Abstract
Objectives:
To investigate the anatomical variations of the mandibular canal through assessment in situ, panoramic radiography, CT or CBCT and assess their frequency.
Methods:
Articles were selected from databases (Cochrane Library, LILACS, ProQuest, PubMed, Scopus, Web of Science and Google Scholar), articles without limitations of language, in which the main objective was to evaluate the frequency of bifurcation of the mandibular canal through assessment in situ, panoramic radiography, CT or CBCT were selected. A meta-analysis of prevalence using random effects was performed.
Results:
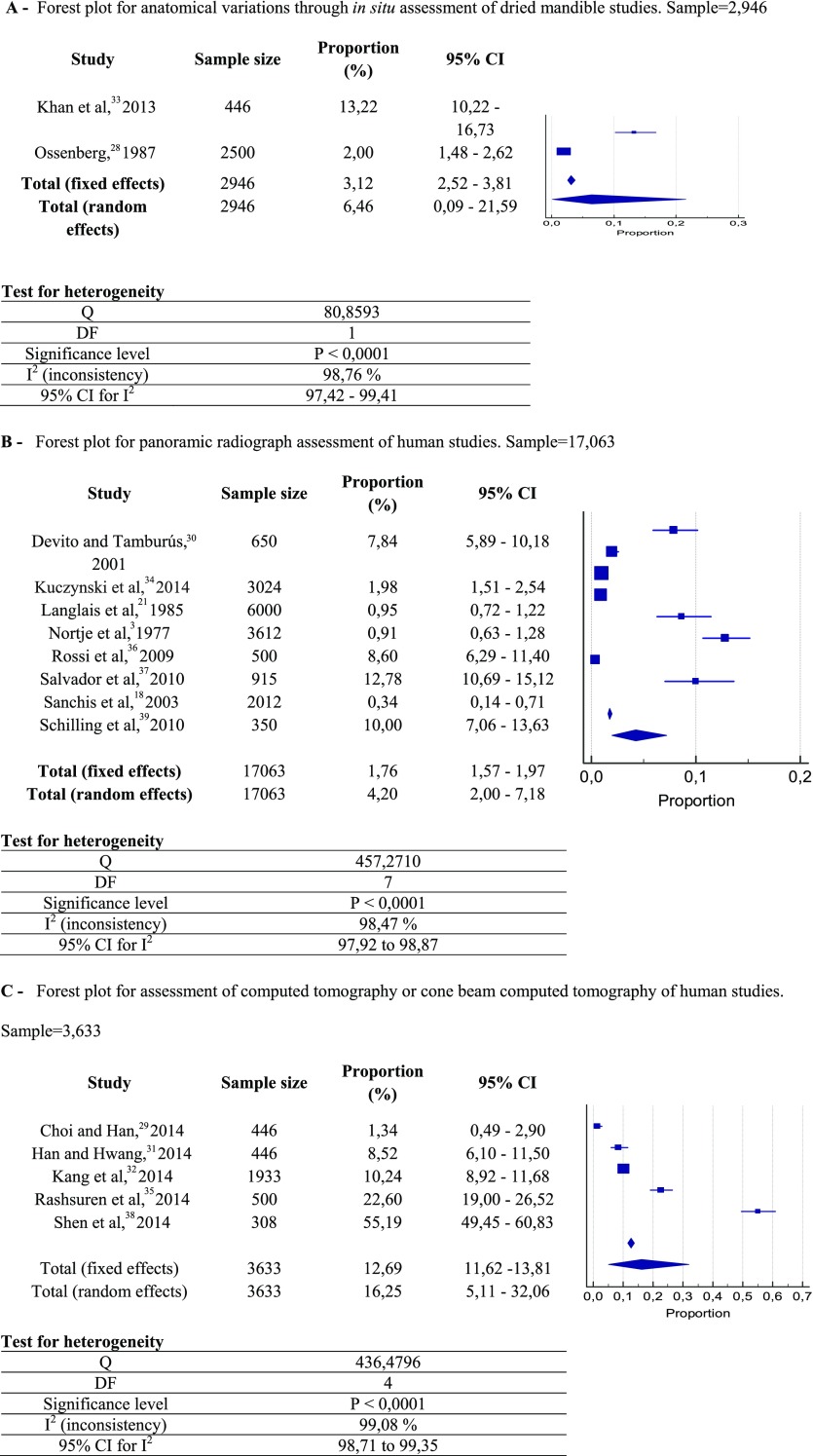
Using a selection process in two phases, 15 articles were identified, and a meta-analysis was conducted. The results from these meta-analyses showed that the overall prevalence of anatomical variations for in situ studies was 6.46%, and through assessment of panoramic radiography and CT or CBCT the overall prevalence shown was 4.20% and 16.25%, respectively.
Conclusions:
There are two types of variations of the mandibular canal: the retromolar canal and bifid mandibular canal. The frequency variations through assessing in situ, panoramic radiography and CT or CBCT were 6.46%, 4.20% and 16.25%, respectively.
Keywords: mandibular nerve, panoramic radiography, X-ray computed tomography, cone beam computerized tomography
Introduction
The mandibular canal is located inside the mandible, extending from the mandibular foramen to the mental foramen. It contains a bundle including a nerve, artery and vein. These components are responsible for somatosensory sensations and blood innervations of the mandibular teeth, interdental papilla and periodontal and alveolar bone tissues.1–7
Often, the mandibular canal is a single structure; however, in some circumstances, it can contain variations such as bifid mandibular canal or retromolar canal, which if not identified, can lead to complications during intraoral dental procedures8 (such as third molar extraction, osteotomy for bone graft and implant placement).1,7,9–12 The most common complications are somatosensory impairment during and after surgery, traumatic neuroma, bleeding and bruising signs.10,13–17 Furthermore, the presence of anatomical variations may be associated with increased difficulty in performing alveolar mandibular nerve block with concomitant patient discomfort.14,15,18,19
Anatomical variations of the mandibular canal were rare occurrences in studies using panoramic radiography, with <1% of prevalence.3,18,20,21 Nevertheless, these variations were more frequent, around 20–30%, in studies using CT and CBCT.1,22–24
Despite the importance of correct diagnosis of mandibular canal anatomical variations in order to avoid clinical complications, the scope of these variations are not well known yet. Because there is no systematic review published on this topic, this review aimed to: (1) evaluate which are the anatomical variations of the mandibular canal that can be diagnosed using assessment in situ, panoramic radiographs and CT scans and (2) assess their frequency.
Methods and materials
This systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist.25 In addition, this systematic review protocol was completed and registered at the International Prospective Register of Systematic Reviews (PROSPERO CRD42014015030).
Eligibility criteria
Inclusion criteria: articles in which the primary objective was to evaluate the anatomical variations of the mandibular canal using assessment in situ, panoramic radiography, CT or CBCT in humans (in vivo, cadavers or dry skulls) were considered. Studies published in any language were selected. Exclusion criteria included: (1) reviews, case reports, letters and personal opinions; (2) studies in which the sample included subjects with pathologies in the area around the mandibular nerve, craniofacial syndrome, previous orthognathic or craniofacial surgery, because these may affect the shape and the mandibular canal, as well as the surrounding bone structures; (3) studies that evaluated other imaging methods such as micro-CT and angiography; and (4) studies with samples <300 individuals.26
Information sources and search
Detailed individual search strategies for each of the following electronic databases were performed: Cochrane Library, LILACS, ProQuest, PubMed, Scopus and Web of Science. Google Scholar and reference lists of the selected articles were hand searched for any additional references that might have been missed in the electronic database searches. All searches were conducted in the databases from their inception through to 2 March 2015. The EndNote Basic® software (Thompson Reuters, New York, NY) was used, and duplicated hits were removed. Appropriate truncation and word combinations were selected with the support of a health sciences librarian and were adapted for each database search (Appendix A).
