0.016 | R2=0.029 | R2=0.024 | R2=0.003 |
| Self-efficacy | 0.88 (0.83 to 0.93)p<0.001 | 0.85 (0.81 to 0.89)p<0.001 | 0.85 (0.80 to 0.91)p<0.001 | 0.95 (0.89 to 1.01)p=0.111 | |
| Model 4—life stressors: | 3703 | R2=0.033 | R2=0.032 | R2=0.025 | R2=0.025 |
| School-related stress | 1.24 (1.14 to 1.35)p<0.001 | 1.22 (1.13 to 1.31)p<0.001 | 1.18 (1.07 to 1.31)p=0.001 | 1.14 (1.04 to 1.25)p=0.008 | |
| Adverse life events | 1.07 (0.97 to 1.17)p=0.169 | 1.08 (0.99 to 1.17)p=0.066 | 1.11 (1.00 to 1.23)p=0.044 | 1.15 (1.04 to 1.27)p=0.005 | |
| Model 5—mental health: | 3876 | R2=0.050 | R2=0.062 | R2=0.033 | R2=0.010 |
| Anxiety/depression | 2.62 (2.07 to 3.31)p<0.001 | 2.81 (2.28 to 3.48)p<0.001 | 2.27 (1.75 to 2.95)p<0.001 | 1.64 (1.23 to 2.20)p=0.001 | |
| Step 2: | |||||
| Model 6 (1+2)—sociodemographic and physical: | 3572 | R2=0.082 | R2=0.058 | R2=0.038 | R2=0.011 |
| Female gender | 1.63 (1.13 to 2.36)p=0.009 | 1.51 (1.09 to 2.11)p=0.015 | 1.66 (1.10 to 2.15)p=0.015 | 1.01 (0.68 to 1.51)p=0.954 | |
| Family income | 0.64 (0.50 to 0.82)p<0.001 | 0.68 (0.54 to 0.85)p=0.001 | 0.63 (0.48 to 0.83)p=0.001 | 0.83 (0.62 to 1.10)p=0.198 | |
| Musculoskeletal pain | 1.29 (1.14 to 1.47)p<0.001 | 1.36 (1.21 to 1.53)p<0.001 | 1.19 (1.03 to 1.38)p=0.018 | 1.12 (0.97 to 1.30)p=0.135 | |
| Physical activity | 0.58 (0.47 to 0.72)p<0.001 | 0.80 (0.67 to 0.96)p=0.016 | 0.86 (0.69 to 1.07)p=0.184 | 0.81 (0.65 to 1.02)p=0.068 | |
| Model 7 (3+4+5) –psychosocial: | 3803 | R2=0.061 | R2=0.071 | R2=0.046 | R2=0.025 |
| Self-efficacy | 0.96 (0.90 to 1.02)p=0.175 | 0.92 (0.87 to 0.97)p=0.003 | 0.88 (0.82 to 0.95)p=0.001 | – | |
| School-related stress | 1.16 (1.06 to 1.27)p=0.001 | 1.13 (1.04 to 1.22)p=0.005 | 1.09 (0.98 to 1.22)p=0.121 | 1.12 (1.01 to 1.25)p=0.030 | |
| Adverse life events | – | – | 1.05 (0.94 to 1.18)p=0.370 | 1.13 (1.02 to 1.26)p=0.018 | |
| Anxiety/depression | 1.95 (1.46 to 2.60)p<0.001 | 2.00 (1.54 to 2.60)p<0.001 | 1.47 (1.00 to 2.15)p=0.049 | 1.15 (0.79 to 1.69)p=0.464 | |
| Step3/final model† (model 6+7): | 3464 | R2=0.100 | R2=0.079 | R2=0.054 | R2=0.030 |
| Female gender | 1.39 (0.93 to 2.07)p=0.109 | 1.23 (0.86 to 1.75)p=0.267 | 1.35 (0.87 to 2.10)p=0.179 | 0.97 (0.64 to 1.47)p=0.892 | |
| Family income | 0.68 (0.53 to 0.87)p=0.002 | 0.74 (0.59 to 0.94)p=0.012 | 0.72 (0.54 to 0.96)p=0.025 | 0.86 (0.64 to 1.16)p=0.333 | |
| Musculoskeletal pain | 1.13 (0.98 to 1.31)p=0.102 | 1.21 (1.06 to 1.38)p=0.006 | 1.06 (0.91 to 1.25)p=0.450 | 0.98 (0.83 to 1.16)p=0.811 | |
| Physical activity | 0.62 (0.49 to 0.77)p<0.001 | 0.86 (0.72 to 1.04)p=0.112 | 0.93 (0.74 to 1.17)p=0.535 | 0.84 (0.67 to 1.05)p=0.131 | |
| Self-efficacy | – | 0.95 (0.89 to 1.01)p=0.077 | 0.92 (0.85 to 0.99)p=0.026 | – | |
| School-related stress | 1.08 (0.98 to 1.20)p=0.138 | 1.04 (0.95 to 1.14)p=0.380 | – | 1.15 (1.04 to 1.28)p=0.010 | |
| Adverse life events | – | – | – | 1.13 (1.01 to 1.26)p=0.036 | |
| Anxiety/depression | 1.69 (1.20 to 2.37)p=0.002 | 1.70 (1.24 to 2.34)p=0.001 | 1.68 (1.17 to 2.39)p=0.005 | – | |
Statistical analyses: hierarchical logistic regression.
