Abstract
Background: Breastfeeding has been recognized to have a great deal of benefits for both the mothers and infants. Moreover, the importance of exclusive breastfeeding in the first six months of life has been greatly acknowledged. Therefore, this study aimed to determine the prevalence of starting breastfeeding in the first hour after delivery and the exclusive breast milk feeding as well as the age at which complimentary foods are provided to the child and duration of breastfeeding in Iran.
Methods: This nationwide cross-sectional study was conducted in the frame of a national survey, Iran Multiple Indicator Demographic and Health Survey (IrMIDHS), in 31 provinces of Iran. Participants were selected by multistage cluster sampling. The target sample was 3,096 clusters consisting of 2,187 urban and 909 rural families. Data were collected using a questionnaire through face-to-face interviews.
Results: The rate of exclusive breastfeeding was 53.13% with higher prevalence in rural (67.76%) than in urban areas (47.79%) (P = 0.04), and among girls (56.35%) compared to boys (50.60%). The prevalence of breastfeeding as the main diet of Iranian infants under six months old was 70.72% and the prevalence of initiation of breastfeeding (up to the first hour after delivery) was 68.70%. The probability of breastfeeding continuance among twelve to fifteen months children was 84.22%; the corresponding figure was 51% among twenty to twenty three months old babies (p=0.03).
Conclusion: Exclusive breastfeeding should be encouraged; and strategies that are more effective should be designed to protect, train and support young mothers to breastfeed their infants. The importance of early beginning of breastfeeding and its continuation should be underscored.
Keywords: Breastfeeding, Infant, Prevalence, Iran
Introduction
Exclusive breastfeeding in the first six months of life is assumed as the most appropriate type of feeding for infants (1-4). Starting complementary foods for six month old babies and continuing breastfeeding until they are 24 months old have several short and long-term benefits for children (5-16). In addition to its benefits during childhood and acting as a protective factor for infectious diseases, breastfeeding has a protective role against chronic diseases; e.g., for different malignancies (5,9), allergic diseases (5-8) and obesity (10-13). Longitudinal studies revealed that breast fed infants will not only have faster development in their cognitive behavior, but they will also be more successful in their academic experiences (15,16). Furthermore, breastfeeding has numerous benefits for maternal health; e.g., reducing the susceptibility to type 2 diabetes, ovarian and breast cancer (5).
Therefore, from 2002, the World Health Organization proposed exclusive breast milk feeding for six months (4,17). This schedule was complemented by continuation of breastfeeding until babies reach two years of age (18-20). Different factors such as cultural and economic status of family, religious beliefs, lifestyle, mother’s employment, parental education, age of marriage, maternal age, advertisement of infant formula companies and motto broadcasting of exclusive breastfeeding by healthcare providers and media affect the prevalence of breastfeeding and its maintenance (19,20). A study conducted in the framework of Demographic and Health Survey (DHS) in Iran revealed that the prevalence of exclusive breastfeeding was 70%, 44.1% and 23.1% in 1991, 2000 and 2005, respectively. However, in 2005, this prevalence varied from 22.7% to 24% in urban and rural areas, respectively (21).
This national study aimed to determine the prevalence of beginning breastfeeding in the first hour after delivery, exclusive breast milk feeding, as well as the age of initiating complimentary feeding and duration of breastfeeding in Iran.
Methods
Data and Instruments
This study was conducted in the framework of a nationwide health survey, entitled as “Iran Multiple Indicator Demographic and Health Survey (IrMIDHS)”, which aimed to provide data on population and health outcomes. The detailed methodology has been published (22); therefore, herein we present it in brief. The survey was conducted in 31 provinces in Iran during 2010. The study was approved by the relevant authorities within the Ministry of Health and Medical Education (MoHME) and the Statistics Center of Iran. All household members who were permanent residents (more than 6 months) of the household were eligible for inclusion in the household members list. The study protocol did not allow substitution of non-responses by another household member; all efforts were made to minimize non-response.
