Abstract
Intimate partner violence (IPV) is a significant global health issue and has been associated with an increased HIV-related risk and vulnerability to HIV-infection. This study examined the potential relationship between IPV and HIV-risk behaviors among women in Nepal. Our findings revealed that IPV against women was associated with the presence of HIV risk behaviors, such as – history of STIs, multiple sex partners, inconsistent condom-use, partner with known HIV-risks, and inability to negotiate safer sexual practices. This highlights a need to develop effective interventions aimed at eliminating IPV to decrease the disproportionate burden of adverse health outcomes including STIs/HIV among women.
Keywords: Intimate partner violence, sexual risk behavior, HIV prevention
INTRODUCTION
Today, over half of the 35 million people living with HIV/AIDS globally are women. Possibly most alarming of all, young women (15-24 years) in sub-Saharan Africa account for 75% of HIV infections and are roughly 3 times more likely to be infected with HIV than their male counterparts (WHO, 2013). Women’s disproportionate vulnerability to the HIV/AIDS pandemic has been attributed to the underlying consequences of gender inequalities and harmful gender norms that promote HIV-related risk behaviors and reduce access to health services, which is often manifested in violence against women (VAW) (Wang, 2010). VAW is well recognized as a gross violation of human rights, with 1 in 3 women worldwide having experienced either physical and/or sexual intimate partner violence (IPV) or non-partner violence (WHO, 2013). While VAW encompasses many other forms of violence to which women may be exposed, this study focuses on two forms of VAW: physical and sexual IPVs and their association with HIV risk behaviors.
Intimate Partner Violence and HIV
Intimate partner violence, which represents a significant public health problem, disproportionately affects women in the hands of their male partner. Over the past decade, there has been growing recognition that IPV is an important contributor to women’s vulnerability to HIV (Campbell, Lucea, Stockman, & Draughon, 2013; Jewkes, Dunkle, Nduna, & Shai, 2010; Laanpere, Ringmets, Part, & Karro, 2013). Studies have shown elevated sexual risk behaviors (i.e., inconsistent condom use, forced unprotected sex, extramarital and multiple sex partners) among abused women, and their partners that place them at increased risk of contracting HIV (Seth, Raiford, Robinson, Wingood, & Diclemente, 2010; Silverman et al., 2011). For example, studies conducted in the United States and South Asia have found elevated rates of HIV/AIDS infections among women attributed to relationships involving IPV (Sareen, Pagura, & Grant, 2009; Silverman et al., 2011), which underscores the interrelation between IPV and HIV/AIDS.
Behavioral evidence has shown that abusive men exhibit a number of HIV-risk behaviors, including having multiple sexual partners, frequent alcohol use, visiting sex workers, and having an STI (Raj et al., 2013; Townsend et al., 2011). Thus, the likelihood of HIV transmission from infected men to women increases through the heightened possibility of physical injury (i.e., tearing or laceration) during forced or non-consensual sexual acts perpetrated by a male partner (Campbell et al., 2013; Silverman et al., 2007; Stockman, Lucea, & Campbell, 2013). In addition, women who are abused or live in fear of violence, may also have limited control over the timing of sex or circumstances under which it takes place, or their capacity to refuse sex or negotiate condom use, thus facilitating HIV transmission in the presence of an infected male partner (Mittal, Senn, & Carey, 2013; Sales et al., 2008). For example, several studies have linked IPV to fear of asking intimate partners to use condoms (Mittal et al., 2013; Sales et al., 2008)and to inconsistent condom use(Mittal et al., 2013; Silverman et al., 2011). Furthermore, IPV may also be an important determinant of social isolation or separation, which in turn may increase a woman’s possibility of engaging in risky sexual behaviors such as having multiple sexual partners, sex with a drug-injecting partner, and trading money or drugs for sex (Hess et al., 2012; Seth et al., 2010; Silverman et al., 2011).
HIV in Nepal is characterized as a concentrated epidemic with an adult (ages 15-49) HIV prevalence of 0.3% in 2011. According to recent estimates, there are approximately 50,000 people living with HIV and of which 33.5% of infections are in women (National Center for AIDS and STD Control, 2012). This relatively high rates of HIV infection among women highlights underlying persistent gender inequalities, notably violence against women. Nepal’s deeply rooted patriarchal structure and its resultant attitude, ignorance and unorthodox norms, illiteracy, unemployment, early marriage have made violence against women such as unescapable issue that it exists across all strata of Nepali society. A recent country-based survey conducted in 2011 indicated that, among women age 15-49, 22% had experienced physical violence and 12% had experienced sexual violence at some point in their lifetime. Among married women, one-third had experienced emotional, physical, or sexual violence from their spouse in their marital relationship, and 17% had experienced it within the last 12 months (Ministry of Health and Population, New ERA, & ICF International Inc., 2012). Although violence against women has been in existence and widespread in Nepali society, it continues to be an underreported, common problem that, if ignored, increases risks for HIV and may prevent women and girls from seeking prevention, treatment, and health services.
As a growing body of evidence has highlighted the behavioral sequelae of IPV resulting in increased HIV risk factors in both developed and developing countries, such studies have not yet been conducted in Nepal. Very few studies in Nepal have documented the potential association of IPV with various health outcomes, such as maternal service utilization, complete child immunization, anemia among children, various physical, mental and reproductive health problems, and sexually transmitted infections (STIs) in abused women in various settings (Dhakal, Berg-Beckhoff, & Aro, 2014; Joshi, Malla, Aryal, & Indur, 2012; Tuladhar, Khanal, K.C., Ghimire, & Onta, 2013). For example, a recent study by Tuladhar and colleagues (2013) reported an association between IPV and childhood anemia in Nepal. Similarly, Dhakal and colleagues (2014) reported that the abused women were 1.88 times more likely to have STIs as compared to women not exposed to any form of IPV.
