Abstract
Objectives. To evaluate the impact of the partial repeal of Michigan’s universal motorcycle helmet law on helmet use, fatalities, and head injuries.
Methods. We compared helmet use rates and motorcycle crash fatality risk for the 12 months before and after the April 13, 2012, repeal with a statewide police-reported crash data set. We linked police-reported crashes to injured riders in a statewide trauma registry. We compared head injury before and after the repeal. Regression examined the effect of helmet use on fatality and head injury risk.
Results. Helmet use decreased in crash (93.2% vs 70.8%; P < .001) and trauma data (91.1% vs 66.2%; P < .001) after the repeal. Although fatalities did not change overall (3.3% vs 3.2%; P = .87), head injuries (43.4% vs 49.6%; P < .05) and neurosurgical intervention increased (3.7% vs 6.5%; P < .05). Male gender (adjusted odds ratio [AOR] = 1.65), helmet nonuse (AOR = 1.84), alcohol intoxication (AOR = 11.31), intersection crashes (AOR = 1.62), and crashes at higher speed limits (AOR = 1.04) increased fatality risk. Helmet nonuse (AOR = 2.31) and alcohol intoxication (AOR = 2.81) increased odds of head injury.
Conclusions. Michigan’s helmet law repeal resulted in a 24% to 27% helmet use decline among riders in crashes and a 14% increase in head injury.
Motorcycle crashes cause an increasingly disproportionate share of fatal and nonfatal unintentional motor vehicle crash injuries. Between 1997 and 2014, US motorcycle crash fatalities more than doubled, increasing to more than 4000 deaths annually.1 Furthermore, motorcyclists represented 14% of all traffic fatalities in 2014, while accounting for only 3% of registered vehicles.1 Crash-involved motorcyclists are 27 times more likely to be killed and 5 times more likely to be nonfatally injured than are crash-involved passenger vehicle occupants.1 Head injury remains the leading cause of fatality2 and a leading cause of serious nonfatal injury among the 30 000 crash-involved motorcyclists admitted from emergency departments (EDs) annually.3
Helmet use is an effective prevention measure to decrease motorcycle-related head injuries.2,4–6 A Cochrane review found that helmets decrease the risks for fatal and nonfatal head injuries by 69% and overall fatalities by 42%.7 Furthermore, the National Highway Traffic Safety Administration estimates that unhelmeted motorcyclists are 40% more likely to suffer fatal head injuries and 15% more likely to suffer nonfatal head injuries than helmeted motorcyclists in a crash.8 Among hospital-based samples, unhelmeted riders have higher rates of head and spine injuries, higher injury severity scores, and worse medical outcomes, including higher rates of disability and mortality than helmeted riders.4,9 Unhelmeted crash-involved riders also incur higher medical costs, with one study finding that the mean total hospital charges were almost double.10
Universal motorcycle helmet laws (UHLs) increase helmet use among riders,6,11 and are associated with fewer head injuries, lower injury severity, and reduced fatality rates after crashes.12–14 Despite their effectiveness, only 19 states currently have UHLs, with many states weakening or repealing their UHLs after Congress revoked federal authority to withhold highway funding for states that do not maintain a UHL in 1975.11 On April 13, 2012, Michigan became the first state since 2003 to weaken its UHL, replacing it with a partial law allowing motorcyclists (aged ≥ 21 years) to ride unhelmeted if they have a valid motorcycle license and a $20 000 vehicle insurance supplement.
Although previous repeals have been associated with decreased helmet use and increased rates of head injury and fatality,11,15–20 few studies have analyzed Michigan’s partial UHL repeal.20–22 Among motorcyclists who died on the scene within the catchment area of a single western-Michigan trauma center, the proportion that was unhelmeted increased from 7% during a 7-month period in 2011 to 28% during the same period following the repeal.22 Accounting for changes in policy limits, medical payment insurance claim severity for Michigan motorcyclists has increased 22% relative to neighboring states.21 However, no previous studies have examined the effects of Michigan’s repeal on head injuries or fatalities statewide.
In addition, previous studies have been limited to population-level fatality rates from crash records,16–18 or fatal and nonfatal injury rates within a single hospital.19,20 Previous hospital-based studies have not adjusted for potentially important crash-related factors such as speed limit (i.e., proxy for vehicle speed) or police-reported helmet use. Furthermore, few studies have captured data across multiple phases of care (e.g., data from the on-scene crash and trauma registry data) or examined both a statewide database of fatalities and serious nonfatal head injury with statewide trauma registry data. Such an approach allows for a comprehensive examination of the statewide impact of the motorcycle helmet repeal and the relative influences of crash-related factors on rider injuries. The objective of the current study was to investigate the impact of Michigan’s UHL repeal on fatalities and head injuries following a motorcycle crash by using an approach that combined on-scene crash data with hospital-based trauma registry data. Secondly, we explored the impact of the repeal on helmet use, and the factors associated with an increased risk for motorcycle fatalities and head injuries. Results will extend the literature and inform public health policy.
METHODS
In this retrospective study, we conducted 2 analyses characterizing the impact of the UHL repeal. First, we examined motorcycle crash fatalities by using a statewide data set of police-reported crashes capturing both in- and out-of-hospital fatalities. Second, we examined head injuries among patients hospitalized at Michigan trauma centers by using a data set formed by linking police-reported crashes and statewide trauma registry data. Of note, helmet use was examined among both data sets. Both analyses examined data from the 12 months before and after the repeal.
Data Sources
We identified fatalities and head injuries from 2 statewide data sets. We identified fatalities by using police-reported crash data (i.e., a data set recording all crashes occurring on public roadways that result in injury or property damage greater than $1000) from the Michigan Criminal Justice Information Center. These data include crash location and circumstances, and vehicle and operator or passenger characteristics.