In each district, clusters were identified at random. Then in each cluster, a systematic sample of 10 households was consecutively selected. All women aged 15-54 and mothers or caregivers of all children younger than five years of age were also eligible for interview.
This cross-sectional study was conducted as a multi-stage stratified cluster-random survey by face-to-face household interviews. The sampling framework was developed using Iran's 2006 population and housing census. Provincial samples ranged from 400 to 6,400 households in various areas. The target sample was 3,096 clusters consisting of 2,187 urban and 909 rural ones. Pamphlets about the importance of the survey, its confidentiality and freeness of the eligible family to participate or refuse the study were prepared for the selected households at least one day prior to the interview. At the beginning of the interview, written consent was obtained from the eligible individuals.
Three types of questionnaires, which were validated previously, were completed for the households (107 questions), for 15-54-year old women (145 questions), and for children younger than five years (88 questions). The questionnaires were researcher-made and showed relative content validity through expert panel opinions.
Ethical committees and relevant authorities in the Ministry of Health and Medical Education and in the Statistics Center of Iran approved the study. A multi-layer supervision and monitoring procedure was established, and all questionnaires were entered twice. The central team conducted a subsequent check of a random sample of the variables. We used the data related to the following items:
Exclusive breastfeeding in infants younger than six months: Percent of infants fed exclusively via breastfeeding.
Breastfeeding as the main nutritional diet in infants younger than six months: Percent of infants fed mainly via breastfeeding.
Percent of infants aged 6-8 months who received complimentary foods
Likelihood of continuing breastfeeding in infants from 12 to 15 months of age: Percent of 12-15-month old children who are presently fed via breastfeeding
Likelihood of continuing breastfeeding in infants from 20 to 23 months of age: Percent of 20-23-month old children who are presently fed via breastfeeding
Bottle-feeding: Number of babies younger than 24 months who were fed via bottle in the day prior to the interview
Duration of breastfeeding
Appropriate time for the initiation of breastfeeding: Percent of mothers with live babies (from two years prior to the survey), who began breastfeeding in the first hour after delivery
After the interview, the field supervisor checked the completed questionnaires. Obvious mistakes and omissions were corrected; when necessary the household was contacted before data entry.
Special data-entry software was prepared. The CSProbased on the CSPro software (provided to the team by the UNICEF) was customized to IrIMDHS questionnaires. The customized data collection software was heavily tested using actual data from three provinces to ensure it was free of bugs and errors. The software provided the opportunity for dual data entry.
Statistical Analysis
Data were analyzed using SPSS-PC Version 18.0 (SPSS Inc., Chicago, IL, USA). The prevalence of exclusive breastfeeding, bottle feeding and initiating breastfeeding in the first hour after birth was shown according to gender and living area. P value less than 0.05 was considered as statistically significant.
Results
This national survey demonstrated that the prevalence of exclusive breastfeeding among Iranian infants under six months of age was 53.13%. A total of 29,609 families from 31,350 predesigned families participated in the study (94.5% participation rate). The prevalence of exclusive breastfeeding among Iranian children aged less than 6 months according to gender and living area is presented in Figure 1.
Fig. 1.