*Patient data from the Norwegian Patient Registry.
†Bonferroni adjusted significance level 0.0083 for the final model of mood, developmental and behavioural disorder, and 0.0071 for anxiety disorders.
All analyses were conducted with SPSS V.21 (IBM software).
Results
In our sample, 21.3% reported two, 13.3% three and 8.9% four musculoskeletal pain sites (table 2). The proportion of mental healthcare users was 13.6% (59.5% women) (table 1), in comparison to 14.9% (850 of 5715) in the total population age cohort.
Table 2.
The number of adolescent musculoskeletal pain sites, by gender and the association with mental healthcare use*, mental healthcare treatment and mental health disorders in young adulthood
| Number of adolescent musculoskeletal pain sites |
|||||||
|---|---|---|---|---|---|---|---|
| Factors (n/%/mean) | n | 0 | 1 | 2 | 3 | 4 | χ2/F-ratio |
| Pain by gender: | 121.42p<0.001 | ||||||
| Females (n (%)) | 1843 | n=395 (21.4) | n=494 (26.8) | n=433 (23.5) | n=314 (17.0) | n=207 (11.2) | |
| Males (n (%)) | 1877 | n=638 (34.0) | n=576 (30.7) | n=359 (19.1) | n=181 (9.6) | n=123 (6.6) | |
| Mental healthcare users (%): | |||||||
| Females | 1843 | 11.1 | 11.3 | 17.3 | 19.7 | 24.2 | 27.28p<0.001 |
| Males | 1877 | 9.2 | 9.5 | 9.2 | 18.8 | 17.9 | 13.32p<0.001 |
| Mental healthcare treatment (M/%): | |||||||
| Total outpatient hours (M) | 3720 | 2.84 | 2.23 | 4.03 | 4.69 | 8.66 | 3.19p=0.013 |
| Inpatients (%) | 3720 | 2.0 | 2.8 | 2.8 | 4.0 | 7.3 | 18.71p<0.001 |
| Total inpatient days (M) | 3720 | 3.08 | 3.11 | 1.36 | 3.71 | 5.97 | 1.36p=0.247 |
| Mental health disorders (%): | |||||||
| Substance use | 3720 | 1.3 | 1.4 | 1.3 | 1.8 | 3.3 | 4.77p=0.029 |
| Psychotic | 3720 | 0.7 | 0.7 | 0.4 | 0.8 | 0.9 | 0.43p=0.835 |
| Mood | 3720 | 2.5 | 2.7 | 4.8 | 6.5 | 7.9 | 29.96p<0.001 |
| Females | 1843 | 3.3 | 2.8 | 7.2 | 8.0 | 8.7 | 16.77p<0.001 |
| Males | 1877 | 2.0 | 2.6 | 1.9 | 3.9 | 6.5 | 5.65p=0.017 |
| Anxiety | 3720 | 2.6 | 3.6 | 5.3 | 8.3 | 10.0 | 44.95p<0.001 |
| Females | 1843 | 3.3 | 4.5 | 7.2 | 8.3 | 11.6 | 20.68p<0.001 |
| Males | 1877 | 2.2 | 2.8 | 3.1 | 8.3 | 7.3 | 16.17p<0.001 |
| Developmental and behavioural | 3720 | 3.0 | 1.9 | 3.0 | 4.6 | 6.7 | 12.85p<0.001 |
| Females | 1843 | 3.8 | 2.4 | 3.7 | 5.7 | 7.2 | 6.94p=0.008 |
| Males | 1877 | 2.5 | 1.4 | 2.2 | 2.8 | 5.7 | 2.47p=0.116 |
| Undiagnosed | 3720 | 2.8 | 2.5 | 2.7 | 4.8 | 3.6 | 3.06p=0.080 |
| Females | 1843 | 2.3 | 2.6 | 3.2 | 4.8 | 4.3 | 4.21p=0.040 |
