Abstract
Background: Postoperative pain is one of the major problems in patients with femoral or hip fracture. Current study investigates the effect of 0.2% and 0.3% bupivacaine in ultrasound-guided fascia iliaca compartment block (FICB) on postoperative pain.
Methods: This randomized clinical trial study was conducted in Rasoul Akram Hospital of Iran University of Medical Sciences. Forty-eight patients with femoral or hip fractures who were candidates for surgery underwent FICB, divided into two groups receiving bupivacaine in 0.2% and 0.3% concentrations. Pain was evaluated with Visual Analog Scale (VAS) at times 2, 6, 12, 24, and 48 hours after surgery. Need for opioids, nausea and vomiting after surgery, patients’ satisfaction with pain control and motor block were also recorded. T-test or Mann- Whitney U test and Repeated measure ANOVA was used for analysis.
Results: Pain score after surgery was significantly lower in groups receiving 0.3% than the group receiving 0.2% concentration. Patients’ satisfaction with pain control in 0.2% group was significantly higher (p=0.04). Time to analgesic onset in both groups had no significant differences (p=0.5). The incidence of nausea and vomiting (p=0.5) and opioid consumption (p=0.1) between the two groups showed no significant difference.
Conclusion: In femoral or hip fracture, bupivacaine with 0.3% concentration in fascia iliaca compartment block can cause lower pain score compared to bupivacaine with 0.2% concentration, but patients’ satisfaction with pain control and severity of motor block is higher in bupivacaine 0.2%.
Keywords: Postoperative pain, Bupivacaine, Fascia iliac block
Introduction
In fractures of the femur and pelvic bones, reduced postoperative pain and patient comfort are concerned (1,2). The consequences of post-operative pain include physiological stress which may lead to an increase in the hemostatic system, deep vein thrombosis resulting from venous stasis and impaired immune system which result in increased infections, fatigue and delay in return of muscle function (3).
Various postoperative pain control methods include intravenous and oral anti-inflammatory drugs, opioids, epidural and peripheral nerve block. Each of mentioned methods has some advantages and disadvantages. The use of opioids is accompanied by side effects such as nausea, vomiting, constipation, itching, dizziness and respiratory depression. Epidural anesthesia is along with the risks such as epidural hematoma (4).
Attempts for creating effective and secure anesthesia have led to design of various methods for local anesthesia (5). Peripheral nerve block is highly considered due to its effective role in reducing postoperative pain, faster release, and movement of patients’ movement (6-9).
The previous limitation in the application of blocks was their limited efficacy which has been eliminated today with the presence of catheters and pumps, though it brings about such risks as catheter infection and toxicity of anesthetic drugs and prolonged block (10-12).
One of the peripheral nerve block methods, which is currently considered in orthopedic surgery is Fascia Iliaca Compartment Block (FICB). Some studies have investigated its efficacy and security on pain reduction in patients (13-17).
Meanwhile, bupivacaine is an amino acid anesthetic local drug which its efficacy has been emphasized in various studies considering its low price and availability (18). Since the volume and concentration of the local anesthetic drug, factors affecting the absorption and tissue distribution of the drug and injection site influence its efficacy (19), efficacy of bupivacaine in different concentrations has been studied as an adjuvant in multimodal analgesia approach in controlling postoperative pain (3,20).
Some studies had shown that the use of 0.5% bupivacaine or 0.25% for peripheral nerve blocks provides longer duration of postoperative analgesia for lower extremity surgery than the other long-acting local anesthetics for example ropivacaine or mepivacaine. Also, bupivacaine may exhibit a longer delay of onset of surgical anesthesia. Despite this, there is concern about the use of higher concentrations of bupivacaine because of the potential for systemic toxicity with larger doses, and there is the potential for prolonged nerve block (20,21).
According to our knowledge, no randomized double-blind trial study has been investigated the effect of bupivacaine in different concentrations in FICB method. Thus, we investigated the effect of bupivacaine in FICB in patients with femoral and hip fractures. Two difference concentrations of bupivacaine were used for achieving maximum pain control so that optimal level of drug is determined which is free from consequences and prolonged motor block in FICB.
Methods
This study was a Double-Blind Randomized Clinical Trial. Research population included 18–70 years old people with a femoral or hip fracture which underwent elective surgery. For calculation of sample size, according to the results of the pilot study (10 cases), difference and SD of pain with Visual Analog Scale (VAS) in the prescription of bupivacaine in doses 0.2% and 0.3% was 1.5. Thus, considering alpha error as 0.05 and power as 90% for this study, and given 10 percent probability of drop out, the sample size was calculated as 24 for each group.