We obtained data on head injuries from a comprehensive data set of all hospitalized trauma patients created by linking the police-reported crash data set outlined previously to a statewide trauma registry. We obtained registry data from the Michigan Trauma Quality Improvement Program (MTQIP), a hospital-based collaborative quality initiative sponsored by Blue Cross/Blue Shield. The MTQIP aggregates de-identified data on patients with an Injury Severity Score (ISS) greater than 5, a hospital length of stay (LOS) of 1 day or more, or those who die at participating trauma centers. The MTQIP includes risk-adjusted outcomes and quality-of-care indicators. Data are validated through annual interrater reliability audits conducted by the clinical coordinating center (target discrepancy rate < 5%).23 Twenty-three hospitals were included, representing all American College of Surgeons Level-1 (n = 9) or Level-2 (n = 14) Michigan trauma centers.
Both the crash and trauma registry data sets were limited to include operators or passengers (aged ≥ 16 years) riding a motorcycle in Michigan who were involved in either a police-reported motorcycle crash or evaluated and treated at a Michigan trauma center for a traumatic injury between April 12, 2011, and April 12, 2013. For the head injury analysis, motorcycle riders involved in crashes and treated at hospitals, but not injured severely enough to require trauma system activation, were not included because they are not routinely captured by the MTQIP data set.
Data Set Variables and Outcome of Interest
Primary outcome measures were fatality and head injury. We identified fatalities within the police-reported crash data set, which includes an on-scene officer-reported assessment of injury using the KABCO scale (K: fatal injury; A: incapacitating injury; B: nonincapacitating injury; C: possible injury; O: uninjured, property damage only).24 All fatalities occurring on-scene or within 30 days of the crash are captured. We identified head injuries within the linked hospital trauma data set according to the Centers for Disease Control and Prevention traumatic brain injury definition.25 This includes an International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM)26 diagnosis of any of the following: (1) fracture of the vault or base of the skull (800.0–801.9); (2) multiple skull fractures (803.0–804.9); (3) intracranial injury including concussion, contusion, laceration, or hemorrhage (850.0–854.1); or (4) a diagnosis of open wound of the head (873.0–873.9) in an expired patient. In addition, we included a diagnosis of head injury, unspecified (959.01).
The crash data set also includes variables on rider sociodemographics (e.g., age, gender), crash location (e.g., intersection) and time (day, time), rider position (operator or passenger), helmet use (yes or no), posted speed limit (miles per hour), operator alcohol intoxication (blood alcohol content [BAC] ≥ 80 mg/dL), state of motorcycle or vehicle registration, and motorcycle type. We used posted speed limit as a surrogate for crash speed. For passengers, BAC is reflective of the operator for the motorcycle that they were riding during the crash.
The trauma registry includes variables on patient sociodemographics (age, gender, race, medical insurance), date and time of the ED treatment or hospitalization, ED or hospital disposition, and helmet use. In-hospital mortality included an ED or hospital disposition of “death” or “expired.” The BAC was measured by using serum analysis (mg/dL) upon arrival to assess for alcohol intoxication (BAC ≥ 80 mg/dL). Hospital service utilization was measured by using hospital or intensive care unit (ICU) LOS, ventilator status, and need for neurosurgical intervention. We calculated ICU and hospital LOS as the cumulative number of full or partial days in the ICU and hospital, respectively. The LOS at a referring hospital before transport to a trauma center was unavailable. Neurosurgical intervention was a composite measure, defined by using ICD-9-CM codes for procedures used to treat severe brain injuries including craniotomy or craniectomy, ventriculostomy, insertion of an intracranial monitor, and use of cerebral oxygen monitoring.
Additional injury severity measures include the Abbreviated Injury Scale (AIS) and ISS. The AIS27 is an anatomically based coding system ranking injury severity for each body region (head/neck, face, thorax/spine, abdomen/pelvis, upper/lower extremity, and unspecified/external) with a 6-level ordinal scale, from AIS-1 (minor) to AIS-6 (severe untreatable injuries). The ISS28 is a cumulative severity measure derived from the sum of the squares of the 3 most severely injured AIS regions (range = 1–75). A maximal AIS of 6 (i.e., unsurvivable) in any region defaults to an ISS of 75.
Probabilistic Linkage of Crash and Trauma Registry Data Sets
We used probabilistic linkage (Centers for Disease Control and Prevention LinkPlus Software), a method for matching records from disparate data sets based on common variables when unique identifiers are unavailable, in this study to link registry and crash data. Probabilistic linkage has been previously validated for use among EMS and trauma populations.29 For this study, we identified 4 linking variables (age, gender, crash time and date, time and date of ED arrival). We used injury date as a blocking variable to constrain linkages to records with exact matches on certain parameters (e.g., age, gender).
We assigned variables match weights (i.e., ratio of the probability for a “true match” to the probability of an “unmatch”). We chose the final cumulative match–weight cutoff to maximize successful matches while minimizing registry cases linked to multiple crash records. We considered high-probability matches with a cumulative match weight above the preset threshold “true matches” and retained these, whereas we excluded those below the match weight. We manually reviewed registry cases with multiple crash matches to resolve discrepancies. Match rates (68.8%) were similar to those (40%–70%) reported for a comparable approach (i.e., fixed cutoff) linking crash and hospital records through the Crash Outcome Data Evaluation System Program.30
Data Analysis
We calculated descriptive statistics for all variables. The on-scene police report of helmet use was the primary helmet variable for analyses. Among cases in the linked data set in which on-scene helmet use was missing (n = 64; 5.5%), we used the trauma registry measure. Helmet use was congruent between data sets in 88.2% of cases in which both were available.