Given the high prevalence of IPV in Nepal and its impact on women’s health, the aim of the present study was to extend prior findings from studies in Nepal and elsewhere by estimating: 1) the prevalence of physical and sexual IPV among married women, 2) the risk factors for IPV, and 3) the potential association between these types of violence and HIV risk behaviors. In the context of nonexistence of country-specific evidence about the relationship of IPV and HIV risk factors, the present study will give insight on how IPV affects the sexual health of Nepalese women. This research is important because advances in HIV prevention require an understanding of factors influencing women’s increased vulnerability to HIV infection, particularly among women who experience abuse from their intimate partners. The use of population-based data from the nationally representative 2011 Nepal Demographic Health Survey (NDHS-2011) offers empirical strength to the current study to assess IPV and HIV risk behaviors while maximizing inferences to the general population (Ministry of Health and Population et al., 2012).
METHODS
Design, Setting and Sample
The NDHS-2011, which is a part of the worldwide DHS project in Nepal, was conducted under the leadership of the Nepal Ministry of Health and Population (MoHP) from February 2 to June 14, 2011. The survey used a two stage stratified cluster-sampling technique. For the purpose of sampling, Nepal was divided into 25 strata. In each stratum, enumeration areas (EAs; wards in the village development committees and sub-wards in the municipalities) were selected using a probability-proportional-to-size strategy. Each household in all selected EAs was listed and mapped. Then, 35 households in each urban EA and 40 households in each rural EA were randomly selected (Ministry of Health and Population et al., 2012). This procedure resulted in identifying 12,918 eligible women (15-49), of which 12,674 completed the survey, and 4,323 eligible men (15-54), of which 4,121 completed the survey. Trained research assistants conducted household-based recruitment and obtained informed consent immediately prior to data collection. The survey was approved by the Nepal Health Research Council, Nepal and the Institutional Review Board of IFC Macro in Maryland, USA (Ministry of Health and Population et al., 2012). Permission for using the data for this study was authorized by ICF International, which coordinates the DHS.
The survey included three questionnaires – the Household Questionnaire, the Woman’s Questionnaire, and the Man’s Questionnaire. The Household Questionnaire was used to identify women eligible for the individual interview, which included questionnaires on domestic violence and awareness and behavior regarding AIDS and other STIs. Only one woman per household was administered the domestic violence module (DVM) - the set of questions to measure spousal violence - to maintain confidentiality. One in every two households was preselected for an interview on violence, and in the selected household one female respondent was randomly selected to receive the questions on domestic violence. The assessment was administered only when privacy could be ensured (Ministry of Health and Population et al., 2012). This resulted in a total of 4,210 women being eligible for the DVM module, of whom 13 eligible women were not interviewed due to lack of privacy, thus leaving 4,197 to successfully complete the interview.
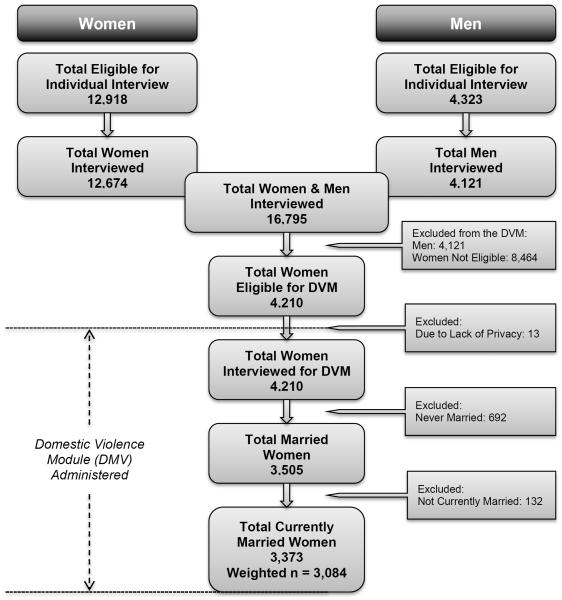
For the purpose of this study, the analytic sample was restricted to “currently married women” because the study focused on spousal violence committed by husbands. This comprised a total of 3,084 currently married women (15-49). Figure 1 shows the schematic representation of sampling plan for this study.
Figure 1.
Schematic representation of sampling plan for the study
Measures
Basic socio-demographic variables including age, religion, place of residence (urban/rural), ecological region, educational status, and employment status (whether respondents are currently working) of the participants were assessed via single self-reported items on the survey. The educational and employment status of the participants were assessed using the questionnaires that included “What is the highest grade you completed?” and “Have you done any work in the last 12 months?” A wealth index of household was calculated based on interviewer-observed household assets (taking into account of urban-rural differences); the resulting score was then divided into quintiles. Husband’s total number of other wives was assessed by the question “Including yourself, in total, how many wives or live-in partners does your husband have?” Questions, including “Have you heard about infections that can be transmitted through sexual contact?”, “During the last 12 months, have you had a disease which you got through sexual contact or had a bad-smelling abnormal genital discharge or had a genital sore/ulcer?”, “Have you ever heard of AIDS?”, were asked to assess participants’ knowledge related to sexually transmitted infections (STIs), including HIV/AIDS. Information for the purpose of measuring risk behaviors was measured with a series of questions on HIV-related risk behaviors. Sample items include: “What is the total number sexual partner you had in your lifetime?”, “Was a condom used every time you had sexual intercourse in the last 12 months?”, “The last time you had sexual intercourse, was a condom used?”, “Can you say no to your partner if you do not want to have sex?”, “Could you ask your partner to use a condom if you wanted him to?”. The husband’s HIV risk behavior was assessed by combining two questionnaires that included: “What was your relationship with whom you had sexual intercourse?” and “Did you use a condom when you had sexual intercourse with this person?”
The physical and sexual IPVs were assessed via self-report questionnaires adapted “shortened and modified version of the Conflict Tactics Scale“ (Straus, Hamby, Boney-Mccoy, & Sugarman, 1996). To assess the status of physical IPV, women were asked following 7 items, “push you, shake you, or throw something at you”, “slap you”, “twist your arm or pull your hair”, “punch you with a fist or something harmful”, “kick, drag or beat you up”, “try to choke or burn you on purpose”, and “threaten or attack you with a knife, gun, or any other weapon.” Similarly, sexual IPV was measured by the following 2 items, “physically force you to have sexual intercourse with him even when you did not want to” or “force you to perform any sexual acts that you did not want to”. Lifetime and recent (i.e., in the last 12 months) physical and sexual IPV was indicated by a positive answer to any of the above items pertaining to occurrences at the hands of their husband.