Study selection
A two-phase selection of the articles was conducted. In Phase 1, two authors (LFH and KD) independently reviewed the titles and abstracts of all references. Any articles that did not appear to meet the inclusion criteria were excluded. In Phase 2, full texts were independently reviewed and screened accordingly. Any disagreement was resolved by means of discussion. When mutual agreement between the first two reviewers was not accomplished, a third author (MC) became involved to make a final decision. At this phase, studies with <300 subjects were excluded.
Data collection process and data items
One author (LFH) extracted data from the selected studies, including study characteristics (authors, year of publication and country), sample characteristics (sample size, observers, number, type and kappa), diagnostic assessment methods (in situ, panoramic radiography, CT or CBCT) and outcome characteristics (frequency). A second author (KD) cross-checked all the retrieved information. Again, any mistyping was resolved by means of discussion, and a third author (MC) became involved to make a final decision.
Risk of bias in individual studies
The methodology of selected studies was evaluated by using the Meta Analysis of Statistics Assessment and Review Instrument. Two authors (LFH and KD) scored each data item as “yes”, “no”, “unclear” or “not applicable” and assessed independently the quality of each included study. The third author (MC) resolved any disagreement between the authors.
Synthesis of results
A prevalence meta-analysis was performed with the aid of MedCalc software (MedCalc, Ostend, Belgium) with significance level set at 5%. The heterogeneity between the studies found in the meta-analysis was high; therefore, a random model was chosen.27
Risk of bias across studies
The number of studies finally included precluded any assessment of the risk of bias across studies such as publication bias or selective reporting. A subgroup analysis was possible as the identified studies were separated into three groups to perform the meta-analysis according to the evaluation method of the identified variations (evaluation in situ in dry mandibles, evaluation in humans by means of panoramic radiography and evaluation in humans by means of CT or CBCT).
Results
Study selection
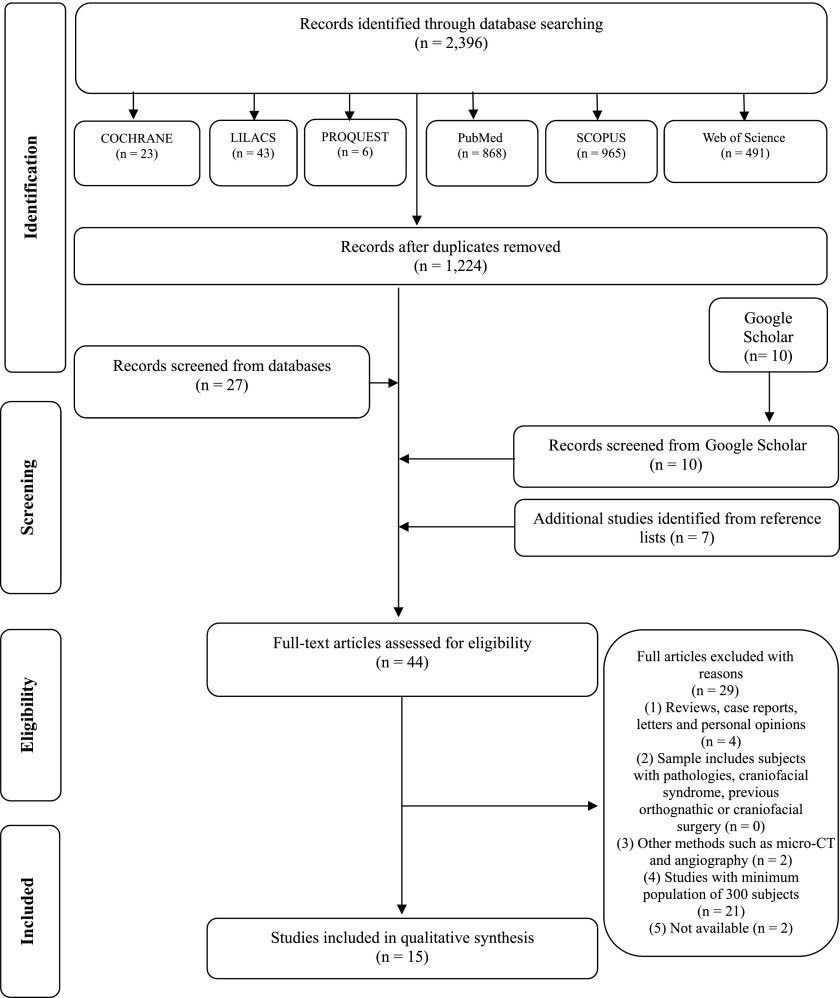
From the 2396 references initially identified, only 44 references remained after Phase 1 of the selection process. After Phase 2 of the selection process, the final included sample was 15 studies. Details about the selection process can be found in Figure 1. Reasons for the exclusion of studies in Phase 2 can be found in Appendix B.
Figure 1.
Flow diagram of literature search and selection criteria.25
Study characteristics
From the 15 studies selected, 1 study was published in an anthropology journal.28 The rest3,18,21,29–39 of the studies were published in dental journals. Sample sizes ranged from 30838 to 193332 CT images and from 35039 to 6000 panoramic radiographic images.21
The studies were conducted in nine different countries: Brazil,30,34,36,37 Canada,28 Chile,39 India,33 Korea,29,31,32,35 South Africa,3 Spain,18 Taiwan38 and USA.21 Most of the articles were published in English,3,18,21,28,29,31–35,38,39 and three articles were published in Portuguese.30,36,37 Most studies included imaging examinations of patients referred for lower third molar surgery and implant placement.
The following tools were used: human dry skulls and in situ analysis,28,33 panoramic radiography,3,21,30,34,36,37,39 panoramic radiography and CT,18 CBCT29,31,32,35 and CBCT and CT.38 A summary of the descriptive characteristics of included articles is provided in Table 1.
Table 1.
Summary of descriptive characteristics of studies in included articles (n = 15)
| Study | Country | Sample (size/type) | Methods |
Observers (number/type/kappa) | Findings overall | |||
|---|---|---|---|---|---|---|---|---|
| In situ | OPT | CT | CBCT | |||||
| Choi and Han, 201429 | Korea | 446 humans | N | N | N | Y | 1 radiologist, kappa: U | 1.35% |
| Devito and Tamburús, 200130 | Brazil | 650 humans | N | Y | N | N | U | 7.85% |
| Han and Hwang, 201431 | Korea | 446 humans | N | N | N | Y | 1 radiologist, kappa: U | 8.50% |
| Kang et al, 201432 | Korea | 1933 humans | N | N | N | Y | 2 radiologist, kappa: U | 10.20% |
| Khan et al, 201333 | India | 446 dry mandibles | Y | N | N | N | U | 13.22% |
| Kuczynski et al, 201434 | Brazil | 3024 humans | N | Y | N | N | 1 examiner, kappa: U | 1.98% |
| Langlais et al, 198521 | USA | 6000 humans | N | Y | N | N | 3 examiners, kappa: U | 0.95% |
| Nortje et al, 19773 | South Africa | 3612 humans | N | Y | N | N | U | 0.90% |
| Ossenberg, 198728 | Canada | 2500 dry mandibles | Y | N | N | N | U | 2.00% |
| Rashsuren et al, 201435 | Korea | 500 humans | N | N | N | Y | 3 radiologists, kappa: U | 22.60% |
| Rossi et al, 200936 | Brazil | 500 humans | N | Y | N | N | 1 examiner under the supervision of a radiologist, kappa = 61% | 8.60% |
| Salvador et al, 201037 | Brazil | 915 humans | N | Y | N | N | U | 12.75% |
| Sanchis et al, 200318 | Spain | 2012 humans | N | Y | Ya | N | U | 0.35% |
| Schilling et al, 201039 | Chile | 350 humans | N | Y | N | N | 1 radiologist, kappa: U | 5.00% |
| Shen et al, 201438 | Taiwan | 308 humans | N | N | Y | Y | 1 radiologist, kappa: U | 27.70% |
N, no; OPT, panoramic radiography; U, unclear; Y, yes.
