Abstract
Disclusion time reduction (DTR) is an objective treatment protocol using T-Scan III (digital analysis of occlusion) and electromyography for treating occlusally activated orofacial pains. Chronic occluso-muscle disorder is a myogenous subset of temporomandibular disorder symptoms. These muscular symptoms are induced within hyperactive masticatory muscles due to prolonged disclusion time, occlusal interferences, and occlusal surface friction that occur during mandibular excursive movements. This case report describes a patient treated by DTR therapy, whereby measured pretreatment prolonged disclusion time was reduced to short disclusion time using the immediate complete anterior guidance development enameloplasty, guided by T-Scan occlusal contact time and force analysis synchronized with electromyographic recordings of four masticatory muscles.
Keywords: Disclusion time, disclusion time reduction, immediate complete anterior guidance development enameloplasty, myofascial pain, T-Scan/Bio-electromyography III
INTRODUCTION
Occlusal interferences and occlusal surface friction present during excursive movements have been considered to be contributory etiological factors for occluso-muscular pain and symptoms observed commonly in temporomandibular disorder (TMD) patients.[1,2,3,4,5] A measurement-driven, computer-guided occlusal adjustment procedure known as immediate complete anterior guidance development (ICAGD),[6] whose primary therapeutic goal of measurably decreasing the time required for all molars and premolars to disclude from each other (known as the disclusion time) in <0.4 s during right and left mandibular excursions commenced from complete intercuspation in maximum intercuspal position (MIP).[6] The ICAGD enameloplasty is guided by the time measurement capability of T-Scan III occlusal analysis system (Tekscan, Inc., South Boston, MA, USA), where specific excursive movement time-duration, numerical end-points must be achieved to verify whether the enameloplasty was properly accomplished.[6,7] ICAGD has repeatedly shown to successfully treat myofascial pain symptoms without requiring the treated patient to wear a splint or deprogrammer.[8,9,10,11,12,13,14]
Shortening the disclusion time with ICAGD is performed with two synchronized occlusal measurement technologies (T-Scan III Computerized Occlusal Analysis System, Tekscan Inc. South Boston, MA, USA; BioEMG III electromyography [EMG], Bioresearch Associates, Milwaukee, WI, USA).[12,13] Together, these two technologies simultaneously record real-time force movies of mandibular excursive movements, and those of same movement-associated masticatory muscle contraction patterns.
Bilateral closure contact time simultaneity can also be clinically established using the T-Scan because it measures from the 1st contact into complete intercuspation, the order and duration of a patient's self-closure contact sequence (known as the occlusion time [OT]).[15] Establishing computer-guided bilateral time simultaneity ensures that no region of the dental arch contacts too early, absorbing excessive early occlusal stress, or too late, being unable to assist other regions of the arch in closure occlusal force dissipation.
Precision force and timing diagnostic and treatment control are made possible because the T-Scan's recording sensor consistently reproduces 256 levels of varying occlusal force (HD Sensor, Tekscan, Inc., South Boston, MA, USA).[16] The force and timing data replace the very inaccurate “hit or miss” method where an operator subjectively interprets colored articulating paper ink marks left on the teeth.[17]
This case report describes an occluso-muscle disorder patient who had their prolonged pretreatment disclusion time reduced to short disclusion time by undergoing the ICAGD enameloplasty. Shortly, thereafter, the patient's dysfunctional muscular symptoms began to abate and lessen, without the patient using any occlusal appliance, deprogrammer, or splint. The findings of this report align very closely with the numerous published papers that have described the rapid physiologic healing effect that disclusion time reduction (DTR) offers myogenous TMD sufferers.
CASE REPORT
A 31-year-old female patient presented with a 3-year history of difficulty in opening her jaw, pain anterior to her ears, and frequent headaches in her temples. She also complained of pain in her jaw, fatigue while chewing, strain behind her eyes, and difficulty in chewing hard foods. Three previous dentists treated her with occlusal splints that she discontinued as appliance therapy did not noticeably reduce her symptoms.
