Abstract
Process mapping, often used as part of the human factors and systems engineering approach to improve care delivery and outcomes, should be expanded to represent the complex, interconnected sociotechnical aspects of health care. Here, we propose a new sociotechnical process modeling method to describe and evaluate processes, using the SEIPS model as the conceptual framework. The method produces a process map and supplementary table, which identify work system barriers and facilitators. In this paper, we present a case study applying this method to three primary care processes. We used purposeful sampling to select staff (care managers, providers, nurses, administrators and patient access representatives) from two clinics to observe and interview. We show the proposed method can be used to understand and analyze healthcare processes systematically and identify specific areas of improvement. Future work is needed to assess usability and usefulness of the SEIPS-based process modeling method and further refine it.
Keywords: Sociotechnical systems, Process mapping, Primary care
1. Introduction
The last decades in health care have been transformative, focused on improving quality of care and patient safety initiated by the US Institute of Medicine report “To Err is Human: Building a Better Health System” (Kohn, Corrigan & Donaldson, 1999). Healthcare delivery is in need of redesign to meet the needs of patients while providing safe, effective and efficient care (Institute of Medicine, 2001). Despite considerable efforts and substantial resources to improve patient safety, the results of the investment to date are equivocal and the need for successful and sustained redesigns remains (Agency for Healthcare Research and Quality, 2015). Health care remains focused on individual tasks, as do many improvement initiatives; only when the focus is shifted to support and add value to processes will quality of care truly improve (Walker & Carayon, 2009).
A systems engineering approach has been proposed to improve healthcare quality and patient safety (Kaplan et al., 2013; President’s Council of Advisors on Science and Technology, 2014; Reid et al., 2005). Human factors engineering, in particular, has gained increasing recognition and can provide system design methods to address the needs and desires of stakeholders in the healthcare system and other important sociotechnical aspects of health care (Gurses, Ozok & Pronovost, 2011; Reid et al., 2005). As Walker and Carayon (2009, p. 471) note, “Human-factors engineering (HFE, the application of knowledge regarding human characteristics to the design of work systems) can provide theoretical and pragmatic guidance to process design.” It is important to shift from task-level to process-level analysis (Carayon, Hancock, et al., 2015; Hettinger et al., 2015).
HFE methods can be utilized to design safer and more efficient processes, resulting in improved patient care quality and provider satisfaction (Walker & Carayon, 2009; Xie & Carayon, 2015). HFE-based process-level analyses are particularly valuable and applicable in primary care where patients experience a wide range of complex, inter-connected care processes. Process modeling methods can be used to document and establish a shared understanding of existing processes; this can be leveraged to identify improvement areas (Jun et al., 2009; Siemieniuch & Sinclair, 2005). The terminology associated with this work has varied, and “workflow” is increasingly used interchangeably with “process”; the term used in the original articles is used in this literature review. In the remainder of the paper, we suggest and use “process.”
2. HFE-based Process Modeling in Health Care
Early process design research was conducted in structured manufacturing environments (Siemieniuch & Sinclair, 2005). Researchers have developed and refined approaches to study increasingly complex workflows, such as those in health care (Unertl et al., 2010). Workflow-modeling methods have been developed and used in other complex industries, but health care has not used these methods systematically (Jun et al., 2009; Unertl et al., 2010). Jun et al. (2009) evaluated eight modeling methods for three healthcare processes:
Patient discharge from a ward
Primary care diabetic patient care
Prostate cancer diagnostic procedure in a hospital.
Clinical and non-clinical staff evaluated the following workflow modeling methods based on familiarity with, usability and utility of the method:
Stakeholder diagrams
Information diagrams
Process content diagrams
Flowcharts
Swim lane activity diagrams
State transition diagrams
Communication diagrams
Data flow diagrams.
According to Jun et al. (2009), the first three methods show hierarchical links between stakeholders, information and activities; the next three preserve temporal links between activities; and the last two show inputs and outputs between stakeholders and activities. Flowcharts and swim lane activity diagrams were found to be the most commonly used, and flowcharts were found to be the most usable and useful of the methods evaluated. Ultimately, all methods were found to produce simplified representations of reality and none could effectively capture all aspects of the complex workflows found in healthcare (Jun et al., 2009).