Analysis
The prevalence estimates of physical and/or sexual IPVs were calculated for the overall sample based on respondents’ self-reports of the husband’s behavior. Univariate analysis was carried out to understand the frequency distribution. A multivariable logistic regression model was first constructed to estimate the odds ratio (OR) and 95% confidence interval (CI) for the association of demographic variables and IPV (physical and sexual IPVs). Subsequently, we constructed multivariable regression models to assess the associations between IPV (physical and sexual IPVs) and HIV risk behaviors. After determining the crude (i.e., unadjusted) relations, models were adjusted for major demographic variables (i.e., age, respondent’s educational status, husband’s educational status, employment status, cohabitation duration, and husband drinking behavior), the selection of which was guided by theoretical considerations and prior studies. Although the nature of the relationships between IPV and HIV risk most likely is bidirectional, we theorized IPV as the predictor variable and the HIV risk as the outcome variable for the purposes of this study. Estimates generated via logistic regression were evaluated for statistical significance based on 95% CIs with p < .5. All analyses were conducted in SPSS software, version 20.0. All of our analyses were weighted using the sample weight for the entire women’s sample standardized to the current analytic sample size to account for selection probability and the complex sampling design of the NDHS survey.
RESULTS
Sociodemographic characteristics
The sociodemographic characteristics of the study sample are presented in Table 1. The mean age of the 3,084 women assessed was 31.1 years (SD = 8.9 years), with the majority identified as Hindu (85%). Over three-fourth of the participants were from rural areas (75.8%), and almost half from the Hill region (47%). Overall, 52% of women and 79.4% of their husbands were educated. In terms of household economic status, all of the women studied were fairly evenly distributed across the wealth quintiles, and 78.8% of women and 98.3% of husband were engaged in some type of income-generating activity. The vast majority of the women indicated that the duration of their relationship with their current primary partner was at least 5 years (79.1%). The proportion of married men who have more than one wife was found to be relatively low (3.8%). Nearly half of the total women reported that their husband do not drink alcohol (48.1%), but 7% and 28.2% of them reported that their husband “often” or “sometimes” gets drunk, respectively.
Table 1.
Sociodemographic Characteristics of The Participants (N = 3084)
| Variables | n | % |
|---|---|---|
| Age (years) | ||
| Mean | 31.1 | |
| SD | 8.9 | |
| Religion | ||
| Hindu | 2643 | 85.7 |
| Buddhist | 259 | 8.4 |
| Muslim | 94 | 3.1 |
| Kirat | 36 | 1.2 |
| Christian | 52 | 1.7 |
| Place of residence | ||
| Urban | 747 | 24.2 |
| Rural | 2338 | 75.8 |
| Ecological region | ||
| Mountain | 319 | 10.3 |
| Hill | 1449 | 47.0 |
| Terai | 1316 | 42.7 |
| Educational status | ||
| No education | 1481 | 48.0 |
| Primary | 564 | 18.3 |
| Secondary | 833 | 27.3 |
| Higher | 207 | 6.7 |
| Employed | 2431 | 78.8 |
| Husband’s educational status |
617 | 20.0 |
| No education | 693 | 22.5 |
| Primary | 1320 | 42.8 |
| Secondary | 438 | 14.2 |
| Higher | 17 | 0.6 |
| Don’t know | ||
| Husband employed | 3032 | 98.3 |
| Wealth index | ||
| Poorest | 638 | 20.7 |
| Poorer | 538 | 17.4 |
| Middle | 592 | 19.2 |
| Richer | 646 | 21.0 |
| Richest | 670 | 21.7 |
| Cohabitation duration (years) |
644 | 20.9 |
| 0 – 4 | 605 | 19.6 |
| 5 – 9 | 504 | 16.3 |
| 10 – 14 | 454 | 14.7 |
| 15 – 19 | 391 | 12.7 |
| 20 – 24 | 501 | 15.7 |
| 25 + | ||
| Number of husband’s other wives |
2967 | 96.2 |
| 0 | 115 | 3.8 |
| 1 + | 3 | 0.1 |
| Don’t know | ||
| Husband ever drunk | ||
| Don’t drink alcohol | 1484 | 48.1 |
| Never | 515 | 16.7 |
| Often | 214 | 7.0 |
| Sometimes | 871 | 28.2 |
Intimate Partner Violence (IPV)
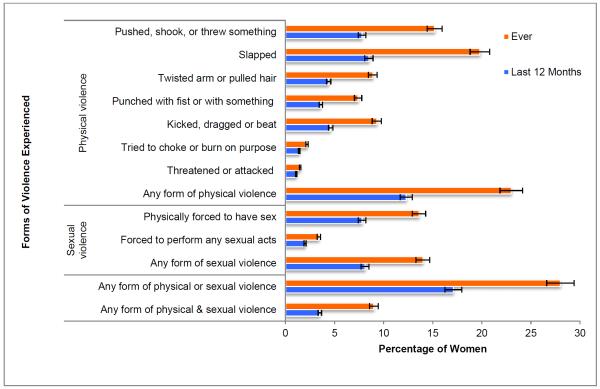
Nearly one in four (23%) of currently married women reported ever experiencing physical violence and that 12.3% experienced physical violence within the preceding 12 months. Over two percent of women reported that they had experienced physical violence often in the past 12 months (2.3%), and 10.1% said they had experienced physical violence sometimes during the past 12 months. Nearly one in six women (14%) reported ever experiencing sexual violence from their husband, and 1.3% of women indicated that such violence occurred often within the last 12 months and 6.8% reported to have experience that sexual violence occurred sometimes in the preceding 12 months. Overall, more than 1 in 4 women reported experiencing physical or sexual violence (28%) from their husband, while 9% of them have experienced both physical and sexual violence in their lifetime (Figure 2).
Figure 2.
Forms of Violence Experienced by The Participants (N = 3084)
The most common form of physical violence experienced by ever-married women was being slapped (19.8%). Over fifteen percent of ever-married women reported having been pushed, shaken, or had something thrown at them (15.2%); 9.3% reported being kicked, dragged, or beaten, and 8.9% reported having their arm twisted or hair pulled. Similarly, 13.6% reported being physically forced to have sexual intercourse and 3.4% reported being forced to perform some kind of sexual act by their husbands (Figure 1).
