Abstract
Background:
Airway management is critical in patients with cervical spondylosis, a population with a high incidence of difficult airway. Intubation with Shikani Optical Stylet (SOS) has become increasingly popular in difficult airway. We compared the effects of intubation with SOS versus Macintosh laryngoscope (MLS) in patients undergoing surgery for cervical spondylosis.
Methods:
A total of 270 patients scheduled for elective surgery for cervical spondylosis of spinal cord and nerve root type from August 2012 to January 2016 were enrolled and randomly allocated to the MLS or SOS group by random numbers. Patients were evaluated for difficult airway preoperatively, and Cormack-Lehane laryngoscopy classification was determined during anesthesia induction. Difficult airway was defined as Cormack-Lehane Grades III–IV. Patients were intubated with the randomly assigned intubation device. The success rate, intubation time, required assistance, immediate complications, and postoperative complaints were recorded. Categorical variables were analyzed by Chi-square test, and continuous variables were analyzed by independent samples t-test or rank sum test.
Results:
The success rate of intubation among normal airways was 100% in both groups. In patients with difficult airway, the success rates in the MLS and SOS groups were 84.2% and 94.1%, respectively (P = 0.605). Intubation with SOS took longer compared with MLS (normal airway: 25.1 ± 5.8 s vs. 24.5 ± 5.7 s, P = 0.426; difficult airway: 38.5 ± 8.5 s vs. 36.1 ± 8.2 s, P = 0.389). Intubation with SOS required less assistance in patients with difficult airway (5.9% vs. 100%, P < 0.001). The frequency of postoperative sore throat was lower in SOS group versus MLS group in patients with normal airway (22.0% vs. 34.5%, P = 0.034).
Conclusions:
SOS is a safe and effective airway management device in patients undergoing surgery for cervical spondylosis. Compared with MLS, SOS appears clinically beneficial for intubation, especially in patients with difficult airway.
Trial Registration:
Chinese Clinical Trial Registry, ChiCTR-IOR-16007821; http://www.chictr.org.cn/showproj.aspx?proj=13203.
Keywords: Airway, Cervical Spondylosis, Intubation, Laryngoscope, Optical Stylet
Introduction
Airway management is critical in anesthesia. Difficult airway is associated with certain adverse effects and trauma. Patients undergoing elective surgery for cervical spondylosis have a higher incidence of difficult airway because of limited neck mobility.[1,2] Endotracheal intubation with the traditionally used Macintosh laryngoscope (MLS) might occasionally be impossible in these patients. A variety of devices have been developed to replace MLS to increase the success rate and decrease the related complications.
The Shikani Optical Stylet (SOS) is manufactured with unique features. It combines the advantages of the visibility of an optical laryngoscope, plasticity of a fiber bronchoscope, and portability of a traditional laryngoscope. It is an effective device in the management of difficult airway.[3] One of the beneficial characteristics of SOS is that it adapts to the natural curve of the airway, allowing intubation without aligning the oral, pharyngeal, and tracheal axes. Therefore, SOS might be a better solution for intubation in patients undergoing surgery for cervical spondylosis, an issue that has been infrequently investigated, especially in patients with difficult airway. This study evaluated the differences between SOS and MLS in endotracheal intubation, including the success rate, intubation time, required assistance, and complications.
Methods
Participants
Ethics committee approval was obtained from the Institutional Review Board at Peking University Third Hospital (No. 2012079 and No. 2015021), and written informed consent was obtained from all participants.
We enrolled 270 patients with American Society of Anesthesiologist's Score I–III, aged between 18 and 75 years who were scheduled for elective surgery for cervical spondylosis of spinal cord and nerve root type under general anesthesia with tracheal intubation from August 2012 to January 2016 (inclusion criteria). Patients were randomly assigned by random numbers generated by Statistical Product and Service Solutions (SPSS) version 19.0 (SPSS Inc., Chicago, IL, USA) to MLS group or SOS group. Exclusion criteria were as follows: patients with cervical spine instability and ankylosing spondylitis, oropharyngeal mass, airway disease, obstructive sleep apnea, and a potential risk of difficult face mask ventilation.