The patient underwent a temporomandibular joint examination using Joint Vibration Analysis (JVA, BioResearch Assoc., Milwaukee, WI, USA) and T-Scan III/BioEMG recordings to determine her occlusal function and the masticatory muscular contraction patterns related to that occlusal function.
The patient is connected to T-Scan and EMG gadgets and then asked to bite into the sensor after inserting it into the mouth. The patient is asked to bite hard into the sensor and open, for three times for a multibite, to bite hard and hold for few seconds, and then to glide to left or right to obtain the records as shown in Figures 1–3.
Figure 1.

Pre-treatment Multi Bite: low EMG amplitude in the 3 clenches due to weak muscles
Figure 3.
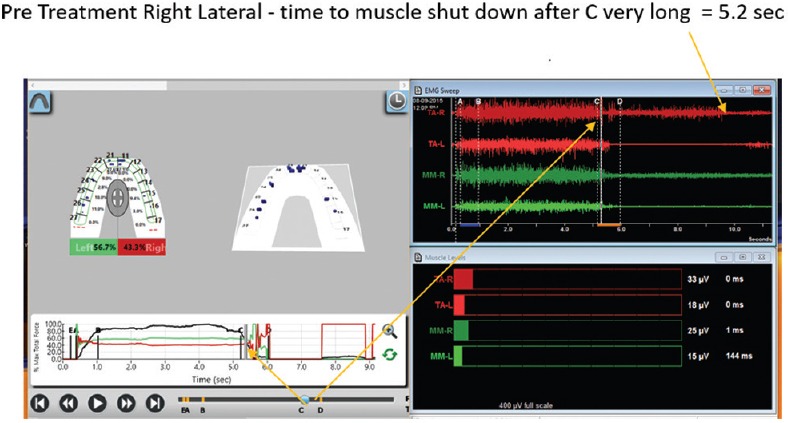
Pre Treatment Right Lateral - time to muscle shut down after C very long = 5.2 sec and “taller force curves in T-Scan data”
The assessment determined that patient had no internal derangements of significance but presented with prolonged OT of 1.32 s when closing into MIP, prolonged left excursive disclusion time of 1.15 s, and prolonged right excursive disclusion time of 0.86 s [Figures 1–3]. These values were outside of the known physiologic ranges (physiologic OT <0.2 s; DT <0.4 s).[9,15] Of note is that the time to muscle shut down[14] of the working temporalis muscles in Figures 2 and 3 ranges between 4.0 and 5.2 s, which is far too long to be physiologic. This prolonged muscle firing is a major contributor to the occluso-muscular symptoms the patient experiences.
Figure 2.
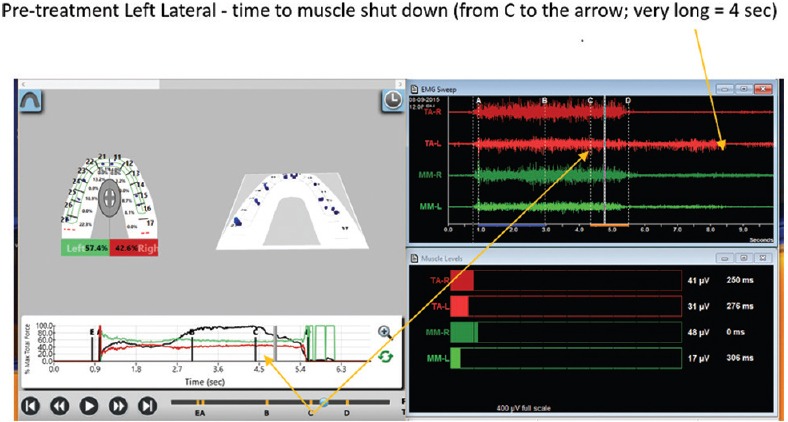
Pre-treatment Left Lateral - time to muscle shut down (from C to the arrow; very long = 4 sec)
The patient was explained that her disclusion times were too long, causing excursive muscle hyperactivity detected in the EMG data [Figures 2 and 3 to the right of line C], which caused her muscular symptoms. She was further explained that her muscular pains could be minimized or eliminated if she elected to have her DTR.