HIV Related Knowledge and Risk Behavior
Table 2 shows that 88.4% of women reported hearing about sexually transmitted infections (STIs). The prevalence of self-reported STIs among this sample was 14.7%. The majority of the participants reported knowing about AIDS (86.2%). A small proportion of women reported having multiple sex partners (4.3%) prior to the survey. Of the women who had ever had sexual intercourse, about 2 in 3 reported using a condom during every instance of penetrative sex with their primary partners in the past 12 months (64.6%), only 1 in every 15 women reported using a condom during their last sexual intercourse, and 6.6% of women reported having a partner who engaged in HIV risk behaviors (i.e., engaged in extra-marital sexual relationship and inconsistent condom use). Over ninety percent of women reported feeling able to refuse to have sexual intercourse if she did not want to (94.1%), and 74.5% felt that they could negotiate condom use with their partner.
Table 2.
HIV Related Knowledge, Risk Factors and Attitude Towards Safe Sex Among The Participants (N = 3084)
| Variables | n | % |
|---|---|---|
| Ever heard of STI | ||
| No | 359 | 11.6 |
| Yes | 2725 | 88.4 |
| History of STI a | ||
| No | 2632 | 85.3 |
| Yes | 452 | 14.7 |
| Ever heard of AIDS | ||
| No | 426 | 13.8 |
| Yes | 2659 | 86.2 |
| Had multiple sex partners | N = 3078 | |
| No | 2945 | 95.7 |
| Yes | 134 | 4.3 |
| Used condom every time in the last 12 months | N = 181 | |
| No | 64 | 35.4 |
| Yes | 117 | 64.6 |
| Used condom during last sex | N = 2739 | |
| No | 2558 | 93.4 |
| Yes | 181 | 6.6 |
| Husband’s with known HIV risk behavior b | N = 2738 | |
| No | 2558 | 93.4 |
| Yes | 180 | 6.6 |
| Respondent can refuse sex | ||
| No | 169 | 5.5 |
| Yes | 2904 | 94.1 |
| Don’t know | 12 | 0.4 |
| Respondent can ask partner to use condom | ||
| No | 747 | 24.2 |
| Yes | 2298 | 74.5 |
| Don’t know | 40 | 1.3 |
Includes bad smelling genital discharge, genital sore/ulcer
Includes extra-marital sex and inconsistent condom use
Relationship Between Sociodemographic Characteristics and Intimate Partner Violence
On a logistic regression model in which IPV was used as the dependent variable, lower education of women and their husband, lower wealth index, and husband’s drinking habits were associated with higher risk of physical IPV. Women with no formal education were 7.07 times more likely than women with high school or higher level of education to report physical IPV. Similarly, women whose husband had no formal education were 3.40 times more likely to report physical IPV compared to their counterparts whose husband had high school or higher level of education. Compared to women in the highest level of economic status (i.e., richest wealth index), women belonging to the lower economic status (i.e. richer and middle wealth index) were 1.64 and 1.60 times more likely to experience physical IPV, respectively. Women who reported that their husband never got drunk were 1.75 less likely and women who reported that their husband often got drunk were 4.50 more likely, respectively, to experience physical IPV as compared to women whose husband sometimes got drunk (Table 3).
Table 3.
Relationship Between Sociodemographic Characteristics and Intimate Partner Violence (IPV), Listed with Odds Ratios (ORs) and 95% Confidence Intervals (CIs)
| Sociodemographic Variables | Physical Violence |
Sexual Violence |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.97 | 0.93-1.00 | 0.059 | 0.97 | 0.93-1.01 | 0.146 |
| Place of residence (Urban) | 1.09 | 0.80-1.49 | 0.577 | 0.94 | 0.66-1.35 | 0.729 |
| Educational status | ||||||
| No formal education | 7.07 | 1.51-33.06 | 0.013 | 2.09 | 0.60-7.30 | 0.247 |
| Primary | 6.38 | 1.37-29.81 | 0.019 | 1.85 | 0.53-6.48 | 0.334 |
| Secondary | 6.32 | 1.38-28.89 | 0.017 | 2.81 | 0.85-9.34 | 0.092 |
| Higher | - | - | - | - | - | - |
| Unemployed | 1.10 | 0.83-1.46 | 0.505 | 0.78 | 0.56-1.09 | 0.145 |
| Husband’s educational status | ||||||
| No formal education | 3.40 | 1.76-6.57 | <0.001 | 4.21 | 1.97-9.04 | <0.001 |
| Primary | 2.41 | 1.27-4.60 | 0.007 | 2.50 | 1.18-5.28 | 0.016 |
| Secondary | 1.99 | 1.08-3.66 | 0.027 | 1.91 | 0.95-3.84 | 0.071 |
| Higher | - | - | - | - | - | - |
| Educational disparity | 1.14 | 0.97-1.35 | 0.122 | 1.23 | 1.01-1.51 | 0.043 |
| Wealth index | ||||||
| Poorest | 0.90 | 0.56-1.44 | 0.649 | 0.47 | 0.28-0.80 | 0.005 |
| Poorer | 1.26 | 0.79-2.02 | 0.335 | 0.72 | 0.43-1.22 | 0.224 |
| Middle | 1.60 | 1.02-2.49 | 0.039 | 0.72 | 0.43-1.18 | 0.196 |
| Richer | 1.64 | 1.07-2.52 | 0.022 | 0.87 | 0.54-1.39 | 0.554 |
| Richest | - | - | - | - | - | - |
| Cohabitation duration (years) | ||||||
| 0 – 4 | 0.38 | 0.14-1.04 | 0.059 | 0.72 | 0.22-2.29 | 0.573 |
| 5 – 9 | 0.73 | 0.31-1.69 | 0.460 | 0.94 | 0.35-2.53 | 0.898 |
| 10 – 14 | 1.18 | 0.59-2.36 | 0.637 | 1.05 | 0.46-2.39 | 0.906 |
| 15 – 19 | 0.99 | 0.57-1.72 | 0.961 | 1.35 | 0.71-2.60 | 0.363 |
| 20 – 24 | 1.19 | 0.75-1.89 | 0.485 | 1.15 | 0.66-1.98 | 0.626 |
| 25 + | - | - | - | - | - | - |
| Husband with single wife | 0.75 | 0.44-1.27 | 0.276 | 1.19 | 0.62-2.30 | 0.604 |
| Husband ever drunk | ||||||
| Never | 0.57 | 0.43-0.76 | <0.001 | 0.56 | 0.40-0.80 | 0.001 |
| Often | 4.50 | 3.22-6.30 | <0.001 | 3.20 | 2.26-4.52 | <0.001 |
| Sometimes | - | - | - | - | - | - |
In terms of sexual violence, husband’s lower educational status, higher wealth index, and husband’s drinking habits were associated with increased risk of sexual IPV. Women who reported that their husband had not received formal education were 4.21 times more likely to experience sexual IPV than those women who reported that their husband had at least been to high school. Similarly, women with differential educational status from their husband were 1.23 times more likely to experience sexual IPV than those women who had similar educational attainment to their husband. Women belonging to the “poorest” wealth quintile were 2.13 times less likely to experience sexual IPV as compared to women belonging to “richest” wealth quintile. Women who reported that their husband never got drunk were 1.79 times less likely and women who reported that their husband often got drunk were 3.20 times more likely, respectively, to experience sexual IPV as compared to women who reported that their husband sometimes got drunk (Table 3).