Measurements
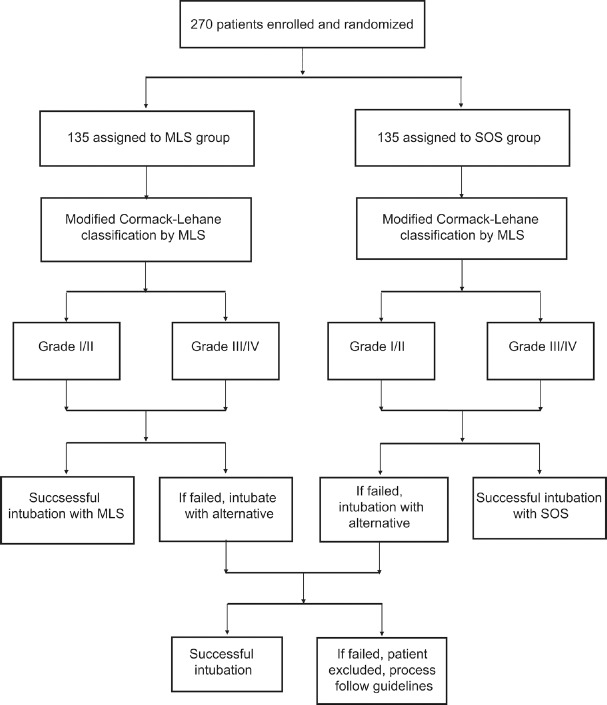
General condition, modified Mallampati classification, mouth opening, thyromental distance, sternomental distance, and neck mobility were evaluated for risks of difficult airway, preoperatively, by an anesthesiologist blinded to the study schemes and not involved in the following procedures. Routine noninvasive monitoring was established before induction of anesthesia, including noninvasive blood pressure (NBP), heart rate (HR), pulse oximetry (SpO2), and electrocardiography (ECG). All patients were preoxygenated with 100% oxygen for 3 min and received intravenous fentanyl at 3 μg/kg and target-controlled infusion (Graseby 3500, AstraZeneca, UK) of propofol 3.5 μg/ml (plasma concentration) for induction of anesthesia. Patients were manually ventilated following loss of consciousness. Neuromuscular blockage was achieved with vecuronium bromide at 0.1 mg/kg. Modified Cormack-Lehane classification was determined with MLS in the sniff position 3 min after injection of relaxant by a skilled anesthesiologist not involved in the detailed preoperative evaluation. After examination of the vocal cords, tracheal intubation was performed with the randomly assigned device by the same anesthesiologist, who was experienced with both devices (more than 60 intubations with the SOS) and who had extensive experience using the devices in difficult airways. Intubation with SOS (Clarus Medical, Minneapolis, MN, USA) was accomplished using the left molar approach.[4] Size #7.5 reinforced tracheal catheters (Covidien, Dublin, Ireland) were used for women and #8.0 were used for men. Intubation time was recorded (time from insertion of the intubation device to the appearance of an end-tidal carbon dioxide trace on capnography) by a nurse who did not participate in the study other than recording data. The intubation attempt was stopped if more than three attempts were necessary or more than 10 min had elapsed, or if desaturation was noted on pulse oximetry (SpO2 <92.0%). If these criteria were met, patients were manually ventilated and the alternative device was used. If attempts with the alternative device failed, intubation was completed following the practice guidelines for the management of the difficult airway by the American Society of Anesthesiologists (2013) [Figure 1].[5]
Figure 1.
Flowchart outlining patient enrollment and allocation for the study. MLS: Macintosh laryngoscope; SOS: Shikani Optical Stylet.
Difficult airway was defined as Grade III–IV modified Cormack-Lehane classification, or if intubation required more than three attempts or more than 10 min, or if desaturation was noted on pulse oximetry (SpO2 <92.0%). All assistance, including external laryngeal pressure, repeated intubation, laryngoscope blade changes, and changing to other devices, were permitted and documented. The success rate for each intubation device was recorded. Immediate complications associated with intubation such as bloodstains on the device, visible lacerations in the oropharynx, and dental trauma were also noted. Postoperative complaints after extubation, such as severe sore throat, hoarseness, and odynophagia, were assessed 24 h after surgery, and patients complaining of these symptoms were followed up for 3 days, postoperatively.