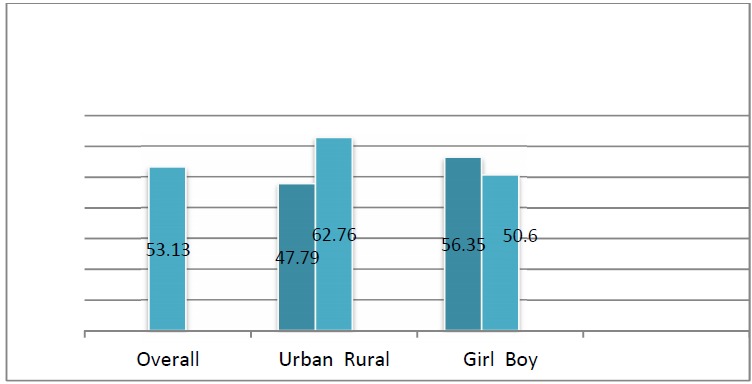
Prevalence of Exclusive Breastfeeding among Iranian Children Younger than 6 months According to Gender and Living Area
This study revealed that the initiation of complementary food (including solid, semi-solid and mashed food) was 75.92% among infants from six to eight months. This figure was different between rural and urban inhabitants (72.97% vs. 77.65%, respectively), and according to gender (71.46% vs. 80.60% in boys and girls, respectively). The likelihood of continuing breastfeeding among 12-15-month-infants was 84.22%, with a different pattern in rural and urban districts (88.74% vs. 81.39%, respectively), and in boys and girls (86.39% vs. 81.48%). Furthermore, the probability of continuing breastfeeding in infants aged 20-23 months was 51%, ranging from 50.48% to 53.3% in urban and rural areas, respectively. The corresponding figure was 52.20% in boys and 49.70% in girls. The prevalence of bottle-feeding among Iranian children younger than 23 months is summarized in Figure 2, presented by gender and living area. The initiation of breastfeeding in the first hour after delivery was reported to be 68.7%.This percentage differed in rural and urban areas (70.64% vs. 67.59%, respectively), as well as among boys (63.59%) and girls (66.64%). The prevalence of beginning breastfeeding immediately during the first hour after birth among Iranian children according to gender and living area is shown in Figure 3. The prevalence of exclusive breastfeeding among Iranian children aged less than six months across the country is demonstrated in Figure 4.
Fig. 2.
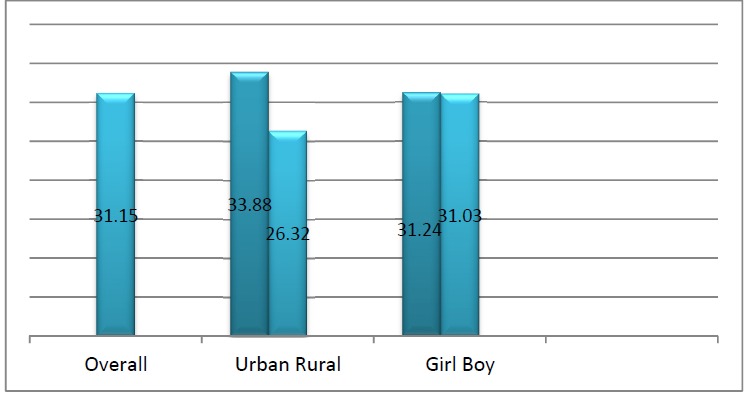
Prevalence of Bottle-Feeding among Iranian Children Younger than 23 Months According to Gender and Living Area
Fig. 3.
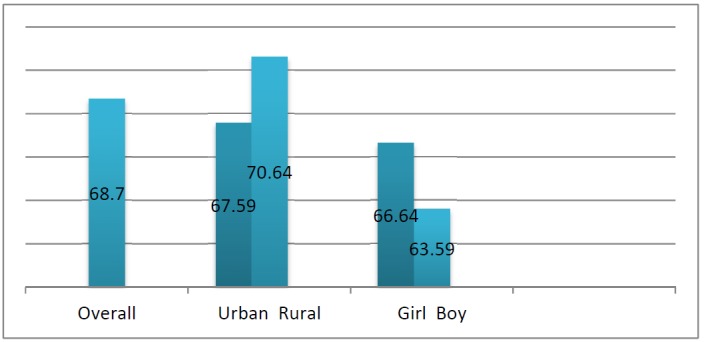
Prevalence of Initiating Breastfeeding in the First Hour after Birth among Iranian Children according to Gender and Living Area
Fig. 4.