Analysis proceeded in 2 stages. First, we compared fatalities before (April 13, 2011, to April 12, 2012) and after (April 13, 2012, to April 12, 2013) the UHL repeal by using the police-reported crash data set. We used the χ2 test and t test to evaluate bivariate associations before and after the repeal. Second, we repeated the analysis examining head injuries among the linked data set. Two multivariate models examined the association of multiple covariates with fatalities in the crash data set and head injuries in the linked data set. We chose covariates on the basis of theory and bivariate significance. Of note, alcohol intoxication for the fatality analysis was from the police crash data, and for the head injury analysis it was from the hospital data.
RESULTS
During the study period, we identified 8126 crash-involved riders (operators or passengers aged ≥ 16 years) in the police-reported crash data set and 1698 hospitalized patients in the trauma registry. In the crash-involved data set (n = 8126), 11.0% (n = 891) of cases were missing data for key variables. Individually, none of the regression variables were missing more that 12% of the data, with most missing less than 3%; therefore, we considered missingness negligible and we excluded missing cases from analysis. In the final crash-involved sample (n = 7235), mean rider age was 42.2 years, 85.7% were male, 92.0% were the operator, and 95.0% were riding a Michigan-registered motorcycle (Table 1). Overall, 33.7% were riding a cruiser during the crash, 23.0% a touring motorcycle, 19.4% a sport motorcycle, and 4.5% a standard motorcycle or moped. There were no differences between the sociodemographics of the crash-involved sample before and after the UHL repeal, with the exception of age; the postrepeal cohort was slightly younger. Mean speed limit was also noted to be lower after the repeal (P < .05). Alcohol intoxication (BAC ≥ 80 mg/dL) and state of motorcycle registration did not vary before and after the repeal.
TABLE 1—
Crash-Involved Motorcyclist (Operators and Passengers) Characteristics for the 12 Months Before (April 13, 2011, to April 12, 2012) and 12 Months After (April 13, 2012, to April 12, 2013) the Partial Repeal of Michigan’s Universal Motorcycle Helmet Law
| Characteristic | Before Repeala (n = 3594; 49.7%), Mean ±SD or No. (%) | After Repealb (n = 3641; 50.3%), Mean ±SD or No. (%) | OR (95% CI) |
| Sociodemographics | |||
| Age, y | 42.5 ±14.7 | 41.8 ±15.0 | 1.00 (1.00, 1.01)c |
| Male gender | 3087 (85.9) | 3111 (85.4) | 1.04 (0.91, 1.18) |
| Position: operator | 3311 (92.1) | 3346 (92.9) | 1.03 (0.87, 1.22) |
| Crash characteristics | |||
| Speed limit, mph | 45.6 ±12.7 | 44.8 ±12.5 | 1.01 (1.00, 1.01)d |
| Helmet use: yes | 3369 (93.7) | 2587 (71.1) | 6.10 (5.24, 7.11) |
| Crash at intersection | 1134 (31.6) | 1219 (33.5) | 0.92 (0.83, 1.01) |
| Medical characteristics: alcohol intoxication (BAC ≥ 80 mg/dL) | 90 (2.5) | 114 (3.1) | 0.80 (0.60, 1.05) |
| Health-related outcomes | |||
| Fatal injuries | 117 (3.3) | 116 (3.2) | 1.02 (0.79, 1.33) |
| Serious injuries, KAe | 710 (19.8) | 743 (20.4) | 0.96 (0.86, 1.08) |
| All fatal and nonfatal injuries, KABCe | 2832 (78.8) | 2873 (78.9) | 0.99 (0.89, 1.11) |
Notes. BAC = blood alcohol content; CI = confidence interval; OR = odds ratio.
April 13, 2011, to April 12, 2012.
April 13, 2012, to April 12, 2013.
OR for age without rounding is 1.00314 (95% CI = 1.00003, 1.00625).
OR for speed limit without rounding is 1.00468 (95% CI = 1.00468, 1.00837).
KABCO scale = K: fatal injury; A: incapacitating injury; B: nonincapacitating injury; C: possible injury; O: uninjured, property damage only.
Among trauma registry patients (n = 1698), we were able to probabilistically link 1164 to the statewide crash data set (match rate 68.6%). Linkage rates did not vary before and after the repeal. Among linked cases (n = 1164), 6.0% (n = 70) were missing data for key variables. We excluded cases after comparisons revealed no evidence of missing data bias. In the final hospital sample (n = 1094), mean age was 44.3 years, 87.9% were male, and 88.2% were White (Table 2). The majority maintained private health insurance (78.0%), with less than 19% requiring a public payer or lacking insurance (i.e., self-pay). Similar to the crash data, nearly all hospital trauma sample patients were riding Michigan-registered motorcycles (96.7%). With the exception of gender, there were no before–after repeal differences in sociodemographics, alcohol intoxication, or mean speed limits of the trauma sample (Table 2). There were also no differences in the proportion reporting a Michigan motorcycle registration before and after the repeal (96.4% vs 96.9%; P = .61).