The primary outcome of this study was the success rate in both laryngoscope groups. The following secondary outcomes were compared between the two groups: assistance required for intubation, intubation time, and complications.
Sample size
According to the success rates in a previous study, a sample size of 135 patients was calculated to have at least 90.0% power to detect a difference between the two groups, estimated with PASS software (version 8.03; NCSS, LLC, Kaysville, UT, USA).[6]
Statistical analysis
SPSS version 19.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Numerical variables are given as mean ± standard deviation (SD). Categorical variables were analyzed by Chi-square test, and continuous variables were analyzed by independent samples t-test or rank sum test. A value of P < 0.05 was considered statistically significant.
Results
Data from 270 patients were recorded for analysis. There were no significant differences between the two groups regarding demographic characteristics [Table 1].
Table 1.
Comparison of the demographic characteristics between the MLS group and SOS group
| General information | MLS group (n = 135) | SOS group (n = 135) | Statistics | P |
|---|---|---|---|---|
| Male/female | 81/54 | 90/45 | 1.292* | 0.256 |
| Age (years) | 53 ± 10 | 54 ± 10 | −0.511† | 0.610 |
| Height (cm) | 166 ± 8 | 167 ± 7 | −0.860† | 0.390 |
| Weight (kg) | 70 ± 12 | 71 ± 12 | −0.717† | 0.474 |
| BMI (kg/m2) | 25.3 ± 3.3 | 25.5 ± 3.4 | −0.377† | 0.706 |
| Neck mobility | ||||
| Normal mobility | 86 (63.7) | 97 (71.9) | 7.307* | 0.063 |
| 1/3 reduced | 39 (28.9) | 29 (21.5) | ||
| 2/3 reduced | 10 (7.4) | 6 (4.4) | ||
| Unable to extend | 0 | 3 (2.2) |
Data are presented as mean ± SD or n (%). *Chi-square value; †t value. MLS: Macintosh laryngoscope; SOS: Shikani Optical Stylet; BMI: Body mass index; SD: Standard deviation.
The incidence of difficult airway was 13.3% (36/270) in all patients, while 14.1% (19/135) of the patients in MLS group and 12.6% (17/135) in SOS group had Grade III/IV Cormack-Lehane classification. Intubation success rates were 97.8% (132/135) in MLS group and 99.3% (134/135) in SOS group, with no statistical difference. Intubation success rates were 100% in both groups in Cormack-Lehane Grade I/II patients and all patients were intubated successfully with the first attempt. In patients with Cormack-Lehane Grade III/IV, the intubation success rate was higher in SOS group (16/17) compared to MLS group (16/19), but no statistically significant differences were found [Table 2]. All successful intubations with the assigned device in difficult airways were completed with the first attempt. In MLS group, the glottis of three patients was still not visible with the assistance of external laryngeal pressure, and endotracheal intubations were completed by SOS. In SOS group, four patients had Grade III/IV Cormack-Lehane classification despite the assistance of external laryngeal pressure. Three patients were successfully intubated by SOS alone while the fourth was intubated with the aid of MLS.
Table 2.
Successful intubation rate comparison between the MLS and SOS groups in normal airway and difficult airway
| Success rate | MLS group (n = 135) | SOS group (n = 135) | P |
|---|---|---|---|
| Total in normal airway | 116/116 (100) | 118/118 (100) | – |
| Total in difficult airway | 16/19 (84.2) | 16/17 (94.1) | 0.605 |
Data are presented as n (%). MLS: Macintosh laryngoscope; SOS: Shikani Optical Stylet; –: No applicable.
Intubation time was longer in SOS group compared to MLS group, whether in normal airway or difficult airway, but there were no significant differences between the two groups. None of the patients with normal airway required assistance during intubation in either group. Fewer patients with difficult airway required assistance to complete the intubation in SOS group (1/17) compared to MLS group (19/19), and the difference was statistically significant. In difficult airway, three patients required more than three attempts in MLS group while this occurred in only one patient in SOS group. The occurrence of postoperative sore throat was lower in SOS group compared to MLS group in patients with normal airway. There were no statistically significant differences in the occurrence of other complications during and after intubation between the two groups in normal airways [Table 3].
