Abstract
The aim of this study was to determine complication of neonatal meningitis due to streptococcus group B in full-term and near–full-term newborns in a tertiary-level neonate intensive care unit.
Keywords: neonatology, infectious diseases, neurology, radiology, general pediatrics
Background
Neonates are at greater risk for sepsis and meningitis than those in other age-groups. Early-onset neonatal meningitis due to streptococcus group B is a serious but uncommon disease. The prevalence of neonatal meningitis is estimated to be 0.15 to 0.5 per 1000 births in industrialized countries, with mortality estimated to be between 8.5% and 15%.1
Objective
The aim of this study was to determine complication of neonatal meningitis due to streptococcus group B in full-term and near–full-term newborns in a tertiary-level neonate intensive care unit.
Study Design
This was a retrospective cohort study of full-term and near–full-term newborns with a diagnosis of meningitis due to streptococcus group B.
We included newborns (0-28 days), and not less than 35 weeks, admitted to the Robert Debré Hospital between 1984 and 2014 with a diagnosis of streptococcus group B meningitis proven by cerebrospinal fluid culture. Laboratory data, clinical features, and imaging were recorded (see Table 1).
Table 1.
Laboratory data, clinical features, and imaging for 9 study patients.
| Case | CRP at Admission (mg/L) | WBC at Admission (/mm3) | Blood Culture | LP WBC (/mm3) | MRI/CT Scan | Neurologic Outcome (abnormal = 1) |
|---|---|---|---|---|---|---|
| A | 117 | 5100 | 0 | 7265 | Stroke ischemic | 1 |
| B | 32 | 2110 | 0 | — | Stroke ischemic/hemorrhage | 0 |
| C | 208 | 14 800 | 0 | 7195 | Ventriculitis | 0 |
| D | 155 | 11 000 | 1 | 1630 | Leukomalacia | 1 |
| E | 91 | 25 600 | 1 | 895 | Stroke ischemic | 0 |
| F | 137 | 2810 | 0 | 3600 | Ventriculitis | 1 |
| G | 5 | 13 100 | 0 | 6300 | Asymmetric periventricular space | 0 |
| H | 6 | 2300 | 0 | 0 | Stroke ischemic | 0 |
| I | 209 | 7100 | 0 | 14 600 | Temporal edema | 0 |
| Mean | 106.6 | 9324.44 | 5189.375 | — | — | |
| Percentage | — | — | 33% | — | — | 25% |
Abbreviations: CRP, C-reactive protein; LP, lumbar puncture; WBC, white blood count; MRI, magnetic resonance imaging; CT, computed tomography.
Twenty-five cases of neonatal meningitis due to streptococcus group B were reported between 1985 and 2010, and 2 cases were excluded because they had congenital anomalies; 14 records have not been found in the archives (see Figure 1).
Figure 1.
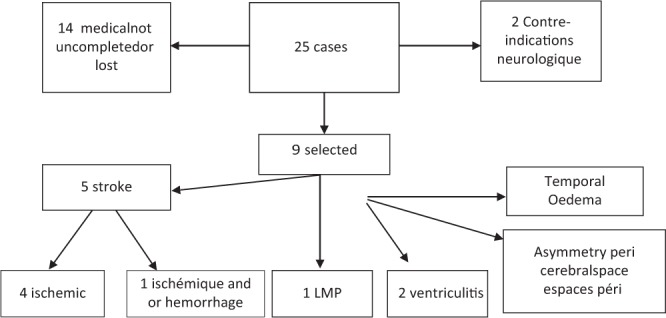
Evaluation of 25 total cases.
Discussion
Streptococcus agalactiae is a Gram positive facultative anaerobe. It has an oval shape and usually measures 0.5 to 1.0 µm. It is β-hemolytic on blood agar with 9 different serotypes (Ia, Ib, II, III, IV, V, VI, VII, and VIII).
The human reservoir is located in the gastrointestinal tract. The vaginal colonization of pregnant women is 10% to 30% during pregnancy.
Despite the common introduction of intrapartum antibiotic prophylaxis, streptococcal infections of streptococcus group B remains a major cause of morbidity and mortality among newborns in Europe, North America, and Australia.