Jun and colleagues (2010) extended this work and evaluated two additional methods: sequence diagrams and Integrated Definition for Function Modeling (IDFM). They also characterized each method based on the focus of the method (activity, stakeholder and information) and linkage type (hierarchical, sequential and information) in order to educate healthcare workers on methods available and their similarities and differences. Healthcare workers were most familiar with flowcharts. The researchers argue that greater use of modeling methods will lead to a better system understanding, especially considering the complexity and diversity of healthcare systems.
Examples of process mapping abound. Risk management projects especially use process mapping to identify vulnerabilities in processes, such as the healthcare failure mode and effects analysis (FMEA); an example of an FMEA can be found in van Tilburg et al. (2006). Flow diagrams showed the proportion of high-risk failures to total potential failure modes of each process step in ordering and administration of chemotherapy in a pediatric oncology unit. Medication ordering and administration processes in hospitals and outpatient care have been described using process mapping (Beuscart-Zéphir et al., 2007; Johnson & Fitzhenry, 2006). The ordering of diagnostic tests and physician interactions with technology have also been studied with process mapping in outpatient settings (Asan, Chiou & Montague, 2014; Hallock, Alper & Karsh, 2006). Unertl and colleagues used process mapping to compare work and information flow across multiple clinics (Unertl et al., 2009) and to look for patterns in health information exchange use across hospitals and clinics (Unertl, Johnson & Lorenzi, 2012). Eason and colleagues (2012) mapped care pathways to study the use of electronic patient information systems to span organizational boundaries. This analysis focused on the entire patient care process, therefore including various organizations and examining interdependencies related to crossing organizational boundaries (Eason et al., 2012). Some studies have modeled workflow of multiple clinicians providing care for individual patients, such as in emergency departments (Laxmisan et al., 2007; Ozkaynak & Brennan, 2013) and hospital admissions (Benyoucef et al., 2011; Puentes et al., 2012). Process mapping has also been used to study communication processes (Kummerow Broman et al., 2015) and interruptions (Brixey et al., 2008).
As these examples demonstrate, process modeling is increasingly used in health care. However, current process models may not systematically capture information on all work system elements (Carayon, 2009; Smith & Carayon-Sainfort, 1989) and may not adequately represent the complex, interconnected sociotechnical aspects of health care (Jun et al., 2009). These methods tend to be primarily used for descriptive purposes but not evaluation, i.e. to identify what is working or not working in the process; one exception is proactive risk analysis such as failure mode and effects analysis (Carayon, Faye, et al., 2011). HFE can help to gain a complete understanding of the process and associated work system (Carayon, Schultz & Hundt, 2004; Walker & Carayon, 2009). In this paper, we propose a new process modeling method to describe and evaluate processes by representing the sociotechnical aspects of the process. The Systems Engineering Initiative for Patient Safety (SEIPS) model (Carayon et al., 2006; Carayon, Wetterneck, et al., 2014) is used as the conceptual framework for the proposed method. A systems approach is needed to ensure all work system elements are considered in the process analysis. We present a case study to demonstrate the application of the SEIPS-based process modeling method and discuss directions for future work.
3. The SEIPS Model as a Conceptual Framework for Process Modeling
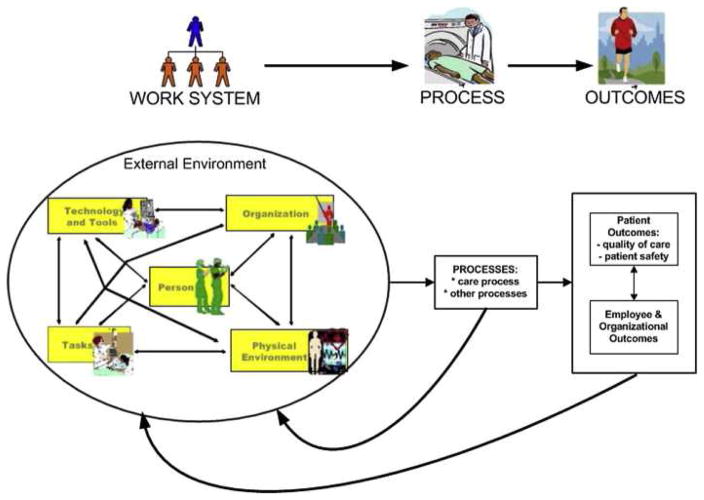
The SEIPS model integrates human factors and healthcare models to propose a systems engineering model to understand the care process by representing all work system elements; this model provides a representation of the complexities of health care (Carayon et al., 2006). The work system in the SEIPS model is composed of six elements and interactions between the elements (Carayon et al., 2006; Carayon, Wetterneck, et al., 2014; Smith & Carayon-Sainfort, 1989) (see Figure 1):
Figure 1.
