Abstract
Virtual Fracture Clinics (VFCs) are an alternative to the conventional fracture clinics, to manage certain musculoskeletal injuries. This has recently been reported as a safe, cost-effective and efficient care model. As demonstrated at vanguard sites in the United Kingdom, VFCs can enhance patient care by standardising treatment and reducing outpatient appointments.
This project demonstrates how a Quality Improvement approach was applied to introduce VFCs in the District General Hospital setting. We demonstrate how undertaking Process Mapping, Driver Diagrams, and Stakeholder Analysis can assist implementation. We discuss Whole Systems Measures applicable to VFCs, to consider how robust and specific data collection can progress this care model.
Three Plan-Do-Study-Act cycles led to a change in practice over a 21-month period. Our target for uptake of new patients seen in VFCs within 6 months of starting was set at 50%. It increased from 0% to 56.1% soon after introduction, and plateaued at an average of 56.4% in the six-months before the end of the study period.
Careful planning, frequent monitoring, and gathering feedback from a multidisciplinary team of varying seniority, were the important factors in transitioning to, and sustaining, a successful VFC model.
Problem
In this project, we explored how to introduce Virtual Fracture Clinics (VFCs) to a modest-sized orthopaedic department at West Middlesex University Hospital, London from November 2014. The unit is comprised of six consultants and two associate specialists, and six registrars, providing orthopaedic services – excluding major trauma level care – in West London. We wanted to introduce VFCs to reduce the number of unnecessary face-to-face (FTF) consultations for simple orthopaedic injuries referred to the department from Accident and Emergency (A&E), and two Urgent Care Centres – one within the same hospital and another at Teddington Memorial Hospital.
We aimed to transition to reviewing at least 50% of new outpatient referrals in VFCs by May 2015, and sustain this service at not less than 50% for the subsequent year, till May 2016. We envisaged concurrent positive effects on patient experience, the waiting time between referral and consultation, and fracture clinic capacity, but this was outside the remit of this study.
Background
In the United Kingdom, there are almost 2 million attendances to Accident & Emergency (A&E) departments each month – an increase of 30% since 2004.1 Approximately 30% of all A&E attendances are related to soft tissue and musculoskeletal injuries. Approximately one in five of these injuries are referred to the on-call Orthopaedic junior doctor for urgent review at the point of presentation – the remainder are managed by A&E doctors.2
In the UK National Health Service (NHS), Between 75-92% of all MSk injuries are followed up by an Orthopaedic surgeon, amounting to 7.1 million appointments per year (2003 data). Of these, 30% are new, and 70% are follow-up reviews.3 Of the new patients, approximately one in six will be discharged with advice,4 suggesting a scope for better education and discharge from A&E for certain conditions.
This cohort of patients therefore represents a significant burden to resources to the NHS. The majority of NHS hospitals have at least once-daily Fracture Clinics during the week, with some Trusts also scheduling appointments on weekends to meet excess demand and meet BOAST targets.5 Data from the Audit Commission showed that more than 25% of patients attending Fracture Clinic are delayed by more than 30 minutes from the scheduled time. In 2012-2013, the rate of patients not attending their appointment (‘Did Not Attend’ – DNA) was 7.3%, representing 6.9 million appointments, and a further 4 million were canceled by the patients.6 This may represent poor patient satisfaction, logistical difficulty in attending Fracture Clinics, and the scope of patients with certain fractures to recover without needing further Specialist input.
Across the NHS, resources are stretched due to a growing population, increased disease burden, and a drive to save £10bn over the next 5 years.7 The Carter Report identified that improving operational productivity and workflow could save £2bn per annum.8 It requires optimisation of resources, including staff, policies and practices.