For early-onset sepsis due to streptococcus group B, incidence is 0 to 43 per 1000 live births (95% confidence interval = 0.37-0.49) and mortality 12.1%, which is 2 times higher than that reported for late infections. The serotype most frequently identified in all regions was serotype III (48.9%), followed by serotypes Ia (22.9%), Ib (7.0%), II (6.2%), and V (1.9%).
The introduction of intrapartum antibiotic prophylaxis is associated with a lower incidence of early-onset streptococcus group B (0.23 per 1000 live births; 95% confidence interval = 0.13-0.59) than when intrapartum antibiotics are not used (0 to 75 per 1000 live births; 95% confidence interval = 0.58-0.89).2,3
The prevalence of neonatal meningitis is estimated to be 0.15 to 0.5 per 1000 live births in industrialized countries, with an estimated mortality of 8.5% to 15%.4
Acute complications of neonatal bacterial meningitis include cerebral edema (vasogenic and cytotoxic), ventriculitis, cerebritis, hydrocephalus, brain abscess, cerebral infarction, and subdural effusion or empyema.4 Development of these complications may lead to moderate to severe neurodisabilities.
Many of these infants have a history of maternal chorioamnionitis. Most affected infants experience cardiorespiratory problems, such as respiratory distress syndrome or pneumonia, in association with hypotension or patent ductus arteriosus during their first days of life. Bacterial infection at birth also appears to be a risk factor.5,6
White matter is primarily responsible for the transmission of nerve impulses that control motor function. This involvement may cause spasticity and intellectual disability. Myelin is an integral part of the white matter. Deterioration of myelin may alter brain function.
Maternal infection, placental inflammation, and vasculitis are also important in the pathogenesis of periventricular leukomalacia. A link between maternal infection, preterm birth, and central nervous system injury has been established by epidemiological studies.2,3
Hermansen and Hermansen conducted immunohistochemical staining analysis on brain from 17 infants: cytokines were documented in 17 (88%) infants with periventricular leukomalacia against only 11% of those who had no periventricular leukomalacia.1
Other studies demonstrate the role of combination of cytokine tumor necrosis factor and infection in periventricular leukomalacia lesions and in the cerebrospinal fluid of infants with cerebral white matter injury.6,7
Conclusion
Neonatal meningitis due to streptococcus group B is rare, but can cause complication in both term and preterm newborns. Neurologic outcome remains the major adverse effect for survivors.
In our study, the main acute neuroimaging complication was stroke, with 25 per 100 neurologic disabilities at 4 years.
Footnotes
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hermansen MC, Hermansen MG. Perinatal infections and cerebral palsy. Clin Perinatol. 2006;33:315-333. [DOI] [PubMed] [Google Scholar]
- 2. Stoll BJ, Hansen NI, Sánchez PJ, et al. Early-onset neonatal sepsis: the burden of group B streptococcal and E. coli disease continues. Pediatrics. 2011;127:817-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Edmond KM, Kortsalioudaki C, Scott S, et al. Group B streptococcal disease in infants aged younger than 3 months: systematic review and meta-analysis. Lancet. 2012;379:547-556. [DOI] [PubMed] [Google Scholar]
- 4. Volpe JJ. Bacterial and fungal intracranial infections. In: Neurology of the Newborn. 4th ed. Philadelphia, PA: WB Saunders; 2001:774. [Google Scholar]
- 5. Nelson KB, Ellenberg JH. Predictors of low and very low birth weight and the relation of these to cerebral palsy. JAMA. 1985;254:1473-1479. [PubMed] [Google Scholar]
- 6. Perlman JM, Risser R, Broyles RS. Bilateral cystic periventricular leukomalacia in the premature infant: associated risk factors. Pediatrics. 1996;97:822-827. [PubMed] [Google Scholar]
- 7. Kadhim H, Tabarki B, Verellen G, De Prez C, Rona AM, Sébire G. Inflammatory cytokines in the pathogenesis of periventricular leukomalacia. Neurology. 2001;56:1278-1284. [DOI] [PubMed] [Google Scholar]