Samples were selected using convenient sampling among patients referred to Rasoul Akram Hospital in Tehran. Infromed written consent was taken from the patients. The study was done from March 2014 to April 2015.
Inclusion criteria were: 1) Patients with femoral or hip fracture at age range 18 to 70 years old 2) Patients with American Society of Anesthesiologist (ASA) 1 and 2 3) Patients with verbal and written communication abilities who could consciously provide the consent for participation in the study
Exclusion criteria were: 1) Multiple fractures in different parts simultaneously (multiple trauma) 2) Sensitivity to amid anesthetic drugs 3) Addiction to alcohol, drugs or cigarettes 4) Body Mass Index (BMI) < 18 and morbid obesity (BMI> 40) 5) Pregnancy 6) Peripheral neuropathy and mental disorders that are potentially effective on pain perception
Patients were randomly assigned to two groups (n=24) based on computer randomized list. One group received 0.2% bupivacaine (Milan, Italy, Markaeen) and the other group received 0.3% bupivacaine. For making study as double-blind, the patient and anesthesiologist who injected drugs were not aware of the prescribed medication.
Patients underwent standard monitoring including ECG, pulse oximetry and noninvasive blood pressure in operation room. All patients experienced general anesthesia in a similar way. It included reception of midazolam 0.02mg/kg and fentanyl 2mcg/ kg as premedication. For induction of anesthesia, thiopental 5mg/kg and atracurium 0.5mg/kg were used. For maintenance of anesthesia, propofol 100mcg/kg/min was used. After the end of the operation and transfer of the patient to the recovery room and necessary monitoring for patients (EKG- NIBP- POM), ultrasound-guided fascia iliaca compartment block was applied on patients using a linear probe. For performing the block, the patient was placed in Supine position. Ultrasound probe was placed in the inguinal region, and following observation of femoral arteries, the probe was moved a little toward the lateral so that iliopsoas muscle is specified as a hypo echo part in lateral to the artery and femoral nerve. After dermal anesthesia with 2 cc lidocaine 1% at the place of needle entry using spinal needle No. 23 as in line, 30 cc of local anesthetic was injected between Fascia Iliaca layer and Iliopsoas muscle after passing Fascia Iliaca layer. Distribution of local anesthetic as inward and outward of injection location and beneath Fascia location is proper. In recovery, pain severity was evaluated using VAS scale every 5 minutes (22) and pain severity below 3 was considered as the initiation of onset of analgesia. In addition, pain severity was measured at rest state at hours 2, 6, 12, 24, and 48 hours after operation based on VAS tool. In the case of non-pain control, pethidine 20 mg was injected intravenously in conditions of pain scores above 4. Also, sedation score was recorded using Ramsay Sedation Scale during 48 h follow-up (23). The frequency of nausea and vomiting was evaluated and recorded. In the case of nausea and vomiting in recovery, metoclopramide 10 mg was used. Satisfaction with the pain control and motor block severity (knee flexion and ability to lift leg), after 48 hours was recorded. Patient satisfaction level from pain control after 48 hours were measured as excellent, good, moderate and poor.
Data collection was done using a questionnaire. Information was collected through an author-made questionnaire and was carried out by one of the main authors.
Collected data were entered into SPSS software. Frequency distribution was used for qualitative variables and mean and Standard Deviation (SD) was used for quantitative variables. Analysis of qualitative data was done using chi-square test. Quantitative data analysis was done using t-test or Mann-Whitney U test. Repeated measure ANOVA was used for comparing pain severity at recorded times in two groups. In statistical analysis, P-value less than 0.05 was considered as significant. In this study, ethical principles of the Helsinki were pursued. The study was approved by Ethical Committee of Iran University of Medical Sciences, and it is registered at IRCT Center coded as IRCT5N20140 81014199.
Results
Fifty-six patients were investigated; one of whom was excluded due to an addiction history. Two patients were excluded due to BMI above 40 and 3 patients were excluded due to age above 70 years, and 2 patients did not consent to participate in the study. Finally, information for 48 patients in two groups (n=24) was analyzed (Fig. 1).
Fig. 1. Flow diagram of patients in the trial.