The traditional fracture clinic model is therefore outdated and no longer suited to the demands of the modern NHS. This can lead to unwarranted variation in practice, a trend towards delay in time to Specialty review, patients attending clinic for unnecessary review, and increased time- and resource-pressure during clinics resulting in poor supervision of junior surgeons and a lower quality of treatment for more complex injuries. A redesigned fracture management pathway targets the Triple Aim of “improving the individual experience of care; improving the health of populations; and reducing the per capita costs of care for populations”.9
Glasgow Royal Infirmary (GRI), Scotland, has pioneered the development of the VFC care model and have published evidence that it does not impact clinical outcome of stable and self-limiting injuries when used in tandem with appropriate A&E decision making, is not an additional administrative or resource burden to A&E, and is not associated with increased unnecessary re-attendance to A&E.10 Indeed, there was a reduction in treatment times for some injuries, an overall increase in patients who were provided definitive management plans, and between 87-95% of patients reported being satisfied with their care.11 12 It was associated also associated with a lower overall use of staff resources.4 Work at Brighton and Sussex University Hospital (BSUH) – a major trauma centre – has similarly shown that some simple fractures can be reviewed and managed in a VFC, in a cost-effective and safe solution.13 However, to date there is limited data on the design or implementation of a VFC service in the district general hospital setting.
Baseline measurement
Baseline Measurement
We intended to collect data on the number of orthopaedic surgeon-patient interactions in fracture clinics before and after the introduction of Virtual Fracture Clinics, as this is an objective and accurate measure of how and when patients with musculokeletal injuries are reviewed. This is routinely measured by the hospital's electronic document and record system (eCamis, HE Information Systems Ltd, UK). In October 2014, we took a snapshot of these interactions over the five weekdays, in four consecutive weeks. We planned to recollect this data on monthly intervals over a 21 month period.
There were six fracture clinic sessions each week, and each was staffed by three orthopaedic surgeons and two healthcare assistants or nurses. There were 18-19 weekly fracture clinic sessions. In the baseline period, there were a total of 958 FTF interactions with patients, of which 412 (43.0%) were with patients at their first attendance. There were no VFC patient interactions.
Design
Intervention Design
Glasgow Royal Infirmary (GRI) have provided an outline on a VFC service in their Orthopaedic department at http://www.fractureclinicredesign.org/ The team have also published protocols to guide evidence-based clinical management of eight simple orthopaedic injuries which do not require further review in fracture clinic (Table 1).
Table 1.
Simple musculoskeletal injuries that are safe for discharge from the A&E department
| Injuries for Direct Discharge for Self Care with Written Advice from Accident and Emergency |
|---|
| Isolated Fifth Metatarsal Undisplaced Fractures |
| Isolated Fifth Metacarpal Undisplaced Neck Fractures |
| Peadiatric Greenstick Fractures |
| Peadiatric Undisplaced Stable Clavicle Fractures |
| Peadiatric Torus Wrist Fractures |
| Mallet Fingers |
| Isolated Undisplaced Radial Head Fractures |
| Elbow ‘fat pad positive’ Injuries |
Patients who have sustained one of these eight injuries are safely discharged with advice from A&E, or, where this is clinical equipoise, referred to a VFC. The former group potentially avoid unnecessary management (including cast immobilisation and follow-up) and the latter group potentially avoid an unnecessary hospital visit. In a VFC, decisions on management are made by an Orthopaedic surgeon reviewing the history and examination findings (which are documented by the initial clerking clinician in A&E or Urgent Care Centre), with corroboration with the radiographs taken at the time of the presentation.
We wanted to apply a Quality Improvement approach to redesigning our fracture clinic model, to demonstrate how careful planning, staff engagement, resource management, and identification of potential barriers to change, could enable a rapid and successful transition.
The team comprised of a senior orthopaedic consultant, the orthopaedic service manager and an orthopaedic registrar for design and implementation of this project. A junior orthopaedic clinician assisted with data collection from the Hospital's administrative department.