After obtaining patient consent, the ICAGD enameloplasty was performed on her right and left excursive movements as previously described[6] to remove the prolonged occlusal surface friction and to reduce the DTs to within physiologic durations. On post-ICAGD, the corrected OT was 0.17 s [Figure 4], the left excursive DT was 0.16 s [Figure 5], and the right excursive DT was 0.22 s [Figure 6]. When comparing the pretreatment excursive EMG hyperactivity [Figures 2 and 3] with the post-ICAGD excursive EMG data as shown in Figures 5 and 6, the excursive hyperactivity in both treated excursions was markedly lessened following ICAGD [Figures 5 and 6 to the right of line C]. In addition, the time to muscle shut down[14] of both working temporalis was drastically shortened from the ICAGD corrections. This is the reason that ICAGD is effective in treating occluso-muscle disorder symptoms; ICAGD shortens the contraction times of the involved muscles, thereby allowing for ischemic and painful muscle fiber reoxygenation and fiber healing.[14]
Figure 4.
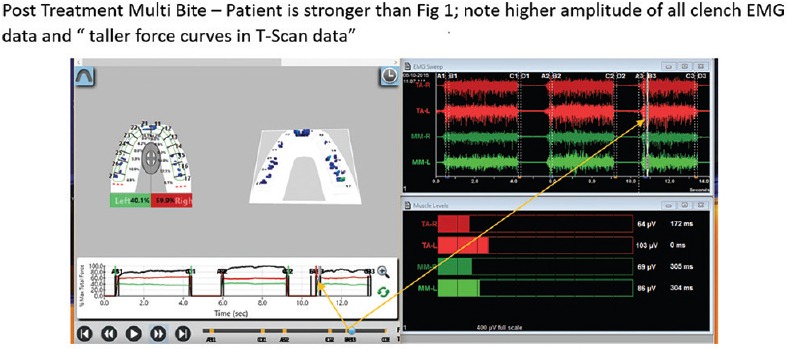
Post Treatment Multi Bite – Patient is stronger than Figure 1; note higher amplitude of all clench EMG data and “taller force curves in T-Scan data”
Figure 5.
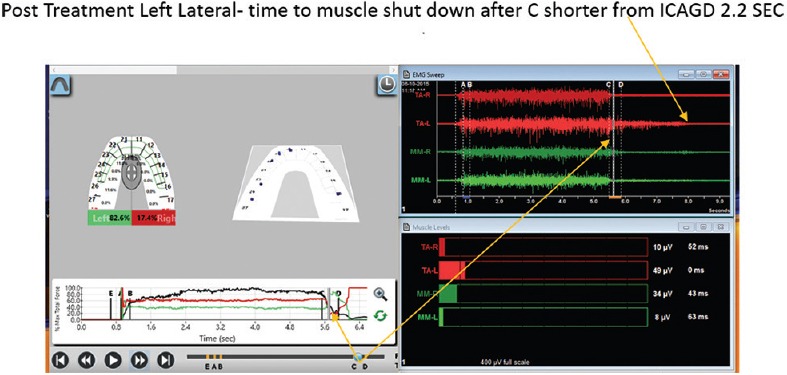
Post Treatment Left Lateral- time to muscle shut down after C shorter from ICAGD
Figure 6.
