Abstract
Aim:
The purpose of this study was to evaluate the effect of different denture cleansers on the color stability, surface hardness, and roughness of different denture base resins.
Materials and Methods:
Three denture base resin materials (conventional heat cure resin, high impact resin, and polyamide denture base resin) were immersed for 180 days in commercially available two denture cleansers (sodium perborate and sodium hypochlorite). Color, surface roughness, and hardness were measured for each sample before and after immersion procedure.
Statistical Analysis:
One-way analysis of variance and Tukey's post hoc honestly significant difference test were used to evaluate color, surface roughness, and hardness data before and after immersion in denture cleanser (α =0.05).
Results:
All denture base resins tested exhibited a change in color, surface roughness, and hardness to some degree in both denture cleansers. Polyamides resin immersed in sodium perborate showed a maximum change in color after immersion for 180 days. Conventional heat cure resin immersed in sodium hypochlorite showed a maximum change in surface roughness and conventional heat cure immersed in sodium perborate showed a maximum change in hardness.
Conclusion:
Color changes of all denture base resins were within the clinically accepted range for color difference. Surface roughness change of conventional heat cure resin was not within the clinically accepted range of surface roughness. The choice of denture cleanser for different denture base resins should be based on the chemistry of resin and cleanser, denture cleanser concentration, and duration of immersion.
Keywords: Color stability, denture base resins, denture cleansers, hardness, surface roughness
INTRODUCTION
Over the years, a variety of materials has been used for the fabrication of the denture bases. Polymethyl methacrylate (PMMA) is the most commonly used denture base resin as they have less cost, easy manipulation, easy construction method, and easiness of repair as compared to other materials available for fabrication of denture.[1] In recent years, new-generation polyamide thermoplastic resins and butadiene styrene graft PMMA copolymer resins are more commonly used in the production of removable dentures. Polyamide denture base materials have flexible and semi-flexible structure, do not contain allergic monomer, are biocompatible, and have low density. The most important advantages of these resins are that they reflect the color of gingival tissue beneath, due to high light transparency; in other words, they have high-quality esthetic properties.
Polyamide are generally preferred for patients with MMA allergy, bruxism cases, in the patients with bone and tuberosity undercut, in thin mucosa and excessive bone resorption, in cases where the patient cannot tolerate the forces applied by the denture, in production of temporary dentures after implants, and particularly in very old patients with low motor capacity.[2]
No matter what kind of denture base material we are using, denture care is indispensable for oral health, otherwise denture become unsanitary and undesirable effects are expected such as bad breath, unpleasant staining and biofilm, calculus accumulation on the denture which can lead to denture stomatitis, angular cheilitis, and poor oral health.[3] Contamination of prostheses can provide a source of cross-contamination between patient and dental personnel. Denture plaque is also a major factor in etiology of opportunistic infections and respiratory tract infection by aspiration in elderly patients.[4]
Denture cleaning is an important measure that can prevent cross-contamination and contributes to patient's health, denture longevity, and overall quality of life. Denture disinfection has been recommended as the essential procedure for maintaining adequate denture hygiene. Several agents are indicated for denture disinfection and maintaining the health of denture, classified into mechanical and chemical agents. Mechanical methods are most commonly used and effective procedure for reducing and removing biofilm formation. Cleaning by chemical method consists of immersion of denture in solutions with solvents, detergents; antibacterial and antifungal actions and such solutions can be employed alone or in association with the mechanical method or ultrasonic method.[5]
Ideally, a disinfection method should be effective without detrimental effects on the properties of materials used for fabrication of denture base.[6] Everyday use of denture cleansers is recommended to prevent microbial colonization on denture and promote good oral health. Daily use of denture cleansers can affect the physical and mechanical properties of denture base material. In choosing a disinfectant for a dental prosthesis, consideration should be given to its compatibility with the type of material to be disinfected to avoid adverse effects.[7] Properties that are mainly affected by denture cleansers are color, surface roughness, and hardness, and these are very important for long-term success of any prosthesis.[4]
The roughness of the acrylic resin surfaces is important since the adhesion of microorganisms to a surface is a prerequisite for the colonization of that surface.[1] Hardness of denture base resin is indicative of the ease of finishing off a material, as well as its resistance to in-service scratching during cleaning procedures.[4,7] The color change is an indicator of aging or damage to dental materials. Color stability of denture base resins may provide important information on the serviceability of the materials.[8]
The present study was conducted to evaluate and compare the effects of two different denture cleansers on the color stability, surface roughness, and hardness of different denture base resins.