TABLE 2—
Hospitalized Trauma Patient Characteristics for the 12 Months Before (April 13, 2011, to April 12, 2012) and 12 Months After (April 13, 2012, to April 12, 2013) the Partial Repeal of Michigan’s Universal Helmet Law
| Characteristic | Before Repeala (n = 537; 49.1%), Mean ±SD or No. (%) | After Repealb (n = 557; 50.9%), Mean ±SD or No. (%) | OR (95% CI) |
| Sociodemographics | |||
| Age, y | 44.1 ±14.7 | 44.4 ±14.3 | 1.00 (0.99, 1.01) |
| White race | 471 (87.7) | 494 (88.7) | 0.91 (0.63, 1.31) |
| Male gender | 484 (90.1) | 478 (85.8) | 1.51 (1.04, 2.19) |
| Insurance status | |||
| Public payer or self-pay | 92 (17.1) | 108 (19.4) | 0.86 (0.63, 1.17) |
| Private payer | 428 (79.7) | 425 (76.3) | 1.22 (0.92, 1.63) |
| Otherc | 16 (3.0) | 16 (2.9) | 1.04 (0.51, 2.10) |
| Crash characteristics | |||
| Speed limit, mph | 46.3 ±12.6 | 46.4 ±11.6 | 1.00 (0.99, 1.01) |
| Helmet use: yes | 489 (91.1) | 369 (66.2) | 5.19 (3.68, 7.33) |
| Operator: yes | 506 (94.2) | 509 (91.4) | 1.54 (0.96, 2.46) |
| Crash at Intersection: yes | 153 (28.5) | 154 (27.6) | 1.04 (0.80, 1.36) |
| Medical characteristics | |||
| Alcohol intoxication (BAC ≥ 80 mg/dL) | 93 (17.3) | 111 (19.9) | 0.84 (0.62, 1.14) |
| Injury Severity Score | 15.3 ±11.6 | 15.4 ±11.0 | 1.00 (0.99, 1.01) |
| Health-related outcomes | |||
| Head injury | 233 (43.4) | 276 (49.6) | 0.78 (0.62, 0.99) |
| In-hospital mortality | 16 (3.0) | 12 (2.2) | 1.40 (0.65, 2.98) |
| Hospital service utilization | |||
| Hospital admission | 446 (83.1) | 445 (79.9) | 1.23 (0.91, 1.68) |
| Intubation or ventilator: yes | 94 (17.5) | 113 (20.3) | 0.83 (0.62, 1.13) |
| ICU admission: yes | 133 (24.8) | 162 (29.1) | 0.80 (0.61, 1.05) |
| ICU LOSd | 6.3 ±7.4 | 6.1 ±6.9 | 1.00 (0.97, 1.04) |
| Neurosurgical intervention | 20 (3.7) | 36 (6.5) | 0.56 (0.32, 0.98) |
Notes. BAC = blood alcohol content; CI = confidence interval; ICU = intensive care unit; LOS = length of stay; OR = odds ratio.
April 13, 2011, to April 12, 2012.
April 13, 2012, to April 12, 2013.
Other insurance status includes workman’s compensation and nonbilled cases.
ICU LOS was calculated as mean number of days in ICU and calculated only among those requiring ICU care.
Effects of Repeal on Helmet Use
Among crash-involved riders, helmet use decreased 24% following the UHL repeal (93.7% vs 71.1%; P < .001; Table 1), with lowest postrepeal rates noted among alcohol-impaired riders (83.8% vs 44.7%; P < .001). In addition, although helmet use decreased among both adult (aged ≥ 21 years; 94.1% vs 70.9%; P < .001) and adolescent (aged 16–20 years; 88.8% vs 72.7%; P < .001) riders, we observed helmet use to decrease more sharply among adults than adolescents (P < .01). Furthermore, although helmet use decreased among both passengers (97.5% vs 71.9%; P < .001) and operators (93.4% vs 71.0%; P < .001), we observed helmet use to decrease more sharply among passengers (P < .05). We noted no changes in helmet use when we examined by gender or state of motorcycle registration.
Among hospitalized patients, helmet use decreased 27% following the repeal (91.1% vs 66.2%; P < .001; Table 2). Similar to the crash data, the lowest postrepeal rates were among alcohol-impaired patients (78.5% vs 51.4%; P < .001). Helmet use decreased significantly among both male and female patients, but decreased more sharply among female (98.1% vs 62.0%; P < .001) than male (90.3% vs 66.9%; P < .001) patients (P < .05). Furthermore, although helmet use decreased among those with private health insurance (93.0% vs 66.4%; P < .001) and those with public payer or no health insurance (83.7% vs 66.7%; P < .05), helmet use decreased more sharply among those with private insurance (P < .05). We identified no race or age differences in helmet use.
Effects of Repeal on Fatalities
The statewide fatality rate (Table 1) did not change significantly following the UHL repeal (3.3% vs 3.2%; P = .87). The fatality rate among nonhelmeted crash-involved riders increased nominally following the repeal from 4.4% to 5.6% (P = .49); however, it was notably 1.9 times higher than among helmeted riders (5.4% vs 2.8%; P < .001). Furthermore, among helmeted crash-involved riders, the fatality rate decreased significantly following the repeal (3.2% vs 2.2%; P = .02). Multivariate modeling (Table 3) found that risk factors for a fatal motorcycle injury among crash-involved riders included male gender, helmet nonuse, alcohol intoxication, and crashes occurring at intersections or within higher speed limit zones. (See Appendix A for the corresponding bivariate comparisons.)
TABLE 3—
Multivariate Logistic Regression Models Examining Covariates Associated With Fatal Injuries and Head Injuries Among the Crash-Involved and Trauma Data Sets, Respectively: Michigan
| Risk Factors | Fatalities,a AOR (95% CI) | Head Injuries,b AOR (95% CI) |
| Age | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.00) |
| Male gender | 1.65 (1.06, 2.58) | 1.34 (0.93, 2.01) |
| White racec | NA | 1.00 (0.67, 1.48) |
| Helmet nonuse | 1.84 (1.36, 2.51) | 2.31 (1.69, 3.15) |
| Alcohol intoxication | 11.31 (7.82, 16.37) | 2.81 (2.00, 3.94) |
| Crash at intersection | 1.62 (1.19, 2.19) | 0.84 (0.63, 1.12) |
| Speed limit | 1.04 (1.03, 1.05) | 0.99 (0.88, 1.11) |
| Public payer or self-payc | NA | 0.77 (0.55, 1.07) |
Notes. AOR = adjusted odds ratio; CI = confidence interval; NA = not available.