| Males | 1877 | 3.1 | 2.4 | 1.9 | 5.0 | 2.4 | 0.02p=0.886 |
| Adolescent anxiety/depression symptoms (%): | |||||||
| Yes: | 679 | ||||||
| Mental healthcare users | 156 | 17.6 | 16.4 | 20.7 | 25.3 | 30.3 | 8.84p=0.003 |
| Inpatients | 37 | 2.7 | 4.5 | 5.2 | 5.4 | 7.7 | 2.54p=0.111 |
| No: | 2967 | ||||||
| Mental healthcare users | 325 | 9.6 | 9.6 | 11.4 | 16.1 | 14.6 | 11.06p=0.001 |
| Inpatients | 78 | 2.0 | 2.5 | 2.1 | 3.4 | 6.7 | 7.36p=0.007 |
| Adolescent pain-related functional impairment (%): | |||||||
| Yes: | 1059 | ||||||
| Mental healthcare users | 178 | 0 | 11.2 | 15.9 | 18.8 | 25.4 | 12.78p<0.001 |
| Inpatients | 36 | 0 | 1.6 | 3.5 | 3.2 | 6.5 | 4.04p=0.044 |
| No: | 1650 | ||||||
| Mental healthcare users | 200 | 7.2 | 10.3 | 12.4 | 20.1 | 14.6 | 15.08p<0.001 |
| Inpatients | 55 | 1.4 | 3.3 | 2.6 | 4.5 | 7.3 | 6.55p=0.010 |
Statistical analyses: χ2 analysis (linear-by-linear association) and one-way ANOVA test for trend. Stratified analyses on gender, adolescent anxiety/depression symptoms and adolescent pain-related functional impairment.
*Patient data from the Norwegian Patient Registry.
ANOVA, analysis of variance
Table 1.
Adult mental healthcare use, mental health disorders and treatment in a cohort of adolescents, registry-based data*
| Factors (%/mean) | Females | Males | Total | χ2/F-ratio |
|---|---|---|---|---|
| Total sample (%): | n=1991 | n=1996 | n=3987 | |
| Mental healthcare users | 16.2 | 11.0 | 13.6 | 22.48p<0.001 |
| Inpatient | 3.0 | 3.4 | 3.2 | 0.28p=0.598 |
| Mental health disorders (%): | ||||
| Substance use | 0.9 | 2.3 | 1.6 | 11.51p=0.001 |
| Psychotic | 0.7 | 0.8 | 0.7 | 0.03p=0.855 |
| Mood | 5.5 | 2.8 | 4.1 | 17.23p<0.001 |
| Anxiety | 6.7 | 3.4 | 5.0 | 23.00p<0.001 |
| Developmental and behavioural | 4.2 | 2.4 | 3.3 | 9.83p=0.002 |
| Undiagnosed | 3.5 | 3.0 | 3.2 | 0.53p=0.465 |
| Mental healthcare users (%/mean): | n=323 | n=220 | n=543 | |
| Public mental healthcare (%) | 93.8 | 95.5 | 94.5 | 0.40p=0.527 |
| Private specialist (%) | 16.7 | 9.5 | 13.8 | 5.07p=0.024 |
| Inpatient (%) | 18.6 | 30.5 | 23.4 | 9.65p=0.002 |
| Total outpatient contacts (M) | 27.54 (60.83) | 22.03 (54.56) | 25.31 (58.38) | 1.17p=0.281 |
| Total outpatient hours (M) | 31.53 (83.79) | 21.31 (63.59) | 27.39 (76.35) | 2.35p=0.126 |
| Total inpatient admissions (M) | 0.61 (2.25) | 0.74 (1.59) | 0.66 (2.01) | 0.54p=0.461 |
| Total inpatient days (M) | 17.00 (70.36) | 32.82 (100.98) | 23.41 (84.39) | 4.63p=0.032 |
Statistical analyses: χ2 analysis and one-way ANOVA.
