Abstract
Objectives. To more clearly articulate, and more graphically demonstrate, the impact of poverty on various health outcomes and social conditions by comparing the poorest counties to the richest counties in the United States and to other countries in the world.
Methods. We used 5-year averages for median household income to form the 3141 US counties into 50 new “states”—each representing 2% of the counties in the United States (62 or 63 counties each). We compared the poorest and wealthiest “states.”
Results. We documented dramatic and statistically significant differences in life expectancy, smoking rates, obesity rates, and almost every other measure of health and well-being between the wealthiest and poorest “states” in the country. The populations of more than half the countries in the world have a longer life expectancy than do US persons living in the poorest “state.”
Conclusions. This analysis graphically demonstrates the true impact of the extreme socioeconomic disparities that exist in the United States. These differences can be obscured when one looks only at state data, and suggest that practitioners and policymakers should increasingly focus interventions to address the needs of the poorest citizens in the United States.
The effects of socioeconomic status on health are well known and thoroughly documented.1–11 Simply put, greater wealth is associated with better health outcomes in most areas, both domestically and internationally. Previous efforts to identify health disparities in the United States based on socioeconomic status have provided important perspectives by using state data, data from broad geographic regions, and data based on race/ethnicity.5,6,9,12 These approaches have been very effective in highlighting health disparities across broad areas and between large population groups. They have been limited, however, in that they normally do not identify the most extreme disparities that may exist within these regions or populations. To better understand health disparities, it has been recognized that there is a value in looking at certain health data at the county level.13–16 Typically, these reports include all counties in the United States or counties that are located in a single state or region.
However, in an effort to better understand, and to more clearly communicate, the actual impact of poverty on health in the United States, we chose to look at the poorest counties in the nation, regardless of where they are geographically located, and compare them with the wealthiest counties. To this end, we stratified all counties and county equivalents on the basis of household income and then compared the wealthiest to the poorest across a range of health and social statistics, to historical trends in the United States, and with comparison countries.
METHODS
We reclassified the 3141 counties in the United States into 50 new “states” by the socioeconomic status indicator of 5-year average median household income. We included a total of 3141 counties in the analysis because these are the county (or county-equivalents) as identified by the County Health Rankings (CHR) National Data.17
Once we had stratified all 3141 counties by 5-year average median household income, we faced the question as to whether we should create our new “states” on the basis of total population (i.e., each new “state” should have the same population) or on total number of counties (i.e., each new “state” should have the same number of counties). A set of analyses (not shown) has indicated that, although population does have a modest impact on health disparities, it is much less impactful than poverty. Using the same number of counties most clearly reflects the impact of extreme poverty on health disparities, so we elected to create our new “states” on the basis of total number of counties. The 2%, or 63 counties, in the United States with the lowest median household income, constitute the poorest “state,” followed by the next 2% of poorest counties, and so on, concluding with the wealthiest “state” comprising the 2% of counties with the highest median household income. Each new “state” had 62 or 63 counties.
Data Sources for Comparison
Data on (1) health behaviors (adult smoking, adult obesity, physical inactivity, and excessive drinking), (2) clinical care (primary care physicians), (3) social and economic environment (high-school graduation, children in poverty, unemployment, and income inequality), and (4) demographics (2011 population, population aged ≥ 65 years, population that is non-Hispanic African American, population that is not proficient in English, population that is female, and population living in rural area) are from the 2015 CHR.17 The CHR aggregates data from many sources to create a resource that includes a variety of health outcome and health factor data. Definitions for all health outcomes and health factors, the data sources, and the source years for the data are at the CHR Web site (http://www.countyhealthrankings.org) within the full data set of the 2015 CHR National Data.
Data on median household income is from the US Census Bureau’s American Community Survey.18 We used 2009 to 2013 American Community Survey 5-year geographic comparison tables to determine median household income for each county. We used the 5-year estimates to reduce sensitivity to outlier years.