Fatalities (vs all other crash-involved riders) were examined among the statewide police-reported crash data set.
Head injuries (vs hospitalized crash-involved riders requiring trauma care) were examined among the combined data set linking the crash and the trauma data sets.
Race/ethnicity (i.e., White vs other) and insurance status (public payer or self-pay vs other) were not available for the statewide police-reported crash data set.
Effects of Repeal on Head Injuries
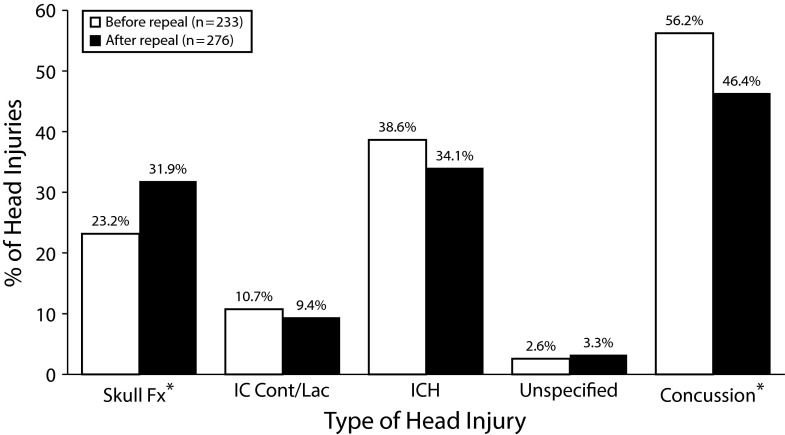
Although overall mean ISS and rates of in-hospital mortality did not change significantly, the percentage of hospitalized patients with head injuries increased 14% (43.4% vs 49.6%; P < .05; Table 2) following the repeal. Among head injury categories (Figure 1), the proportion of those attributable to concussion-type injuries decreased (56.2% vs 46.4%; P < .05), whereas those attributable to skull fractures increased (23.2% vs 31.9%; P < .05). Although we noted more overall head injuries and a different distribution of head injury subtypes after the repeal, there were no differences in standardized injury severity measures among head-injured patients (mean AIS head or neck = 2.6 ±1.2 vs 2.6 ±1.2; NS). Finally, the need for neurosurgical intervention increased following the repeal (3.7% vs 6.5%; P < .05).
FIGURE 1—
Patterns of Head Injuries (n = 509) Diagnosed Among Crash-Involved Motorcyclists Requiring Trauma Care Before (April 13, 2011, to April 12, 2012; n = 233) and After (April 13, 2012, to April 12, 2013; n = 276) the Partial Repeal of Michigan’s Universal Motorcycle Helmet Law
Note. Concussion = minor head injury, including concussion diagnosis; IC Cont/Lac = intracerebral contusion or cerebral laceration; ICH = intracranial hemorrhage, including epidural hematoma, subdural hematoma, subarachnoid hemorrhage, and other; skull Fx = skull fracture; unspecified = unspecified head injury. Patients could be diagnosed with more than 1 type of head injury. There were no patients within the sample diagnosed with head injury before or after partial repeal of the helmet law based on diagnosis of superficial scalp laceration (International Classification of Diseases, Ninth Revision, Clinical Modification, code 873.0–873.9) with concurrent fatal injury.
*P < .05 for comparisons of before vs after.
Head-injured patients did not differ from those without head injuries in sociodemographics, motorcycle type, or motorcycle registration state. However, those with head injuries were more likely to be intoxicated (27.7% vs 10.8%; P < .001) and less likely to be wearing a helmet (70.1% vs 85.6%; P < .001). Multivariate modeling (Table 3) found that alcohol intoxication and helmet nonuse significantly increased the odds of a head injury. (See Appendix A, available as a supplement to the online version of this article at http://www.ajph.org, for the corresponding bivariate comparisons.) Furthermore, head-injured patients were more likely than non–head-injured patients to require intensive hospital services, including intubation or ventilator support (30.1% vs 9.2%; P < .001), neurosurgical intervention (10.8% vs 0.2%; P < .001), and ICU admission (38.3% vs 17.1%; P < .001). Head-injured patients also had a longer LOS in the ICU (7.1 ±7.9 vs 4.2 ±4.7 days; P < .01).
DISCUSSION
There is considerable evidence that UHLs increase helmet use6,11 and decrease fatal and nonfatal injuries, including motorcycle crash–related head injuries.12–14 Furthermore, studies have consistently demonstrated the detrimental impact of weakening UHLs.11,15–20 Our study is the first to evaluate the statewide impact of Michigan’s partial UHL repeal. Similar to previous work, we found that the repeal had a detrimental impact on health outcomes, leading to 24% and 27% declines in helmet use in the crash and trauma samples, respectively, and a 14% increase in head injuries among hospitalized motorcyclists. Although we would expect more unhelmeted riders in a trauma sample than in the general riding population, we found that one third of crash-injured patients were unhelmeted following the repeal, as opposed to less than 10% before the repeal. The repeal also affected the types of injuries treated at trauma centers. Although relative injury severity did not change, head injury types shifted from those attributable to concussions to more injuries attributable to skull fractures. Such findings further reinforce the public health benefits of UHLs and corroborate previous research.