Only three had CT simultaneously.
Risk of bias within studies
The studies were not homogeneous. 1 study33 presented moderate risk of bias while 14 studies3,18,21,28–32,34–39 presented high risk of bias. More information about the risk of bias assessment can be found in Table 2 and Appendix C.
Table 2.
Criteria met, according to the prevalence critical appraisal toola
| Study | Quality assessment tool for prevalence critical appraisal |
|---|---|
| Choi and Han, 201429 | High |
| Devito and Tamburús, 200130 | High |
| Han and Hwang, 201431 | High |
| Kang et al, 201432 | High |
| Khan et al, 201333 | Moderate |
| Kuczynski et al, 201434 | High |
| Langlais et al, 198521 | High |
| Nortje et al, 19773 | High |
| Ossenberg, 198728 | High |
| Rashsuren et al, 201435 | High |
| Rossi et al, 200936 | High |
| Salvador et al, 201037 | High |
| Sanchis et al, 200318 | High |
| Schilling et al, 201039 | High |
| Shen et al, 201438 | High |
INSTITUTE TJB. Joanna Briggs Institute Reviewers' Manual: 2014 edition/Supplement. The University of Adelaide, South Australia, 5005 2014.
Results of individual studies
Retromolar foramen size was analysed in dry mandibles by two studies;28,33 its diameter ranged from 0.5 mm to about 3.0 mm.28 The retromolar foramen on the right side was generally positioned further back in the retromolar region than in the left side.33 In some cases, especially those with larger diameter (>1 mm), they were positioned more anteriorly.28 In rare cases with large diameters, the foramen was located in the anterior temporal crest of the coronoid process.28
Seven studies3,21,30,34,36,37,39 evaluated the presence of a bifid mandibular canal through panoramic radiography. There was no statistically significant difference based on sex.21,34,36 Only one study18 assessed simultaneously the variation of the mandibular canal through panoramic radiography and CT. However, from a sample of 2012 panoramic radiographic images, from 3 patients with bifid mandibular canal as per panoramic radiography, only 2 CT confirmed the presence of bifid mandibular canal. Only one study38 assessed the variation of the mandibular canal through CT and CBCT; but, this study did not compare the two methods, only examined two samples: one sample considering CT (173) and another sample considering only CBCT (135). Four studies29,31,32,35 evaluated the variations of the mandibular canal through CBCT. Most of these studies31,32,35 showed no statistically significant difference based on sex or age. The average diameter of a bifid mandibular canal varied from 1.27 mm32 to 2.20 mm,35 with no statistically significant difference of bifurcation types (retromolar, forward, buccolingual and trifid canals).32,35 The average bifid mandibular canal length was from 14.97 mm32 to 16.9 mm.35 Kang et al32 found the following values for the average length of bifid mandibular canal: 14.03 mm in the case of the forward canal, 16.03 mm in the case of the buccolingual canal, 8.71 mm in the case of the dental canal and 16.20 mm in the case of the retromolar canal. Rashsuren et al35 reported the following measures for the length of the bifid mandibular canal: 18.9 mm of the forward-type canal, 10.7 mm of the dental-type canal, 17.9 mm of the retromolar canal type and 20.1 mm of the trifid canal type. There was no statistically significant difference between the retromolar, forward and buccolingual canals; however, there was significant difference between the average length of the dental canal and other types of the bifid mandibular canal32 and between the dental canal type and the trifid canal type.35
Synthesis of results
3 meta-analyses were performed after the 15 selected studies had been divided into 3 groups: (1) 2 dried mandible studies through assessment in situ;28,33 (2) 8 human studies through assessment by panoramic radiography;3,18,21,30,34,36,37,39 and (3) 5 human studies through assessment by CT or CBCT.29,31,32,35,38
The results from these meta-analysis showed that the overall prevalence of anatomical variations for in situ studies was 6.46% (n = 2946; 95% = CI 0.09 to 21.59; Figure 2a). The prevalence through assessment of panoramic radiography was 4.20% (n = 17,063; 95% = 2.00 to 7.18; Figure 2b). The prevalence through assessment of CT or CBCT was 16.25% (n = 3633; 95% = CI 5.11 to 32.06; Figure 2c).
Figure 2.
Prevalence of anatomical variations through in situ assessment of dried mandible studies (a) panoramic radiography of human studies and (b) assessment of CT or CBCT of human studies (c). Results from two types of meta-analysis: fixed and random effects. CI, confidence interval.
Risk of bias across studies
As can be seen from the previous section, the prevalence clearly varied based on diagnostic method. Although studies had a similar study design (retrospective), the main methodological problem concerns sample origin and size. Most of the selected studies18,21,28,29,31,32,35,36,38 did not have clear consistent inclusion criteria. The collected samples may not represent the overall population prevalence.
Discussion
Overall, this systematic review and meta-analysis suggested that the prevalence of bifurcation of the mandibular canal is significant (around 16%). In other words, for every six patients, one patient presented bifid mandibular canal. This finding could have important clinical implications and should be considered when planning dental procedures involving the posterior mandible.
In situ evaluation of dried mandibles
The prevalence of retromolar foramen in situ evaluation studies ranged from 3.2%28 to 13.22%.33 This rate was lower than that found in other studies40 that reported a prevalence of 26.58% of retromolar foramen. This discrepancy is probably due to several factors, such as ethnic differences, genetic and environmental factors as well as the sample size used in each study.
Studies measuring the distance between the retromolar foramen and third molar reported distances between 1 mm41 and 4.23 mm,9 and the diameter of the foramen was on an average 2 mm.42 These differences suggest that the location of the retromolar foramen is not constant. Previously, it was suggested that the location of the retromolar foramen is relatively variable, and its presence is not related to the position of the last tooth in the dental arch.9
Panoramic radiography evaluation of fresh mandibles
Prevalence of bifurcations of the mandibular canal found in earlier studies3,21 were different as compared with that of the most recent ones.30,34,36,37,39 This discrepancy varied from 0.9%3 to 34.6%.37 The difference among these values is possibly due to the quality of panoramic radiographic images, method of image analysis, rater experience and different ethnicities analysed. Conventional radiographic images have substantially improved over time, which explains the higher incidence of bifurcations of the mandibular canal found in the later studies.30,34,36,37,39 For instance, another aspect to be considered is that in the study by Salvador et al,37 the choice of the sample was based on the quality of the radiographic image (good sharpness, contrast and density), which allowed raters to clearly identify the mandibular canal. Obviously, these criteria for image selection helped in the identification of variations of the mandibular canal, thus contributing to a higher prevalence of bifurcations.
Panoramic radiography is a two-dimensional imaging method. Because of this, it is important to have a deep knowledge of related pertinent mandible anatomy, such as the oblique line, mylohyoid nerve path and insertion of the mylohyoid muscle on the inner surface of the mandible. The oblique line may overlap with the mandibular canal, which could lead to misdiagnoses. The mylohyoid nerve and insertion in the mylohyoid muscle could create a radio-opaque line parallel to the mandibular canal, which may also provide false diagnosis of bifurcations of the mandibular canal.7,34,39,43–45 Furthermore, the identification of the mandibular canal and its variations may be difficult owing to the shadow generated by the overlapping of the pharynx airways, soft palate and uvula.1,23,46
Another point to be considered in the analysis of conventional radiographic images would be rater experience. Among the studies using panoramic radiography to assess bifid mandibular canals, in one of them,36 the rater was under the supervision of a radiologist, and only in one study, the rater was also a radiologist.39 Thus, not only the quality of the radiographic image but also the rater expertise may change the prevalence of bifid mandibular canals.