We used the following tools:
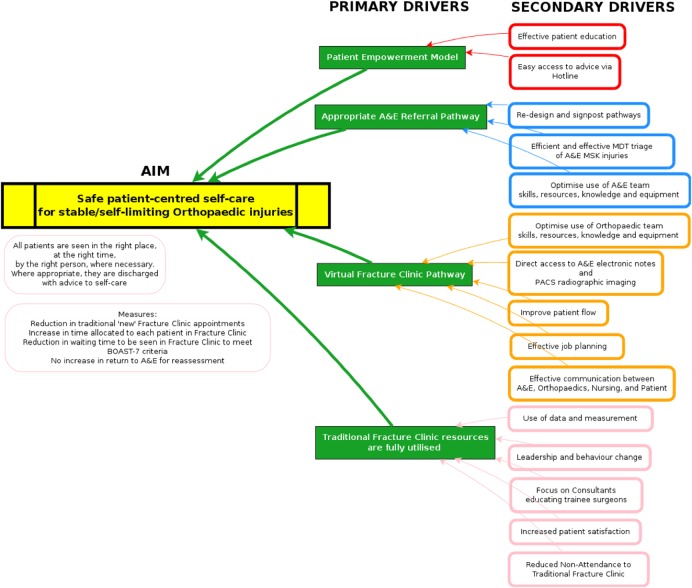
Driver Diagrams
To explore the potential for a VFC solution alongside safe discharge of some patients with musculoskeletal injuries from A&E, we constructed a Driver Diagram (Figure 1) with the aim to a) redesign A&E pathways to identify and manage stable/self-limiting fractures, b) empower patients to take responsibility for their care in a safe and effective way, c) create a new Virtual Fracture Clinic model for the review of patients who could not be discharged from A&E and who did not require immediate admission for surgery and d) better utilise time and resources within the conventional fracture clinic, which may improve quality of clinical care and teaching.
Figure 1.
A driver diagram for achieving a safe, patient centred virtual clinic model for orthopaedic injuries
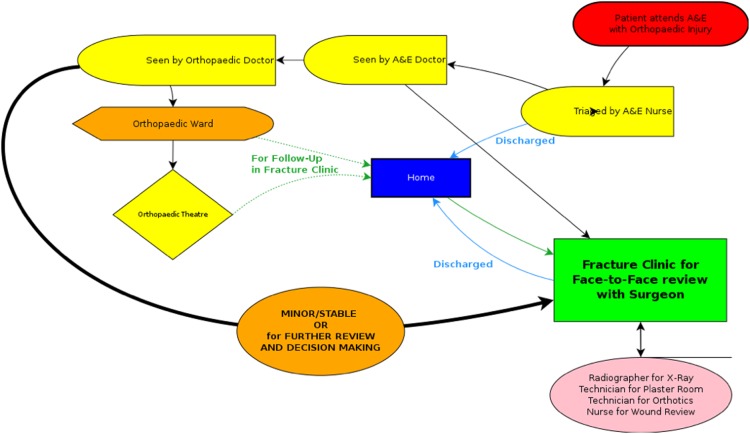
Process Mapping
By ‘alking the patient pathway’ and then applying LEAN methodology (more value with less work) we could identify where in the fracture clinic service there was spare capacity, and areas of strain or reduced productivity. The Process Map (Figure 2) demonstrates the conventional pathway in the NHS for musculoskeletal injuries seen in A&E. Patients either require admission or urgent planned surgery, or are referred to a face-to-face conventional fracture clinic. There is no differentiation between minor/stable injuries, and those that require active orthopaedic management.
Figure 2.
A patient flow-diagram in the traditional fracture clinic model
The GRI group have identified deficiencies with the conventional fracture clinic, for patients who have fractures that do not need surgery, including: a large number of patients, not all of whom are reviewed by a consultant, and many with no change in their treatment. They suggested that patient experience is poor, and that there may be an unnecessary number of changes to plaster.14 In our own department, we too observed that there was limited space in waiting areas, lengthy waiting times, and pressure on the Plaster team to remove casts that had been unnecessarily applied in A&E for one of the eight injuries. We discussed the available resources to implement a VFC with the hospital's service managers – though there a drive to demonstrate quality improvement within clinical departments, there was no spare staff capacity to accommodate an additional VFC session within existing sessions, nor capacity to create separate VFC sessions at new time-slots.