Relationship Between Intimate Partner Violence and HIV Related Knowledge and Risk factors
The logistic regression models presented in Table 4 show that after adjustment for sociodemographic variables – including age, respondent’s educational status, husband’s educational status, employment status, cohabitation duration, and husband drinking behavior – the relationships between IPV and HIV risk factors remained significant. In our sample, women who experienced physical violence from their husband were 2.27 times less likely to have heard about STIs, 2.38 times less likely to have heard about AIDS, and 1.68 times more likely to have a history of STIs compared to women who reported no physical violence. Among participants who reported being engaged in sexual intercourse with their partners in the past 12 months, women who reported experiencing any physical violence from their husbands were 2.89 times more likely to report having multiple sex partners, and 2.44 times less likely to report using a condom during their last sexual intercourse as compared to women who reported not experiencing any physical violence. Women who reported being physically abused were 1.96 times less likely to report being able to negotiate condom use with their partner during sexual intercourse compared to those who did not report physical violence.
Table 4.
Relationship Between Intimate Partner Violence (IPV) and HIV risk factors, Listed with Odds Ratios (ORs) and 95% Confidence Intervals (CIs)
| HIV Risk Variables | Physical Violence |
Sexual Violence |
||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | Adjusted OR a |
95% CI |
OR | 95% CI | Adjusted OR a |
95% CI |
|
| Ever heard of STI | 0.44* | 0.34-0.57 | 0.66* | 0.50-0.86 | 1.03 | 0.75-1.41 | 1.06 | 0.76-1.49 |
| History of STI | 1.68* | 1.33-2.14 | 1.74* | 1.37-2.22 | 1.51* | 1.14-1.99 | 1.52* | 1.15-2.00 |
| Ever heard of AIDS | 0.42* | 0.34-0.54 | 0.63* | 0.49-0.81 | 0.91 | 0.68-1.21 | 0.92 | 0.67-1.25 |
| Had multiple sex partnerb,c | 2.89* | 1.97-4.27 | 2.31* | 1.56-3.43 | 1.47 | 0.95-2.28 | 1.41 | 0.90-2.19 |
| Used condom during last sex d | 0.41* | 0.25-0.68 | 0.53* | 0.35-0.97 | 1.07 | 0.64-1.79 | 1.16 | 0.68-1.99 |
| Husband with known HIV risk | 2.49* | 1.50-4.11 | 1.75* | 1.04-2.94 | 0.95 | 0.57-1.60 | 0.87 | 0.51-1.50 |
| Can refuse sex | 1.10 | 0.75-1.64 | 1.45 | 0.97-2.15 | 0.38* | 0.25-0.56 | 0.39* | 0.26-0.59 |
| Can ask partner to use condom | 0.51* | 0.42-0.62 | 0.69* | 0.56-0.85 | 0.61* | 0.48-0.78 | 0.61* | 0.47-0.78 |
Adjusted for age, respondent’s educational status, husband’s educational status, employment status, cohabitation duration, and husband’s drinking behavior.
Husband excluded
Only women who reported the number of their partners were included.
Only women who reported having sexual intercourse in the last 12 months were included.
Statistically significant (p < 0.05)
We also restricted analyses so as to compare only women who reported sexual violence by their husband versus women who reported no instances of sexual IPV, and found that three HIV risk behaviors were significantly associated with sexual IPV. Compared to women reporting no sexual IPV within their primary relationships, women who reported sexual IPV were 1.52 times more likely to report a history of STIs in the past 12 months. In addition, compared to women who reported no sexual IPV, women who reported sexual IPV from their husband were 2.56 times less likely to report feeling able to refuse having sex when they did not want to and 1.64 times less likely to report feeling able to negotiate condom use with their partner during sexual intercourse (Table 4).
DISCUSSION
The current study was designed to assess the prevalence of physical and/or sexual IPV among currently married women (15-49 years) using a nationally representative sample. The prevalence of IPV against women in the current study was somewhat similar to what was found among women in other countries, including Nepal (Dhakal et al., 2014; Ministry of Health and Population et al., 2012; WHO, 2013). Among our study sample, nearly one in four women reported experiencing physical violence and one in six women reported sexual violence at some point in their current relationships. This is comparable to a national estimate by the NDHS-2011, which revealed that 22% and 12% of women age 15-49 reported experiencing physical and sexual violence, respectively, from their spouse (Ministry of Health and Population et al., 2012; Tuladhar et al., 2013). Likewise, the WHO estimate of the global prevalence of intimate partner violence, including physical and/or sexual IPV, among all ever-partnered women was 30% (WHO, 2013).