Table 3.
Ease of intubation and complications between the MLS and SOS groups
| Items | MLS group (n = 116a,19b) | SOS group (n = 118a,17b) | Statistics | P |
|---|---|---|---|---|
| Intubation time (s) | ||||
| Normal airway | 24.5 ± 5.7 | 25.1 ± 5.8 | -0.798* | 0.426 |
| Difficult airway | 36.1 ± 8.2 | 38.5 ± 8.5 | -0.872* | 0.389 |
| Required assistance | ||||
| Normal airway | 0 | 0 | – | |
| Difficult airway | 19 (100) | 1 (5.9) | 32.188† | <0.001‡ |
| Intubation attempts (difficult airway) | ||||
| 1 | 16 | 16 | – | 0.605 |
| 2 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| >3 | 3 | 1 | ||
| Complication incidence (normal airway) | ||||
| Lip or mucosal trauma | 3 (2.6) | 1 (0.8) | – | 0.368 |
| Postoperative sore throat | 40 (34.5) | 26 (22.0) | 4.477† | 0.034§ |
| Postoperative odynophagia | 1 (0.9) | 0 | – | 0.496 |
Data are presented as mean ± SD or n (%). a: Normal airway; b: Difficult airway. *t value; †Chi-square value; ‡P<0.05, intubation with SOS required less assistance in patients with difficult airway. §P<0.05, the frequency of postoperative sore throat was lower in the SOS group versus the MLS group in patients with normal airway. MLS: Macintosh laryngoscope; SOS: Shikani optical stylet. –: No applicable; SD: Standard deviation.
Discussion
Airway management is one of the most critical processes in clinical anesthesia of patients with cervical spondylosis. MLS is the most commonly used intubation device. However, direct vision of the vocal cords is essential when intubating with MLS and can be complicated by the need to lift the epiglottis. Failed intubation might occur in patients with poor alignment of the mouth-pharyngeal-laryngeal axes due to limited neck extension, occasionally, and might result in unexpected cancellation of surgery or even major damage. Alternative intubation devices including SOS have been introduced to address these concerns.
SOS combines the features of a light wand and fiberoptic bronchoscope and has a J-shaped endoscope with a narrow shaft of malleable stainless steel. The left molar intubation approach is complicated by interference from the maxillary structures in the line of view. However, compared with the midline approach, the left molar approach is faster and improves glottis view, especially in patients with restricted neck mobility.[7,8] We speculated that the unique features of SOS provided advantages over MLS in improving the intubation success rate and lowering the incidence of complications. Considering the higher incidence of difficult airway in patients with cervical spondylosis and few previous studies of the airway in these patients regarding its influence on success rate and intubation time, we determined a Cormack-Lehane classification score in each patient and assigned the population to Cormack-Lehane Grade I/II (normal airway) and III/IV (difficult airway) groups. We hypothesized that a difficult airway might increase complications because of the relatively longer intubation time. Considering the variability and limited number of patients with difficult airway, we documented the complications only in patients with Cormack-Lehane Grade I/II.
The success rate was high in the study; 100% in both groups in patients with Cormack-Lehane Grade I/II. All of the successful intubations with the assigned device were completed with the first attempt including in those with difficult airway. This result was unexpected and differed from previous studies.[3,9,10,11,12] It might have resulted from the anesthesiologist's extensive experience. Patients undergoing elective surgery for cervical spondylosis carry a high risk of difficult airway. Studies have shown that the overall prevalence of difficult airway in patients undergoing cervical spine surgery is 14.9–20.0%.[1,2] In the study, the prevalence of difficult airway was 13.3%, lower than previously reported, but still much higher than in the general population (5.8%).[13] One of the reasons was that patients undergoing surgery for cervical spondylosis have variable degrees of reduced cervical mobility, which might prevent adequate alignment of the axes. The limited neck mobility hampers visualization of the glottis when direct laryngoscopy is attempted, which can make intubation with MLS more challenging. SOS can be used not only in the general population but also in patients with difficult airway.[14] In patients with Cormack-Lehane Grade III/IV, the success rate was higher in SOS group compared to MLS group (94.1% vs. 84.2%, respectively), but there were no significant differences. The success rate of the first attempt with the SOS (94.1%) in difficult airway was comparable with studies by Liu et al. (90.0%) and Phua et al. (97.0%),[6,15] much higher than that for intubation by MLS (84.2%). Previous studies showed the risk of intubation failure at first attempt was approximately 15.0–35.0% with MLS in patients with increased risk for difficult tracheal intubation.[3,16,17] Considering the clinical significance and overall intubation success rate and first attempt success, SOS appears to be preferable in intubation for this specific population.