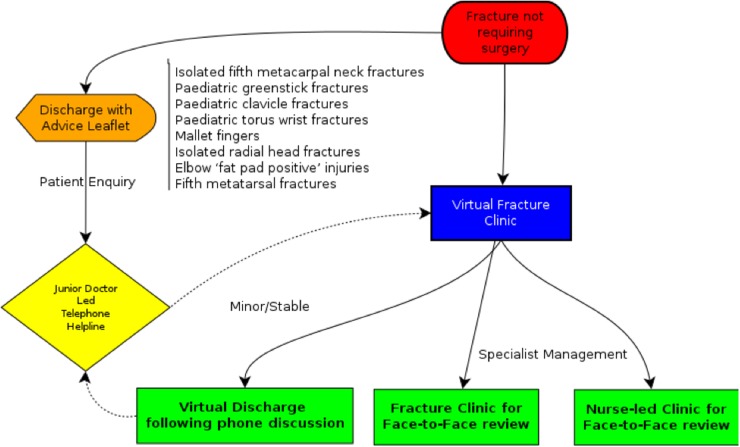
A process map for the implementation of the VFC in our unit is shown in Figure 3. After review by the orthopaedic surgeon in the VFC, the plan is communicated via phone-call with the patient by the Nurse or Healthcare Assistant. There are three possible subsequent outcomes: virtual discharge, through telephone call or voice-mail, and written summary letter copied to the patient and their General Practitioner; Nurse-led clinical review, most commonly for wound checks, plastering, splinting with orthotics devices, or wound dressings; or Referral to the conventional fracture clinic for FTF review and further management.
Figure 3.
A patient flow-diagram in the virtual fracture clinic model Reference: adapted from Glasgow Royal Infirmary Orthopaedic Department (2015). “Fracture Clinic Redesign.” Retrieved 23rd March, 2016, from http://www.fractureclinicredesign.org/.
Though the model of care developed at the GRI referred patients needing face-to-face review directly to an Orthopaedic Specialty Team (i.e. specialty clinics covering hand/wrist, foot and ankle, shoulder and elbow, or hip and knee), most Orthopaedic departments in the United Kingdom will have just one of each of these clinics each week, which are reserved for Elective referrals and post-operative reviews. To meet the local context, we have adapted the model for patients to be seen in a Fracture Clinic rather than Specialty Clinic review.
Stakeholder Analysis
A stakeholder analysis for orthopaedic fracture clinics identified the ‘9 Cs’ – Commissioners, Collaborators, Contributors, Channels, Commentators, Consumers, Champions, and Competitors. This includes staff from the hospital's CEO to junior doctors in A&E. This is assembled as a Four Sector Table (Table 2) to identify those stakeholders to satisfy, inform, manage or monitor – and communicate with before and during the implementation of this new care model.
Table 2.
Stakeholder analysis of healthcare professionals involved in management of orthopaedic injuries
| High power | Chief executive Finance director |
Consultant A&E staff Consultant Orthopaedic staff Clinical coding manager Medical director Surgical Operational Manager Nursing lead for Trauma |
| Low power | Medical records staff Medical secretaries |
Clinical audit and Data managers Junior doctors IT systems manager Plaster technicians Fracture Clinic nurses |
| Low impact/stacke holding | High impact/stake holding |
Strategy
Strategies for Implementation
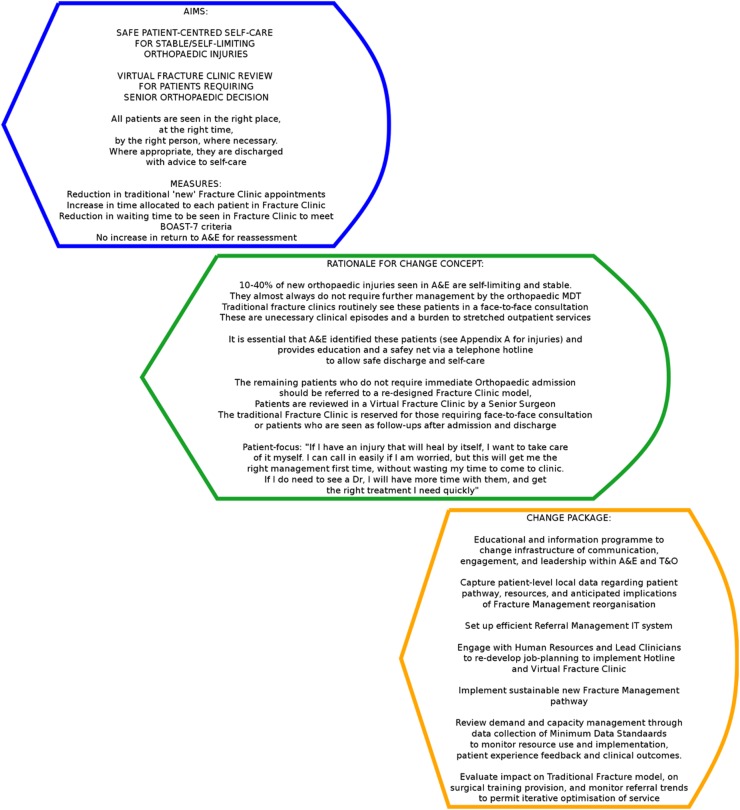
A. Create an ideal Change Package
A Change Package is shown in Figure 4, based on the drivers and rationale for introducing the VFC model. This is an effort to segment the plan for implementation into smaller packets to deploy to specific teams, which integrate as part of the re-designed pathway. Though for this project we measured only capacity and the transition to the model, we consider here a number of reach goals for the future, such as reducing waiting times, increased length of consultation slots, improved cost-effectiveness and improved patient-reported outcome measures.