Despite our head injury finding, the overall fatality rate did not change significantly. Although this is contrary to previous research,11,15–17,19 it is consistent with data observed in Pennsylvania, where head injury hospitalizations and deaths attributable to head injury increased but the rate of overall deaths per 10 000 rider registrations remained unchanged following the state’s UHL repeal.18 The nonsignificant change in fatalities may reflect the finding that Michigan’s helmet use following the repeal remained higher than that observed in other states that have undergone similar repeal efforts.16,31 Furthermore, as the overall number of motorcycle crash fatalities are smaller than nonfatal injuries and there is normal variability in year-to-year fatality numbers, 1 year of crash data may not be enough to fully observe the changes resulting from the law change. Regardless, further study is needed over additional years to fully assess the impact of the repeal on fatalities.
Alcohol intoxication significantly increased both fatality and head injury risk. Helmet use among intoxicated riders and patients declined 47% and 35% in the crash and trauma samples, respectively. These decreases were the most observed across any subgroup. This is consistent with research demonstrating that impaired motorcyclists have lower helmet use, higher incidence of severe head injuries, and higher ISS scores than do nonimpaired crash-involved motorcyclists.32 Intoxicated operators are also more likely to exceed speed limits, ride without a license, and be in single-vehicle crashes.32,33 Nationally, in 2013, 28% of all fatally injured motorcyclists and 40% of fatally injured motorcyclists involved in single-vehicle crashes were intoxicated.1 These data indicate that intoxicated motorcyclists are not only more likely to exhibit multiple co-occurring risk behaviors, but also are one of the subgroups most affected by UHL repeals. In the absence of UHLs, our results suggest a stronger role for enforcement of existing impaired driving laws and novel policies that reduce negative outcomes in this subgroup.34
Hospitalized trauma patients experiencing head injuries had higher use of costly services including ICU admission, mechanical ventilation, and neurosurgical intervention. There was also overall greater need for neurosurgical intervention after the repeal. This is consistent with evidence that unhelmeted crash-involved motorcyclists have more brain injuries, acute care costs, and long-term health care needs.10,18,35 A recent single Michigan trauma center study found that the average acute care cost for unhelmeted riders was about $33 000, 35% higher than that for helmeted riders.20 Given this, acute care costs for our sample likely increased following the repeal, potentially affecting both private insurers and safety-net programs. Further study is needed to fully understand such cost implications, including the substantial costs that have long-term impacts for the crash-involved riders, their families, and society as a whole. One study36 found that the absence of a UHL increased out-of-state rider fatalities by 18% compared with UHL states. However, we found no evidence for an increase in out-of-state riders. This suggests that Michigan’s UHL repeal did not increase tourism, a key motivation cited by advocates of the repeal.
Limitations
Limitations should be noted. As unhelmeted riders are more likely than helmeted riders to be injured, crashes involving unhelmeted riders may be more likely to be included in police-reported data. Also, trauma center data did not capture lower-severity injuries treated at other hospitals or patients who were discharged directly from the ED. We used ICD-9-CM codes to identify head injuries. However, these are not routinely assessed for validity and reliability, and coding practices may not be consistent across hospitals. In the linked data, there is potential for differences resulting from cases that linked compared with those that did not. However, analyses among the full trauma registry (n = 1698) yielded similar results regarding helmet use, head injury, and mortality.
The subset of riders aged 16 to 20 years was too small to analyze separately the impact of the repeal on those younger than the legal age for riding unhelmeted. In addition, hospital charge and cost data were unavailable, limiting our ability to fully characterize societal costs, including costs for rehabilitation, lost productivity, and legal issues. Lastly, assessments of long-term functional status, especially with regard to ability to return to work and perform activities of daily living, were not available.
Conclusions
Michigan’s partial UHL repeal decreased helmet use and increased head injury among crash-involved motorcyclists. Furthermore, helmet nonuse doubled the odds of a fatality and tripled the odds of a head injury. Those sustaining head injuries experienced higher rates of costly treatment services. Future research should examine the impact of Michigan’s helmet repeal by using additional years of data as they become available and examine the underlying direct and indirect costs associated with the repeal, especially the societal costs associated with providing more long-term head injury care for patients involved in motorcycle crashes. Furthermore, until UHLs are reinstated, public health and injury prevention efforts should also continue to focus on addressing high-risk subgroups (e.g., drinking riders), enforcing existing laws, and developing novel evidence-based interventions that can increase helmet use among the current riding population.
ACKNOWLEDGMENTS
This work was funded by the Insurance Institute for Highway Safety under contract 7634 and, in part, by the Centers for Disease Control and Prevention (1R49CE002099) and, in part, by K23DA039341. Blue Cross Blue Shield of Michigan/Blue Care Network provides support to the University of Michigan as the Coordinating Center for Michigan Trauma Quality Improvement Program (MTQIP).