The SEIPS model of work system and patient safety (Carayon, Wetterneck, et al., 2014)
People, including the patient, their family and/or caregivers and health care professionals involved in the process
Tasks, which are goal-oriented activities within the process
Tools and technologies, including health information technology and other tools used in the process
Organization, including characteristics such as the culture, rules, procedures, management and leadership
Physical environment, including layout, lighting, noise and distractions
External environment, including payment, care delivery and legal and reporting systems.
A process is a “set of interrelated or interacting activities that use inputs to deliver an intended result” (ISO, 2015). In health care, outcomes include (1) patient outcomes, including quality of care and patient safety, and (2) employee and organizational outcomes such as job satisfaction and stress (Carayon et al., 2006; Carayon, Wetterneck, et al., 2014; Schultz et al., 2005). The work system can be used to describe a care process as: “a series of tasks performed by individuals using various tools and technologies in a specific environment” in an organized way (Carayon, Wetterneck, et al., 2014, p. 17). In other words, the process and the work system are intertwined and cannot be separated; the process is embedded in the work system.
One example of the application of the SEIPS model to describe a process is a case study of a wrong site surgery in an ambulatory surgery center (Carayon et al., 2004). The work system model was applied to describe the care process for a surgery patient and identify work system elements that contributed to wrong site surgeries. Each step in the process is a task involving various people using various tools and technologies, occurring in a specific environment within an organization. A process map representing the work system elements identifies care transitions and other elements that could contribute to a wrong site surgery (Carayon et al., 2004). This example demonstrates that a process is embedded in a work system; the work system provides the context in which the care process occurs (Rivera-Rodriguez et al., 2013), and the process mediates the impact of the work system on outcomes (Carayon, Wetterneck, et al., 2014).
4. SEIPS-based Process Modeling
We propose the SEIPS-based process modeling method to assess and improve healthcare processes, with the objective of integrating HFE with quality improvement science as suggested by Hignett et al. (2015). We view the process as a series of tasks and preserve the temporal task sequence in the process map. Our method integrates the work system model by including all work system elements. This ensures that resources needed in the process and mechanisms for coordination, communication and information flow are also depicted (Unertl et al., 2010).
The resulting process map is most similar to the swim-lane diagram and flowchart described by Jun et al. (2009). Major tasks are shown on the process map and identify the person who performs the task and the process chronology. Columns represent the person or team completing the task, the physical environment, the organizational unit, or some combination of those. Rows are generally temporal, and the arrows also depict temporality. The task boxes are numbered and labeled to easily find the corresponding row in the supplementary tables. Each task box contains icons indicating tools and technologies used to perform the task. Arrows show linkages between tasks and represent mechanisms for coordination, communication and information flow (organizational factors). The specific organization, i.e. clinic, is also represented in the process map; in particular we highlight differences in tasks and tools/technologies used in the clinics. An accompanying table provides details about the tasks shown in the map.
The process map and accompanying table are used to evaluate the process; this evaluation is based on identification of barriers and facilitators (Carayon, DuBenske, et al., 2011; Carayon et al., 2005; Carayon, Li, et al., 2014; Gurses & Carayon, 2007). Barriers and facilitators can be found throughout the work system (Carayon, Wetterneck, et al., 2014) and are often related to specific steps in the process. The barriers and facilitators are represented by red and green dots, respectively, and appear on the process map alongside the associated tasks. Further details about the work system barriers and facilitators are also included in the accompanying table.