Figure 4.
The change package, segmenting the plan for implementation of a novel virtual fracture clinic model
B. Identify Barriers to implementation
For example, these could be technological (access to radiographs), administrative (access to a patient's A&E/UCC documentation), or because of resistance to changing an accepted, physician-centric model of care, or the perception that the redesign will cost rather than save money and time.10 Hospitals within the NHS are paid through Clinical Commissioning Groups (CCGs). The tariff for seeing a new patient in a Fracture Clinic is higher than for seeing a ‘follow-up’. In the current system, it is possible that by discharging more patients from A&E, reviewing patients ‘virtually’ in VFC, and seeing a minority as ‘new patients’ in the conventional fracture clinic, a hospital would stand to lose money by providing a leaner and higher quality service, whilst a CCG would save money.
C. Consider Whole System Measures for quality
Though outside the scope of this project, we envision creating a minimum dataset on patients within the new model (VFC running alongside the conventional fracture clinic). The US Institute of Medicine (IOM) and the Institute for Healthcare Improvement (IHI) co-developed Whole System Measures (WSMs) for Quality in Healthcare.15 These coupled IOM's six dimensions of quality with IHI's focused measures to evaluate a health care system. We applied this methodology to our planned new care model, to advise a data collection for deploying future fracture clinic improvement initiatives (Table 3).
Table 3.
Institute of Medicine Dimensions and Institute for Healthcare Improvement Whole System Measures to set priorities for implementing the VFC
| IOM Dimension | Fracture Management Re-design | IHI Whole System Measure |
|---|---|---|
| Effective | Providing an evidence-based service to manage Orthopaedic fracture | Realiability of core measures Functional Health Outcomes Score Hospital re-admission percentage |
| Safe | By avoiding preventable harm including over-treating injuries or mismanaging complex ones, and ensuring appropriate surgical or conservative management provided by trained specialists | Rate of Adverse Events |
| Patient-centered | By providing a fracture management plan that is individually tailored to a patient's own needs and values and socioeconomic factors, and enabling the patient to take responsibility for their own care | Patient Experience Score Patient Satisfaction with Care Score |
| Timely | By providing a fracture management service in a timely manner. Orthopaedic injuries can be very painful, and there is a defined window of opportunity for surgical intervention | Days to next available appointment/specialist review |
| Equitable | Irrespective of the geographic location or the tertiary trauma capability of the hospital which the patient attends, and independent of local pressures on resources, the quality of care should not vary. Patients should be able to be transferred to super-specialist centers (e.g. poly-trauma or hand) where necessary, and the management plan should not deviate due to availability of resources or economic factors. | Equity Stratification |
| Efficient | By provideing a fracture serivce which is an efficient use of A&E and Orthopaedic department resources to provide value to the populatin which it serves | Health care cost / capita |
After implementation, these can be monitored routinely on run-charts to visualise the impact of the new pathway on management, and to identify opportunity for adaptation and evaluation. These measures (Table 4) should be reviewed by the project lead regularly, e.g. quarterly, and the results disseminated to stakeholders and relevant staff to provide a feedback loop and impetus for change.
Table 4.