MATERIALS AND METHODS
Three commercially available denture base resins, conventional heat cure resin (Group I, Trevalon, Dentsply India Pvt. Ltd.), high impact resin (Group II, Trevalon, Dentsply India Pvt. Ltd.), and polyamide resin (Group III, Lucitone FRS, Dentsply India Pvt. Ltd.) and two commercially available denture cleansers such as sodium hypochlorite (Vishal Dentocare Pvt. Ltd.) and sodium perborate (Vovantis Laboratories Pvt. Ltd.) were used in this study.
Metal discs of dimension 3 mm thickness and 20 mm diameter (Rukiye Durkan) were invested in dental flasks using dental stone. The mold space thus obtained was used for the preparation of the test specimens for Groups I and II. Separating medium was applied on the dental stone mold. The conventional heat cure resin (Group I) and high impact heat cure acrylic resin (Group II) were used in the powder-liquid form. The powder and liquid were mixed as recommended by the manufacturer. When the mix reached the dough stage, it was kneaded and packed into the mold space, and final closure was done under bench press. The flasks were allowed to undergo short-time polymerization in a water bath at 72°C for 1.5 h, followed by 30 min boiling in 100°C water in an dental acrylizer. After completion of the curing cycle, the flasks were bench cooled till they reached room temperature. The specimens were recovered, and the flash was trimmed.
Following polymerization, all specimens were finished with no. 120, 200, 800 silicone carbide grinding papers and polished with 1000 grade abrasive waterproof paper, rinsed with tap water, and air dried. Specimens were polished using a slurry of water and pumice with brush wheel followed by a slurry of tin oxide with a cloth wheel.
For fabricating specimens of polyamide denture base material (Group III), injection molding system was used. Metal discs were invested in injection molding flask and sprued with modeling wax in a manner that each disc was connected with the sprue so that polyamide denture base material could flow into each mold space. After spruing, the flask was counter poured. The flask was kept for dewaxing after setting of dental stone, and the metal discs were removed to obtain the mold space. Flask was closed and tightened with the screws and was placed on the bench press. The cartridge of polyamide denture base resin was kept in the heating unit and heated according to manufacturer's instruction (300°C for 20 min) and then was placed on the flask. The pressure was applied to the cartridge from bench press so that the material flew into the mold space through sprues. Once processed, the flask was allowed to bench cool for 2 h. Specimens were ground using progressively smoother aluminum oxide paper (200, 600, 800, and 1000 grit). Twenty samples were fabricated with each denture base material [Figure 1]. Specimens of each denture base materials were grouped into two groups of ten specimens for immersion in sodium hypochlorite and sodium perborate denture cleanser.
Figure 1.
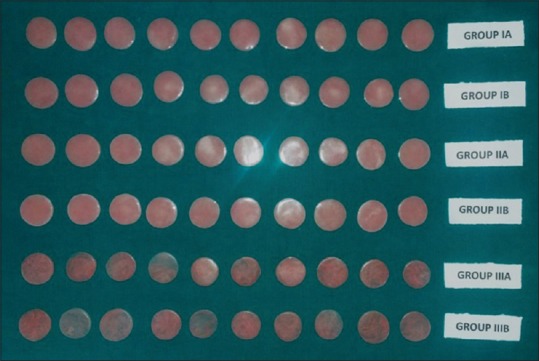
Finished and polished specimens (original photograph)
Marking and numbering were done on the surface of the test specimen. Initial measurements for color, surface roughness, and hardness were performed. The color was measured with a spectrophotometer using Commission International de l'Eclairage L*a*b* system [Figure 2]. The surface roughness (Ra, µm) was analyzed with a profilometer [Figure 3]. Ra is the mathematical average of the absolute values of the measure profile height of surface irregularities, measured from a mean line within a preset length of the specimen; microhardness measurements were obtained with a Vickers hardness tester [Figure 4]. Diamond indenter point in the shape of a square-based pyramid was used for measuring hardness. Fifty gram load and a 30 s period were used.