*Patient data from the Norwegian Patient Registry.
ANOVA, analysis of variance.
A calculated approximation of mental healthcare users in our non-registry sample was 17.8% (307 of 1728).
Women reported more musculoskeletal pain (table 2), had more mental healthcare outpatient contacts and total treatment hours, while men had more inpatient admissions and almost double the number of inpatient days (table 1). Anxiety and mood disorders were more prevalent, while 23.8% were undiagnosed. Few of the undiagnosed participants (n=9) were at risk of remaining undiagnosed due being evaluated only at the end of the registration period (the past 3 months). This group had less outpatient treatment (mean=5.25 hours) than the other diagnostic groups (mean=36.46–149.26 hours).
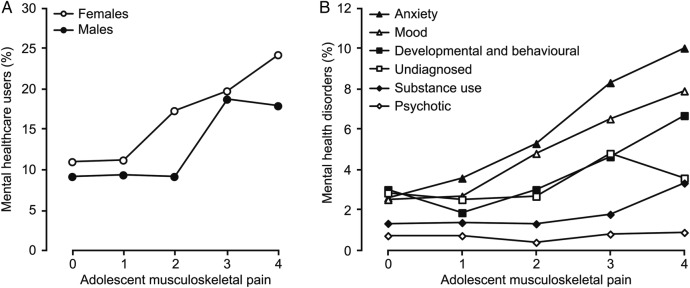
There was a significantly higher proportion of adult mental healthcare users (figure 1) and increased mental healthcare treatment in participants reporting two or more musculoskeletal pain sites in adolescence, even stratified by adolescent anxiety/depression and regardless of pain-related functional impairment (table 2). A higher proportion of mental healthcare users were found in the participants reporting pain-related functional impairment, 17.7% compared to 12.2% in the non-impaired (χ2 (1, n=2900)=16.22, p<0.001). The association with adolescent musculoskeletal pain was stronger in anxiety and mood disorders (figure 1 and table 2).
Figure 1.
χ2 Test for trend. The relationship between the number of adolescent musculoskeletal pain sites and (A) mental healthcare users and (B) mental health disorders (data in table 2).
Table 3 shows the multivariable analysis for the prediction of mental healthcare use in young adulthood, with an 8.1% explained variance for the final model. The unadjusted OR for the association between adolescent musculoskeletal pain and later mental healthcare use was OR=1.30 (1.20 to 1.39), p<0.001.
Adolescent anxiety/depression symptoms, low family income, low physical activity and school-related stress were the significant predictors in the final model. Musculoskeletal pain remained significant in the second step when adjusted for physical activity, gender and family income. However, when we adjusted for psychosocial factors in the final model, then musculoskeletal pain was no longer significantly associated with mental healthcare use in young adulthood. Sami ethnicity was not significant (table 3).
Table 4 presents the multivariable analyses for the included mental health disorders. The final model explained 10.0% of the variance for mood disorders, 7.9% for anxiety disorders and lower explained variance for developmental and behavioural disorders and the undiagnosed. We found some differences in predictors in the final models for the different diagnostic groups, with musculoskeletal pain predicting anxiety disorders adjusted for gender, family income, physical activity and adolescent psychosocial factors (table 4).
In the year prior to the NAAHS, 6.1% of the participants had seen a psychiatrist/psychologist. Of these, 41.7% were registered as mental healthcare users in young adulthood, compared to 11.9% in those who had not seen a psychiatrist/psychologist in adolescence (χ2 (1, n=3936)=166.70, p<0.001).
Discussion
Main findings
We found multisite adolescent musculoskeletal pain to be associated with an increase in mental healthcare use and mental health disorders in young adulthood, in both genders.
Overall, this association was attenuated after controlling for adolescent psychosocial and mental health problems. However, adolescent musculoskeletal pain was associated with later anxiety disorder, when adjusted for adolescent psychosocial problems.
Interpretation of the results and comparison to previous findings
A high proportion of adolescents were found to be mental healthcare users in young adulthood, comparable to national data and with a representative distribution of disorders.40
The significant univariate associations between the number of adolescent musculoskeletal pains and later mental health disorders, mental healthcare use and the amount of treatment, support earlier research in which pain, and other physical symptoms, have been found to be predictive of mental health problems.14 16 41–43 However, the relationship between adolescent musculoskeletal pain and later mental health problems was attenuated after controlling for adolescent psychosocial and mental health problems. This could be due to confounding or mediating effects, indicating an intertwined relationship between adolescent psychosocial problems and musculoskeletal pain in predicting mental health problems.