The authors wish to acknowledge Wendi Mohl for her assistance in article preparation. The authors also wish to acknowledge Judy Mikhail and Jill Jakubus within the MTQIP for their assistance with data acquisition and management. We would also like to acknowledge the following participants for their care of the trauma patients and submission of data to MTQIP: Tom Rohs, Mican DeBoer, and Jodie Vining, of Borgess Health; Michael Rebock, Barb Smith, Shauna DiPasquo, and Robin Lebeis, of Botsford Hospital; Scott Davidson, Rita Cox, and Liz Sarwar, of Bronson Methodist Hospital; Sujal Patel, Deb Falkenberg, Deanne Krajkowski, and Stacey Lopez, of Covenant HealthCare; Anna Ledgerwood, Markyta Armstrong-Goldman, Katherine Dhue, and Greta Eagger, of Detroit Receiving Hospital; Brian Shapiro, Zachary Landers, and Raquel Yapchai, of Genesys Health System; Pat Patton, Jerry Stassinopoulos, Beth Fasbinder, Velma Cuevas, and Cheryl Church, of Henry Ford Hospital; Scott Barnes, Chris McEachin, Michelle Jaskot, and Rose Morrison, of Henry Ford Macomb Hospital; Michael McCann, Michelle Maxson, Amber Dombroswski, and Shirley Ulmer, of Hurley Medical Center; Nick Nunnally, Ashley Brown, and Erin Veit, of McLaren Lapeer Hospital; Douglas Paulk, Sue Schafer, April Pizzo, and Leslie Frezza, of McLaren Macomb Hospital; John Ketner, Courtney Berry, and Stephanie Flynn, of McLaren Oakland Hospital; Wayne VanderKolk, Sherri Veurink-Balicki, and Coleen Kelly, of Mercy Health St Marys; Thomas Veverka, Tom Wood, and Lori Coppola, of MidMichigan Health; David Kam, Shamarie Regenold, and Jill Jean, of Munson Medical Center; John Fath, James Wagner, Barbara Ferrari, Gail Colton, and Judy Ellis, of Oakwood Dearborn Hospital; Allan Lamb, Kathy Franzen, and Heather Payton, of Oakwood Southshore Hospital; Michael White, Gwyn Navas, Adelaide Ammon, Danielle Finn, and Patty Danhoff, of Sinai Grace Hospital; John Kepros, Penny Stevens, and Marie Maier, of Sparrow Hospital; Gaby Iskander, Amy Koestner, Kristen Thornton, and Kelly Burns, of Spectrum Health; Joseph Buck, Karrie Brown, Mary Claire Rawlings, and Kathleen Waderlow, of St John Hospital; Mary-Margaret Brandt, Wendy Wahl, Kathy Kempf, Donna Tommelein, and Erica Cox, of St Joseph Mercy Hospital Ann Arbor; Alicia Kieninger, Carol Spinweber, Ellen Noone-Eustice, and Natalie Crook, of St Joseph Mercy Hospital Oakland; Samer Kais, Josh Chernich, Valerie Blake, and Nancy Walter, of St Marys of Michigan; Lena Napolitano, Chris Wagner, Cece Roiter, and Diane Tuttle-Smith, of University of Michigan Health System; Larry Lewis, Jason Doney, and Lisa Taylor, of UP Health System Marquette; and Randy Janczyk, Holly Bair, and Bobbie McFall, of William Beaumont Hospital.
Note. Mark Hemmila serves as the director of MTQIP. The views in the article do not necessarily reflect those of the Centers for Disease Control and Prevention or MTQIP.
HUMAN PARTICIPANT PROTECTION
The University of Michigan institutional review board granted a notice of exemption as it was a review of existing de-identified secondary data from established data sets and did not require direct interaction with human participants.
REFERENCES
- 1.National Highway Traffic Safety Administration. Traffic safety facts 2013 data—motorcycles. Washington, DC: US Department of Transportation; 2015.
- 2.Cook LJ, Kerns TJ, Burch CA, Thomas A, Bell E. Motorcycle helmet use and head and facial injuries: crash outcomes in CODES-linked data. National Highway Traffic Safety Administration. 2009. DOT HS 811 208. Available at: https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/811208. Accessed November 1, 2016.
- 3.Coben JH, Steiner CA, Miller TR. Characteristics of motorcycle-related hospitalizations: comparing states with different helmet laws. Accid Anal Prev. 2007;39(1):190–196. doi: 10.1016/j.aap.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 4.Crompton JG, Oyetunji T, Stevens KA et al. Motorcycle helmets save lives, but not limbs: a National Trauma Data Bank analysis of functional outcomes after motorcycle crash. J Surg Res. 2010;158(1):1–5. doi: 10.1016/j.jss.2009.06.034. [DOI] [PubMed] [Google Scholar]
- 5.Philip AF, Fangman W, Liao J, Lilienthal M, Choi K. Helmets prevent motorcycle injuries with significant economic benefits. Traffic Inj Prev. 2013;14(5):496–500. doi: 10.1080/15389588.2012.727109. [DOI] [PubMed] [Google Scholar]
- 6.Mayrose J. The effects of a mandatory motorcycle helmet law on helmet use and injury patterns among motorcyclist fatalities. J Safety Res. 2008;39(4):429–432. doi: 10.1016/j.jsr.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Liu BC, Ivers R, Norton R et al. Helmets for preventing injury in motorcycle riders. Cochrane Database Syst Rev. 2008;(1):CD004333. doi: 10.1002/14651858.CD004333.pub3. [DOI] [PubMed] [Google Scholar]
- 8.National Highway Traffic Safety Administration. Traffic safety facts—motorcycle helmet use laws. Washington, DC: US Department of Transportation; 2008.