Figure 2.

Color measurement using spectrophotometer (original photograph)
Figure 3.
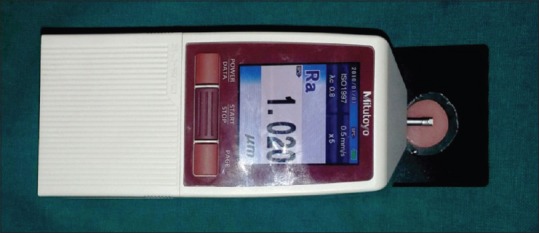
Surface roughness measurement using profilometer (original photograph)
Figure 4.

Hardness measurement using Vicker's hardness tester (original photograph)
Denture cleanser solutions used were 0.5% sodium hypochlorite and 3.8% sodium perborate. All the specimens were stored in distilled water for 24 h. Ten specimens of each group were immersed in sodium hypochlorite denture cleanser for 10 min daily at room temperature and named as Sub-group A and another ten were immersed in sodium perborate for 10 min daily at room temperature and named as Sub-group B. After 10 min, specimens were thoroughly washed and stored in distilled water at room temperature. This procedure was repeated daily for 180 days.[7,9,10]
Final measurements of color, surface roughness, and hardness were performed after 180 days of immersion procedure. Color differences (▲E) between specimens were calculated using formula ▲E = ([▲L*]2+ [▲a*]2+ [▲b*]2)½. The difference in surface roughness and hardness was also calculated.
RESULTS
The results and statistical analysis of the study are summarized in Tables 1–6. The results of the study revealed that all the denture base resin specimens used in the study exhibited a change in color with immersion in different denture cleansers. The maximum color change was seen in polyamide denture base resin specimens immersed in sodium perborate denture cleanser which was significantly different from other groups (P < 0.05).
Table 1.
One-way analysis of variance of color difference of different denture base resins immersed in sodium hypochlorite and sodium perborate denture cleansers
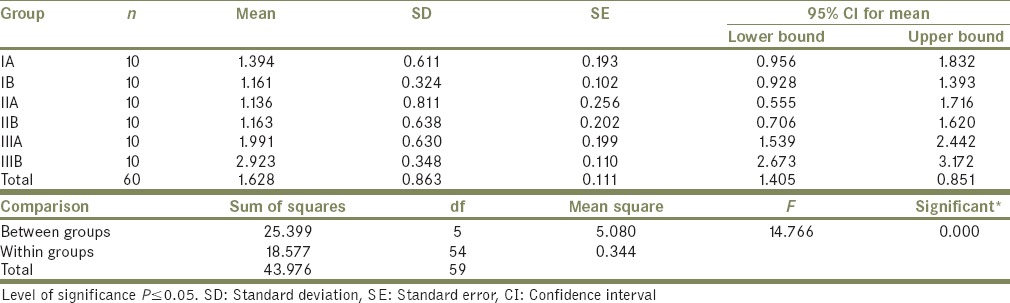
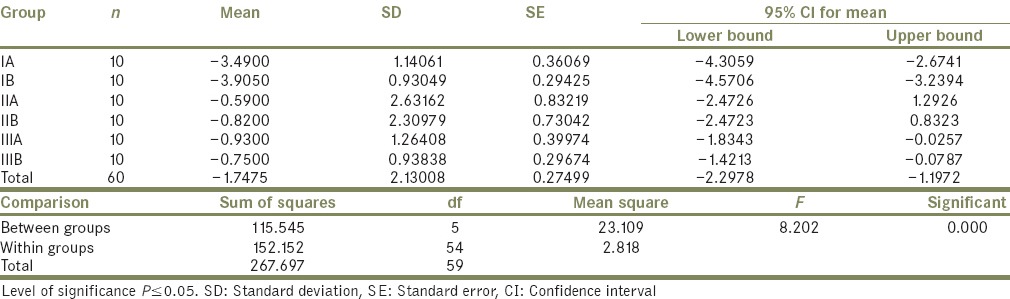
Table 6.