An ideal minimum data-set to collect data on quality of patient outcome, individual experience of care, cost of implementing VFC model
| What | Quality Aim | Measurement | By Whom |
|---|---|---|---|
| Waiting time to Orthopeadic decision | Timely and equitable | Time to review in VFC/Traditional Fracture Clinic vs. BOAST-7 criteria | Fracture Clinic Operational Manager and Team |
| Key Performance Indicators | Effective | Time allocated to each patient in Traditional Fracture Clinic Number of patients discharged from A&E for self-care |
A&E and Fracture Clinic Operational Team |
| Demand, Capacity, Activity | Efficient | Number of patients referred to Traditional or VFC | A&E and Fracture Clinic Operational Team |
| Patient satisfaction | Patient-centered | EQ5D start and end score variations | |
| Risk register | Safe | Number of patients returning to A&E for assessment after discharge | Local Safety and Governance team |
During this project's study period, patient activity data in orthopaedic fracture clinics was collected on a monthly basis. We focused on four time-points over a 21-month period, with three PDSA cycles. As we did not have additional time or staff capacity to introduce new VFC sessions, we opted to remove one consultant orthopaedic surgeon from the conventional clinic. He or she worked with a Healthcare Assistant or Nurse, reviewing referrals from A&E/UCC using departmental clerking documentation and a dedicated computer with Picture Archiving Communication System (PACS) to see radiographs.
D. Plan-do-study-act Cycles
Adopting these strategies, we performed three PDSA cycles.
The aim of the first PDSA cycle was to conduct a pilot test of the VFC model on 3 clinics over 2 weeks, to identify major pathway problems and gather informal feedback from surgeons. The change hypothesis was that the new pathway would facilitate discharge of patients with benign orthopaedic injuries without the need for face-to-face review. Details of the new model and the diagnostic qualification criteria had been disseminated amongst the clinicians. We then gathered individual feedback from consultant and registrar orthopaedic surgeons and nurses, as well as the number of patient ‘interactions’ in the new VFC. 36 patients with minor musculoskeletal injuries who had been referred to the conventional fracture clinic were siphoned into the 3 VFC sessions, reflecting 2.5% of all new patients referred to fracture clinic. We offered patients the option of a face-to-face (FTF) appointment instead of the VFC. 10 of the 36 patients opted out. There was a mixed response from the surgeons – including a scepticism on making clinical decisions without seeing and examining a patient. The Clinical Lead reinforced that the VFC model was validated, and may ease pressure on a stretched service, and carefully reassured reluctant clinicians to persevere. The feedback and results led us to separate the VFC to a quieter room separate from the fracture clinic outpatient area, and we sought to obtain more of the clerking documentation from A&E. The data also demonstrated feasibility of the VFC model, for our next PDSA cycle – a full roll-out.
PDSA cycle 2 aimed to assess the impact of the VFC model on all fracture clinics, with data on the number of virtual and in-hospital interactions collected on a monthly basis.This cycle therefore reflected the new 2-tiered clinic model going ‘live’. The change hypothesis was that the model would provide a reliable, safe and acceptable ‘virtual’ review system for the agreed simple musculoskeletal injuries. To implement it, A&E clinical leads were informed of the change in referral pathway, and patients did not have an opt-out option. Of the new patient referrals, 56.6% were seen in VFC. There was a nominal target of 50%, though we expected variation of the prevalence of the six simple fractures depending on local case-mix. For example, the GRI unit saw 67% of new patients in VFC.10
Not all patients who required FTF follow-up after VFC needed to be seen in the next available clinic session. On occasion, a conventional fracture clinic was full or overbooked due to referrals from the preceding week's VFC. We therefore introduced a diary of available FTF slots for the 3 weeks after a VFC. The surgeon could then decide how quickly the patient required a FTF consultation or Plaster Room appointment alone. He or she could thus actively manage the conventional clinic.
VFC surgeons noted that some patients had been seen by the orthopaedic on-call SHO in A&E, the case had been discussed on the day with a more senior surgeon (Registrar or Consultant), and a plan provided and documented in the A&E/UCC clerking. These patients do not need VFC review first, and some may not need a FTF consultation either – this was reviewed in the next PDSA cycle.
Cycle 2 also revealed discrepancy in the availability of scanned clerking documentation from A&E (the Urgent Care Centres used electronic health records). We communicated our difficulties with the A&E administration team, to instigate scrupulous scanning of notes to facilitate the VFC.