Regarding the ease of intubation, both devices provided success with the first attempt in patients with Cormack-Lehane Grade I/II. In the study, intubation by SOS required a similar length of time compared with MLS. Both groups required no additional assistance, such as external pressure or head position change in normal airway patients. In patients with difficult airway, all patients in the MLS group required external pressure to improve visualization of the glottis while this was necessary for only one patient in the SOS group. In contrast to MLS, alignment of the mouth-pharyngeal-laryngeal axes was not necessary during intubation by SOS. The plasticity of SOS means that it can adapt to the natural curve of the airway. Liu et al.[6] also reported that SOS had advantages over MLS in the management of difficult airway. These outcomes suggest that SOS might be a better choice for managing difficult airway in patients with cervical spondylosis.
Regarding complications associated with tracheal intubation, MLS intubation can result in mucosal lacerations and sore throat because of the larger blade size and heavier lifting force to expose the glottis. More patients in the study had postoperative sore throat in the MLS group, which was consistent with this concern. In contrast, SOS might be associated with minimal trauma and a decreased incidence of airway complication because of the narrow shaft, reduced contact, and reduced force. A higher incidence of lip and upper airway injury by MLS was expected. Previous studies showed the lowest incidence of lip and mucosal trauma with SOS compared with MLS and Glidescope.[6,14] However, in the study, only three patients in MLS group and one in SOS group had evidence of small lacerations on the lip or oral mucosa. None of the four patients required further treatment, and all resolved within 24 h. These results might be related to the Cormack-Lehane classification applied in all patients before undergoing intubation and the extensive experience of the operator.
The results support the safety of intubation with SOS. Considering its potential application in other patients with limited mouth opening, loose or absent teeth, and the impact of neck movement, SOS is gaining more acceptance in clinical practice.
This study has certain limitations. First, this was a single-center study and all intubations were performed by an experienced anesthesiologist; therefore, results might differ in the hands of novices. Second, determining the Cormack-Lehane classification before intubation in all subjects helped us identify difficult airways but might also have affected the success rate of intubation and the observation of complications. Third, patients with difficult airway were limited in number, which influenced the observation of complications.
In conclusion, our results showed that SOS provides a higher success rate and a comparable intubation time with fewer adverse effects. We believe that SOS is a safe and effective intubation device for patients undergoing elective surgery for cervical spondylosis of spinal cord and nerve root type, especially for patients with difficult airways.