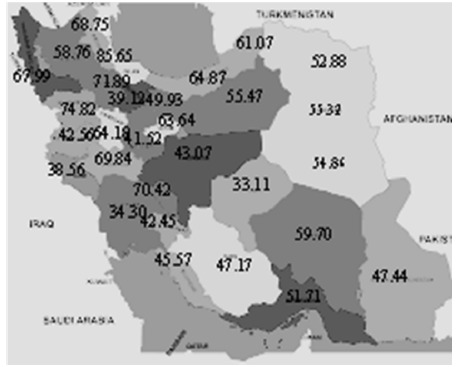
Prevalence of Exclusive Breastfeeding among Iranian Children Younger than 6 Months across the Country
Discussion
This study presented the prevalence rates related to beginning and continuing breastfeeding in a nationwide population-based sample of Iranian children.
We found that the frequency of exclusive breastfeeding in the first six months of life was 53.13% in Iranian infants. During 2000 to 2006, the rate of exclusive breastfeeding (until six months of age) reported to be 28% in the Middle-East North Africa (MENA) region (23). This prevalence varies in different countries located in the MENA region; for instance, it is reported to be 16% in Pakistan, 25% in Iraq, 38% in Saudi Arabia and 44% in Iran (23).
Similarly, compared to some Western countries, Iran has a higher rate of breastfeeding. A study that compared breastfeeding in Iran and Australia revealed higher prevalence of breastfeeding in Iran; it also showed that Australian women usually discontinue breastfeeding before the recommended time. Variables that negatively contributed to the lower breastfeeding practice might be inadequate national programs to encourage mothers to breastfeed, less uptake of Baby-Friendly Hospital Initiative, cultural problems and less supported return to work in Australia (24). A similar pattern has been reported from Canada (25), where the rate of breastfeeding initiation (90.3%) and intention (90.0%) was relatively high, exclusive breastfeeding duration decreased compared to globally recommended standards. Exclusive breastfeeding rates at 6 months after birth (14.4%) were lower than the desirable rate, emphasizing a low adherence to several best practices supported by the Baby-Friendly Hospital Initiative (25).
The frequency of exclusive breastfeeding in Iran declined from 70% in 1991 to 27% in 2004. However, such national activities as increasing public awareness, encouraging mothers, governmental support, breastfeeding education, increased knowledge and awareness of young mothers as well as improving their attitudes toward breastfeeding benefits for both mothers and neonates have led to the relative increment in breastfeeding initiation and promotion in Iran (26,27).
In 2000, the national DHS found that approximately 90% of Iranian infants received breastfeeding, whereas the rate of exclusive breastfeeding at six months of age was less than 45%. In 2000, 44% of infants were exclusively breastfed and the trend was dropped to 27% in 2004 (27).
The health benefits of breastfeeding to growth and development of infants and the overall health condition of mothers are well established (26,28). However, its pattern varies between diverse populations and these differences might origin from varying socio-cultural factors. Despite a widespread knowledge and outstanding efforts to promote breastfeeding due to its unique biological and emotional effects on the health status of both the mother and child, still a large number of mothers use artificial formulas for their children. In our study, breastfeeding was more prevalent in rural than urban areas. Less than half of young urban mothers living in urban areas nursed their infants. This finding is consistent with previous studies in Iran indicating that only 46.5% of mothers exclusively breastfed their babies in the first six months of life (29-31).
Factors as early initiation of formula supplementation in hospitals, widespread conflicting infant feeding advices, mothers poor intention for breastfeeding initiation and continuance have negative impacts on breastfeeding practices (29). In our study, the differences in the prevalence of breastfeeding between urban and rural mothers may be explained by more commitment to the traditional culture in the rural than in the urban districts, and lower frequency of working out of home in the rural than in the urban areas. On the other hand, early return to work, higher socio-economic status and higher educational level might contribute to lower rates of breastfeeding among urban than in rural mothers (30).