Data on 2013 male and female life expectancies for all counties in the United States are from the Institute for Health Metrics and Evaluation US county profiles.19 Data on 2010 male and female life expectancies for the international comparison are from the United Nations Department of Economic and Social Affairs, Population Division.20
Data on US male and female prospective life expectancies from 2020 to 2060 are from the US Census Bureau, Population Division.21 Data on life expectancies from 1900 to 2010 are 3-year estimates from the Centers for Disease Control and Prevention’s National Vital Statistics Division.22
Graphic and Analysis Methods
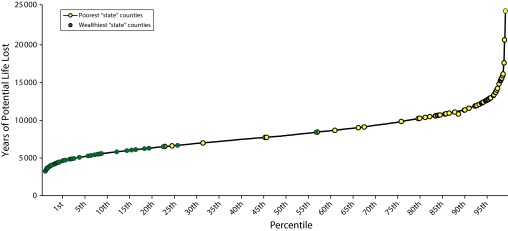
We created a method that allows readers to graphically visualize the health disparities between the wealthiest “state” and the poorest “state.” This visualization is based on a graph that ranks all counties or county equivalents for continuous data measures. Counties that constitute the wealthiest “state” and poorest “state” can then be plotted onto this continuum. This method is useful because it can graphically demonstrate both the comparison between the wealthiest “state” and the poorest “state” and how these “states” compare with the other counties in the nation. Data for this visualization of years of potential life lost are from the 2016 CHR.23
We used the various data sources to compare measures on key dependent variables for the wealthiest “state” with the poorest “state” by using the independent t test on SPSS version 21 (IBM Corp, Somers, NY). This provided the basis for examining the association between socioeconomic status and health outcomes in the United States without allowing geography to conceal the impact of poverty. We also calculated the average for each county in the United States and included it in the graph.
We then compared the male and female life expectancies for the wealthiest “state” and the poorest “state” to those for other countries. Finally, we compared current male and female life expectancies of the wealthiest “state” and poorest “state” to the US life expectancies for men and women from 1900 to 2060 to see where our new states would fall in regard to temporal life expectancies in the United States.
RESULTS
We used years of potential life lost for all US counties to create a continuum from the first percentile (least number of years of potential life lost) to the 99th percentile (greatest number of years of potential life lost), and we plotted the counties that constitute the wealthiest “state” and the counties that constitute the poorest “state” onto this continuum (Figure 1).
FIGURE 1—
Premature Death (Years of Potential Life Lost) of Counties in the Wealthiest “State” and Poorest “State”
Comparisons between the wealthiest “state” and poorest “state” are statistically significant on most measures (Table 1). In the wealthiest “state” the median household income is $89 723, whereas in the poorest “state” it is $24 960, barely above the US Census Bureau’s 2014 poverty threshold24 for a family of 4. There is an average of approximately 362 000 people per county in the wealthiest “state” compared with an average of approximately 14 000 people per county in the poorest “state.” Likewise, only 21% of the population in the wealthiest “state” is living in a rural area compared with 75% of the population in the poorest “state.” The percentage of the population that is non-Hispanic African American in the poorest “state” is 4.5 times that in the wealthiest “state.”
TABLE 1—
Social and Demographic Descriptors: Wealthiest “State,” Poorest “State,” and US Average
| Variable | Wealthiest “State” (n = 63), Mean ±SD or % | Poorest “State” (n = 63), Mean ±SD or % | P | US Average (n = 3141), Mean or % |
| Demographics | ||||
| Median household income,a,b $ | 89 722.92 ±9715.9 | 24 959.56 ±1825.4 | < .01 | 45 922.02 |