Simultaneous panoramic radiography and CBCT evaluation of fresh mandibles
Sanchis et al18 evaluated the presence of bifid mandibular canals using 2012 panoramic radiographs, and in 3 cases in which there was suspected variation of the mandibular canal, the authors performed CT scanning. CT confirmed the existence of bifid mandibular canal in only two of those three cases. In those patients, a triangular shape was identified with its vertex at the root of the lower third molar, indicating bifurcation of the mandibular canal. The authors reported this could be a pathognomonic sign of variations of the mandibular canal.
Neves et al43 assessed the presence of bifid mandibular canals using panoramic radiography and CBCT. Although a higher prevalence of bifurcation of the mandibular canal has been observed through CBCT (a value higher by 2.4%) than with panoramic radiography, no statistical difference was demonstrated. Because of this, the authors suggested panoramic radiography may help the radiologist in determining the variations of the mandibular canal. A possible explanation for the similarity in prevalence found between panoramic radiography and CBCT may arise from the fact that in this study sample, most variations of the mandibular canals had large diameters, which could then be seen through both imaging techniques, which is very unusual.
Simultaneous CT or CBCT evaluation of fresh mandibles
Naitoh et al47 conducted a study comparing CT and CBCT in 28 patients, and 4 of the 19 canals observed in CBCT were not seen on CT. However, despite the fact that CBCT showed higher incidence of bifurcation of the mandibular canal than CT, the authors stated that both imaging methods were able to detect the bifurcation of the mandibular canal. Nevertheless, the image acquisition protocols were different for CT and CBCT. The voxel size used for CT was 0.5 mm and for CBCT the voxel size was 0.2 mm. That is, the voxel size used in CT images was twice the one used in CBCT. This difference in voxel size could explain why the authors found more bifid mandibular canals through CBCT. In addition, artefacts generated by metal fillings and/or metal crowns may have influenced the diagnosis of variants of the mandibular canal in the retromolar area.
Although CT and CBCT showed similar results in the diagnosis of the maxillomandibular region, CBCT presents some relevant advantages in comparison with CT: (1) relatively low radiation dose; (2) more affordable equipment; and (3) increased image quality level of the bone tissue than CT.48
Studies analysing the variations of the mandibular canal through CBCT29,31,32,35,47 have shown different results on the prevalence of bifurcation of the mandibular canal. Such disagreement is possibly due to the ethnic groups studied, size and characteristics of each sample and criteria used for classification of bifurcation of the mandibular canal. The examiners who analysed the images, protocols used for image acquisition and reconstruction used may also have contributed to the divergence between the studies.
Overall summary
Bilecenoglu and Tuncer9 analysed the material obtained from a retromolar canal and histology confirmed presence of neurovascular bundle inside the retromolar canal including striated muscle fibres and thin myelinated nerve fibres, many venules and containing an artery lumen 120–130 μm. Similarly, Fukami et al10 in a study of cadaver showed the presence of many nerve bundles and arteries of various sizes inside the bifid mandibular canal. These nerve bundles come from the inferior alveolar nerve and emit ramifications for the oral mucosa and the gums in the regions of lower molars and premolars.49 Anderson et al50 suggested these fibres innervate part of the temporal muscles and buccinator, region of the retromolar triangle and pulp of the lower third molars. Finally, it has been reported an aberrant course of the buccal nerve, deriving the inferior alveolar nerve still within the branch, passing through the retromolar canal and were externalized by retromolar.51
These neurovascular tissue variations of the mandibular canal have great clinical significance. The bifid mandibular canals may contribute to surgical complications during the extraction of the third molars.15,18,22,52–54 The injury to bifid mandibular canal during the extraction of third molars or during sagittal split osteotomy of the branch can cause bleeding during or after surgery and post-operative paraesthesia, especially the retromolar canals or forked canals in the mandibular body.14,15,21 Inadequate anaesthesia can occur especially in cases of bifurcation with two independent foraminas.55
The bifurcation of the mandibular canal occurring in the body of the lower jaw can cause complications in endodontic procedures.56 The bifurcation of the mandibular canal may also influence the support aids57 and insertion of dental implants.58 In addition to these complications, in cases of maxillofacial trauma in the mandibular region, reduction of mandibular fractures should be performed with caution when there is presence of bifurcation of the mandibular canal,15 as the commitment of the mandibular canal and/or bifurcations of the mandibular canal can cause bleeding and repair, compromising the region.59
In view of the above-mentioned elements, the correct knowledge of the anatomy of mandibular canal and its variations is critical. Bifurcations of the mandibular canal are frequent. Therefore, diagnosis of these variations is essential for success in dental procedures involving the mandible.
Although some authors47 state there are no differences between CT and CBCT regarding the diagnosis of anatomical variations of the mandibular canal, we suggest that CBCT is the examination of choice for this purpose when preliminary conventional radiography does not show a clear relationship between the inferior alveolar nerve and adjacent anatomical structures or when there is suspect bifurcation of the mandibular canal.32,60
Final considerations
The limitations of panoramic radiography are known, and caution must be employed when indicating it to assess variations of the mandibular canal.
The inherent limitations relative to conventional radiographic technique, and a higher radiation dose and more cost regarding CT,61,62 suggest that CBCT may be the most appropriate imaging method to assess the mandibular canal because it provides better visualization of anatomical structures, including location, shape and relationship with adjacent structures.43,63
Among the particularities of each study, the protocol used to capture the image in CBCT (voxel and field of view) is of outmost importance. Smaller voxel results in images with better space resolution and allows the diagnosis of reduced-diameter anatomical variations. Nevertheless, it requires a longer exposure time, which generates increased radiation. On the other hand, small fields of view may not contemplate the entire area of retromolar region, especially in the upper region towards the ascending mandibular ramus and, as a result, it may not cover the site where the anatomical variation is located.
Limitations
Despite the different diagnostic methods used by the studies and the diversity of the ethnic groups analysed, the main methodological limitations identified in the selected studies were regarding the examiners. Most studies were not clear or did not describe whether the evaluators were radiologists, how many professionals analysed the images, the correlation among them and if they were calibrated. These factors explain the high risk of bias among the selected studies.
In addition, most of the selected studies did not have clear consistent inclusion criteria. The collected samples may not represent the overall population prevalence.
Conclusions
There are basically two types of variations of the mandibular canal: retromolar canal and bifid mandibular canal. The frequency of the variations of the mandibular canal through evaluation in situ was 6.46%, and through assessment of panoramic radiography and CT or CBCT, the frequency of the variations was 4.20% and 16.25%, respectively.