The higher proportion of later mental healthcare users in the pain-related functional impairment group support that daily function, in relation to symptoms, is an important predictor of mental health outcome. However, the relationship between adolescent musculoskeletal pain and later mental health problems was evident regardless of functional impairment.
Physical problems, such as pain, are part of the clinical picture of mental health disorders, especially anxiety and mood disorders.20–22 39 Our findings support this and show the relevance of adolescent physical and psychosocial problems in predicting later mental health disorders. The physical aspects were further highlighted in the final regression models where adolescent musculoskeletal pain was significantly associated with anxiety disorders, and low physical activity with mood disorders. This is in line with the clinical picture of these disorders.39
Shanahan et al16 found pain in youth to be predictive of anxiety and mood disorders in young adulthood adjusted for psychosocial mediators. In our results, this was the case just for anxiety disorders, but the relationship between adolescent musculoskeletal pain and mental health disorders was stronger for anxiety and mood disorders in both genders, supporting the findings of Shanahan et al.16 The differences in our findings may be due to the different methodology and adolescent mediators. Interestingly, Shanahan et al16 found that pain persisting across developmental periods increased the risk of mental health problems in young adulthood. We could not examine this in our study, but we did find a significant positive relationship between the number of adolescent pain sites and mental healthcare outpatient treatment and the proportion of inpatients in young adulthood. This indicates that adolescents with multisite pain and psychosocial problems may have an increased risk of being worse off later on.
The dominant predictors for the undiagnosed group were different from those diagnosed with a mental health disorder. The impact of school-related stress and adverse life events may indicate that this group struggles with everyday stressors and life experiences, and are not in need of long-term treatment. However, a potential bias in the undiagnosed group is dropout from treatment. This group's low treatment hours could indicate that they were evaluated and not satisfying a diagnosis or it might indicate patient dropouts. It was impossible to differentiate this in the registry data.
Adolescent anxiety/depression problems, low family income and low physical activity were highly associated with later mental health disorders in the final model. Low family income might result in or be a result of social inequalities and thereby increase the risk of mental health problems.24 44 Sagatun et al33 found adolescent physical activity to be weakly associated with later mental health problems at 3-year follow-up, however only in men. School-related stress was significant and adverse life events a strong trend in the final model. Pressure to succeed and the risk of academic failure can be a stressor in all social classes and educational levels, as it is often associated with personal expectations and limited employment opportunities for young people.24 The adverse life events measure, although crude, included known risk factors of mental illness such as bullying and sexual abuse.24
Almost half of those who had consulted a psychiatrist/psychologist in adolescence were registered as later mental healthcare users, indicating that a considerable proportion of adolescents with mental health problems have a long-term need for specialised services.
A low recognition of adolescent mental health disorders in primary care has been shown.19 With short consultations, discovering underlying mental health problems might be challenging for clinicians in patients presenting with physical symptoms. Therefore, physical symptoms, such as pain, should not be ignored in the early detection of mental health problems. Most patients with mental health problems presenting physical symptoms acknowledge their emotional problems when asked about them.20 Early detection might reduce the duration of illness and the splitting of physical and psychosocial problems.
Methodological strengths and limitations
The main strength of this study is the linkage of a large unselected population-based study to a national patient registry, making it possible to study a wide range of predictors of mental healthcare use and disorders. The study had equal gender distribution and a high participation rate. We had a representative sample of mental healthcare users in our sample compared to the total population estimation.
The NPR is a national patient registry for specialist care of high quality, and we found few logical errors. Ideally, it would have been preferable to differentiate between primary and secondary diagnoses, but from a close inspection of the NPR data it was clear that attempting this would not be trustworthy due to the evident difference in the specialists’ diagnostic coding practice. However, most of the primary and secondary diagnoses were within their respective main chapters of the ICD-10.
This study has several weaknesses. The specification of a 12-month period for the pain questions may have increased the risk of recall bias compared to shorter time periods. The expression ‘several times’ is objectively vague and is open to interpretation, but it indicates some regularity and seriousness of pain. However, the importance of multisite pain is still emphasised.