Our analysis replicates prior research showing that completing higher education tends to have a protective effect on IPV risk, such that – compared to women with higher education, women with secondary level education had a six-fold increase and almost three-fold increase in the frequency of physical and sexual IPV, respectively (Abramsky et al., 2011; Tumwesigye, Kyomuhendo, Greenfield, & Wanyenze, 2012). This suggests that educated women may be less likely to accept traditional gender roles and could be more vocal in their response to violence by their husbands. However, studies conducted elsewhere have presented conflicting results, with some studies showing higher education to be protective (Abramsky et al., 2011; Tumwesigye et al., 2012) while others tend to show higher education as a risk factor (Deyessa et al., 2010; Lamichhane, Puri, Tamang, & Dulal, 2011; Martin, Taft, & Resick, 2007). Furthermore, disparity in educational attainment between women and their husband was significantly associated with an increased risk of sexual IPV among women, which is consistent with the findings of Abramsky and colleagues, and thus highlights the importance of equal educational opportunity for both boys and girls (Abramsky et al., 2011).
Interestingly, in our sample of currently married women, the decreasing gradient of economic status (i.e., from richest to poorest) was associated with lower likelihood of experiencing physical IPV. This finding contradicts previous results, which have found an inverse relationship between economic status and IPV (i.e., higher economic status was generally associated with lower levels of IPV) (Abramsky et al., 2011; Vyas & Watts, 2009). This apparent conflict may be explained by the suggestion that the relationship between economic status and IPV could be curvilinear (i.e., an increase in economic status corresponds to an increase in IPV). It may also be that the relationship between economic status and IPV could be a function of culture and it is possible that same association may not be the same across cultures or contexts.
Corroborating previous findings, problematic alcohol use among husband was found to be strongly associated with IPV: women who reported their husband to have been drunk “often” were more likely to report IPV as compared to those who reported their husband to have been drunk “once in a while” (Abramsky et al., 2011; Kiss et al., 2012). Evidence from various countries, including Nepal, has shown that the episode and severity of IPV against women increases due to alcohol use among male partners (Abramsky et al., 2011; Joshi et al., 2012; Kiss et al., 2012; Oshiro, Poudyal, Poudel, Jimba, & Hokama, 2011; Puri, Frost, Tamang, Lamichhane, & Shah, 2012; WHO, 2010). A study by Oshiro and colleagues among ever-married women between the ages of 15 and 49 years in Kathmandu, the capital city of Nepal, showed a strong association between the husband’s drinking and intimate partner violence (Oshiro et al., 2011). Similarly, a similar study by Puri et al. among married women in four districts (Dolakha, Sindhupalchowk, Dang, and Kapilvastu) reported that alcohol use by the husband plays a significant precipitating role in sexual violence (Puri et al., 2012). Furthermore, a study by O’Leary and Schumacher in the United States suggested that the effects of alcohol consumption present a threshold effect – only higher or problematic levels of alcohol use among men is associated with a higher odds of perpetrating IPV against their partners (O'Leary & Schumacher, 2003). While it is difficult to establish the temporality of the observed associations, this relationship is critical and requires proper attention while designing and targeting IPV intervention programs.
The current study also looked at the association between two epidemics threatening the health and safety of women in Nepal and around the world (i.e., IPV and HIV risk behaviors). Women who experienced any form of IPV (i.e., physical and/or sexual) had significantly higher risk of incident of STIs compared to those who did not report any form of IPV. This confirms findings of previous studies reporting that women with a history of abuse have a higher incidence of STIs than women are not abused (Dhakal et al., 2014; Kishor, 2012; Seth et al., 2010). While the nature of the data prevents us from establishing any chronological sequence between abuse and infection, our findings suggest that the relationship between IPV and STI diagnoses may likely have been mediated through sexually coercive behaviors of the abusive male partner.
The current study also revealed that physical violence, but not sexual violence, was associated with an almost three-fold increased likelihood of having multiple sex partners and over two-fold reduced likelihood to have used condom in the last sexual intercourse. These findings are consistent with those of a growing body of literature that suggests women who experience IPV are with having sex with multiple partners, including those who are HIV-positive, injection drug users, and non-monogamous, and having unprotected sex(Hess et al., 2012; Seth et al., 2010; Silverman et al., 2011). However, there are some studies which have found no or negative relationships between IPV and unprotected sex (Teitelman, Ratcliffe, Dichter, & Sullivan, 2008; Tucker, Wenzel, Elliott, Marshall, & Williamson, 2004). These variations may be attributable to discrepancies in methodological approach across studies, and to assessment of sexual partner of women (i.e., primary vs. non-primary), and condom use practice (i.e., frequency of condom use vs. condom use during last sex).
Self-reported information by our sample regarding their partner’s behavior within their relationship suggests that abused women report more high-risk behaviors among their partners than non-abused women. For example, women who had experienced physical abuse from their husband at some point in their life were two-fold more likely to have a partner who engaged in HIV risk behaviors (i.e., engaged in extra-marital sexual relationship and inconsistent condom use). This is consistent with findings from earlier studies that have found that male perpetrators of IPV engage in behavior that puts their partners at greater risk for HIV infection and transmission (Hembling & Andrinopoulos, 2014; Townsend et al., 2011). These findings suggest that those women who are aware of their partners’ risk behaviors may increase their risk of IPV while trying to negotiate safer sexual practices.
Previous studies have also linked IPV to fear among women, eventually leading to increased communication gap between partners regarding safer sexual practices including consensual sex, monogamy, and condom use negotiation (Mittal et al., 2013; Sales et al., 2008). Consistent with these findings, our sample of married women who were sexually abused by their husband were 2.56 times less likely to refuse sex when they did not want to and 1.64 times less likely to ask their partner to use condom during sexual intercourse compared to women who were not sexually abused. These results suggest that women who insist that their husband practice safer sex (i.e., using condom) may be seen as accusing their partner of infidelity, or may be subject to an even greater degree of IPV.