- 9.Brown CV, Hejl K, Bui E, Tips G, Coopwood B. Risk factors for riding and crashing a motorcycle unhelmeted. J Emerg Med. 2011;41(4):441–446. doi: 10.1016/j.jemermed.2009.07.024. [DOI] [PubMed] [Google Scholar]
- 10.Heldt KA, Renner CH, Boarini DJ, Swegle JR. Costs associated with helmet use in motorcycle crashes: the cost of not wearing a helmet. Traffic Inj Prev. 2012;13(2):144–149. doi: 10.1080/15389588.2011.637252. [DOI] [PubMed] [Google Scholar]
- 11.Houston DJ, Richardson LE., Jr Motorcycle safety and the repeal of universal helmet laws. Am J Public Health. 2007;97(11):2063–2069. doi: 10.2105/AJPH.2006.094615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morris CC. Generalized linear regression analysis of association of universal helmet laws with motorcyclist fatality rates. Accid Anal Prev. 2006;38(1):142–147. doi: 10.1016/j.aap.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Kraus JF, Peek C, McArthur DL, Williams A. The effect of the 1992 California motorcycle helmet use law on motorcycle crash fatalities and injuries. JAMA. 1994;272(19):1506–1511. [PubMed] [Google Scholar]
- 14.Fleming NS, Becker ER. The impact of the Texas 1989 motorcycle helmet law on total and head-related fatalities, severe injuries, and overall injuries. Med Care. 1992;30(9):832–845. doi: 10.1097/00005650-199209000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Homer J, French M. Motorcycle helmet laws in the United States from 1990 to 2005: politics and public health. Am J Public Health. 2009;99(3):415–423. doi: 10.2105/AJPH.2008.134106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bledsoe GH, Schexnayder SM, Carey MJ et al. The negative impact of the repeal of the Arkansas motorcycle helmet law. J Trauma. 2002;53(6):1078–1086. doi: 10.1097/00005373-200212000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Kyrychenko SY, McCartt AT. Florida’s weakened motorcycle helmet law: effects on death rates in motorcycle crashes. Traffic Inj Prev. 2006;7(1):55–60. doi: 10.1080/15389580500377833. [DOI] [PubMed] [Google Scholar]
- 18.Mertz KJ, Weiss HB. Changes in motorcycle-related head injury deaths, hospitalizations, and hospital charges following repeal of Pennsylvania’s mandatory motorcycle helmet law. Am J Public Health. 2008;98(8):1464–1467. doi: 10.2105/AJPH.2007.123299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Keeffe T, Dearwater SR, Gentilello LM et al. Increased fatalities after motorcycle helmet law repeal: is it all because of lack of helmets? J Trauma. 2007;63(5):1006–1009. doi: 10.1097/TA.0b013e31815644cd. [DOI] [PubMed] [Google Scholar]
- 20.Chapman AJ, Titus R, Ferenchick H, Davis A, Rodriguez C. Repeal of the Michigan helmet law: early clinical impacts. Am J Surg. 2014;207(3):352–356. doi: 10.1016/j.amjsurg.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Highway Loss Data Institute. The effects of Michigan’s weakened motorcycle helmet use law on insurance losses. HLDI Bulletin. 2013;30(9):1–16. [Google Scholar]
- 22.Striker RH, Chapman AJ, Titus RA, Davis AT, Rodriguez CH. Repeal of the Michigan helmet law: the evolving clinical impact. Am J Surg. 2016;211(3):529–533. doi: 10.1016/j.amjsurg.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Michigan Trauma Quality Improvement Program. On-site data validation. Available at: http://www.mtqip.org/resources/#policies. Accessed November 1, 2016.
- 24.Manual on Classification of Motor Vehicle Traffic Accidents. 5th ed. Itasca, IL: National Safety Council; 1990. ANSI D-16.11–1989. [Google Scholar]
- 25.Centers for Disease Control and Prevention. Traumatic brain injury in the United States: a report to Congress. 2001.
- 26.International Classification of Disease, Ninth Revision, Clinical Modification. Geneva, Switzerland: World Health Organization, Practice Management Information Corporation; 1998. [Google Scholar]
- 27.The Abbreviated Injury Scale (AIS) 2005—Update 2008. Barrington, IL: Association for the Advancement of Automotive Medicine; 2008. [PMC free article] [PubMed]
- 28.Baker SP, Oneill B, Haddon W, Long WB. Injury Severity Score—method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 29.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13(1):69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 30.McGlincy MH. ASA Proceedings of the Joint Statistical Meetings. Alexandria, VA: American Statistical Association; 2004. A Bayesian record linkage methodology for multiple imputation of missing links; pp. 4001–4008. [Google Scholar]
- 31.Buckley L, Bingham CR, Flannagan CA et al. Observation of motorcycle helmet use rates in Michigan after the partial repeal of the universal motorcycle law. Accid Anal Prev. 2016;95(pt A):178–186. doi: 10.1016/j.aap.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peek-Asa C, Kraus JF. Alcohol use, driver, and crash characteristics among injured motorcycle drivers. J Trauma. 1996;41(6):989–993. doi: 10.1097/00005373-199612000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Shankar BS, Ramzy AI, Soderstrom CA, Dischinger PC, Clark CC. Helmet use, patterns of in jury, medical outcome, and costs among motorcycle drivers in Maryland. Accid Anal Prev. 1992;24(4):385–396. doi: 10.1016/0001-4575(92)90051-j. [DOI] [PubMed] [Google Scholar]
- 34.Sun SW, Kahn DM, Swan KG. Lowering the legal blood alcohol level for motorcyclists. Accid Anal Prev. 1998;30(1):133–136. doi: 10.1016/s0001-4575(97)00055-9. [DOI] [PubMed] [Google Scholar]
- 35.Eastridge BJ, Shafi S, Minei JP et al. Economic impact of motorcycle helmets: from impact to discharge. J Trauma. 2006;60(5):978–983. doi: 10.1097/01.ta.0000215582.86115.01. [DOI] [PubMed] [Google Scholar]
- 36.French MT, Gumus G, Homer JF. Motorcycle fatalities among out-of-state riders and the role of universal helmet laws. Soc Sci Med. 2012;75(10):1855–1863. doi: 10.1016/j.socscimed.2012.06.022. [DOI] [PubMed] [Google Scholar]