5. Methods
The example provided, part of a larger project on the use of health information technology (IT) to support care management for chronically ill patients (Carayon, Hundt, et al., 2015), focused on redesigning primary care to increase provider efficiency and quality of care through use of health IT. Primary care is an essential component of health care, functioning as the entry into health care and medical home of patients (Beasley, Escoto & Karsh, 2007; Sepulveda, Bodenheimer & Grundy, 2008). Increased primary care access has been associated with improved health, improved quality in outcomes and reduced costs (Beasley et al., 2007; Engström, Foldevi & Borgquist, 2001). However, these benefits have not been fully realized as primary care faces numerous challenges, such as a shrinking workforce, capital shortage and inadequate health IT (Pentecost, 2006).
5.1 Primary Care Processes
The primary care redesign portion of the larger project evaluated three processes in two clinics: (1) previsit planning, (2) patient outreach for panel management and (3) checkout. These processes are local to the participating healthcare system, although previsit planning has been described elsewhere (Sinsky et al., 2013). In previsit planning, a nurse calls patients with scheduled appointments to advise them of tests and procedures to be done prior to the appointment (Sinsky et al., 2013). The nurse then arranges for the patient to complete the necessary tests. The second process, patient outreach for panel management, ensures that patients have regular contact with their primary care provider (PCP) to maintain their health and address any health issues in a timely manner. In this process, a patient access representative (PAR) contacts patients who have not had a recent primary care appointment and helps schedule a visit. The third process is the checkout process after a primary care visit, when a PAR schedules follow-up appointments and tests for the patients. This typically happens before the patient leaves the clinic. If the patient leaves without completing the checkout process, the patient access representative calls the patient and completes it over the phone.
5.2 Setting and Sample
We used purposeful sampling to select staff members from the two clinics for observation and interview. Participation was voluntary. One clinic is a family medicine clinic with six providers (i.e. physicians and advanced practice providers); the second clinic has twelve internal medicine and family medicine providers in primary care, and also offers other specialty care. We observed and interviewed three clinic-based care managers, two providers, four nurses, three administrators and two PARs. The Institutional Review Board of the participating healthcare system approved the research.
5.3 Data Collection Methods
We collected data during three visits to each primary care clinic between February and June 2013. The first visit included a clinic tour, an introductory meeting with clinic leadership and combined observation and interview data collection. During these combined observation and interview data collections, participants completed each process as usual, with researchers asking clarifying questions whenever possible without interrupting patient interactions and care, noting various system elements required for each step or activity. The second visit continued the combined observation and interview data collection as described and included a “mock patient experience” at each clinic, in which one researcher acted as a patient while another observed the processes being performed from arrival to the clinic, through patient rooming and finally to check out. During the third visit, we completed data collection with more combined observation and interviews; during this visit, we also reviewed draft process maps with clinic staff. We completed nineteen combined observation/interviews for a total of 15.5 hours of data collection.
The combined observations and semi-structured interviews were based on the SEIPS model (Carayon et al., 2006; Carayon, Wetterneck, et al., 2014) and centered on the work system elements (Carayon, 2009; Smith & Carayon-Sainfort, 1989). During each observation, we sat or stood behind the nurse or PAR, noting when each task was done, what tools and technologies were used, and any environment or organization factors influencing the tasks. The participants described their cognitive activities while completing these processes. The interviews, conducted immediately following the observation, first focused on clarifying questions about the process, then probes around the work system elements, and finally barriers and facilitators in the process. Observation notes were typed and interviews were audio-recorded and transcribed by a professional transcription service.
5.4 Data Analysis and Process Map Development
We conducted a qualitative analysis of the observation notes and interview transcripts to identify the tasks of each staff member, task sequence, use of technology and tools and work system barriers and facilitators. Through this qualitative data analysis, we developed process maps in Microsoft® Visio (Microsoft Office, 2013) and Adobe Illustrator CC© (Adobe Systems Incorporated, 2014). We also created supplementary tables to provide further details and describe variation of tasks, barriers and facilitators. Each process map was reviewed by all researchers and iteratively refined until all researchers agreed each map was complete. Study participants validated the process maps during the final site visit; we made slight modifications based on staff feedback.