| 2011 population estimate,c no. | 36 1707 ±43 2011 | 14 173 ±10 547 | < .01 | 10 0646 |
| Population aged ≥ 65 yc | 12.4 | 15.5 | < .01 | 17.2 |
| Population that is non-Hispanic African Americanc | 7.9 | 37.0 | < .01 | 8.9 |
| Population not proficient in Englishc | 3.0 | 2.2 | .29 | 1.8 |
| Population femalec | 50.0 | 48.9 | .09 | 49.9 |
| Population living in rural areac | 21.3 | 75.3 | < .01 | 58.6 |
| Health outcomes | ||||
| Female life expectancy,a,d y | 83.08 ±1.43 | 76.00 ±1.74 | < .01 | 79.98 |
| Male life expectancy,a,d y | 79.30 ±1.69 | 69.75 ±2.23 | < .01 | 75.04 |
| Health behaviors | ||||
| Adult smokinga,c | 13.8 | 27.6 | < .01 | 21.3 |
| Adult obesityc | 24.4 | 36.7 | < .01 | 30.7 |
| Physical inactivityc | 19.7 | 33.2 | < .01 | 27.0 |
| Excessive drinkingc | 18.0 | 14.0 | .10 | 16.5 |
| Clinical care: primary care physiciansa,c | 1631:1 | 3961:1 | 2564:1 | |
| Social and economic environment | ||||
| High-school graduationa,c | 88.7 | 79.0 | < .01 | 83.0 |
| Children in povertyc | 8.9 | 48.4 | < .01 | 24.6 |
| Unemploymentc | 5.6 | 12.2 | < .01 | 7.3 |
| Income inequalityc | 3.98 ±0.63 | 5.56 ±0.67 | < .01 | 4.48 |
The wealthiest “state” achieved better outcomes in nearly every comparison. Female residents of the wealthiest “state” have an average life expectancy of 83 years, 7.08 years longer than those in the poorest “state.” Male residents of the wealthiest “state” have a life expectancy of 79.3 years, nearly a decade longer than the average of 69.8 years in the poorest “state.” Adults in the poorest “state” have double the smoking prevalence of those in the wealthiest “state” and are 50% and 69% more likely, respectively, to be obese and physically inactive. Those in the wealthiest “state” might be more likely to drink excessively, though this finding was not statistically significant. The wealthiest “state” also has a higher high-school graduation rate and less than half the unemployment rate of the poorest “state.” There are more than twice as many persons per primary care physician in the poorest “state” compared with the wealthiest “state.”
Counties included in our poorest “state” come from 13 actual states (AL, AR, GA, IL, KY, LA, MS, OK, SC, SD, TN, TX, and WV), and the counties in the wealthiest “state” come from 20 actual states (AK, CA, CO, CT, GA, IL, IN, KY, MD, MA, MN, OH, NJ, NM, NY, PA, UT, TN, TX, and VA). There are 5 states, therefore, that have contributed 1 or more counties to both the poorest “state” and the wealthiest “state” (GA, IL, KY, TN, and TX).
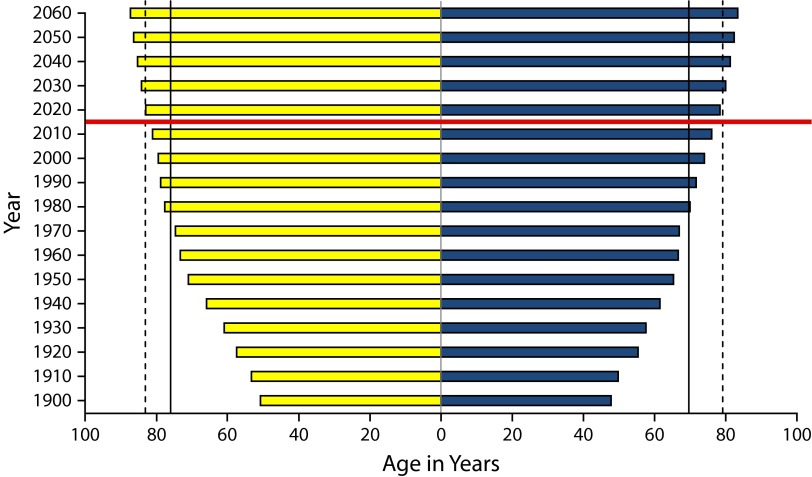
When we compared male and female life expectancies in the wealthiest “state” and the poorest “state” to the US Census temporal trend in US life expectancies from 1900 to 2060 (Figure 2),21,22 male and female life expectancy in the poorest “state” would be about the equivalent of life expectancy in the United States, overall, in approximately 1980 and 1975, respectively. The national male and female life expectancy in the United States, overall, is not expected to reach the current levels of the wealthiest “state” until the mid-2020s and 2020, respectively, assuming that current trends continue. This means that the poorest “state” is between 40 and 50 years behind the life expectancy currently achieved by the wealthiest “state.”
FIGURE 2—
Projected and Actual US Male and Female Life Expectancies From 1910 to 2060 With Poorest and Wealthiest “States’” Current Life Expectancies
Note. Blue bars represent male life expectancy and yellow bars represent female life expectancy. Bars above the red line are projected life expectancies, and bars below the red line are actual life expectancies. Solid vertical lines represent the poorest “state’s” current life expectancy, and the dotted vertical lines represent the wealthiest “state’s” current life expectancy.