Appendix A Search strategy in databases
1. Cochrane
(tw: ((retromolar AND canal*) OR (foramen AND retromolar) OR (mandibular AND nerve) OR (bifid AND mandibular AND canal*) OR (inferior AND alveolar AND nerve))) AND (tw: (pantomograph* OR orthopantomograph* OR panoramic OR tomograph* OR “cbct” OR “cone beam” OR “ct scan*” OR “volume* ct” OR “volume* computed” OR “spiral ct*” OR “ct* spiral” OR “spiral computed” OR “ct image*” OR “helical ct*” OR “helical computed” OR “spiral cat scan*” OR “spiral scan*” OR “spiral ct”)) AND (instance:“regional”) AND (collection: (“02-cochrane”)) (retromolar AND canal*) OR (foramen AND retromolar) OR (mandibular AND nerve) OR (bifid AND mandibular AND canal*) OR (inferior AND alveolar AND nerve)
AND
(Pantomograph* OR Orthopantomograph* OR Panoramic OR Tomograph* OR “CBCT” OR “cone beam” OR “ct scan*” OR “volume* ct” OR “volume* computed” OR “spiral ct*” OR “ct* spiral” OR “spiral computed” OR “ct image*” OR “helical ct*” OR “helical computed” OR “spiral cat scan*” OR “spiral scan*” OR “spiral ct”)
2. Lilacs
(retromolar AND canal*) OR (foramen AND retromolar) OR (mandibular AND nerve*) OR (bifid AND mandibular AND canal*) OR (inferior AND alveolar AND nerve*) OR (cana* AND retromolar*) OR (forame AND retromolar*) OR (nervo AND mandibular) OR (cana* AND mandibular* AND nervo*) OR (nervo* AND alveolar* AND inferior*) AND (“Radiografia Panorâmica” OR “radiography, panoramic” OR Pantomografia* OR ortopantomografia* OR Panoramica* OR “tomography, X-ray computed” OR “Tomografia Computadorizada por Raios X“ OR “cone-beam CT” OR “Tomografia Computadorizada de Feixe Cônico” OR “tomography, spiral computed” OR “Tomografia Computadorizada Espiral” OR tomografia* OR “feixe conico” OR espiral OR helicoidal OR Tomograph* OR “cone beam” OR “ct scans” OR “ct scan” OR “volumetric ct” OR “volume ct” OR “volumetric computed” OR “volume computed” OR “spiral ct” OR “spiral cts” OR “ct spiral” OR “spiral computed” OR “ct images” OR “ct image” OR “helical ct” OR “helical cts” OR “helical computed” OR “spiral cat scan” OR “spiral cat scans” OR “spiral scan” OR “spiral scans” OR “spiral CT”)
3. ProQuest
(“retromolar” AND “canal*”) OR (“foramen” AND “retromolar”) OR (“mandibular” AND “nerve”) OR (“bifid” AND “mandibular” AND “canal*”) OR (“inferior” AND “alveolar” AND “nerve”) AND ((Pantomograph* OR Orthopantomograph* OR Panoramic) OR (Tomograph* OR “cone beam” OR “ct scan*” OR “volume* ct” OR “volume* computed”) OR (“spiral ct*” OR “ct* spiral” OR “spiral computed” OR “ct image*” OR “helical ct*” OR “helical computed” OR “spiral cat scan*” OR “spiral scan*” OR “spiral ct”))
4. PubMed
(“retromolar” AND (“canal” OR “canals”)) OR (“foramen” AND “retromolar”) OR (“mandibular” AND “nerve”) OR (“bifid” AND “mandibular” AND (“canal” OR “canals”)) OR (“inferior” AND “alveolar” AND “nerve”) AND ((Pantomography OR Pantomographies OR Orthopantomography OR Orthopantomographies OR Panoramic) OR (Tomography OR tomographies OR “cone beam” or “CBCT” OR “ct scans” OR “ct scan” OR “volumetric ct” OR “volume ct” OR “volumetric computed” OR “volume computed”) OR (“spiral ct” OR “spiral cts” OR “ct spiral” OR “spiral computed” OR “ct images” OR “ct image” OR “helical ct” OR “helical cts” OR “helical computed” OR “spiral cat scan” OR “spiral cat scans” OR “spiral scan” OR “spiral scans” OR “spiral CT”))
5. Scopus
((“retromolar” W/5 “canal*”) OR (“foramen” W/5 “retromolar”) OR (“mandibular” W/5 “nerve”) OR (“bifid” W/5 “mandibular” W/5 “canal*”) OR (“inferior” W/5 “alveolar” W/5 “nerve”)) AND ((Pantomograph* OR Orthopantomograph* OR Panoramic) OR (tomograph* OR “CBCT” OR “cone beam” OR “ct scan*” OR “volume* ct” OR (“volume* W/5 computed”)) OR (“spiral ct*” OR “ct* spiral” OR “spiral computed” OR “ct image*” OR “helical ct*” OR “helical computed” OR “spiral cat scan*” OR “spiral scan*” OR “spiral ct”))
6. Web of Science
(“retromolar” AND “canal*”) OR (“foramen” AND “retromolar”) OR (“mandibular” AND “nerve”) OR (“bifid” AND “mandibular” AND “canal*”) OR (“inferior” AND “alveolar” AND “nerve”) AND ((Pantomograph* OR Orthopantomograph* OR Panoramic) OR (Tomograph* OR “CBCT” OR “cone beam” OR “ct scan*” OR “volume* ct” OR “volume* computed”) OR (“spiral ct*” OR “ct* spiral” OR “spiral computed” OR “ct image*” OR “helical ct*” OR “helical computed” OR “spiral cat scan*” OR “spiral scan*” OR “spiral ct”))
Appendix B Articles excluded and reasons for exclusion
Table A1.
Articles excluded and the reasons for exclusion
| Author | Reasons for exclusion |
|---|---|
| 1. Akhtar et al 2014 | 4 |
| 2. Bilecenoglu and Tuncer 2006 | 4 |
| 3. Correr et al 2013 | 4 |
| 4. Driscoll 1990 | 1 |
| 5. Fernandes et al 2013 | 4 |
| 6. Fu et al 2012 | 4 |
| 7. Kawai et al 2012 | 4 |
| 8. Kiersch and Jordan 1973 | 1 |
| 9. Kim et al 2011 | 3 |
| 10. Kumar and Kesavi 2010 | 4 |
| 11. Kuribayashi et al 2010 | 4 |
| 12. Leite et al 2014 | 4 |
| 13. Lizio et al 2013 | 4 |
| 14. López-Videla Montano et al 2010 | 4 |
| 15. Motta-Junior et al 2012 | 4 |
| 16. Naitoh et al 2009 | 4 |
| 17. Naitoh et al 2010 | 4 |
| 18. Narayana et al 2002 | 3 |
| 19. Neves et al 2014 | 4 |
| 20. Oliveira-Santos et al 2012 | 4 |
| 21. Orhan et al 2011 | 4 |
| 22. Patil et al 2013 | 4 |
| 23. Patterson and Funke et al 1973 | 1 |
| 24. Perin et al 2004 | 1 |
| 25. Pyle et al 1999 | 5 |
| 26. Rossi et al 2012 | 4 |
| 27. Sawyer and Kiely 1991 | 5 |
| 28. Shantharam et al 2013 | 4 |
| 29. Von arx et al 2011 | 4 |
(1) Reviews, case reports, letters and personal opinions; (2) sample includes subjects with pathologies, craniofacial syndrome, previous orthognathic or craniofacial surgery; (3) other methods such as micro-CT and angiography; (4) studies with minimum population of 300 subjects; and (5) not available.
References
- 1. Akhtar MJ, et al. A morphological study of retromolar foramen and canal in indian dried mandibles. Journal of Evolution of Medical and Dental Sciences, v. 3, n. 58, 2014.
- 2. Bilecenoglu, B.; Tuncer, N. Clinical and anatomical study of retromolar foramen and canal. In: (Ed.). J Oral Maxillofac Surg United States, v. 64, 2006. p.1493–7. [DOI] [PubMed]
- 3. Correr GM. et al. Classification of bifid mandibular canals using cone beam CT. Braz Oral Res, v. 27, n. 6, p. 510–6, Nov-December 2013. ISSN 1806–8324. [DOI] [PubMed]
- 4. Driscoll, C. F. Bifid mandibular canal. Oral Surg Oral Med Oral Pathol, v. 70, n. 6, p. 807, December 1990. [DOI] [PubMed]
- 5. Fernandes, L. M. P. d. S. R. et al. Variações anatômicas do canal mandibular detectadas em imagens de tomografia computadorizada de feixe cônico. ImplantNews, v. 10, n. 3, p. 757–760, 2013.