Psychosomatic problems are complex, and with only one cross-sectional study linked to the patient registry there might be other factors influencing the associations found in this study. The population study relied on self-reports with the risk of information bias. Some scales did not have a defined time period and the HSCL-10 measured only anxiety/depressive symptoms during the previous week. Some of the scales from the population study are not frequently used by other studies, making it hard to exactly replicate the findings, though their internal consistency was high. The lack of linearity between the ordinal groups in the type of mental healthcare users could be caused by the fact that we only had a single study from adolescence.
At first glance the explained variance of the multivariable models might be considered to be low; however, explained variance is a relative value, dependent on the nature of the associations examined. In outcomes with multiple determinants the size of the explained variance is limited by nature.45 For most of the adolescent factors it was not possible to say whether they appeared before or after the adolescent musculoskeletal pain. This makes it difficult to decipher whether the adolescent psychosocial factors are confounders or mediators. If they were mediators then the multivariable models are at risk of over-adjustment bias.
Conclusions
Multisite adolescent pain and can be part of the clinical picture and serve as an early clinical marker of mental health problems in youth. Adolescents with multisite musculoskeletal pain and psychosocial problems are at increased risk of mental health disorders in young adulthood, especially mood and anxiety disorders. Since it is common for youth troubled by mental health problems to present physical symptoms in a primary care setting it is therefore important to examine for psychosocial problems in such cases, in order to offer early interventions.
Footnotes
Contributors: CE has contributed to the concept and design of the study, the acquisition of registry data, analysis and interpretation of data, drafting and revising the manuscript. BS has contributed in the analysis and interpretation of data, critical review and revision of the manuscript. SK has contributed in the concept and design of the study, acquisition of data, analysis and interpretation of data, critical review and revision of the manuscript.
Funding: UiT–The Arctic University of Norway, The Centre for Sami Health Research and the Norwegian Institute of Public Health for funding of the Norwegian Arctic Adolescent Health Study, The University Hospital of North Norway and Nordland Hospital for funding the registry linkage. Data from the Norwegian Patient Register (NPR) has been used in this publication. The interpretation and reporting of these data are the sole responsibility of the authors, and no endorsement by the NPR is intended nor should be inferred.
Competing interests: None declared.
Ethics approval: The students and their parents were given written information about the study, and the students provided written consent. The Norwegian Data Inspectorate and the school authorities approved the NAAHS. The Regional Medical Ethical Committee approved the NAAHS and the registry linkage. The Norwegian Institute of Public Health and Statistics Norway carried out the linkage.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.King S, Chambers CT, Huguet A et al. . The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 2011;152:2729–38. 10.1016/j.pain.2011.07.016 [DOI] [PubMed] [Google Scholar]
- 2.Hoftun GB, Romundstad PR, Zwart JA et al. . Chronic idiopathic pain in adolescence—high prevalence and disability: the young HUNT Study 2008. Pain 2011;152:2259–66. 10.1016/j.pain.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 3.Eckhoff C, Kvernmo S. Musculoskeletal pain in Arctic indigenous and non-indigenous adolescents, prevalence and associations with psychosocial factors: a population-based study. BMC Public Health 2014;14:617 10.1186/1471-2458-14-617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hakala P, Rimpelä A, Salminen JJ et al. . Back, neck, and shoulder pain in Finnish adolescents: national cross sectional surveys. BMJ 2002;325:743 10.1136/bmj.325.7367.743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ståhl MK, El-Metwally AA, Rimpelä AH. Time trends in single versus concomitant neck and back pain in Finnish adolescents: results from national cross-sectional surveys from 1991 to 2011. BMC Musculoskelet Disord 2014;15:296 10.1186/1471-2474-15-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain 2004;8:187–99. [DOI] [PubMed] [Google Scholar]
- 7.Jones GT, Silman AJ, Power C et al. . Are common symptoms in childhood associated with chronic widespread body pain in adulthood? Results from the 1958 British Birth Cohort Study. Arthritis Rheum 2007;56:1669–75. [DOI] [PubMed] [Google Scholar]
- 8.Kamaleri Y, Natvig B, Ihlebaek CM et al. . Number of pain sites is associated with demographic, lifestyle, and health-related factors in the general population. Eur J Pain 2008;12:742–8. 10.1016/j.ejpain.2007.11.005 [DOI] [PubMed] [Google Scholar]