Source. US Census Bureau21 and US Department of Health and Human Services.22
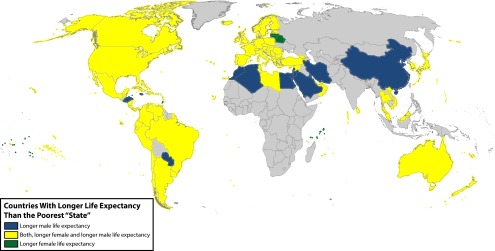
When compared with the 222 countries with appropriate data,20 life expectancy for the wealthiest “state” would rank eighth and 25th, respectively, for men and women. Life expectancy for the poorest “state,” however, would rank 123rd and 116th for men and women, respectively, meaning that more than half of the countries in the world have a longer life expectancy than the poorest counties in the United States. Figure 3 shows, in yellow, those countries with a longer life expectancy for both men and women, when compared with people living in our poorest “state” (including the United States’ overall life expectancy). In addition, the countries in blue and green have a longer life expectancy for men and women, respectively. Islands too small to be pictured in Figure 3 are represented by points and coded by their respective color.
FIGURE 3—
Comparison of Poorest “State’s” Male and Female Life Expectancies to International Life Expectancies
Note. Poorest “state’s” male and female life expectancies drawn from 2013 data. International life expectancies drawn from 2010 data.
Source. Institute for Health Metrics and Evaluation19 and United Nations Department of Economic and Social Affairs.20
DISCUSSION
In this study, we used a simple but powerful approach to better understand the health impact of socioeconomic disparities in the United States. By using median household income data to create 50 new “states,” we have identified health disparities that have been largely masked by past state-level evaluations. We also believe that we have identified an effective mechanism to more easily demonstrate the impact of poverty on health for policymakers and, indeed, all persons living in the United States.
This study demonstrates that looking at state-level data hides the impact of socioeconomic disparities on both the best-off and worst-off counties in the United States. Comparing the poorest and wealthiest “states” and also comparing these “states” to countries across the world highlights the vast disparities that exist within the United States.
Public Health Implications
At the most basic level, this study suggests that public health policymakers, public health professionals, funders, and others with an interest in improving the overall health status of the United States should increasingly focus on the needs of its poorest counties. This study suggests that state-level data, in aggregate, may be a less useful indicator of public health need than local county data, and that statewide public health programs may be less effective than more targeted programs.
This study should provide significant incentive to federal, state, and local officials, and to foundations and other funding agencies, to increasingly focus on the poorest counties and, perhaps, less on statewide interventions. With limited and finite resources, methods of pinpointing the poorest counties can assist in the allocation of resources and programs to those communities that are in the greatest need. In addition, the development of local-level interventions that take into account the culture and community characteristics in their design and implementation may have a greater impact on reversing the ill effects of poverty on health. The challenges facing the United States’ poorest “state” are, of course, multiple and complex. It is abundantly clear that special emphasis should be given to programs and interventions that bring together health care providers, educators, economic development programs, and many other key community partners to improve the quality of life in these regions, creating resilient communities.
Although it is beyond the scope or purview of this study, the fact that there are 5 states that have counties in both the wealthiest “state” and the poorest “state” suggests that, at least to some degree, some of the challenges associated with poverty in the United States are related to factors associated with unequal distribution of resources within states, as opposed to simple lack of resources.
From a data standpoint, this study strongly suggests that current data sources are inadequate to really understanding the greatest health risks in the United States. Ultimately, the most useful data will be those that are largely focused on identifying groups of individuals and families who are at the lowest end of the socioeconomic ladder, regardless of where they are physically located.
Study Limitations
This analysis demonstrates the dramatic health impact of socioeconomic disparities in the United States. However, as dramatic as these disparities are, this analysis actually underestimates the differences in health status between the wealthiest and the poorest persons in the United States. This is because there remain pockets of poverty in the wealthiest counties while, at the same time, a significant number of people in the poorest counties are not living in poverty. Specifically, 8.9% of the children in the wealthiest “state” live below the federal poverty line, while about half of the children in the poorest “state” live above the federal poverty line. This suggests that the health disparities between the wealthiest and the poorest US persons are even greater than those suggested by this analysis.