- 6. Fu E. et al. Bifid mandibular canals and the factors associated with their presence: a medical CT evaluation in a Taiwanese population. Clin Oral Implants Res, v. 25, n. 2, p. e64–7, February 2014. [DOI] [PubMed]
- 7. KawaiT. et al. Observation of the retromolar foramen and canal of the mandible: a CBCT and macroscopic study. Oral Radiol, v. 28, p. 10–14, 2012.
- 8. Kiersch, TA.; JordanJ. E. Duplication of the mandibular canal. Oral Surg Oral Med Oral Pathol, v. 35, n. 1, p. 133–4, January 1973. ISSN 0030–4220 (Print) 0030–4220. [DOI] [PubMed]
- 9. Kim MS. et al. A false presence of bifid mandibular canals in panoramic radiographs. Dentomaxillofac Radiol, v. 40, n. 7, p. 434–8, October 2011. [DOI] [PMC free article] [PubMed]
- 10. Kumar SS.; D., K. A Study on the incidence of Retromolar Foramen and Canal in Indian Dried Human Mandibles and its Clinical Significance. International Journal of Anatomical Sciences, v. 1, p. 14–16, 2010.
- 11. Kuribayashi A. et al. Bifid mandibular canals: cone beam CT evaluation. Dentomaxillofac Radiol, v. 39, n. 4, p. 235–9, May 2010. [DOI] [PMC free article] [PubMed]
- 12. Leite GM. et al. Anatomic variations and lesions of the mandibular canal detected by cone beam CT. Surg Radiol Anat, v. 36, n. 8, p. 795–804, October 2014. ISSN 0930–1038. [DOI] [PubMed]
- 13. Lizio G. et al. Radiographic assessment of the mandibular retromolar canal using cone-beam CT. Acta Odontol Scand, v. 71, n. 3–4, p. 650–5, May-July 2013. [DOI] [PubMed]
- 14. López-Videla Montano, J. et al. Prevalencia de variables anatómicas en el recorrido de los conductos mandibulares. Estudio mediante tecnología cone beam. Rev Fac Odontol Univ Antioq, v. 22, n. 1, p. 23–32, 2010.
- 15. Motta-Junior J. et al. Forame retromolar: sua repercussão clínica e avaliação de 35 mandíbulas secas. Rev Odontol UNESP, v. 41, n. 3, p. 164–168, 2012.
- 16. Naitoh M. et al. Observation of bifid mandibular canal using cone-beam CT. Int J Oral Maxillofac Implants, v. 24, n. 1, p. 155–9, Jan-February 2009. [PubMed]
- 17. Naitoh M. et al. Comparison between cone-beam and multislice CT depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, v. 109, n. 1, p. e25–31, January 2010. ISSN 1079–2104. [DOI] [PubMed]
- 18. Narayana K et al. The retromolar foramen and canal in south Indian dry mandibles. Eur J Anat. 6 141–6 p. 2002.
- 19. Neves FS. et al. Comparative analysis of mandibular anatomical variations between panoramic radiography and cone beam CT. Oral Maxillofac Surg, v. 18, n. 4, p. 419–24, December 2014. [DOI] [PubMed]
- 20. de Oliveira-Santos C et al. Assessment of variations of the mandibular canal through cone beam CT. Clin Oral Investig, v. 16, n. 2, p. 387–93, Apr 2012. ISSN 1432–6981. [DOI] [PubMed]
- 21. Orhan K et al. Evaluation of bifid mandibular canals with cone-beam CT in a Turkish adult population: a retrospective study. Surg Radiol Anat, v. 33, n. 6, p. 501–7, August 2011. [DOI] [PubMed]
- 22. Patil S. et al. Retromolar canals as observed on cone-beam CT: their incidence, course, and characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol, v. 115, n. 5, p. 692–9, May 2013. [DOI] [PubMed]
- 23. Patterson JE.; Funke FW. Bifid inferior alveolar canal. Oral Surg Oral Med Oral Pathol, v. 36, n. 2, p. 287–8, August 1973. [DOI] [PubMed]
- 24. Perin CP. et al. Importância das variações anatômicas dos canais mandibulares e suas implicações clínicas. JBC J Bras Clin Odontol Integr 8 : 144–6 p. 2004.
- 25. Pyle MA et al. Perineural spread of squamous cell carcinoma of the lip: the importance of follow-up and collaboration. Spec Care Dentist, v. 19, n. 3, p. 118–22, May-June 1999. [DOI] [PubMed]
- 26. Rossi AC. et al. Incidence of Retromolar Foramen in Human Mandibles:Ethnic and Clinical Aspects. Int J Morphol, v. 30, n. 3, p. 1074–1078, 2012.
- 27. Sawyer DR.; Kiely M L. Retromolar foramen: a mandibular variant important to dentistry. Ann Dent, v. 50, n. 1, p. 16-8, Summer 1991. [PubMed]
- 28. Shantharam V et al. Retromolar Foramen in South Indian Mandibles. Anatomica Karnataka, v. 7, n. 1, 2013.
- 29. von Arx T et al. Radiographic study of the mandibular retromolar canal: an anatomic structure with clinical importance. J Endod, v. 37, n. 12, p. 1630–5, December 2011. [DOI] [PubMed]
Appendix C Prevalence critical appraisal tool criteria fulfilled (The Joanna Briggs Institute, 2014)
| Item | Choi and Han, 201429 | Devito and Tamburús, 200130 | Han and Hwang, 201431 | Kang et al, 201432 | Khan et al, 201333 | Kuczynski et al, 201434 | Langlais et al, 198521 | Nortje et al, 19773 | Ossenberg, 198728 | Rashsuren et al, 201435 | Rossi et al, 200936 | Salvador et al, 201037 | Sanchis et al, 200318 | Schilling et al, 201039 | Shen et al, 201438 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Was the study based on a random or pseudorandom sample? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 2 Were the criteria for inclusion in the sample clearly defined? | N | Y | N | N | Y | Y | N | Y | N | N | N | Y | N | Y | N |
| 3 Were confounding factors identified and strategies to deal with them stated? | N | N | N | N | N | N | N | N | N | N | N | N | N | N | N |
| 4 Were outcomes assessed using objective criteria? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | U | Y | Y |
| 5 If comparisons are being made, was there sufficient description of the groups? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | U | NA | NA |
| 6 Was the follow-up carried out over a sufficient time period? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 7 Were the outcomes of people who withdrew described and included in the analysis? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 8 Were the outcomes measured in a reliable way? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 9 Was an appropriate statistical analysis used? | NA | NA | Y | Y | Y | NA | Y | NA | NA | Y | NA | NA | NA | NA | NA |
| % yes/risk | 33.33, high | 44.44, high | 44.44, high | 44.44, high | 55.55, moderate | 44.44, high | 44.44, high | 44.44, high | 33.33, high | 44.44, high | 33.33, high | 44.44, high | 22.22, high | 44.44, high | 33.33, high |
N, no; NA, not applicable; U, unclear; Y, yes.
Contributor Information
Letícia F Haas, Email: leticia_haas@hotmail.com.
Kamile Dutra, Email: kamileldutra@gmail.com.
André Luís Porporatti, Email: andreporporatti@yahoo.com.br.
Luis A Mezzomo, Email: lmezzomo@hotmail.com.
Graziela De Luca Canto, Email: graziela.canto@ufsc.br.
Carlos Flores-Mir, Email: carlosflores@ualberta.ca.
Márcio Corrêa, Email: profmarcioufsc@gmail.com.
