Abstract
The management of parapharyngeal tumor is surgical, but the approach remains a challenge. Attention should be paid to avoidance intra-operative bleeding or cranial nerves damage. We report a case of a 67-year-old male complaining of left-ear fullness. A submucosal mass arising from the lateral wall of oropharynx on the left side was observed. Magnetic resonance imaging detected a mass arising from the parotid gland, in particular from the deep lobe, and a fine needle biopsy was compatible with “Warthin tumor.” We performed a mini-invasive transoral approach under magnification, previous isolation of homolateral vessels. The decision on which surgical approach to be used is determined by site, size vascularity, and histology of the tumor. A literature review of the main surgical approaches was performed. We performed a combined transoral dissection under magnification with cervicotomic exposure of the neck vascular bundle allowing to dissect the tumor and manage any intra-operative complications.
Keywords: Parapharyngeal mass, transoral resection, cervical resection, Warthin tumor
Introduction
In parapharyngeal space (PPS), tumors are rare and most of them are benign, originating from salivary glands.1,2 PPS is an inverted pyramid-like virtual space that extends from the base of the skull to the hyoid bone. It is bounded by the temporal bone above, the vertebrae and prevertebral muscles behind, the buccopharyngeal fascia medially, and both the condyle of the mandible and the medial pterygoid muscle laterally. It is divided into two spaces: the pre-styloid and carotid space (CS). Magnetic resonance imaging (MRI) with gadolinium and fine needle aspiration cytology (FNAC) or core are commonly used to establish the management and to reach diagnosis. If MRI cannot be taken into consideration for patient-related problems (metal implants, pacemaker, claustrophobia, etc.) it is possible to perform a computed tomography (CT) with contrast and a FNAC. The parapharyngeal (PP) masses treatment is surgical, but the approach remains a challenge. Among the external approach, the cervical approach is the most common, followed by cervical-parotid approach associated or not with mandibulotomy, while transoral approach is not commonly used.1 We report a primary benign salivary tumor arising from the PPS treated by a transoral approach under magnification, previous via cervicotomic isolation of neck homolateral nervous-vascular bundle.
Case report
A 67-year-old male presented to our ear, nose, and throat (ENT) unit, with a 4-month history of left-ear fullness. A submucosal mass arising from the lateral wall of oropharynx on the left side dislocating the soft palate and the left anterior tonsillar pillar anteromedially was observed (Figure 1). Audiometric tests showed a left mild conductive hearing loss, with type “B” tympanogram. MRI showed a mass of 22 × 43 × 56 mm3 arising from the deep lobe of the parotid gland (Figure 2). A fine needle biopsy was compatible with “Warthin tumor.” Previous nasotracheal intubation, a standard tonsillectomy position is used. Before oral incision, we isolated the left internal jugular vein (IJV) and the carotid arteries via cervicotomic approach (Figure 3). Under microscope magnification, with a grade of magnification depending on the operational requirements, monopolar diathermy is employed to make the incision with an extension from the tongue base to the soft palate. Standard dissection is used to mobilize the tumor on all sides. Then, the flap is replaced and repaired with biodegradable sutures. The specimen confirmed the FNAC diagnosis of Warthin tumor (Figure 4). After 2 days of operation, patient developed a small collection of saliva of the surgical oral field treated with drainage and intravenous antibiotics in ambulatory setting. After 5 days of surgical operation, following the resolution of this collection, the patient was discharged home.
Figure 1.

The mass arising from the lateral wall of the left oropharynx.
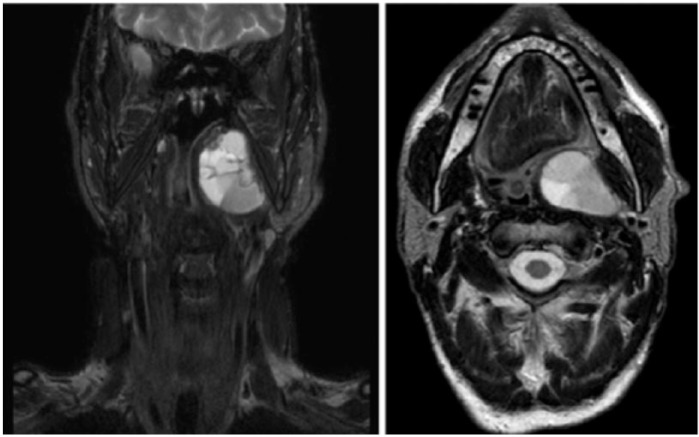
Figure 2.
The MRI shows that the mass measures 22 × 43 × 56 mm3 and arises from the deep lobe of the parotid gland.
Figure 3.
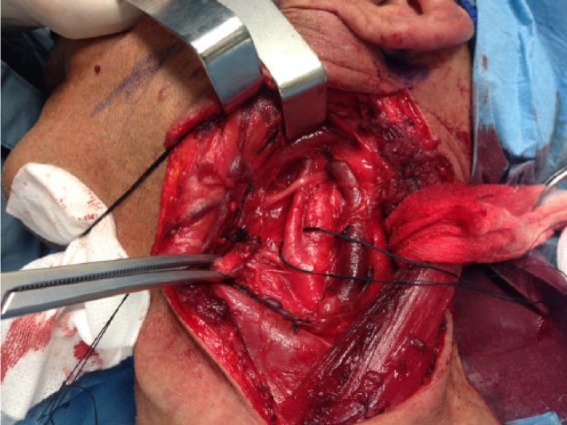
Isolation of internal jugular vein, common carotid artery, carotid bifurcation, internal carotid artery, and external carotid artery.