- 9.Skrove M, Romundstad P, Indredavik MS. Chronic multisite pain in adolescent girls and boys with emotional and behavioral problems: the Young-HUNT study. Eur Child Adolesc Psychiatry 2015;24:503–15. 10.1007/s00787-014-0601-4 [DOI] [PubMed] [Google Scholar]
- 10.Hoftun GB, Romundstad PR, Rygg M. Factors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: the young–HUNT study 2008. J Pain 2012;13:874–83. 10.1016/j.jpain.2012.06.001 [DOI] [PubMed] [Google Scholar]
- 11.Mangerud WL, Bjerkeset O, Lydersen S et al. . Chronic pain and pain-related disability across psychiatric disorders in a clinical adolescent sample. BMC Psychiatry 2013;13:272 10.1186/1471-244X-13-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lien L, Green K, Thoresen M et al. . Pain symptoms as risk factor for mental distress: a three-year follow-up study. Eur Child Adolesc Psychiatry 2011;20:509–16. 10.1007/s00787-011-0211-3 [DOI] [PubMed] [Google Scholar]
- 13.Mikkelsson M, El-Metwally A, Kautiainen H et al. . Onset, prognosis and risk factors for widespread pain in schoolchildren: a prospective 4-year follow-up study. Pain 2008;138:681–7. 10.1016/j.pain.2008.06.005 [DOI] [PubMed] [Google Scholar]
- 14.Lewandowski Holley A, Law EF, Zhou C et al. . Reciprocal longitudinal associations between pain and depressive symptoms in adolescents. Eur J Pain 2013;17:1058–67. 10.1002/j.1532-2149.2012.00272.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knook LM, Lijmer JG, Konijnenberg AY et al. . The course of chronic pain with and without psychiatric disorders: a 6-year follow-up study from childhood to adolescence and young adulthood. J Clin Psychiatry 2012;73:e134–9. 10.4088/JCP.10m06751 [DOI] [PubMed] [Google Scholar]
- 16.Shanahan L, Zucker N, Copeland WE et al. . Childhood somatic symptoms predict generalized anxiety and depressive disorders during young adulthood in a community sample. Psychol Med 2015;45:1721–30. 10.1017/S0033291714002840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paananen MV, Taimela SP, Auvinen JP et al. . Risk factors for persistence of multiple musculoskeletal pains in adolescence: a 2-year follow-up study. Eur J Pain 2010;14:1026–32. 10.1016/j.ejpain.2010.03.011 [DOI] [PubMed] [Google Scholar]
- 18.Jones GT. Pain in children--a call for more longitudinal research. Pain 2011;152:2202–3. 10.1016/j.pain.2011.06.016 [DOI] [PubMed] [Google Scholar]
- 19.Kramer T, Garralda ME. Psychiatric disorders in adolescents in primary care. Br J Psychiatry 1998;173:508–13. 10.1192/bjp.173.6.508 [DOI] [PubMed] [Google Scholar]
- 20.Simon GE, VonKorff M, Piccinelli M et al. . An international study of the relation between somatic symptoms and depression. N Engl J Med 1999;341:1329–35. 10.1056/NEJM199910283411801 [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Jackson JL, Chamberlin J. Depressive and anxiety disorders in patients presenting with physical symptoms: clinical predictors and outcome. Am J Med 1997;103:339–47. 10.1016/S0002-9343(97)00241-6 [DOI] [PubMed] [Google Scholar]
- 22.Bair MJ, Robinson RL, Katon W et al. . Depression and pain comorbidity: a literature review. Arch Intern Med 2003;163:2433–45. 10.1001/archinte.163.20.2433 [DOI] [PubMed] [Google Scholar]
- 23.Garralda ME. The interface between physical and mental health problems and medical help seeking in children and adolescents: a research perspective. Child Adolesc Ment Health 2004;9:146–55. 10.1111/j.1475-3588.2004.00098.x [DOI] [PubMed] [Google Scholar]
- 24.Patel V, Flisher AJ, Hetrick S et al. . Mental health of young people: a global public-health challenge. Lancet 2007;369:1302–13. 10.1016/S0140-6736(07)60368-7 [DOI] [PubMed] [Google Scholar]
- 25.Colman I, Wadsworth ME, Croudace TJ et al. . Forty-year psychiatric outcomes following assessment for internalizing disorder in adolescence. Am J Psychiatry 2007;164:126–33. 10.1176/ajp.2007.164.1.126 [DOI] [PubMed] [Google Scholar]
- 26.Goodman A, Joyce R, Smith JP. The long shadow cast by childhood physical and mental problems on adult life. Proc Natl Acad Sci USA 2011;108:6032–7. 10.1073/pnas.1016970108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hunfeld JA, Perquin CW, Duivenvoorden HJ et al. . Chronic pain and its impact on quality of life in adolescents and their families. J Pediatr Psychol 2001;26:145–53. 10.1093/jpepsy/26.3.145 [DOI] [PubMed] [Google Scholar]
- 28.Lewandowski AS, Palermo TM, Stinson J et al. . Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain 2010;11:1027–38. 10.1016/j.jpain.2010.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sleed M, Eccleston C, Beecham J et al. . The economic impact of chronic pain in adolescence: methodological considerations and a preliminary costs-of-illness study. Pain 2005;119:183–90. 10.1016/j.pain.2005.09.028 [DOI] [PubMed] [Google Scholar]
- 30.Groenewald CB, Palermo TM. The price of pain: the economics of chronic adolescent pain. Pain Manag 2015;5:61–4. 10.2217/pmt.14.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Norwegian Directorate of Health. The Norwegian Patient Registry 2008. https://helsedirektoratet.no/norsk-pasientregister-npr (accessed Apr 2015).