Financial support and sponsorship
This study was supported by a grant from the Peking University Third Hospital (No. BYSY2014019).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
References
- 1.Calder I, Calder J, Crockard HA. Difficult direct laryngoscopy in patients with cervical spine disease. Anaesthesia. 1995;50:756–63. doi: 10.1111/j.1365-2044.1995.tb06135.x. doi: 10.1111/j.1365-2044.1995.tb06135.x. [DOI] [PubMed] [Google Scholar]
- 2.Xu M, Li X, Wang J, Guo X. Application of a new combined model including radiological indicators to predict difficult airway in patients undergoing surgery for cervical spondylosis. Chin Med J. 2014;127:4043–8. doi: 10.3760/cma.j.issn.0366-6999.20141345. [PubMed] [Google Scholar]
- 3.Suppan L, Tramèr MR, Niquille M, Grosgurin O, Marti C. Alternative intubation techniques vs. Macintosh laryngoscopy in patients with cervical spine immobilization: Systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2016;116:27–36. doi: 10.1093/bja/aev205. doi: 10.1093/bja/aev205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yao YT, Jia NG, Li CH, Zhang YJ, Yin YQ. Comparison of endotracheal intubation with the Shikani Optical Stylet using the left molar approach and direct laryngoscopy. Chin Med J. 2008;121:1324–7. [PubMed] [Google Scholar]
- 5.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 6.Liu L, Yue H, Li J. Comparison of three tracheal intubation techniques in thyroid tumor patients with a difficult airway: A randomized controlled trial. Med Princ Pract. 2014;23:448–52. doi: 10.1159/000364875. doi: 10.1159/000364875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta A, Thukral S, Lakra A, Kumar S. A comparison between left molar direct laryngoscopy and the use of a Bonfils intubation fibrescope for tracheal intubation in a simulated difficult airway. Can J Anaesth. 2015;62:609–17. doi: 10.1007/s12630-015-0336-9. doi: 10.1007/s12630-015-0336-9. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto K, Tsubokawa T, Ohmura S, Itoh H, Kobayashi T. Left-molar approach improves the laryngeal view in patients with difficult laryngoscopy. Anesthesiology. 2000;92:70–4. doi: 10.1097/00000542-200001000-00016. doi: 10.1097/00000542-200001000-00016. [DOI] [PubMed] [Google Scholar]
- 9.McElwain J, Laffey JG. Comparison of the C-MAC® Airtraq® and Macintosh laryngoscopes in patients undergoing tracheal intubation with cervical spine immobilization. Br J Anaesth. 2011;107:258–64. doi: 10.1093/bja/aer099. doi: 10.1093/bja/aer099. [DOI] [PubMed] [Google Scholar]
- 10.Gaszynska E, Stankiewicz-Rudnicki M, Wieczorek A, Gaszynski T. A comparison of conventional tube and EndoFlex tube for tracheal intubation in patients with a cervical spine immobilisation. Scand J Trauma Resusc Emerg Med. 2013;21:79–84. doi: 10.1186/1757-7241-21-79. doi: 10.1186/1757-7241-21-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–30. doi: 10.1093/bja/aen231. doi: 10.1093/bja/aen231. [DOI] [PubMed] [Google Scholar]
- 12.Kok T, George RB, McKeen D, Vakharia N, Pink A. Effectiveness and safety of the Levitan FPS Scope™ for tracheal intubation under general anesthesia with a simulated difficult airway. Can J Anaesth. 2012;59:743–50. doi: 10.1007/s12630-012-9726-4. doi: 10.1007/s12630-012-9726-4. [DOI] [PubMed] [Google Scholar]
- 13.Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance. Anesthesiology. 2005;103:429–37. doi: 10.1097/00000542-200508000-00027. doi: 10.1097/00000542-200508000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Agrò F, Cataldo R, Carassiti M, Costa F. The seeing stylet: A new device for tracheal intubation. Resuscitation. 2000;44:177–80. doi: 10.1016/s0300-9572(00)00137-4. doi: 10.1016/S0300-9572(00)00137-4. [DOI] [PubMed] [Google Scholar]
- 15.Phua DS, Mah CL, Wang CF. The Shikani optical stylet as an alternative to the GlideScope® videolaryngoscope in simulated difficult intubations – A randomised controlled trial. Anaesthesia. 2012;67:402–6. doi: 10.1111/j.1365-2044.2011.07023.x. doi: 10.1111/j.1365-2044.2011.07023.x. [DOI] [PubMed] [Google Scholar]
- 16.Dhonneur G, Abdi W, Ndoko SK, Amathieu R, Risk N, El Housseini L, et al. Video-assisted versus conventional tracheal intubation in morbidly obese patients. Obes Surg. 2009;19:1096–101. doi: 10.1007/s11695-008-9719-0. doi: 10.1007/s11695-008-9719-0. [DOI] [PubMed] [Google Scholar]
- 17.Maharaj CH, Costello JF, Harte BH, Laffey JG. Evaluation of the Airtraq and Macintosh laryngoscopes in patients at increased risk for difficult tracheal intubation. Anaesthesia. 2008;63:182–8. doi: 10.1111/j.1365-2044.2007.05316.x. doi: 10.1111/j.1365-2044.2007.05316.x. [DOI] [PubMed] [Google Scholar]