While this study advances the current state of knowledge on IPV and its association with HIV risk behaviors, it must be considered in light of few study limitations. These include the cross-sectional nature of the study, which limits our ability to establish a temporal relationship. While the analyses were based on a conceptual framework positing that husbands are more likely to perpetrate IPV within the relationship, we cannot rule out the possibility that wives can also be perpetrators of violence against their husbands. A further limitation is that the study relied on the self-report assessment approach, which may have constrained our ability to precisely measure some variables of interest (i.e., IPV, STIs, and sexual risk behaviors) due to participants’ reluctance to report these stigmatized and sensitive issues. In addition, the IPV assessment was dichotomized for ease of interpretation; further investigation is needed to evaluate the extent to which patterns identified may vary across severity levels.
CONCLUSION
To our knowledge, this is the first study to look at the association between IPV and HIV risk behaviors among women in Nepal. The findings from this population-based study contribute to mounting evidence that the experience of being physically and/or sexually abused by a male intimate partner is associated with a greater likelihood of HIV infection due to presence of sexual risk behaviors among themselves and their partners (Abramsky et al., 2011; Campbell et al., 2013; Mittal et al., 2013). Given the circumstance that over one in four women are physically or sexually abused at the hands of their husbands, both in the current sample and worldwide (WHO, 2013), there is a clear need to develop effective interventions aimed at eliminating IPV to decrease the disproportionate burden of adverse health outcomes including STIs/HIV among women.
Acknowledgements
Authors would like to acknowledge the MEASURE DHS Data Archive, ICF International for providing us with the datasets for further analysis.
Funding
Funding to support the preparation of the article was provided by a National Institute of Health (NIH) Grant (K02DA033139) to Michael M. Copenhaver.
Author Biographies
Roman Shrestha is a Doctoral student in the Department of Community Medicine and Health Care at the University of Connecticut Health Center. His research interests include HIV/AIDS and sexually transmitted diseases, health care disparities, and program evaluation. His current research involves developing an evidence-based intervention targeting high-risk returnee migrant workers in Nepal. He also works as a research assistant for the ‘Secondary HIV prevention and adherence among HIV-infected drug users’ project under the direction of Dr. Michael Copenhaver.
Michael Copenhaver is an associate professor of Health Promotion in the Department of Allied Health Sciences and the Department of Psychology, a PI at the Center for Health, Intervention, and Prevention (CHIP), and a licensed clinical psychologist. His current research involves adapting and evaluating evidence-based behavioral interventions for optimal use in clinical settings (drug treatment, prison) where high risk drug users may be more effectively reached.
Footnotes
Authors’ Note
Points of view in this document are those of the authors. NIH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
REFERENCES
- Abramsky T, Watts CH, Garcia-Moreno C, Devries K, Kiss L, Ellsberg M, Heise L. What factors are associated with recent intimate partner violence? Findings from the WHO multi-country study on women's health and domestic violence. BMC Public Health. 2011;11:109-2458–11-109. doi: 10.1186/1471-2458-11-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC, Lucea MB, Stockman JK, Draughon JE. Forced sex and HIV risk in violent relationships. American Journal of Reproductive Immunology (New York, N.Y.: 1989) 2013;69(Suppl 1):41–44. doi: 10.1111/aji.12026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyessa N, Berhane Y, Ellsberg M, Emmelin M, Kullgren G, Hogberg U. Violence against women in relation to literacy and area of residence in Ethiopia. Global Health Action. 2010;3 doi: 10.3402/gha.v3i0.2070. 10.3402/gha.v3i0.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhakal L, Berg-Beckhoff G, Aro AR. Intimate partner violence (physical and sexual) and sexually transmitted infection: Results from Nepal Demographic Health Survey 2011. International Journal of Women's Health. 2014;6:75–82. doi: 10.2147/IJWH.S54609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hembling J, Andrinopoulos K. Evidence of increased STI/HIV-related risk behavior among male perpetrators of intimate partner violence in Guatemala: Results from a national survey. AIDS Care. 2014:1–8. doi: 10.1080/09540121.2014.913766. [DOI] [PubMed] [Google Scholar]
- Hess KL, Javanbakht M, Brown JM, Weiss RE, Hsu P, Gorbach PM. Intimate partner violence and sexually transmitted infections among young adult women. Sexually Transmitted Diseases. 2012;39(5):366–371. doi: 10.1097/OLQ.0b013e3182478fa5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- Joshi SK, Malla A, Aryal UR, Indur D. Impact of intimate partner violence on women's health—a population based study in Nepal [Abstract] Injury Prevention. 2012;18(Suppl 1):A183–A183. doi: 10.1136/injuryprev-2012-040590q.17. [DOI] [Google Scholar]
- Kishor S. Married women's risk of STIs in developing countries: The role of intimate partner violence and partner's infection status. Violence Against Women. 2012;18(7):829–853. doi: 10.1177/1077801212455358. [DOI] [PubMed] [Google Scholar]
- Kiss L, Schraiber LB, Heise L, Zimmerman C, Gouveia N, Watts C. Gender-based violence and socioeconomic inequalities: Does living in more deprived neighbourhoods increase women’s risk of intimate partner violence? Social Science & Medicine. 2012;74(8):1172–1179. doi: 10.1016/j.socscimed.2011.11.033. doi: http://dx.doi.org/10.1016/j.socscimed.2011.11.033. [DOI] [PubMed] [Google Scholar]
- Laanpere M, Ringmets I, Part K, Karro H. Intimate partner violence and sexual health outcomes: A population-based study among 16-44-year-old women in Estonia. European Journal of Public Health. 2013;23(4):688–693. doi: 10.1093/eurpub/cks144. [DOI] [PubMed] [Google Scholar]
- Lamichhane P, Puri M, Tamang J, Dulal B. Women's status and violence against young married women in rural Nepal. BMC Women's Health. 2011;11:19-6874–11-19. doi: 10.1186/1472-6874-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin EK, Taft CT, Resick PA. A review of marital rape. Aggression and Violent Behavior. 2007;12(3):329–347. doi: http://dx.doi.org/10.1016/j.avb.2006.10.003. [Google Scholar]