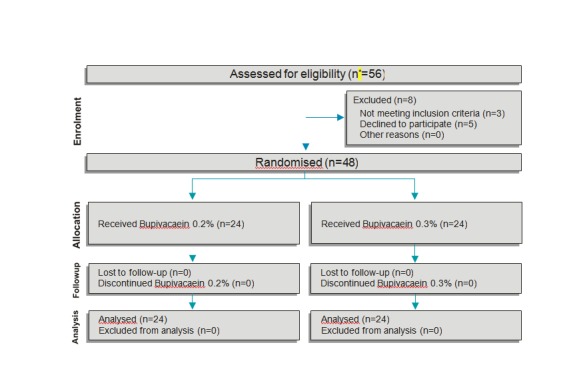
*n= number of patient
18 patients (37.5%) were female and 30 patients (62.5%) were male. Mean±SD age of the patients was 43.4±17.4 years. Demographic information of patients, blood pressure and heart rate before the blocks and type of fractures are given in Table 1 in terms of two groups. Statistically, significant difference was not observed between the two groups and it may suggest the right patient randomization in two groups (p<0.05).
Table 1. Demographic data type of fracture in two groups of patients .
| Variable |
Bupivacaine 0.2% (n = 24) |
Bupivacaine 0.3% (n = 24) |
p |
| Age (year) | 40.7±17.1* | 45.1±15.7 | 0.4 |
| Gender (female/male) | 8.16 | 10.14 | 0.5 |
| Body Mass Index (Kg/m2) | 23.5±2.3 | 23.5±2.8 | 0.99 |
| Type of fracture (Femur / Hip) | 22.2 | 22.2 | 0.99 |
*Data presented as mean ± SD
Overall pain score after the operation was lower in the group receiving 0.3 doses, and this difference was statistically significant (p<0.001) (Fig. 2).
Fig. 2.
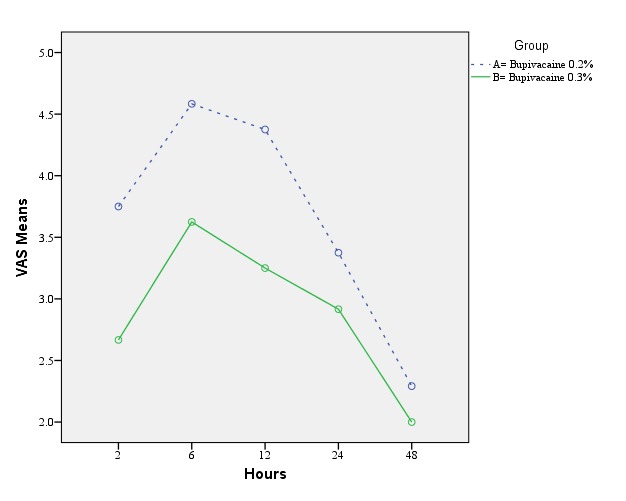
Comparison of pain score changes in different times in two groups (VAS = Visual Analog Scale (0-10))
Pain score of patients after 2, 6, 12, 24, and 48 hours of the operation are given in Table 2 for two groups. After 24 hours, no significant different pain score was observed in two groups.
Table 2. Pain score in term of times 2, 6, 12, 24 and 48 hours after operation .
| Time | Mean VAS (0-10) | p | |
| Bupivacaine 0.2% (n = 24) | Bupivacaine 0.3% (n = 24) | ||
| 2 | 3.7±0.9* | 2.7±0.9 | < 0.001 |
| 6 | 4.6±1.4 | 3.6±1.1 | 0.01 |
| 12 | 4.4±1.3 | 1.3±0.9 | 0.002 |
| 24 | 3.4±2.9 | 1.5±0.8 | 0.02 |
| 48 | 2.3±1 | 2±0.4 | 0.04 |
*Data presented as mean ± SD
As observed in Table 3, time to analgesic onset was not significantly different between the two groups (p=0.5). The occurrence of nausea and vomiting was higher in the group receiving 0.3 doses, but there was no statistically significant difference (p=0.5). The number of patients requiring opioid consumption (analgesic) (p=0.1) and opioid dose (p=0.6) was lower in the group receiving 0.3 doses, but with no statistically significant difference. The number of patients with high satisfaction (excellent score) of postoperative pain control and motor block severity (knee flexion and ability to lift leg) was significantly higher in the group receiving 0.2 doses (p=0.04) (Table 3).