Figure 4.

The specimen after surgical removal.
Discussion
PPS is a complex anatomic region. Into this potential space are cranial nerves (CN) IX, X, XI, and XII, the sympathetic chain, carotid artery, the IJV, and lymph node. The choice of the approach is driven by the size, site, vascularity, and histology of the tumor, and it should meet a wide intra-operative visibility for safe radical dissection and minimal functional or cosmetic after-effects.1 External approaches provide a good access to the PPS tumors, but they are associated with cosmetic sequelae and higher risk of CN deficit, especially if the tumor arises from deep lobe of parotid.
Trans-cervical approach provides a good access to the inferior CS compartment tumors, but it is not best suited for deep-lobe parotid or other tumors in the pre-styloid compartment; similarly, access to the supero-medial CS compartment is limited.
Trans-parotid approach is suitable only for the deep-lobe parotid tumors which extend into the PPS. It requires either superficial parotidectomy or anterior reflection of superficial lobe with identification and preservation of the facial nerve, challenging for larger deep-lobe tumors. Access to the CS compartment is also limited.
Trans-parotid trans-cervical approach may provide a wide exposure, but the CN deficit risk is equally high.
Trans-parotid trans-cervical approach or cervical approach combined with a mandibulotomy is indicated for malignant lesions. A mandibulotomy approach may require a covering tracheostomy, longer hospital stay, and a delay in oral nutrition. It also carries risks of mandibular displacement, temporomandibular joint dysfunction, and loss of dentition and CN deficit.
Transoral approach described in 19503 was indicated for small, non-vascular tumors, as it offers poor exposition and does not give adequate control in the event of hemorrhage. According to Olsen,4 the transoral approach is considered to be unsafe since it is correlated with many post-operative complications such as hemorrhage, fistulas, dehiscence, and nerve damage, and for these same reasons, the combined transoral-transcervical approach should also be avoided. McElroth et al.5 in 1963, to reduce intra-operative bleeding risk, described transoral approach with ligature of the external carotid artery to remove PPS tumors in a study on 112 patients with good results. In 1988, Goodwin and Chandler6 concluded that transoral approach provide an adequate access to the PPS. Compared with trans-cervical approach, it is associated with a lower post-operative complications rate and shows some advantages and limitations.7 The main limitation is a narrowed access which may jeopardize complete removal of tumor and enhance risk of neurovascular injury; some authors do not advocate routine use of this technique, as we feel the limited exposure incurs a higher risk of tumor rupture, incomplete removal, uncontrollable hemorrhage, and facial nerve injury. In select cases, however, Betka et al.8 advocate this approach due to its superior visual control of dissection over the medial and upper parts of the tumor, short surgical and hospitalization times, and good functional and cosmetic outcome. In recent years, transoral robotic surgery has been employed to resect benign lesions within the PPS with good result;9,10 for the limited availability of the equipment required, there are very few centers worldwide that undertake this approach.
We purpose a transoral approach under magnification for deepest tumor of the PPS with oral bulging; a concomitant via cervicotomic isolation of the common, external, and internal carotid arteries and IJV allow to mobilize the mass and could give a full control of major complications, like uncontrollable bleeding and CN damage.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for their anonymized information to be published in this article.
References
- 1. Kuet ML, Kasbekar AV, Masterson L, et al. Management of tumors arising from the parapharyngeal space: a systematic review of 1,293 cases reported over 25 years. Laryngoscope 2015; 125(6): 1372–1381. [DOI] [PubMed] [Google Scholar]
- 2. Khafif A, Segev Y, Kaplan DM, et al. Surgical management of parapharyngeal space tumors: a 10-year review. Otolaryngol Head Neck Surg 2005; 132: 401–406. [DOI] [PubMed] [Google Scholar]
- 3. Ehrlich H. Mixed tumors of the pterygomaxillary space; operative removal; oral approach. Oral Surg Oral Med Oral Pathol 1950; 3(11): 1366–1371. [DOI] [PubMed] [Google Scholar]
- 4. Olsen KD. Tumors and surgery of the parapharyngeal space. Laryngoscope 1994; 104: 1–28. [DOI] [PubMed] [Google Scholar]
- 5. McElroth DC, Remine WH, Devine KD. Tumours of the parapharyngeal region. Surg Gyneco Obstet 1963; 116: 88–94. [Google Scholar]
- 6. Goodwin WJ, Jr, Chandler JR. Transoral excision of lateral para-pharyngeal space tumors presenting intraorally. Laryngoscope 1988; 98(3): 266–269. [DOI] [PubMed] [Google Scholar]
- 7. Carrau RL, Myers EN, Johnson JT. Management of tumors arising in the parapharyngeal space. Laryngoscope 1990; 100(6): 583–589. [DOI] [PubMed] [Google Scholar]
- 8. Betka J, Chovanec M, Klozar J, et al. Transoral and combined transoral-transcervical approach in the surgery of parapharyngeal tumors. Eur Arch Otorhinolaryngol 2010; 267: 765–772. [DOI] [PubMed] [Google Scholar]
- 9. Ansarin M, Tagliabue M, Chu F, et al. Transoral robotic surgery in retrostyloid parapharyngeal space schwannomas. Case Rep Otolaryngol 2014; 2014: 296025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee HS, Kim J, Lee HJ, et al. Transoral robotic surgery for neurogenic tumors of the prestyloid parapharyngeal space. Auris Nasus Larynx 2012; 39: 434–437. [DOI] [PubMed] [Google Scholar]