Our findings are consistent with some previous studies that showed living in rural area, the increment in birth order and being a housewife were associated with longer duration of breastfeeding practice (31). Furthermore, high level of stress has been suggested to increase the risk of early weaning (31). It seems that more practical approaches including higher health education efforts are necessary to support and promote the practice of breastfeeding, especially among young, less educated urban mothers who are employees (31).
The breastfeeding tradition is well-known in Iran and its history refers to the fourth century in the Canon Medicine of Avicenna (32). Because of the unique and long-term benefits of human milk (33,34), breastfeeding has been extensively encouraged in Iran (35); however, its facilitators and barriers should be studied and managed in more detail to encourage and promote breastfeeding.
Study Limitations and Strengths: The main limitation of this study was its cross-sectional nature. Moreover, the recall bias of reporting the prevalence and duration of breastfeeding practice during the interview process might have occurred. We did not assess the determinants and factors associated with breastfeeding experiences. The main strength of this study was its nationwide coverage and including both urban and rural residents. Therefore, our findings could present a comprehensive picture of breastfeeding rates across the country.
Conclusion
Breastfeeding rate in Iran is in a good condition compared to several developing and developed countries. However, the prevalence of exclusive breastfeeding indicated a downward trend at 4 and 6 months of life. Protection, promotion and supportive programs are necessary for the initiation and increased duration of breastfeeding to meet the World Health Organization (WHO) recommendations.
Acknowledgements
The study was conducted as a national health survey, and received partial support from the United Nations Population Fund (UNFPA) and the United Nations Children’s Fund. We thank the UNFPA for provision of financial support for the preparation of this paper.
Conflict of Interest
The authors declared there is no conflict of interest.
Cite this article as: Kelishadi R, Rashidian A, Jari M, Khosravi A, Khabiri R, Elahi E, Bahreynian M. A national survey on the pattern of breastfeeding in Iranian infants: The IrMIDHS study. Med J Islam Repub Iran 2016 (16 October). Vol. 30:425.
References
- 1.Espinoza H, Lutter C, Rabeneck S. Breastfeeding and Complementary Feeding In: Nutrition Throughout the Life Cycle 4th Report on The World Nutrition Situation. Sub-Committee on Nutrition (ACC/SCN) and International Food Policy Research Institute (IFPRI) 2000:33–9. [Google Scholar]
- 2. Horta B. Evidence on the long-term effects of breastfeeding, Geneva: World Health Organization 2007.
- 3.Quigley MA, Kelly YJ, Sacker A. Breastfeeding and hospitalization for diarrheal and respiratory infection in the United Kingdom Millennium Cohort Study. Pediatrics. 2007 Apr;119(4):e837–42. doi: 10.1542/peds.2006-2256. [DOI] [PubMed] [Google Scholar]
- 4. Kramer MS, Kakuma R. The optimal duration of exclusive breastfeeding. A Systematic review. (Report No.WHO/NHD/01.08). Geneva, World Health Organization,2002. 2002.