This cross-sectional study does not allow for analysis of causality (i.e., low income leads to poor health vs poor health leads to lower income). Future research should attempt to identify causal pathways between income and health outcomes. The data used for this study are also somewhat limited in the fact that they come from multiple different sources collected over different time periods. Although this is an important factor to acknowledge, it probably has a relatively limited impact on the conclusions of this study, as these differences exist equally in both the wealthiest “state” and the poorest “state.”
Future research will be needed to better understand whether the factors relating poverty to poor health outcomes are stable over time, or whether there are counties that have seen significant improvement (or deterioration) in health status despite relatively consistent socioeconomic conditions. In addition, it will be important to identify counties that have seen significant changes in the socioeconomic status, and to follow these counties to see if health status begins to change and, if so, over what period of time. It will be equally important to see whether unique local factors, such as cost of living, mitigate the impact of poverty on health in the United States.
Future research should more comprehensively attempt to separate the impacts of population and poverty on health. There are significant population differences between the wealthiest “state” and poorest “state,” an average of 361 707 and 14 173 persons per county, respectively. It is difficult to separate out the impact of population compared with that of poverty because levels of rurality have been shown to be inversely related to socioeconomic status.25 Though our preliminary analyses (not shown) strongly suggest that poverty exerts a greater impact on health than does population, further research should be conducted on this issue.
Future research should also look at outcome factors other than premature mortality (notably morbidity statistics) and determine the impact of socioeconomic conditions on these factors. In addition, future work should attempt to understand “causality”—developing a better understanding of the relative impact of factors such as smoking, obesity, and others on ultimate health outcomes.
Conclusions
We believe that creating 50 new “states”—organized by median household income, instead of geographic locality—provides a highly effective mechanism to help public health workers and, more importantly, policymakers and the general public both understand and communicate the impact of poverty on health in the United States.
This study should remind all persons living in the United States that poverty has a remarkable effect on health, and that this impact is found across the country, not just in those states normally thought of as being “poor.” It should also remind policymakers that efforts to improve health will be dependent, in large part, on efforts to address economic inequality. We posed the hypothetical question, “What if we redefined America, not by geography or race, but by socioeconomic status,” and the results should be deeply disturbing to all persons in the country. Women and men in the poorest “state” will live, on average, 7 to 10 fewer years than their counterparts in the wealthiest “state,” and in almost every factor compared between the wealthiest and poorest “state,” those living in the wealthiest “state” achieved dramatically better outcomes. Life expectancy in the poorest “state” falls below that of more than half the countries in the world, meaning that, in essence, there are several developing countries hidden within the borders of the United States—regions defined, in this case, by poverty. The “state” of poverty in this country is dramatic and deeply disturbing.
ACKNOWLEDGMENTS
The authors would like to acknowledge the geographic information system support of Amy Poole (who developed the final map included in this article) and Winn Ketchum (who both developed maps that were not used in this article of the distribution of poor counties in the United States) and to Rob Pack who provided both conceptual and editorial assistance.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed for this study because analysis of de-identified, publicly available data does not constitute human research.
Footnotes
See also Galea and Vaughan, p. 17.
REFERENCES
- 1. The John D. and Catherine T. MacArthur Foundation. Reaching for a Healthier Life: Facts on Socioeconomic Status and Health in the US. 2007. Available at: http://www.macses.ucsf.edu/downloads/Reaching_for_a_Healthier_Life.pdf. Accessed August 11, 2015.
- 2.Biggs B, King L, Basu S, Stuckler D. Is wealthier always healthier? The impact of national income level, inequality, and poverty on public health in Latin America. Soc Sci Med. 2010;71(2):266–273. doi: 10.1016/j.socscimed.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 3. Marmot M. Status Syndrome. London, England: Bloomsbury; 2004.