Table 3. Incidence of nausea-vomiting, opioid consumption, patient’s satisfaction and time to analgesic onset .
| Variable |
Bupivacaine 0.2% (n=24) |
Bupivacaine 0.3% (n=24) |
p |
| Number of patient with nausea-vomiting | 8 (31.3%)* | 10 (41.7%)* | 0.5 |
| Number of patients requiring opioid consumption | 19 (79.2%)* | 14 (58.3%)* | 0.1 |
| Consumption opioid dose (mg) | 24.3±11.6** | 22.1±6.3** | 0.6 |
| Number of patients with high satisfaction | 15 (62.5%)* | 8 (33.3%)* | 0.04* |
| Time to analgesic onset (minute) | 20.2±6.3** | 18.9±5.4** | 0.5 |
*N(%), ** Mean±SD
Discussion
Local anesthesia techniques are preferred for pain control in orthopedic operations (4). FICB is mainly used for analgesia in hip and femoral surgery (13). Bupivacaine is a long-acting local anesthetic which is used as an adjuvant in local anesthesia techniques (24). Peripheral nerve block techniques can reduce postoperative pain and drug use, though they may cause long-term numbness and weakness and thus delays in the ability to movement in the affected patient and the patient's dissatisfaction (4). Hence, it is necessary that mentioned anesthesia techniques are investigated in terms of advantages and disadvantages by performing more accurate studies. Several studies have demonstrated the effectiveness of FICB method in pain control in patients with orthopedic operations (13–16). However, the efficacy of bupivacaine with different concentrations, as an adjunct in local anesthesia techniques has been studied in other peripheral nerve blocks.
In the current study, effect of 0.2% and 0.3% bupivacaine in FICB on postoperative pain in femoral or hip fractures was studied. Current study indicates though pain score of patients with 0.3% bupivacaine was lower than 0.2% (p<0.001), satisfaction patients with pain control and motor block severity was significantly lower in the group receiving 0.3% bupivacaine (p=0.04). Although block anesthesia time was not directly measured in the current work, it seems lower satisfaction of patients was due to lengthened motor block in higher doses of bupivacaine and occurrence of numbness, weakness and delay in the walking (4).
Although some previous studies have compared bupivacaine with the other long-acting local anesthetics, few studies compared two difference concentrations of bupivacaine as an adjuvant in multimodal analgesia approach in controlling postoperative pain (20).
Mulroy studied the effect of femoral nerve block along with 0.25 and 0.5% bupivacaine on the duration of anesthesia time in patients undergoing an arthroscopic operation to repair the anterior cruciate ligament of the knee. Findings showed bupivacaine in 0.25% and 0.5% concentrations is accompanied by acceptable anesthesia, and duration of anesthesia showed no difference with two different concentrations of bupivacaine (20).
Xie investigated the effect of peripheral nerve blocks (femoral, obturator and lateral femoral transcutaneous) with two different concentrations of bupivacaine in pain after total knee arthroplasty. Research findings suggested that patients receiving 0.25% bupivacaine had lower pain and higher satisfaction compared to the group receiving 0.5% bupivacaine (4).
In the study by Krych, use of multi-modal analgesia with fascia iliaca block fascia in acute pain control in patients undergoing hip arthroscopy was investigated. This study indicated that multi-modal analgesia with FICB in patients undergoing hip arthroscopy is secure and effective. The quality of initial analgesia after the operation is great by FICB leading to the lower use of opioid, high pain control quality and high patient satisfaction (14).
In another by Fujihara, FICB effect on pain control in patients with femoral fracture was compared with NSAID prescription after the operation. Finally, the study concluded that FICB is secure and effecting in developing analgesia and it is suggested for old patients with femoral fracture (15).
Pain score in the current study showed a reduction in both groups after 24 hours, but there was no significant difference between two groups. In a study by Xie, femoral nerve block with bupivacaine showed a significant effect on early pain reduction after the operation, but it showed lower effect on pain after one day (4). In the study by de Lima E Souza, femoral nerve block using 0.25% ropivacaine or 0.5% bupivacaine was effective for postoperative analgesia after total knee replacement or anterior cruciate ligament reconstruction, particularly for the first 10 hours after spinal anesthesia (25).
Findings in the current study are similar to findings by Xie (4) indicating no significant difference in opioid consumption in both high and low dose of bupivacaine.
There was no significant difference in terms of occurrence of nausea and vomiting in both groups in this work which is consistent with findings by Xie (4).
Limitations of this study include lack of investigation of pain in patients in different motor states, lower numbers of patients with hip fracture and lack of measurement of analgesia duration of the block.
It is recommended that effect of peripheral nerve block procedures such as FICB with auxiliary local anesthetic drugs on the duration of anesthesia and pain in various motor states and other long-term consequences of the femoral and hip operations are studied in the future works.