Summary of post hoc Tukey's test for change in hardness of different denture base resins immersed in sodium hypochlorite and sodium perborate denture cleansers
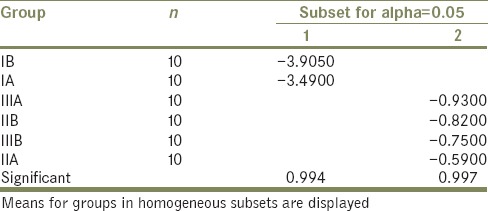
Table 2.
Summary of post hoc Tukey's test for color difference of different denture base resins immersed in sodium hypochlorite and sodium perborate denture cleansers
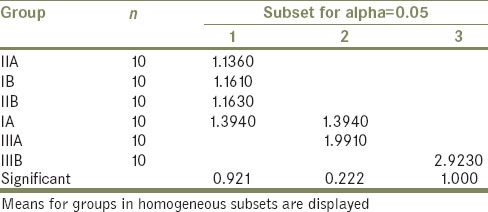
Table 3.
One-way analysis of variance of change in surface roughness of different denture base resins immersed in sodium hypochlorite and sodium perborate denture cleansers
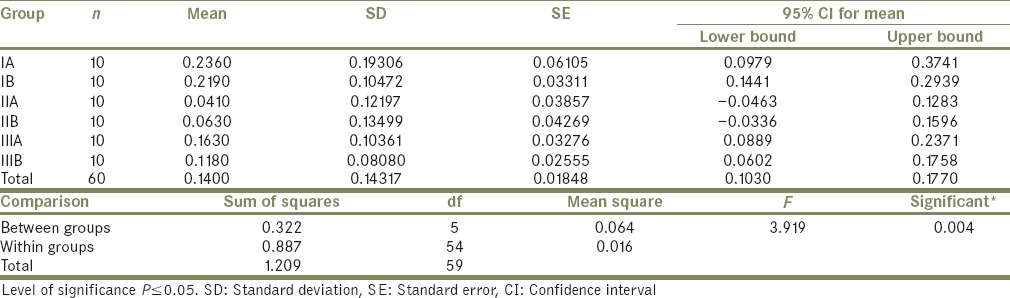
Table 4.
Summary of post hoc Tukey's test for change in surface roughness of different denture base resins immersed in sodium hypochlorite and sodium perborate denture cleansers
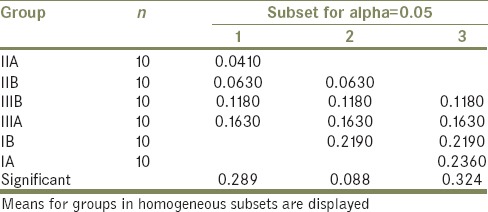
Table 5.
One-way analysis of variance of change in hardness of different denture base resins immersed in sodium hypochlorite and sodium perborate denture cleansers
All the denture base resin specimens in the present study exhibited an increase in surface roughness with immersion in different denture cleansers. Conventional heat cure acrylic resin and polyamide resin specimens exhibited more increase in surface roughness as compared to high impact acrylic resin. The difference between the effects of denture cleansers on the surface roughness of individual denture base resins was not statistically significant (P > 0.05).
Polyamide resin exhibited less initial hardness than both acrylic resins. All the denture base resin specimens in the present study exhibited a decrease in hardness with immersion in different denture cleansers. Conventional heat cure acrylic resin specimens exhibited more decrease in hardness as compared to high impact acrylic resin and polyamide resin. The difference between the effects of denture cleansers on the hardness of individual denture base resins was not statistically significant (P > 0.05).
DISCUSSION
Denture cleaning is an important measure that can prevent cross-contamination and contributes to patient's health, denture longevity, and overall quality of life. Denture disinfection has been recommended as the essential procedure for maintaining adequate denture hygiene. Several agents are indicated for denture disinfection and maintaining the health of denture, classified into mechanical and chemical agents. Ideally, a disinfection method should be effective without detrimental effects on the properties of materials used for fabrication of denture base.