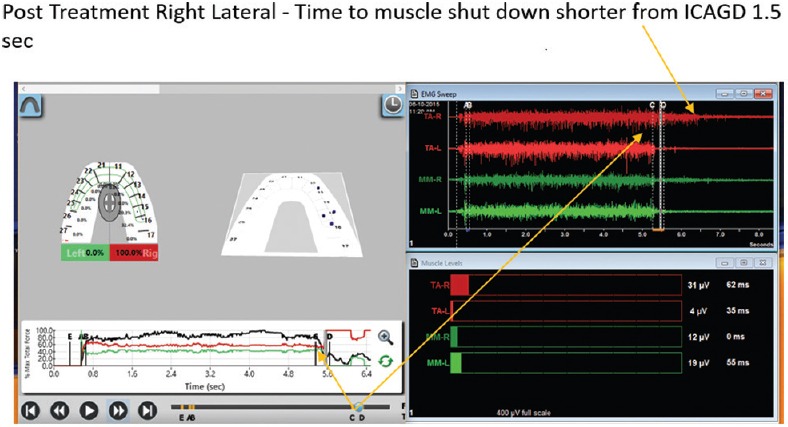
Post Treatment Right Lateral - Time to muscle shut down shorter from ICAGD 1.5 sec
DISCUSSION
The presented case illustrates that muscular TMD symptoms respond well to occlusal adjustment therapy that is guided by precise closure and excursive timing measurements. This patient's response mirrors as that has been reported in many published ICAGD studies and clinical reports[8,9,10,11,12,13,14] since the inception of the T-Scan I technology in the mid-1980's[18,19] such that treating the myofascial pain dysfunction with ICAGD is not new. Lengthy disclusion time has been shown in EMG studies to elevate excursive muscle activity levels, and that proper reduction of the disclusion time to <0.4 s can reduce the muscle hyperactivity and related myofascial pain symptoms.[9,12,13]
The beauty of this computer-guided treatment approach is that it lessens hyperactive muscles from within the central nervous system, by controlling the molar periodontal ligament (PDL) mechanoreceptors, which synapse directly with efferent motor fibers that contract the four masticatory muscles.[20] Prolonged excursive frictional contacts increased the total time PDL mechanoreceptors are compressed in excursive movements where the PDL compression time is equal to the disclusion time of that same excursion.[7] The more time the excursive interferences contact, the longer time the PDLs are compressed, resulting in prolonged durations of masticatory muscle contractions.[9,12,13] By reducing the length of time, the posterior occlusal surfaces contact excursively, the volume and duration that PDL mechanoreceptors are reduced, thereby interrupting the PDL compression-to-muscle hypercontraction. Post-ICAGD, the PDL no longer hyperfunctions the involved muscles into a painful ischemic state, allowing for reoxygenation and muscle fiber recovery, leading to symptom resolution without the patient wearing an appliance, undergoing transcutaneous electrical nerve stimulation, taking pain, muscle relaxant, or anti-inflammatory medications, or requiring trigger point and/or Botox injections. Properly performed ICAGD is a marked improvement in the treatment of myofascial pain dysfunction symptoms when compared to unmeasured occlusal equilibration involving centric relation manipulation[1,21] and to the many commonly employed symptomatic, nonocclusal therapies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tsolka P, Preiskel HW. Kinesiographic and electromyographic assessment of the effects of occlusal adjustment therapy on craniomandibular disorders by a double-blind method. J Prosthet Dent. 1993;69:85–92. doi: 10.1016/0022-3913(93)90246-k. [DOI] [PubMed] [Google Scholar]
- 2.Forssell H, Kirveskari P, Kangasniemi P. Effect of occlusal adjustment on mandibular dysfunction. A double-blind study. Acta Odontol Scand. 1986;44:63–9. doi: 10.3109/00016358609041309. [DOI] [PubMed] [Google Scholar]
- 3.Thumati P. The influence of immediate complete anterior guidance development technique on subjective symptoms in myofascial pain patients: Verified using digital analysis of occlusion (Tekscan) for analyzing occlusion: A 3 year's clinical observation. J Indian Prosthet Soc. 2015;3:218–23. doi: 10.4103/0972-4052.158079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerstein RB, Farrell S. Treatment of myofascial pain-dysfunction syndrome with occlusal equilibration. J Prosthet Dent. 1990;63:695–700. doi: 10.1016/0022-3913(90)90328-a. [DOI] [PubMed] [Google Scholar]