Conclusion
In patients with femoral or hip fracture, bupivacaine with 0.3% concentration in fascia iliaca block can cause lower pain score than bupivacaine with 0.2% concentration after the operation, but the satisfaction of patients with pain control and motor block severity is higher in 0.2% concentration.
Thus, use of 0.2% concentration in fascia iliaca block is recommended for postoperative pain control in patients with femoral or hip fracture.
Acknowledgements
The authors wish to acknowledge all the participating teams who have helped us on this project.
Conflict of interest
The authors have no conflicts of interest to declare.
Cite this article as: Rahimzadeh P, Imani F, Sayarifard A, Sayarifard S, Faiz SHR. Ultrasound-guided fascia iliaca compartment block in orthopedic fractures: Bupivacaine 0.2% or 0.3%?. Med J Islam Repub Iran 2016 (24 October). Vol. 30:433.
References
- 1.Kearns RJ, Macfarlane AJ, Anderson KJ, Kinsella J. Intrathecal opioid versus ultrasound guided fascia iliaca plane block for analgesia after primary hip arthroplasty: study protocol for a randomised, blinded, noninferiority controlled trial. Trials . 2011 Feb21;12:51. doi: 10.1186/1745-6215-12-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rahimzadeh P, Imani F, Faiz SH, Nikoubakht N, Sayarifard A. Effect of intravenous methyl-prednisolone on pain after intertrochanteric femor-al fracture surgery. J Clin Diagn Res. 2014 Apr;8(4):GC01–4. doi: 10.7860/JCDR/2014/8232.4305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joshi GP, Ogunnaike BO. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North America. 2005 Mar;23(1):21–36. doi: 10.1016/j.atc.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Xie Z, Hussain W, Cutter TW, Apfelbaum JL, Drum ML, Manning DW. Three-in-one nerve block with different concentrations of bupivacaine in total knee arthroplasty: randomized, placebo-controlled, double-blind trial. J Arthroplasty. 2012 May;27(5):673–8. doi: 10.1016/j.arth.2011.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Mosaffa F, Salimi A. Evaluation of the analgesic effects of two doses of verapamil added to bupivacaine compared with bupivacaine alone in interscalene. Journal of Anesthesiology and intensive care. 2005;51(3):8–22. [Google Scholar]
- 6.Paul JE, Arya A, Hurlburt L, Cheng J, Thabane L, Tidy A. et al. Femoral nerve block improves analgesia outcome after total knee arthroplasty A meta-analysis of randomized controlled trials. Anesthesiology. 2010 Nov;113(5):1144–62. doi: 10.1097/ALN.0b013e3181f4b18. [DOI] [PubMed] [Google Scholar]
- 7.Hadzic A, Houle TT, Capdevila X, Ilfeld BM. Femoral nerve block for analgesia in patients having knee arthroplasty. Anesthesiology. 2010 Nov;113(5):1014–5. doi: 10.1097/ALN.0b013e3181f4b43d. [DOI] [PubMed] [Google Scholar]
- 8.Xu J, Chen XM , Ma CK, Wang XR . Peripheral nerve blocks for postoperative pain after major knee surgery . Cochrane Database Syst Rev. 2014;(12):CD010937. doi: 10.1002/14651858.CD010937.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Chan EY, Fransen M, Parker DA, Assam PN, Chua N. Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst Rev. 2014 May 13;(5):CD009941. doi: 10.1002/14651858.CD009941.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bouderka MA, Al-Harrar R, Bouaggad A, Harti A. Neostigmine added to bupivacaine in axillary plexus block: which benefit? Ann Fr Anesth Reanim. 2003 Jun;22(6):510–3. doi: 10.1016/s0750-7658(03)00184-9. [DOI] [PubMed] [Google Scholar]
- 11.Hay DC, Mayle Jr RE, Goodman SB. Third-degree heart block associated with bupivacaine infusion following total knee arthroplasty. J Bone Joint Surg Am. 2009 Sep;91(9):2238–40. doi: 10.2106/JBJS.H.00723. [DOI] [PubMed] [Google Scholar]
- 12.Bickler P, Brandes J, Lee M, Bozic K, Chesbro B, Claassen J. Bleeding complications from femoral and sciatic nerve catheters in patients receiving low molecular weight heparin. Anesth Analg. 2006 Oct;103(4):1036–7. doi: 10.1213/01.ane.0000237230.40246.44. [DOI] [PubMed] [Google Scholar]