Daily use of denture cleansers can affect the physical and mechanical properties of denture base material. Many chemical denture cleansers are available for cleaning the denture. About 5.25% sodium hypochlorite solution is an effective method for killing adherent microorganism. However, in high concentration, this disinfecting solution may damage denture materials. de Freitas Fernandes et al.[11] and Davi et al.[12] found that hypochlorite solution in low concentration (0.5%) is also effective in eliminating all microorganisms. In the present study, 0.5% sodium hypochlorite and 3.8% sodium perborate were used for immersion procedure. Paranhos et al.,[5] Neppelenbroek et al.,[7] Ural et al.,[9] and Gornitsky et al.[13] found sodium hypochlorite and sodium perborate at this concentration as appropriate denture cleansers for protecting prosthesis from microbial colonization and maintaining oral and denture health. Amin et al.,[10] Neppelenbroek et al.,[7] and Ural et al.[9] found that daily 10 min of immersion is needed for sodium hypochlorite and sodium perborate denture cleanser solutions to completely disinfect the denture.
The difference in color changes of denture base resins can be attributed to their composition and the solution in which they were immersed. Denture cleansers cause loss of soluble component and plasticizers from the denture base resins. Higher ionic concentration of denture cleansers compared to water led to a higher release of soluble components. Further absorption of water and other salivary components by the denture base materials leads to surface roughness and color change
The PMMA denture base resins are hydrophilic that attract more water soluble materials on the surface that absorption is undoubtedly due primarily to the polar properties of resin molecules. However, it has been proven that the mechanism is diffusion of water molecules that penetrate according to diffusion law, but still the high bond due to cross-linking agent gives it resistance to changes due to denture cleansers. On the contrary, polyamide resin has increased absorption of water and dissolution of plasticizers leading to more deterioration of properties.[14]
Further, color changes for polyamide denture base resin were more in sodium perborate denture cleanser as compared to sodium hypochlorite denture cleansers. This is attributed to the chemical effect of perborate denture cleanser along with oxygen release through effervescent effect. This released oxygen by sodium perborate denture cleanser has a high dissolving effect on plasticizers and loosens debris through mechanical means. Therefore, the use of this denture cleanser causes hydrolysis and decomposition of polymerized acrylic resin itself.[8] Nikawa et al.[15] in his study observed that high peroxide content and level of oxygenation in the strongly alkaline solution is a damaging factor for denture base materials. The color difference for Group I and Group II in sodium hypochlorite and sodium perborate denture cleansers was not statistically significant, and this result was consistent with a study done by Sato et al.[16] and Paranhos et al.[5]
The critical remark of the color change (▲E) has been quantified by the National Bureau of Standards (NBS), as NBS units of color difference. NBS units are expressed by the following formula: NBS unit = ▲E × 0.92.[17] In the present study, NBS unit of color difference for Groups IA, IB, IIA, IIB, IIIA, and IIIB are 1.282, 1.068, 1.045, 1.069, 1.831, and 2.689, respectively. A material is considered esthetically and clinically acceptable if NBS units lie in the range of 3.7 NBS unit, and NBS unit value over 1 was considered perceivable by the human eye. Differences above 3.7 NBS unit are rated a “mismatch” and considered as clinically unacceptable. In the present study, color changes of all denture base resins were within the clinically accepted range for color difference.
High impact heat cure resin shows the least change in surface roughness. This can be attributed to high cross-linking structure present in high impact heat cure resins causing fewer surface changes in it as compared to other materials.[18] Polyamide resins show a change in surface roughness because of leaching out of plasticizers due to the effect of denture cleansers and conventional heat cure shows a change in surface roughness because of less crosslinking of structure. In a study conducted by Bollen et al.[19] and Abuzar et al.,[20] it was found that Ra value of 0.2 µm is the threshold surface roughness value for microbial retention below which no further reduction in bacterial accumulation could be expected. An increase in surface roughness above this threshold roughness, however, resulted in a simultaneous increase in plaque accumulation. In the present study, surface roughness change of conventional heat cure resin was not within the clinically accepted range of surface roughness. The surface roughness of all other groups was found to be in clinically acceptable range.
Decrease in hardness of conventional heat cure acrylic resin specimens can be attributed to the continuous polymerization reaction, monomer release, and the combination of monomers with free active radicals by bonding with liberated oxygen. High impact resin has less residual monomer and no residual monomer in polyamide resin, so less decrease in hardness of these materials.[1] Less decrease in hardness of high impact resins is because of high cross-linking and butadiene styrene graft copolymer. Pinto Lde et al.[21] reported that polyamide resins have higher mechanical resistance than conventional heat cure resins, so they show less decrease in hardness. The difference between the effects of denture cleansers on the hardness of individual denture base resins was not statistically significant.