References
- 1.Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants 2009; 24: 155–9. [PubMed] [Google Scholar]
- 2.Kiersch TA, Jordan JE. Duplication of the mandibular canal. Oral Surg Oral Med Oral Pathol 1973; 35: 133–4. doi: 10.1016/0030-4220(73)90107-2 [DOI] [PubMed] [Google Scholar]
- 3.Nortje CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg 1977; 15: 55–63. [DOI] [PubMed] [Google Scholar]
- 4.Wadu SG, Penhall B, Townsend GC. Morphological variability of the human inferior alveolar nerve. Clin Anat 1997; 10: 82–7. doi: [DOI] [PubMed] [Google Scholar]
- 5.Juodzbalys G, Wang HL, Sabalys G. Anatomy of mandibular vital structures. Part I mandibular canal and inferior alveolar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res 2010; 1: e2. doi: 10.5037/jomr.2010.1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacobs R, Lambrichts I, Liang X, Martens W, Mraiwa N, Adriaensens P, et al. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 683–93. [DOI] [PubMed] [Google Scholar]
- 7.Kalantar Motamedi MH, Navi F, Sarabi N. Bifid mandibular canals: prevalence and implications. J Oral Maxillofac Surg 2015; 73: 387–390. doi: 10.1016/j.joms.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 8.Fu E, Peng M, Chiang CY, Tu HP, Lin YS, Shen EC. Bifid mandibular canals and the factors associated with their presence: a medical computed tomography evaluation in a taiwanese population. Clin Oral Implants Res 2014; 25: 64–7. doi: 10.1111/clr.12049 [DOI] [PubMed] [Google Scholar]
- 9.Bilecenoglu B, Tuncer N. Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg 2006; 64: 1493–7. doi: 10.1016/j.joms.2006.05.043 [DOI] [PubMed] [Google Scholar]
- 10.Fukami K, Shiozaki K, Mishima A, Kuribayashi A, Hamada Y, Kobayashi K. Bifid mandibular canal: confirmation of limited cone beam CT findings by gross anatomical and histological investigations. Dentomaxillofac Radiol 2012; 41: 460–5. doi: 10.1259/dmfr/60245722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawai T, Asaumi R, Sato I, Kumazawa Y, Yosue T. Observation of the retromolar foramen and canal of the mandible: a CBCT and macroscopic study. Oral Radiol 2012; 28: 10–14. doi: 10.1007/s11282-011-0074-9 [DOI] [Google Scholar]
- 12.Teerijoki-Oksa T, Jääskeläinen SK, Forssell K, Forssell H, Vähätalo K, Tammisalo T, et al. Risk factors of nerve injury during mandibular sagittal split osteotomy. Int J Oral Maxillofac Surg 2002; 31: 33–9. doi: 10.1054/ijom.2001.0157 [DOI] [PubMed] [Google Scholar]
- 13.Silva FM, Cortez AL, Moreira RW, Mazzonetto R. Complications of intraoral donor site for bone grafting prior to implant placement. Implant Dent 2006; 15: 420–6. doi: 10.1097/01.id.0000246225.51298.67 [DOI] [PubMed] [Google Scholar]
- 14.Wadhwani P, Mathur RM, Kohli M, Sahu R. Mandibular canal variant: A case report. J Oral Pathol Med 2008; 37: 122–4.doi: 10.1111/j.1600-0714.2007.00573.x [DOI] [PubMed] [Google Scholar]
- 15.Claeys V, Wackens G. Bifid mandibular canal: literature review and case report. Dentomaxillofac Radiol 2005; 34: 55–8. doi: 10.1259/dmfr/23146121 [DOI] [PubMed] [Google Scholar]
- 16.Kaufman E, Serman NJ, Wang PD. Bilateral mandibular accessory foramina and canals: a case report and review of the literature. Dentomaxillofac Radiol 2000; 29: 170–5. doi: 10.1038/sj/dmfr/4600526 [DOI] [PubMed] [Google Scholar]
- 17.Renton T, Dawood A, Shah A, Searson L, Yilmaz Z. Post-implant neuropathy of the trigeminal nerve. A case series. Br Dental J 2012; 212: E17. doi: 10.1038/sj.bdj.2012.497 [DOI] [PubMed] [Google Scholar]
- 18.Sanchis JM, Peñarrocha M, Soler F. Bifid mandibular canal. J Oral Maxillofac Surg 2003; 61: 422–4. doi: 10.1053/joms.2003.50004 [DOI] [PubMed] [Google Scholar]
- 19.Yeong-Hoon K, Hun-Mu Y. Conventional panoramic radiograph cannot identify the bifid mandibular canal. J Craniofac Surg 2015; 26: e674–5. doi: 10.1097/SCS.0000000000002058 [DOI] [PubMed] [Google Scholar]
- 20.Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg 1983; 41: 177–9. doi: 10.1016/0278-2391(83)90076-9 [DOI] [PubMed] [Google Scholar]
- 21.Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc 1985; 110: 923–6. doi: 10.14219/jada.archive.1985.0033 [DOI] [PubMed] [Google Scholar]
- 22.Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T. Bifid mandibular canals: cone beam computed tomography evaluation. Dentomaxillofac Radiol 2010; 39: 235–9. doi: 10.1259/dmfr/66254780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orhan K, Aksoy S, Bilecenoglu B, Sakul BU, Paksoy CS. Evaluation of bifid mandibular canals with cone-beam computed tomography in a turkish adult population: a retrospective study. Surg Radiol Anat 2011; 33: 501–7. doi: 10.1007/s00276-010-0761-y [DOI] [PubMed] [Google Scholar]
- 24.Muinelo-Lorenzo J, Suárez-Quintanilla JA, Fernández-Alonso A, Marsillas-Rascado S, Suárez-Cunqueiro MM. Descriptive study of the bifid mandibular canals and retromolar foramina: cone beam CT vs panoramic radiography. Dentomaxillofac Radiol 2014; 43: 20140090. doi: 10.1259/dmfr.20140090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Reprint-preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther 2009; 89: 873–80. [PubMed] [Google Scholar]
- 26.Lwanga SK, Lemeshow S. Sample size determination in health studies: a practical manual. Geneva, Switzerland: World Health Organization; 1991. [Google Scholar]
- 27.Deeks JJ PHJ, Altman DG. Chapter. analysing data and undertaking meta-analyses. In: Mrc biostatistics unit c, united kingdom, australasian cochrane centre mu, melbourne, australia, eds. Cochrane handbook for systematic reviews of interventions: Cochrane book series. The cochrane collaboration 2008. pp. 54. [Google Scholar]
- 28.Ossenberg NS. Retromolar foramen of the human mandible. Am J Phys Anthropol 1987; 73: 119–28. doi: 10.1002/ajpa.1330730112 [DOI] [PubMed] [Google Scholar]
- 29.Choi YY, Han SS. Double mandibular foramen leading to the accessory canal on the mandibular ramus. Surg Radiol Anat 2014; 36: 851–5. doi: 10.1007/s00276-014-1310-x [DOI] [PubMed] [Google Scholar]
- 30.Devito KL, Tambúrus JR. Anatomia do canal da mandíbula: classificação radiográfica das variações. Revista da APCD 2001; 55: 261–6. [Google Scholar]
- 31.Han SS, Hwang YS. Cone beam CT findings of retromolar canals in a korean population. Surg Radiol Anat 2014; 36: 871–6. doi: 10.1007/s00276-014-1262-1 [DOI] [PubMed] [Google Scholar]