- Ministry of Health and Population. New ERA. ICF International Inc . Nepal Demographic Health Survey 2011. Kathmandu, Nepal, Calverton, Maryland. Ministry of Health and Population, New ERA, and ICF International, Calverton, Maryland; Kathmandu, Nepal: 2012. [Google Scholar]
- Mittal M, Senn TE, Carey MP. Fear of violent consequences and condom use among women attending an STD clinic. Women & Health. 2013;53(8):795–807. doi: 10.1080/03630242.2013.847890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for AIDS and STD Control . National estimates of HIV infections in nepal 2012. Ministry of Health and Population, National Center for AIDS and STD Control; Kathmandu, Nepal: 2012. [Google Scholar]
- O'Leary KD, Schumacher JA. The association between alcohol use and intimate partner violence: Linear effect, threshold effect, or both? Addictive Behaviors. 2003;28(9):1575–1585. doi: 10.1016/j.addbeh.2003.08.034. doi: http://dx.doi.org.ezproxy.lib.uconn.edu/10.1016/j.addbeh.2003.08.034. [DOI] [PubMed] [Google Scholar]
- Oshiro A, Poudyal AK, Poudel KC, Jimba M, Hokama T. Intimate partner violence among general and urban poor populations in Kathmandu, Nepal. Journal of Interpersonal Violence. 2011;26(10):2073–2092. doi: 10.1177/0886260510372944. Retrieved from http://jiv.sagepub.com/content/26/10/2073.abstract. [DOI] [PubMed] [Google Scholar]
- Puri M, Frost M, Tamang J, Lamichhane P, Shah I. The prevalence and determinants of sexual violence against young married women by husbands in rural Nepal. BMC Research Notes. 2012;5:291-0500–5-291. doi: 10.1186/1756-0500-5-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj A, Kidd JD, Cheng DM, Coleman S, Bridden C, Blokhina EA, Samet JH. Associations between partner violence perpetration and history of STI among HIV-infected substance using men in Russia. AIDS Care. 2013;25(5):646–651. doi: 10.1080/09540121.2012.722188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sales JM, Salazar LF, Wingood GM, DiClemente RJ, Rose E, Crosby RA. The mediating role of partner communication skills on HIV/STD-associated risk behaviors in young African American females with a history of sexual violence. Archives of Pediatrics & Adolescent Medicine. 2008;162(5):432–438. doi: 10.1001/archpedi.162.5.432. [DOI] [PubMed] [Google Scholar]
- Sareen J, Pagura J, Grant B. Is intimate partner violence associated with HIV infection among women in the United States? General Hospital Psychiatry. 2009;31(3):274–278. doi: 10.1016/j.genhosppsych.2009.02.004. [DOI] [PubMed] [Google Scholar]
- Seth P, Raiford JL, Robinson LS, Wingood GM, Diclemente RJ. Intimate partner violence and other partner-related factors: Correlates of sexually transmissible infections and risky sexual behaviours among young adult African American women. Sexual Health. 2010;7(1):25–30. doi: 10.1071/SH08075. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Gupta J, Maheshwari A, Willis BM, Raj A. HIV prevalence and predictors of infection in sex-trafficked Nepalese girls and women. JAMA : The Journal of the American Medical Association. 2007;298(5):536–542. doi: 10.1001/jama.298.5.536. doi:298/5/536 [pii] [DOI] [PubMed] [Google Scholar]
- Silverman JG, McCauley HL, Decker MR, Miller E, Reed E, Raj A. Coercive forms of sexual risk and associated violence perpetrated by male partners of female adolescents. Perspectives on Sexual and Reproductive Health. 2011;43(1):60–65. doi: 10.1363/4306011. [DOI] [PubMed] [Google Scholar]
- Stockman JK, Lucea MB, Campbell JC. Forced sexual initiation, sexual intimate partner violence and HIV risk in women: A global review of the literature. AIDS and Behavior. 2013;17(3):832–847. doi: 10.1007/s10461-012-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-Mccoy S, Sugarman DB. The revised conflict tactics scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. doi: 10.1177/019251396017003001. [DOI] [Google Scholar]
- Teitelman AM, Ratcliffe SJ, Dichter ME, Sullivan CM. Recent and past intimate partner abuse and HIV risk among young women. Journal of Obstetric, Gynecologic, and Neonatal Nursing : JOGNN / NAACOG. 2008;37(2):219–227. doi: 10.1111/j.1552-6909.2008.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend L, Jewkes R, Mathews C, Johnston L, Flisher A, Zembe Y, Chopra M. HIV risk behaviours and their relationship to intimate partner violence (IPV) among men who have multiple female sexual partners in Cape Town, South Africa. AIDS and Behavior. 2011;15(1):132–141. doi: 10.1007/s10461-010-9680-5. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Wenzel SL, Elliott MN, Marshall GN, Williamson S. Interpersonal violence, substance use, and HIV-related behavior and cognitions: A prospective study of impoverished women in Los Angeles County. AIDS and Behavior. 2004;8(4):463–474. doi: 10.1007/s10461-004-7330-5. [DOI] [PubMed] [Google Scholar]
- Tuladhar S, Khanal KR, K.C. L, Ghimire PK, Onta K. Women's empowerment and spousal violence in relation to health outcomes in Nepal: Further analysis of the 2011 nepal demographic and health survey. Nepal Ministry of Health and Population, New ERA, and ICF International; Calverton, Maryland, USA: 2013. [Google Scholar]
- Tumwesigye N, Kyomuhendo G, Greenfield T, Wanyenze R. Problem drinking and physical intimate partner violence against women: Evidence from a national survey in Uganda. BMC Public Health. 2012;12(1):399. doi: 10.1186/1471-2458-12-399. Retrieved from http://www.biomedcentral.com/1471-2458/12/399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas S, Watts C. How does economic empowerment affect women's risk of intimate partner violence in low and middle income countries? A systematic review of published evidence. Journal of International Development. 2009;21(5):577–602. doi: 10.1002/jid.1500. [DOI] [Google Scholar]
- Wang SK. Violence and HIV/AIDS: Violence against women and girls as a cause and consequence of HIV/AIDS. Duke Journal of Gender Law and Policy. 2010;17(2):313–332. [Google Scholar]
- WHO WHO facts on intimate partner violence and alcohol. 2010 Retrieved from http://www.who.int/violence_injury_prevention/violence/world_report/factsheets/fs_intimate.pdf.
- WHO . Global and regional estimates of violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence. World Health Organization; Geneva: 2013. [Google Scholar]