In the present study, all combinations of denture cleansers with denture base materials exhibited a change in color, surface roughness, and hardness. The changes were found to be clinically acceptable for high impact acrylic resin and polyamide resin. Conventional heat cure resin exhibited an increase in the surface roughness above a threshold value of clinically acceptable limit with both the denture cleansers. Denture cleansers used in the study were appropriate for disinfecting the polyamide and high impact denture base resins at given concentration. Although color change and hardness changes for conventional heat cure were acceptable at this concentration, roughness was increased above clinically acceptable value, so an alteration in concentration or duration of immersion is required. The choice of denture cleanser for different denture base resins should be based on the chemistry of resin and cleanser, denture cleanser concentration, and duration of immersion. In addition to appropriate choice of denture cleanser, proper use of denture cleanser as prescribed by the manufacturer should be strictly followed by the patients with reference to the concentration of denture cleanser, temperature of solution, and duration of immersion.
CONCLUSION
All denture base resins tested exhibited change in color, surface roughness, and hardness to some degree in both denture cleansers
The color changes in polyamide resin were significantly greater than those of heat cure acrylic resin and high impact heat cure acrylic resin
Color change for polyamide denture base resin was more in sodium perborate denture cleanser as compared to sodium hypochlorite denture cleanser
Color changes of all denture base resins were within the clinically accepted range for color difference
Surface roughness change in conventional heat cure resin was significantly greater than high impact resin and insignificantly greater than polyamide resin
Surface roughness change of conventional heat cure resin was not within the clinically accepted range of surface roughness
Change in hardness of conventional in heat cure resin was significantly greater than those of high impact and polyamide acrylic resin
Chemical structure, polymerization technique, degree of cross-linking, amount of plasticizers, absorption, solubility, surface treatment, and finishing and polishing methods of the denture base resins are the factors which significantly affect the color stability, surface roughness, and hardness of denture base resins
Chemical structure, immersion time, temperature of solution, and mechanism of action of a denture cleanser are the factors which affect the color stability, surface roughness, and hardness of denture base resins immersed in them.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hersek N, Canay S, Uzun G, Yildiz F. Color stability of denture base acrylic resins in three food colorants. J Prosthet Dent. 1999;81:375–9. doi: 10.1016/s0022-3913(99)80001-8. [DOI] [PubMed] [Google Scholar]
- 2.Ucar Y, Akova T, Aysan I. Mechanical properties of polyamide versus different PMMA denture base materials. J Prosthodont. 2012;21:173–6. doi: 10.1111/j.1532-849X.2011.00804.x. [DOI] [PubMed] [Google Scholar]
- 3.Salman M, Saleem S. Effect of different denture cleanser solutions on some mechanical and physical properties of nylon and acrylic denture base materials. J Baghdad Coll Dent. 2011;23:19–24. [Google Scholar]
- 4.Machado AL, Breeding LC, Vergani CE, Perez LE. Hardness and surface roughness of reline and denture base acrylic resins after repeated disinfection procedures. J Prosthet Dent. 2009;102:115–22. doi: 10.1016/S0022-3913(09)60120-7. [DOI] [PubMed] [Google Scholar]
- 5.Paranhos Hde F, Peracini A, Pisani MX, Oliveira Vde C, de Souza RF, Silva-Lovato CH. Color stability, surface roughness and flexural strength of an acrylic resin submitted to simulated overnight immersion in denture cleansers. Braz Dent J. 2013;24:152–6. doi: 10.1590/0103-6440201302151. [DOI] [PubMed] [Google Scholar]