The four researchers independently coded each barrier and facilitator according to the work system elements, writing an explanation for how the work system elements interacted when the barrier or facilitator was coded to multiple elements. The independent coding of all researchers was combined and distributed for review. We then discussed and agreed upon each coding through a consensus process that determined the most immediate, proximal work system element(s) that corresponded with the barrier or facilitator. For example, in step 1 (access IT applications and reports) of previsit planning in clinic 1, the second barrier was coded as tools and technologies by all four researchers and task by one researcher. Following a discussion, the final coding agreed upon was tools and technologies; although the barrier was related to task performance, the most proximal work system element was tools and technologies due to the slow health IT application.
6. Results
6.1 Process Maps
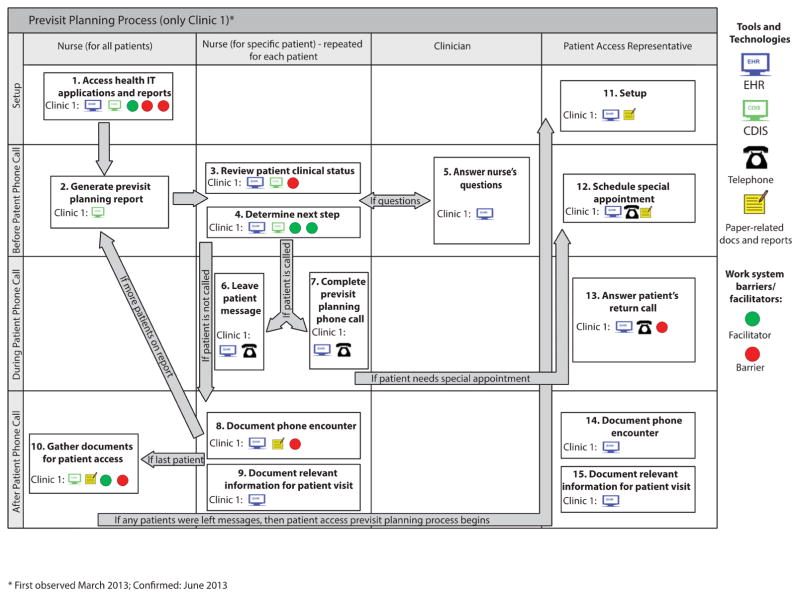
A map was developed for each of the 3 processes. Figure 2 shows the previsit planning process map for clinic 1; additional information can be found in Table 1. In this process, the nurse accesses two health IT applications and generates the previsit planning report that identifies the patients she should call (tasks 1 and 2). For each patient on the report, she reviews their clinical status and determines what should be done before their visit (tasks 3 and 4). She may need to ask a clinician what they would like to have done in preparation for the visit (transition between tasks 4 and 5), and then she calls the patient. If the patient does not answer, the nurse leaves a voicemail and prints documents to share with the PAR (tasks 6 and 9); otherwise, she completes the call (task 7). Each call is documented, as the nurse makes notes for the patient visit (task 8). After all patients are called, she gathers the documents she printed when patients did not answer (task 10), and delivers them to the PAR. The PAR answers the return calls and schedules the appropriate tests, documenting the phone contact and relevant information for each visit (tasks 11 through 15). The previsit planning process consists of 15 tasks spread across 3 roles: nurse, clinician and PAR (9, 1 and 5 tasks, respectively).
Figure 2.
Previsit planning process map (only clinic 1).
Table 1.
Additional description and evaluation of the previsit planning process (only clinic 1).