- 13.Kumar N S, N K, M R, Sebastian D, Gowda Rm P. Dexamethasone as an additive to bupivacaine in fascia lliaca compartment block: a prospective, randomized and double blind study. J Clin Diagn Res. 2014 Aug;8(8):GC05–8. doi: 10.7860/JCDR/2014/8754.4687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krych AJ, Baran S, Kuzma SA, Smith HM, Johnson RL, Levy BA. Utility of multimodal analgesia with fascia iliaca blockade for acute pain management following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014 Apr;22(4):843–7. doi: 10.1007/s00167-013-2665-y. [DOI] [PubMed] [Google Scholar]
- 15.Fujihara Y, Fukunishi S, Nishio S, Miura J, Koyanagi S, Yoshiya S. Fascia iliaca compartment block: its efficacy in pain control for patients with proximal femoral fracture. J Orthop Sci. 2013 Sep;18(5):793–7. doi: 10.1007/s00776-013-0417-y. [DOI] [PubMed] [Google Scholar]
- 16.Høgh A, Dremstrup L, Jensen SS, Lindholt J. Fascia iliaca compartment block performed by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. Strategies Trauma Limb Reconstr. 2008 Sep;3(2):65–70. doi: 10.1007/s11751-008-0037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dulaney-Cripe E, Hadaway S, Bauman R, Trame C, Smith C, Sillaman B, Laughlin R. A Continuous infusion fascia iliaca compartment block in hip fracture patients: a pilot study. J Clin Med Res. 2012 Feb;4(1):45–8. doi: 10.4021/jocmr724w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zohar E, Luban I, Zunser I, Shapiro A, Jedeikin R, Fredman B. Patient – controlled bupivacaine wound Instillation following cesarean section: the lack of efficacy of adjuvant ketamine. J Clin Anesth. 2002 Nov;14(7):505–11. doi: 10.1016/s0952-8180(02)00422-1. [DOI] [PubMed] [Google Scholar]
- 19.Zohar E, Shapiro A, Phillipov A, Hoppenstein D, Klein Z, Fredman B. The post operative Analogesic efficacy of wound instillation with Ropivacaine 01% versus Ropivacain 02% J Clin Anesth. 2004 Sep;16(6):399–404. doi: 10.1016/j.jclinane.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Mulroy MF, Larkin KL, Batra MS, Hodgson PS, Owens BD. Femoral nerve block with 025% or 05% bupivacaine improves postoperative analgesia following outpatient arthroscopic anterior cruciate ligament repair. Reg Anesth Pain Med. 2001 Jan-Feb;26(1):24–9. doi: 10.1053/rapm.2001.20773. [DOI] [PubMed] [Google Scholar]
- 21.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SFMPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measu re of Intermittent and Constant OsteoarthritisPain (ICOAP) Arthritis Care Res (Hoboken) 2011 Nov;63 Suppl 11:S240–52. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 22.Sessler CN, Jo Grap M, Ramsay MA. Evaluating and monitoring analgesia and sedation in the intensive care unit. Critical Care. 2008;12(Suppl 3):S2. doi: 10.1186/cc6148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cuvillon P, Nouvellon E, Ripart J, Boyer JC, Dehour L, Mahamat A, L'hermite J, Boisson C, Vialles N, Lefrant JY, de La Coussaye JE. A comparison of the pharmacodynamics and pharmacokinetics of bupivacaine, ropivacaine (with epinephrine) and their equal volume mixtures with lidocaine used for femoral and sciatic nerve blocks: a double-blind randomized study. Anesth Analg. 2009 Feb;108(2):641–9. doi: 10.1213/ane.0b013e31819237f8. [DOI] [PubMed] [Google Scholar]
- 24.Karnawat R, Chhabra S, Mohammed S, Paliwal B. Comparison of Effect of Epidural Bupivacaine, Epidural Bupivacaine Plus Fentanyl and Epidural Bupivacaine Plus Clonidine on Postoperative Analgesia after Hip Surgery. J Anesth Clin Res. 2013;4(12):370–376. [Google Scholar]
- 25.de Lima E Souza R, Correa CH, Henriques MD, de Oliveira CB, Nunes TA, Gomez RS. Single-injection femoral nerve block with 025% ropivacaine or 025% bupivacaine for postoperative analgesia after total knee replacement or anterior cruciate ligament reconstruction. J Clin Anesth. 2008 Nov;20(7):521–7. doi: 10.1016/j.jclinane.2008.05.016. [DOI] [PubMed] [Google Scholar]