Finally, the Plaster team were seeing patients referred to them from the VFC, with no FTF consultation with a doctor planned. The team raised concerns about responsibility of care for these patients, particularly when the need for clinical decision may arise. Examples include a patient in significant pain, or skin blisters underneath plaster casts. This too was addressed in the next PDSA cycle. Overall, there was improved satisfaction and buy-in from the surgeons for VFCs, and most clinicians embraced the new care model.
PDSA cycle 3 was the last. The change hypothesis was that iterative design changes and the bedding-in of the VFC model to the department's culture would safely maintain throughput to greater than 50%. We implemented diary management, and reinforced the patient pathway to orthopaedic and A&E staff, to reduce inappropriate referrals. For patients requiring further radiographs and FTF follow-up, we mandated that the VFC surgeon request investigations at the time of first review, to improve patient flow. When clinical decisions were required for patients seen by the Plaster team, the patient was to be reviewed by one of the two surgeons seated in the conventional fracture clinic. At the final data collection point, 60.1% of all new referrals were seen in VFC, with an average of 56.4% in the last 6 months of the study.
Results
Our main outcome measure for this project was the percentage of total new referrals seen in the Virtual Fracture Clinic. Our run-chart demonstrates that after the test-period, we saw between 54.6% and 63.7% of new referrals in the VFC. There was seasonal variation in the number of patients seen within the fracture clinic service, but a modest increase in capacity – an average of 1124 patients were seen monthly during the 19 months in which the VFC was fully implemented, compared to 1043 patients in the 15 months prior (See supplementary – Run Chart for Results section).
bmjqir.u220211.w7861supp.pdf (53.7KB, pdf)
Lessons and limitations
This project aim was to introduce a novel pathway to a care-model which has changed little since the advent of modern orthopaedics. While several vanguard centres, including Glasgow Royal Infirmary and Brighton and Sussex NHS Trust, have demonstrated successful implementation, we wished to apply careful quality improvement methodology to plan the transition in the DGH setting, and guide future development of the service.
A key lesson learnt was to engage all stakeholders early, including service managers, nursing staff, A&E clinicians, plaster technicians, and both senior and junior orthopaedic surgeons. Feedback from them advised our PDSA cycles. The test period, prior to the new pathway going ‘live’, was critical to success. As proof-of-principle, it garnered local buy-in from stakeholders, and safely trialled the new model on a small subset of patients in a defined time-frame. It identified problems and local hurdles to successful change that were missed by theoretical planning.
Finally, the run charts demonstrate that we have achieved a sustainable fracture clinic service, which is now the accepted model at this hospital. In our opinion, this reflects well on our QI approach. A longer time-series with a trend analysis would also confirm that the improvements were not due to random fluctuations. Introducing the VFC model may have also increased the fracture clinic capacity, though the increase in total patient episodes may simply reflect the increased burden on the NHS in general. Other confounders that we have not been able to factor for are selection bias and reporting bias for referring patients from Emergency staff adapting to the VFC and the list of simple of musculoskeletal injuries.
This project is limited by the data we chose to collect – we measured only the uptake of the VFC service. Compared to the VFC model, the traditional fracture clinic design does not protect the Orthopaedic department against unnecessary attendances, and thus places more pressure on a time- and resource-poor service. Data on time to specialty review, patient satisfaction, or the quality of teaching/training available to junior surgeons before and after the VFC intervention, would add important another clinically relevant dimension to this report. In creating the Change Package, exploring Whole System Measures and considering a minimum data-set, the Unit next intends to collect data for quality, not simply quantity. Finally, the Change Package was designed for the district general hospitals setting and may not be applicable or effective when applied to a major trauma centre. The incidence of simple musculoskeletal injuries may be lower, the clinical burden and proportion of patients in longer term follow-up is likely larger, and all patients may not be suitable to attend an unselected fracture clinic as in this report's home institution.
Conclusion
We have successfully adopted a VFC care model, alongside conventional fracture clinics, without requiring additional surgeons or new clinic sessions. The project demonstrates how a quality improvement approach can plan for the implementation of VFCs in the district general hospital setting, and guide future research and development of the service. The use of regular staff feedback from across the patient-pathway led to incremental improvements in service design, as applied through three PDSA cycles. Over 54% of all patients with musculoskeletal injuries requiring senior review were routinely seen in the virtual clinic, and coincided with a 8% increase in outpatient fracture clinic capacity. Further work is underway to further implement the change package, enhance awareness, and assess the quality, patient-satisfaction and cost-effectiveness related to the new service through the creation of a Minimum Dataset for VFCs (Table 4). We have shared our processes first to other hospitals within this institution's NHS Trust and then locally in West London, and are working with the regional major trauma centre to adapt our Change Package for implementation there. We hope that in this way, departments can quickly and sustainably integrate VFCs alongside the conventional fracture clinic model.