| Box # | Activity | Activity Description | Barriers | Facilitators |
|---|---|---|---|---|
| 1 | Access IT Applications and Reports | Clinic 1
|
Clinic 1
|
Clinic 1
|
| 2 | Generate Previsit Planning Report | Clinic 1
|
||
| 3 | Review Patient Clinical Status | Clinic 1
|
Clinic 1
|
|
| 4 | Determine Next Step | Clinic 1
|
Clinic 1
|
|
| 5 | Answer Nurse’s Questions | Clinic 1
|
||
| 6 | Patient Does Not Answer | Clinic 1
|
||
| 7 | Patient Answers | Clinic 1
|
||
| 8 | Document Phone Encounter | Clinic 1
|
Clinic 1
|
|
| 9 | Document Relevant Information for Patient Visit | Clinic 1
|
||
| 10 | Gather Documents for Senior PAR | Clinic 1
|
Clinic 1
|
Clinic 1
|
| 11 | Setup | Clinic 1
|
||
| 12 | Schedule Specialty Appointment | Clinic 1
|
||
| 13 | Patient Calls Back | Clinic 1
|
Clinic 1
|
|
| 14 | Document Phone Encounter | Clinic 1
|
||
| 15 | Document Relevant Information for Patient Visit | Clinic 1
|
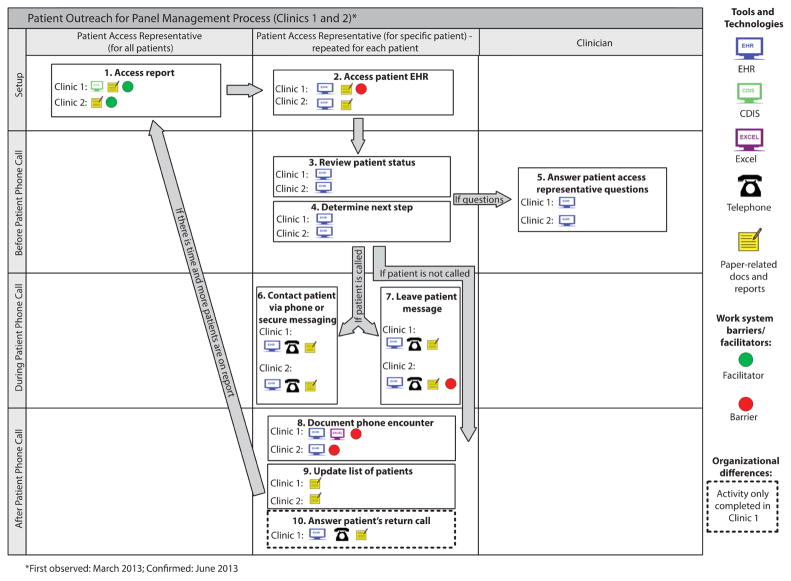
Figure 3 shows the patient outreach for panel management process map; the associated supplementary information is in Table 2. The PAR accesses the report, either paper or electronic (task 1). For each patient on the report, she reviews their EHR, noting their clinical status to determine what to do for each patient (tasks 2, 3 and 4). If the PAR has questions, she follows up with the clinician (task 5). She may contact the patient via secure messaging, phone (leaving a message if they do not answer), or choose not to contact the patient if s/he has already been contacted, or is no longer a patient at the clinic (tasks 6 and 7). Once speaking with the patient, the PAR attempts to schedule a visit to re-engage the patient with their PCP. Each communication is documented, and the list of patients is updated (tasks 8 and 9). If the PAR has more time available, she continues to the next patient. Otherwise, she simply answers return calls as they arrive (task 10). The patient outreach for panel management process consists of 10 tasks spread across 2 roles: a PAR and clinician (9 and 1 tasks, respectively).
Figure 3.
Patient outreach for panel management process map (clinics 1 and 2).
Table 2.
Additional description and evaluation of the patient outreach for panel management process (clinics 1 and 2).