- 6.Machado AL, Giampaolo ET, Vergani CE, Souza JF, Jorge JH. Changes in roughness of denture base and reline materials by chemical disinfection or microwave irradiation: Surface roughness of denture base and reline materials. J Appl Oral Sci. 2011;19:521–8. doi: 10.1590/S1678-77572011000500015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neppelenbroek KH, Pavarina AC, Vergani CE, Giampaolo ET. Hardness of heat-polymerized acrylic resins after disinfection and long-term water immersion. J Prosthet Dent. 2005;93:171–6. doi: 10.1016/j.prosdent.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 8.Hong G, Murata H, Li Y, Sadamori S, Hamada T. Influence of denture cleansers on the color stability of three types of denture base acrylic resin. J Prosthet Dent. 2009;101:205–13. doi: 10.1016/S0022-3913(09)60032-9. [DOI] [PubMed] [Google Scholar]
- 9.Ural C, Sanal FA, Cengiz S. Effect of different denture cleansers on surface roughness of denture base materials. Clin Dent Res. 2011;35:14–20. [Google Scholar]
- 10.Amin F, Iqbal S, Azizuddin S, Afridi FI. Effect of denture cleansers on the color stability of heat cure acrylic resin. J Coll Physicians Surg Pak. 2014;24:787–90. [PubMed] [Google Scholar]
- 11.de Freitas Fernandes FS, Pereira-Cenci T, da Silva WJ, Filho AP, Straioto FG, Del Bel Cury AA. Efficacy of denture cleansers on Candida spp. biofilm formed on polyamide and polymethyl methacrylate resins. J Prosthet Dent. 2011;105:51–8. doi: 10.1016/S0022-3913(10)60192-8. [DOI] [PubMed] [Google Scholar]
- 12.Davi LR, Felipucci DN, de Souza RF, Bezzon OL, Lovato-Silva CH, Pagnano VO, et al. Effect of denture cleansers on metal ion release and surface roughness of denture base materials. Braz Dent J. 2012;23:387–93. doi: 10.1590/s0103-64402012000400013. [DOI] [PubMed] [Google Scholar]
- 13.Gornitsky M, ParadisI I, Landaverde G, Malo AM, Velly AM. A clinical and microbiological evaluation of denture cleansers for geriatric patients in long-term care institutions. J Can Dent Assoc. 2002;68:39–45. [PubMed] [Google Scholar]
- 14.Garcia RM, Léon BT, Oliveira VB, Del Bel Cury AA. Effect of a denture cleanser on weight, surface roughness, and tensile bond strength of two resilient denture liners. J Prosthet Dent. 2003;89:489–94. doi: 10.1016/s0022-3913(03)00126-4. [DOI] [PubMed] [Google Scholar]
- 15.Nikawa H, Iwanaga H, Hamada T, Yuhta S. Effects of denture cleansers on direct soft denture lining materials. J Prosthet Dent. 1994;72:657–62. doi: 10.1016/0022-3913(94)90300-x. [DOI] [PubMed] [Google Scholar]
- 16.Sato S, Cavalcante MR, Orsi IA, Paranhos Hde F, Zaniquelli O. Assessment of flexural strength and color alteration of heat-polymerized acrylic resins after simulated use of denture cleansers. Braz Dent J. 2005;16:124–8. doi: 10.1590/s0103-64402005000200007. [DOI] [PubMed] [Google Scholar]
- 17.Nimeroff I. Colorimetry National Bureau of Standards. Monograph 104. Washington D.C: U.S. Government Printing Office; 1968. p. 47. [Google Scholar]
- 18.Durkan R, Ayaz EA, Bagis B, Gurbuz A, Ozturk N, Korkmaz FM. Comparative effects of denture cleansers on physical properties of polyamide and polymethyl methacrylate base polymers. Dent Mater J. 2013;32:367–75. doi: 10.4012/dmj.2012-110. [DOI] [PubMed] [Google Scholar]
- 19.Bollen CM, Papaioanno W, Van Eldere J, Schepers E, Quirynen M, van Steenberghe D. The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clin Oral Implants Res. 1996;7:201–11. doi: 10.1034/j.1600-0501.1996.070302.x. [DOI] [PubMed] [Google Scholar]
- 20.Abuzar MA, Bellur S, Duong N, Kim BB, Lu P, Palfreyman N, et al. Evaluating surface roughness of a polyamide denture base material in comparison with poly (methyl methacrylate) J Oral Sci. 2010;52:577–81. doi: 10.2334/josnusd.52.577. [DOI] [PubMed] [Google Scholar]
- 21.Pinto Lde R, Acosta EJ, Távora FF, da Silva PM, Porto VC. Effect of repeated cycles of chemical disinfection on the roughness and hardness of hard reline acrylic resins. Gerodontology. 2010;27:147–53. doi: 10.1111/j.1741-2358.2009.00282.x. [DOI] [PubMed] [Google Scholar]