- 5.Kerstein RB. Treatment of myofascial pain dysfunction syndrome with occlusal therapy to reduce lengthy disclusion time – A recall evaluation. Cranio. 1995;13:105–15. doi: 10.1080/08869634.1995.11678053. [DOI] [PubMed] [Google Scholar]
- 6.Kerstein R. Disclusion time reduction therapy with immediate complete anterior guidance development: The technique. Quintessence Int. 1992;23:735–47. [PubMed] [Google Scholar]
- 7.Kerstein RB. A comparison of traditional occlusal equilibration and immediate complete anterior guidance development. Cranio. 1993;11:126–39. doi: 10.1080/08869634.1993.11677954. [DOI] [PubMed] [Google Scholar]
- 8.Thumati P, Manwani R, Mahantshetty M. The effect of reduced disclusion time in the treatment of myofascial pain dysfunction syndrome using immediate complete anterior guidance development protocol monitored by digital analysis of occlusion. J Craniomandib Pract. 2014;32:289–99. doi: 10.1179/2151090314Y.0000000004. [DOI] [PubMed] [Google Scholar]
- 9.Kerstein RB, Wright NR. Electromyographic and computer analyses of patients suffering from chronic myofascial pain-dysfunction syndrome: Before and after treatment with immediate complete anterior guidance development. J Prosthet Dent. 1991;66:677–86. doi: 10.1016/0022-3913(91)90453-4. [DOI] [PubMed] [Google Scholar]
- 10.Kerstein RB, Chapman R, Klein M. A comparison of ICAGD (Immediate complete Anterior Guidance Development) to “mock ICAGD” for symptom reductions in chronic myofascial pain dysfunction patients. J Craniomandib Pract. 1997;15:21–37. doi: 10.1080/08869634.1997.11745990. [DOI] [PubMed] [Google Scholar]
- 11.Kerstein R. Disclusion time measurement studies: Stability of disclusion time – A 1-year follow-up. J Prosthet Dent. 1994;72:164–8. doi: 10.1016/0022-3913(94)90075-2. [DOI] [PubMed] [Google Scholar]
- 12.Kerstein RB, Radke J. Masseter and temporalis excursive hyperactivity decreased by measured anterior guidance development. Cranio. 2012;30:243–54. doi: 10.1179/crn.2012.038. [DOI] [PubMed] [Google Scholar]
- 13.Kerstein RB, Radke J. The effect of disclusion time reduction on maximal clench muscle activity levels. Cranio. 2006;24:156–65. doi: 10.1179/crn.2006.026. [DOI] [PubMed] [Google Scholar]
- 14.Kerstein RB. Reducing chronic masseter and temporalis muscular hyperactivity with computer-guided occlusal adjustments. Compend Contin Educ Dent. 2010;31:530–4, 536, 538. [PubMed] [Google Scholar]
- 15.Kerstein RB, Grundset K. Obtaining bilateral simultaneous occlusal contacts with computer analyzed and guided occlusal adjustments. Quintessence Int. 2001;S32:7–18. [Google Scholar]
- 16.Kerstein RB, Lowe M, Harty M, Radke J. A force reproduction analysis of two recording sensors of a computerized occlusal analysis system. Cranio. 2006;24:15–24. doi: 10.1179/crn.2006.004. [DOI] [PubMed] [Google Scholar]
- 17.Kerstein RB, Radke J. Clinician accuracy when subjectively interpreting articulating paper markings. Cranio. 2014;32:13–23. doi: 10.1179/0886963413Z.0000000001. [DOI] [PubMed] [Google Scholar]
- 18.Maness WL, Benjamin M, Podoloff R, Bobick A, Golden RF. Computerized occlusal analysis: A new technology. Quintessence Int. 1987;18:287–92. [PubMed] [Google Scholar]
- 19.Maness WL. Force movie, A time and force view of occlusal contacts. Compend Contin Educ Dent. 1988;10:404–8. [Google Scholar]
- 20.Haines DE. Neuroanatomy; an Atlas of Structures, Sections, and Systems. 8th ed. Baltimore, MD, USA: Lippincott, William and Wilkins; 2000. pp. 175–193. [Google Scholar]
- 21.Dawson PE. Evaluation, Diagnosis and Treatment of Occlusal Problems. 2nd ed. St. Louis: CV Mosby Co; 1989. pp. 434–56. [Google Scholar]