| Box # | Activity | Activity Description | Barriers | Facilitators |
|---|---|---|---|---|
| 1 | Access Panel Management Report | Clinic 1
|
Clinic 1
|
|
Clinic 2
|
Clinic 2
|
|||
| 2 | Access Patient EHR | Clinic 1
|
Clinic 1
|
|
Clinic 2
|
||||
| 3 | Review Patient Clinical Status | Clinic 1
|
||
Clinic 2
|
||||
| 4 | Determine Next Step | Clinic 1
|
||
Clinic 2
|
||||
| 5 | Answer Senior PAR’s Questions | Clinic 1
|
||
Clinic 2
|
||||
| 6 | Contact Patient Via Phone or Secure Messaging | Clinic 1
|
||
Clinic 2
|
||||
| 7 | Patient Does Not Answer Phone Call | Clinic 1
|
||
Clinic 2
|
Clinic 2
|
|||
| 8 | Document Phone Encounter | Clinic 1
|
Clinic 1
|
|
Clinic 2
|
Clinic 2
|
|||
| 9 | Update List of Patients | Clinic 1
|
||
Clinic 2
|
||||
| 10 | Patient Returns Call/Message | Clinic 1
|
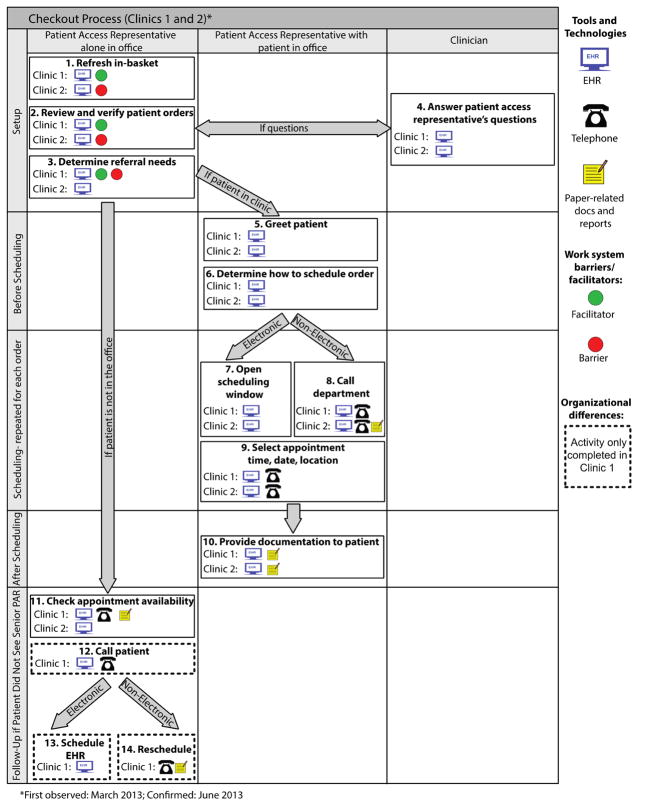
Figure 4 shows the checkout process map; its supplementary information is in Table 3. In this process, the PAR is constantly monitoring her in-basket in the EHR system to view orders associated with patient visits that are concluding (task 1). She reviews and verifies these orders, determining what referrals are needed for the patient (tasks 2 and 3). If she has questions or needs more information, she poses them to the clinician (task 4). When the patient arrives at the PAR’s office, she greets the patient and schedules each order, either electronically or by phone (tasks 5 through 9). The PAR provides documentation, e.g. visit reminders, to the patient after each order has been scheduled, and the patient leaves (task 10). If the patient did not meet with the PAR, for example because she was occupied, the PAR checks appointment availability for each order and contacts the patient (tasks 11 through 14); these vary by clinic. The checkout process consists of 14 tasks spread across 2 roles: a PAR and a provider (13 and 1 tasks, respectively). Six of 13 tasks performed by the PAR were done in collaboration with the patient.
Figure 4.
Checkout process map (clinics 1 and 2).
Table 3.
Additional description and evaluation of the checkout process (clinics 1 and 2).
| Box # | Activity | Activity Description | Barriers | Facilitators |
|---|---|---|---|---|
| 1 | Refresh In-Basket | Clinic 1
|
Clinic 1
|
|
Clinic 2
|
Clinic 2
|
|||
| 2 | Review and Verify Patient Orders | Clinic 1
|
Clinic 1
|
|
Clinic 2
|
Clinic 2
|
|||
| 3 | Determine Referral Needs | Clinic 1
|
Clinic 1
|
Clinic 1
|
Clinic 2
|
||||
| 4 | Answer Senior PAR’s Questions | Clinic 1
|
||
Clinic 2
|
||||
| 5 | Greet Patient | Clinic 1 [Patient already seen at reception desk, received visit summary and directed to senior PAR for scheduling.]