- 4.Frank JW, Cohen R, Yen I, Balfour J, Smith M. Socioeconomic gradients in health status over 29 years of follow-up after midlife: the Alameda County study. Soc Sci Med. 2003;57(12):2305–2323. doi: 10.1016/j.socscimed.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Geronimus AT, Bound J, Waidmann TA, Hillemeier MM, Burns PB. Excess mortality among Blacks and Whites in the United States. N Engl J Med. 1996;335(21):1552–1558. doi: 10.1056/NEJM199611213352102. [DOI] [PubMed] [Google Scholar]
- 6.Geronimus AT, Bound J, Waidmann TA. Poverty, time, and place: variation in excess mortality across selected US populations, 1980–1990. J Epidemiol Community Health. 1999;53(6):325–334. doi: 10.1136/jech.53.6.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hahn RA, Eaker ED, Barker ND, Teutsch SM, Sosniak WA, Krieger N. Poverty and death in the United States. Int J Health Serv. 1996;26(4):673–690. doi: 10.2190/967K-LC4F-DU66-W5P9. [DOI] [PubMed] [Google Scholar]
- 8.Isaacs SL, Schroeder SA. Class—the ignored determinant of the nation’s health. N Engl J Med. 2004;351(11):1137–1142. doi: 10.1056/NEJMsb040329. [DOI] [PubMed] [Google Scholar]
- 9.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marmot M. Public health social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 11.Marmot M. The influence of income on health: views of an epidemiologist. Health Aff (Millwood) 2002;21(2):31–46. doi: 10.1377/hlthaff.21.2.31. [DOI] [PubMed] [Google Scholar]
- 12.Murray CJL, Kulkarni SC, Michaud C et al. Eight Americas: investigating mortality disparities across races, counties, and race–counties in the United States [erratum in PLoS Med. 2006;3(12):e545] PLoS Med. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dwyer-Lindgren L, Flaxman AD, Ng M, Hansen GM, Murray CJL, Mokdad AH. Drinking patterns in US counties from 2002 to 2012. Am J Public Health. 2015;105(6):1120–1127. doi: 10.2105/AJPH.2014.302313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dwyer-Lindgren L, Freedman G, Engell RE et al. Prevalence of physical activity and obesity in US counties, 2001–2011: a road map for action. Popul Health Metr. 2013;11(1):7. doi: 10.1186/1478-7954-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Casper M, Kramer MR, Quick H, Schieb LJ, Vaughan AS, Greer S. Epidemiology and prevention changes in the geographic patterns of heart disease mortality in the United States 1973 to 2010. Circulation. 2016;133(12):1171–1180. doi: 10.1161/CIRCULATIONAHA.115.018663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D’Angelo H, Ammerman A, Gordon-Larsen P, Linnan L, Lytle L, Ribisl KM. Sociodemographic disparities in proximity of schools to tobacco outlets and fast-food restaurants. Am J Public Health. 2016;106(9):1556–1562. doi: 10.2105/AJPH.2016.303259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.University of Wisconsin Population Health Institute. County Health Rankings: 2015 County Health Rankings National Data. 2015. Available at: http://www.countyhealthrankings.org. Accessed May 30, 2015.
- 18.US Census Bureau. American Community Survey, income in the past 12 months (in 2013 inflation-adjusted dollars), 2009–2013 American Community Survey 5-year estimates, Table S1901. Available at: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_13_5YR_S1901&prodType=table. Accessed April 10, 2015.
- 19.Institute for Health Metrics and Evaluation. US county profiles. 2015. Available at: http://www.healthdata.org/us-county-profiles. Accessed May 11, 2015.
- 20.United Nations Department of Economic and Social Affairs. Table 2a—life expectancy. 2012. Available at: http://unstats.un.org/unsd/demographic/products/socind. Accessed July 22, 2015.
- 21.US Census Bureau Population Division. Table 10. Projected life expectancy at birth by sex, race, and Hispanic origin for the United States: 2015 to 2060 (NP2012-T20). 2012. Available at: https://www.census.gov/population/projections/files/summary/NP2012-T10.csv. Accessed August 6, 2015.
- 22.US Department of Health and Human Services. Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. Table 21. Life expectancy by age, race, and sex: death registration states, 1900–1902 to 1919–21, and United States, 1929–31 to 2010. 2014. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr63/nvsr63_07.pdf. Accessed November 3, 2016. [DOI] [PubMed]
- 23.University of Wisconsin Population Health Institute. County Health Rankings: 2016 County Health Rankings National Data. 2016. Available at: http://www.countyhealthrankings.org. Accessed March 24, 2016.
- 24.US Census Bureau. Poverty. Poverty thresholds by size of family and number of children: 2014. 2015. Available at: https://www.census.gov/hhes/www/poverty/data/threshld. Accessed August 10, 2015.
- 25.Singh GK, Siahpush M. Widening rural–urban disparities in life expectancy, U.S., 1969–2009. Am J Prev Med. 2014;46(2):e19–e29. doi: 10.1016/j.amepre.2013.10.017. [DOI] [PubMed] [Google Scholar]