Acknowledgments
Dr. Annie McKirdy – Clinical Fellow
Mrs Catherine Hill – Orthopaedics Service Manager
Footnotes
Declaration of interests: Nothing to declare
Ethical approval: Ethical approval was not sought for this project, as this was an improvement study, and no novel datasets were collected beyond routine.
References
- 1.NHS England. A&E Attendances and Emergency Admissions 2015-16 (Monthly and Quarterly) NHS England 2016 [cited 2016 24th October]. Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/statistical-work-areasae-waiting-times-and-activityae-attendances-and-emergency-admissions-2015-16-monthly-3/. [Google Scholar]
- 2.Health & Social Care Information Centre. Accident and Emergency Attendances in England (Experimental Statistics) 2007-2008. HSCIC: NHS England; 2009. [Google Scholar]
- 3.Department of Health Audit Commission. Outpatients – Review of National Findings Department of Health 2003 [cited 2016 October 24th]. Available from: http://archive.audit-commission.gov.uk/auditcommission/nationalstudies/health/other/pages/outpatients.aspx. [Google Scholar]
- 4.Jenkins PJ, Morton A, Anderson G, Van Der Meer RB, Rymaszewski LA. Fracture clinic redesign reduces the cost of outpatient orthopaedic trauma care. Bone Joint Res. 2016;5:33–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.British Orthopaedic Association. BOAST 7: Fracture Clinic Services 2013 [cited 2016 October 24th]. Available from: https://www.boa.ac.uk/wp-content/uploads/2014/12/BOAST-7.pdf. [Google Scholar]
- 6.Harrop V. Virtual healthcare delivery: defined, modeled, and predictive barriers to implementation identified. Proc AMIA Symp 2001. p. 244–48. [PMC free article] [PubMed] [Google Scholar]
- 7.NHS England. Five Year Forward View: NHS England; 2014. [cited 2016 24th October]. Available from: https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf. [Google Scholar]
- 8.Carter RP. Operational productivity and performance in English NHS acute hospitals: Unwarranted variations. Department of Health, 2016. [Google Scholar]
- 9.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27:759–69. [DOI] [PubMed] [Google Scholar]
- 10.Vardy J, Jenkins PJ, Clark K, Chekroud M, Begbie K, Anthony I et al. Effect of a redesigned fracture management pathway and ‘virtual’ fracture clinic on ED performance. BMJ Open. 2014;4:e005282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gamble D, Jenkins PJ, Edge MJ, Gilmour A, Anthony IC, Nugent M et al. Satisfaction and functional outcome with “self-care” for the management of fifth metacarpal fractures. Hand (N Y). 2015;10:607–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jayaram PR, Bhattacharyya R, Jenkins PJ, Anthony I, Rymaszewski LA. A new “virtual” patient pathway for the management of radial head and neck fractures. J Shoulder Elbow Surg. 2014;23:297–301. [DOI] [PubMed] [Google Scholar]
- 13.NHS England. Brighton and Sussex NHS Trust Virtual Fracture Clinic 2016 [cited 2016 24th October]. Available from: https://www.england.nhs.uk/challengeprizes/about/winners-1516/virtual-fracture-clinic/. [Google Scholar]
- 14.Glasgow Royal Infirmary Orthopaedic Department. Fracture Clinic Redesign 2015 [cited 2016 23rd March]. Available from: http://www.fractureclinicredesign.org/. [Google Scholar]
- 15.Martin LA, Nelson EC, Lloyd RC, TW N. Whole System Measures Cambridge, Massachusetts and www.IHI.org: Institute for Healthcare Improvement; 2007. [cited 2016 October 24th]. Available from: http://www.ihi.org/resources/pages/ihiwhitepapers/wholesystemmeasureswhitepaper.aspx. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqir.u220211.w7861supp.pdf (53.7KB, pdf)