- 5. Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evidence report/technology assessment 2007 Apr; 153:1-186. [PMC free article] [PubMed]
- 6.Saarinen UM, Kajosaari M. Breastfeeding as prophylaxis against atopic disease: prospective follow-up study until 17 years old. Lancet . 1995 Oct 21;346(8982):1065–9. doi: 10.1016/s0140-6736(95)91742-x. [DOI] [PubMed] [Google Scholar]
- 7.Gdalevich M, Mimouni D, David M, Mimouni M. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. Journal of the American Academy of Dermatology. 2001 Oct;45(4):520–7. doi: 10.1067/mjd.2001.114741. [DOI] [PubMed] [Google Scholar]
- 8.Gdalevich M, Mimouni D, Mimouni M. Breast-feeding and the risk of bronchial asthma in childhood: a systematic review with meta-analysis of prospective studies. The Journal of pediatrics. 2001 Aug;139(2):261–6. doi: 10.1067/mpd.2001.117006. [DOI] [PubMed] [Google Scholar]
- 9.Davis MK. Review of the evidence for an association between infant feeding and childhood cancer. International journal of cancer Supplement = Journal international du cancer Supplement. 1998;11:29–33. [PubMed] [Google Scholar]
- 10.Kelishadi R, Hashemi poor M, Famoori F, Sabet B. Breastfeeding effect in prevention of obesity in children. J Qazvin University of Medicine. 2005;9(2):60–4. (Persian). [Google Scholar]
- 11.Mayer-Davis EJ, Rifas-Shiman SL, Zhou L, Hu FB, Colditz GA, Gillman MW. Breast-feeding and risk for childhood obesity: does maternal diabetes or obesity status matter? Diabetes care. 2006 Oct;29(10):2231–7. doi: 10.2337/dc06-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weyermann M, Rothenbacher D, Brenner H. Duration of breastfeeding and risk of overweight in childhood: a prospective birth cohort study from Germany. International journal of obesity (2005) 2006 Aug;30(8):1281–7. doi: 10.1038/sj.ijo.0803260. [DOI] [PubMed] [Google Scholar]
- 13.Gillman MW, Rifas-Shiman SL, Camargo CA Jr, Berkey CS, Frazier AL, Rockett HR. et al. Risk of overweight among adolescents who were breastfed as infants. JAMA : the journal of the American Medical Association. 2001 May 16;285(19):2461–7. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- 14.von Kries R, Koletzko B, Sauerwald T, von Mutius E, Barnert D, Grunert V. et al. Breast feeding and obesity: cross sectional study. BMJ (Clinical research ed) . 1999 Jul 17;319(7203):147–50. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lucas A, Morley R, Cole TJ, Lister G, Leeson-Payne C. Breast milk and subsequent intelligence quotient in children born preterm. Lancet . 1992 Feb 1;339(8788):261–4. doi: 10.1016/0140-6736(92)91329-7. [DOI] [PubMed] [Google Scholar]
- 16.Horwood LJ, Fergusson DM. Breastfeeding and later cognitive and academic outcomes. Pediatrics. 1998 Jan;101(1):E9. doi: 10.1542/peds.101.1.e9. [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization. Global Strategy for Infant and Young Child Feeding. 54th World Health Assembly (Report no. A54/INF.DOC./4). Geneva WHO. 2001.
- 18.Merewood A, Patel B, Newton KN, MacAuley LP, Chamberlain LB, Francisco P. et al. Breastfeeding duration rates and factors affecting continued breastfeeding among infants born at an inner-city US Baby-Friendly hospital. Journal of human lactation : official journal of International Lactation Consultant Association. 2007 May;23(2):157–64. doi: 10.1177/0890334407300573. [DOI] [PubMed] [Google Scholar]
- 19.Lee WT, Wong E, Lui SS, Chan V, Lau J. Decision to breastfeed and early cessation of breastfeeding in infants below 6 months old--a population-based study of 3,204 infants in Hong Kong. Asia Pacific journal of clinical nutrition. 2007;16(1):163–71. [PubMed] [Google Scholar]
- 20. Li R, Zhao Z, Mokdad A, Barker L, Grummer-Strawn L. Prevalence of breastfeeding in the United States: the 2001 National Immunization Survey. Pediatrics 2003 May;111(5 Pt 2):1198-201. [PubMed]
- 21.Khabazkhoob M, Fotoohi A, Majdi M, Moradi A, Javaharforoosh A, Haerikermani Z. et al. Breastfeeding and some factors associated with in children in Mashhad. Iran Epidemiology Special Journal. 2007;3(384):45–53. (Persian). [Google Scholar]
- 22.Rashidian A, Karimi-Shahanjarini A, Khosravi A, Elahi E, Beheshtian M, Shakibazadeh E. et al. Iran's Multiple Indicator Demographic and Health Survey - 2010: Study Protocol. International journal of preventive medicine. 2014 May;5(5):632–42. [PMC free article] [PubMed] [Google Scholar]
- 23. The state of the world's children. 2008, [Child survival] New York: Unicef; 2007.