- 32.The Norwegian Institute of Public Health. Youth Studies. http://www.fhi.no/artikler/?id=105586 (accessed Apr 2015).
- 33.Sagatun A, Søgaard AJ, Bjertness E et al. . The association between weekly hours of physical activity and mental health: a three-year follow-up study of 15-16-year-old students in the city of Oslo, Norway. BMC Public Health 2007;7:155 10.1186/1471-2458-7-155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Røysamb E, Schwarzer R, Jerusalem M. Norwegian Version of the General Perceived Self-Efficacy Scale 1998. http://userpage.fu-berlin.de/~health/norway.htm (accessed Apr 2015).
- 35.DI Alsaker FD, Olweus D. A growth curve approach to the study of parental relations and depression in adolescence. Seattle: Pap. Present. Biannu. Meet. Soc. Res. Child Dev, 1991. [Google Scholar]
- 36.Derogatis LR, Lipman RS, Rickels K et al. . The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci (Basel) 1974;19:1–15. [DOI] [PubMed] [Google Scholar]
- 37.Strand BH, Dalgard OS, Tambs K et al. . Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36). Nord J Psychiatry 2003;57:113–18. 10.1080/08039480310000932 [DOI] [PubMed] [Google Scholar]
- 38.Statistics Norway. Norwegian Standard Classification of Education Revised 2000 2003. http://www.ssb.no/a/english/publikasjoner/pdf/nos_c751_en/nos_c751_en.pdf (accessed Apr 2015).
- 39.World Health Organization. The International Classification of Diseases version 10 (ICD-10). Int Classif, 1994. http://www.who.int/classifications/icd/en/ (accessed Apr 2015). [Google Scholar]
- 40.The Norwegian Directorate of Health. Activity data from specialized mental health care in Norway, 2012 (Norwegian) 2013. http://www.finnmarkssykehuset.no/reorganisere-dogntilbudet-innen-psykisk-helse-og-tsb/aktivitetsdata-for-psykisk-helsevern-for-voksne-og-tverrfaglig-spesialisert-behandling-av-rusmiddel-bruk-2012-article103955-31283.html (accessed Apr 2015).
- 41.Hotopf M, Carr S, Mayou R et al. . Why do children have chronic abdominal pain, and what happens to them when they grow up? Population based cohort study. BMJ 1998;316:1196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kroenke K, Wu J, Bair MJ et al. . Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain 2011;12:964–73. 10.1016/j.jpain.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gerrits MMJG, van Oppen P, van Marwijk HWJ et al. . Pain and the onset of depressive and anxiety disorders. Pain 2014;155:53–9. 10.1016/j.pain.2013.09.005 [DOI] [PubMed] [Google Scholar]
- 44.Lorant V, Kampfl D, Seghers A et al. . Socio-economic differences in psychiatric inpatient care. Acta Psychiatr Scand 2003;107:170–7. 10.1034/j.1600-0447.2003.00071.x [DOI] [PubMed] [Google Scholar]
- 45.O'Grady KE. Measures of explained variance: cautions and limitations. Psychol Bull 1982;92:766–77. 10.1037/0033-2909.92.3.766 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-012035supp_table.pdf (54KB, pdf)