- 32.Kang JH, Lee KS, Oh MG, Choi HY, Lee SR, Oh SH, et al. The incidence and configuration of the bifid mandibular canal in Koreans by using cone-beam computed tomography. Imaging Sci Dent 2014; 44: 53–60. doi: 10.5624/isd.2014.44.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khan MA, Agarwal S, Mandloi RS. Prevalence of retromolar foramen in dried mandible along with morphometric and analytical study in north india. Natl J Med Dental Res 2013; 2: 11–14. [Google Scholar]
- 34.Kuczynski A, Kucharski W, Franco A, Westphalen FH, de Lima AA, Fernandes Â. Prevalence of bifid mandibular canals in panoramic radiographs: a maxillofacial surgical scope. Surg Radiol Anat 2014; 36: 847–50. doi: 10.1007/s00276-014-1298-2 [DOI] [PubMed] [Google Scholar]
- 35.Rashsuren O, Choi JW, Han WJ, Kim EK. Assessment of bifid and trifid mandibular canals using cone-beam computed tomography. Imaging Sci Dent 2014; 44: 229–36. doi: 10.5624/isd.2014.44.3.229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rossi PM, Brücker MR, Rockenbach MIB. Canais mandibulares bifurcados: análise em radiografias panorâmicas. Rev Ciênc Méd 2009; 18: 99–104. [Google Scholar]
- 37.Salvador JF, Medeiros PL, Ferreira Junior O, Capelozza ALA. Anatomia radiográfica do canal mandibular e suas variações em radiograficas panorâmicas. Innov Implant J, Biomater Esthet 2010; 5: 19–24. [Google Scholar]
- 38.Shen EC, Fu E, Fu MM, Peng M. Configuration and corticalization of the mandibular bifid canal in a taiwanese adult population: a computed tomography study. Int J Oral Maxillofac Implants 2014; 29: 893–7. doi: 10.11607/jomi.3435 [DOI] [PubMed] [Google Scholar]
- 39.Schilling Lara J, Quezada AS, Valenzuela JSP. Mandibular canal duplication prevalence, digital panoramic radiography analysis. Int J Odontostomat 2010; 4: 207–13. doi: 10.4067/S0718-381X2010000300001 [DOI] [Google Scholar]
- 40.Rossi AC, Freire AR, Prado GB, Prado FB, Botacin PR, Caria PHF. Incidence of retromolar foramen in human mandibles:Ethnic and clinical aspects. Int J Morphol 2012; 30: 1074–8. doi: 10.4067/S0717-95022012000300051 [DOI] [Google Scholar]
- 41.Shantharam V, Manjunath KY, Aruna N, Shastri D. Retromolar foramen in south indian mandibles. Anatomica Karnataka 2013; 7: 34–7. [Google Scholar]
- 42.Priya R, Manjunath KY, Balasubramanyam. Retromolar foramen. Indian J Dent Res 2005; 16: 15–16. [PubMed] [Google Scholar]
- 43.Neves FS, Nascimento MC, Oliveira ML, Almeida SM, Bóscolo FN. Comparative analysis of mandibular anatomical variations between panoramic radiography and cone beam computed tomography. Oral Maxillofac Surg 2014; 18: 419–24. doi: 10.1007/s10006-013-0428-z [DOI] [PubMed] [Google Scholar]
- 44.Auluck A, Pai KM, Shetty C. Pseudo bifid mandibular canal. Dentomaxillofac Radiol 2005; 34: 387–8. doi: 10.1259/dmfr/59445082 [DOI] [PubMed] [Google Scholar]
- 45.Arensburg B, Nathan H. Anatomical observations on the mylohyoid groove, and the course of the mylohyoid nerve and vessels. J Oral Surg 1979; 37: 93–6. [PubMed] [Google Scholar]
- 46.White S, Pharoah M. Oral radiology—principles and interpretation. 5th edn. Rio de Janeiro, Brazil: Elsevier; 2007. [Google Scholar]
- 47.Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e25–31. doi: 10.1016/j.tripleo.2009.08.027 [DOI] [PubMed] [Google Scholar]
- 48.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc 2006; 72: 75–80. [PubMed] [Google Scholar]
- 49.Kodera H, Hashimoto I. A case of mandibular retromolar canal: elements of nerves and arteries in this canal. [In Japanese] Kaibogaku Zasshi 1995; 70: 23–30. [PubMed] [Google Scholar]
- 50.Anderson LC, Kosinski TF, Mentag PJ. A review of the intraosseous course of the nerves of the mandible. J Oral Implantol 1991; 17: 394–403. [PubMed] [Google Scholar]
- 51.Jablonski NG, Cheng CM, Cheng LC, Cheung HM. Unusual origins of the buccal and mylohyoid nerves. Oral Surg Oral Med Oral Pathol 1985; 60: 487–8. doi: 10.1016/0030-4220(85)90235-X [DOI] [PubMed] [Google Scholar]
- 52.Rouas P, Nancy J, Bar D. Identification of double mandibular canals: literature review and three case reports with CT scans and cone beam CT. Dentomaxillofac Radiol 2007; 36: 34–8. doi: 10.1259/dmfr/27374727 [DOI] [PubMed] [Google Scholar]
- 53.Lew K, Townsen G. Failure to obtain adequate anaesthesia associated with a bifid mandibular canal: a case report. Aust Dent J 2006; 51: 86–90. doi: 10.1111/j.1834-7819.2006.tb00406.x [DOI] [PubMed] [Google Scholar]
- 54.Mizbah K, Gerlach N, Maal TJ, Bergé SJ, Meijer GJ. The clinical relevance of bifid and trifid mandibular canals. Oral Maxillofac Surg 2012; 16: 147–51. doi: 10.1007/s10006-011-0278-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DeSantis JL, Liebow C. Four common mandibular nerve anomalies that lead to local anesthesia failures. J Am Dent Assoc 1996; 127: 1081–6. doi: 10.14219/jada.archive.1996.0333 [DOI] [PubMed] [Google Scholar]
- 56.Moiseiwitsch JR. Position of the mental foramen in a North American, white population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 85: 457–60. doi: 10.1016/S1079-2104(98)90074-9 [DOI] [PubMed] [Google Scholar]
- 57.al Jasser NM, Nwoku AL. Radiographic study of the mental foramen in a selected Saudi population. Dentomaxillofac Radiol 1998; 27: 341–3. doi: 10.1038/sj/dmfr/4600388 [DOI] [PubMed] [Google Scholar]
- 58.de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig 2012; 16: 387–93. doi: 10.1007/s00784-011-0544-9 [DOI] [PubMed] [Google Scholar]
- 59.Correr GM, Iwanko D, Leonardi DP, Ulbrich LM, Araújo MR, Deliberador TM. Classification of bifid mandibular canals using cone beam computed tomography. Braz Oral Res 2013; 27: 510–16. doi: 10.1590/S1806-83242013000600011 [DOI] [PubMed] [Google Scholar]
- 60.Lizio G, Pelliccioni GA, Ghigi G, Fanelli A, Marchetti C. Radiographic assessment of the mandibular retromolar canal using cone-beam computed tomography. Acta Odontol Scand 2013; 71: 650–5. doi: 10.3109/00016357.2012.704393 [DOI] [PubMed] [Google Scholar]
- 61.Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 2009; 71: 461–8. doi: 10.1016/j.ejrad.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 62.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice ct (MSCT) Part I. On subjective image quality. Eur J Radiol 2010; 75: 265–9. doi: 10.1016/j.ejrad.2009.03.042 [DOI] [PubMed] [Google Scholar]
- 63.Imada TS, Fernandes LM, Centurion BS, de Oliveira-Santos C, Honorio HM, Rubira-Bullen IR. Accessory mental foramina: prevalence, position and diameter assessed by cone-beam computed tomography and digital panoramic radiographs. Clin Oral Implants Res 2014; 25: e94–9. doi: 10.1111/clr.12066 [DOI] [PubMed] [Google Scholar]