- 24.Zareai M, O'Brien ML, Fallon AB. Creating a breastfeeding culture: a comparison of breastfeeding practises in Australia and Iran. Breastfeeding review : professional publication of the Nursing Mothers' Association of Australia. 2007 Jul;15(2):15–20. [PubMed] [Google Scholar]
- 25.Chalmers B, Levitt C, Heaman M, O'Brien B, Sauve R, Kaczorowski J. Breastfeeding rates and hospital breastfeeding practices in Canada: a national survey of women. Birth (Berkeley, Calif) 2009 Jun;36(2):122–32. doi: 10.1111/j.1523-536X.2009.00309.x. [DOI] [PubMed] [Google Scholar]
- 26.Kramer MS, Kakuma R. The optimal duration of exclusive breastfeeding: a systematic review. Advances in experimental medicine and biology. 2004;554:63–77. doi: 10.1007/978-1-4757-4242-8_7. [DOI] [PubMed] [Google Scholar]
- 27. The Ministry of Health IR of Iran, Breastfeeding office [http://www.bfps.ir/(i5emlr 45w1kdeg45tov0ysem)/Persian/Home.aspx].
- 28.Binns CW, Lee MK. Exclusive breastfeeding for six months: the WHO sixmonths recommendation in the Asia Pacific Region. Asia Pacific journal of clinical nutrition. 2014 Sep;23(3):344–50. doi: 10.6133/apjcn.2014.23.3.21. [DOI] [PubMed] [Google Scholar]
- 29.Noughabi ZS, Tehrani SG, Foroushani AR, Nayeri F, Baheiraei A. Prevalence and factors associated with exclusive breastfeeding at 6 months of life in Tehran: a population-based study. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. 2014 Jan;20(1):24–32. [PubMed] [Google Scholar]
- 30.Olang B, Farivar K, Heidarzadeh A, Strandvik B, Yngve A. Breastfeeding in Iran: prevalence, duration and current recommendations. International breastfeeding journal. 2009;4:8. doi: 10.1186/1746-4358-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hajian-Tilaki KO. Factors associated with the pattern of breastfeeding in the north of Iran. Annals of human biology. 2005 Nov-Dec;32(6):702–13. doi: 10.1080/03014460500272764. [DOI] [PubMed] [Google Scholar]
- 32.Modanlou HD. Avicenna (AD 980 to 1037) and the care of the newborn infant and breastfeeding. Journal of perinatology : official journal of the California Perinatal Association. 2008 Jan;28(1):3–6. doi: 10.1038/sj.jp.7211832. [DOI] [PubMed] [Google Scholar]
- 33.Kelishadi R, Farajian S. The protective effects of breastfeeding on chronicnon-communicable diseases in adulthood: A review of evidence. Adv Biomed Res . 2014 Jan 9;3:3. doi: 10.4103/2277-9175.124629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kelishadi R, Ardalan G, Gheiratmand R, Majdzadeh R, Delavari A, Heshmat R. et al. CASPIAN Study Group Blood pressure and its influencing factors in a nationalrepresentative sample of Iranian children and adolescents: the CASPIAN Study. EurJ CardiovascPrevRehabil. 2006;13(6):956–63. doi: 10.1097/01.hjr.0000219109.17791.b6. [DOI] [PubMed] [Google Scholar]
- 35.Marandi SA, Ezzeddin-Zanjani N. On the occasion of the world breastfeedingweek: the promotion of breastfeeding in the IR Iran. Int J Prev Med. 2012;3(8):520–1. [PMC free article] [PubMed] [Google Scholar]