|
||
Clinic 2
|
||||
| 6 | Determine How to Schedule Order | Clinic 1
|
||
Clinic 2
|
||||
| 7 | Open Scheduling Window | Clinic 1
|
||
Clinic 2
|
||||
| 8 | Call Department | Clinic 1 | ||
Clinic 2
|
||||
| 9 | Select Time, Date, Location | Clinic 1
|
||
Clinic 2
|
||||
| 10 | Provide Documentation to Patient | Clinic 1
|
||
Clinic 2
|
||||
| 11 | Check Appointment Availability | Clinic 1
|
||
Clinic 2
|
||||
| 12 | Communicate with Patient | Clinic 1
|
||
| 13 | Schedule in EHR | Clinic 1
|
||
| 14 | Reschedule | Clinic 1
|
6.2 Process Evaluation
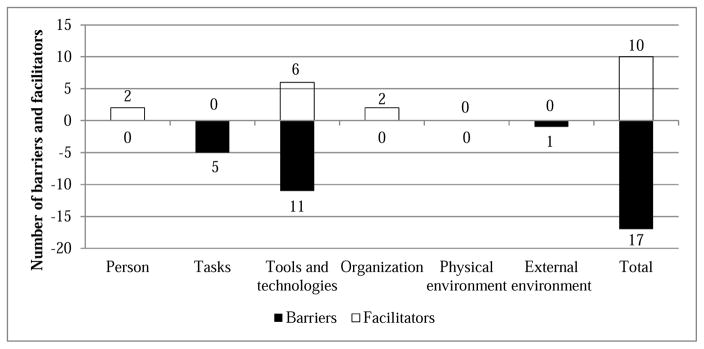
We identified 22 work system barriers and facilitators in the three processes (13 barriers and 9 facilitators); these were coded by work system element (see figure 5). Four barriers and one facilitator were coded to two work system elements.
Figure 5.
Work system barriers and facilitators
Only facilitators are linked to the person element of the work system, and both are due to the familiarity of the nurse and PAR with the clinician’s preferences and habits (clinic 1 previsit planning step 4 and clinic 1 checkout step 3), as the nurse at clinic 1 noted: “The fact that I have worked with the providers for long enough, I know what labs they like ordered.” This allows each of them to interpret and anticipate what the clinician would like the patient to do. The task element is associated with five barriers. One barrier is linked solely to the task element, while the other four are the result of interaction between the task and tools and technologies work system elements. In step 8 of clinic 1’s previsit planning process, the nurse completes the documentation required, including entering “dummy orders” for the provider to “get credit” for any tests that the patient completes outside of the health system. Her task, completing the documentation for providers work to be recognized, necessitates her entering orders that have been completed elsewhere because the technologies are not linked.
Barriers and facilitators were most frequently associated with tools and technologies, showing both challenges and benefits that technology can provide. The tools and technologies barriers were due to lack of fit between the tools and technologies and the task, or the tools and technologies creating additional work. Barriers included issues with speed of computer programs, repeated login requirements (clinic 1 previsit planning step 1) and multiple passwords (clinic 1 checkout step 3). Other barriers included two highly related but unlinked computer systems creating extra work (clinic 1 previsit planning step 3 and panel management step 2), and lack of fit between the technology and task (clinic 1 previsit planning step 10, clinic 2 checkout steps 1 and 2 and both clinics panel management step 8). For example, a nurse noted that one of the computer programs that generated a report did not list everything in the patient record: “… it doesn’t always pick up everything that’s in their health maintenance that’s flagging, so I’m not sure why that happens, sometimes, because I thought that it should pick up everything.” (nurse, clinic 1). The facilitators resulted from matching the tool/technology with the task; for example, using dual computer monitors when two applications must be accessed simultaneously (clinic 1 previsit planning step 1 and clinic 1 checkout step 1), or paper lists that can be updated as needed by the user (both clinics panel management step 1). For example, the patient access representative at clinic 2 mentioned preferring to use a paper list to write her notes: “I like the paper list, because then I can write on it and make little notes to myself and stuff like that.”
The organization element was linked to two facilitators that were related to the communication, cooperation and coordination exhibited between multiple team members in step 4 of clinic 1 previsit planning process. For example, the patient access representative felt comfortable interrupting a physician for clarification: “Now if the patient would check out and say he told me I need to see orthopedics, and there’s not an order in there, I usually go back to the doctor and … just ask them are you going to put one in, so I can kind of get the process started. And then, you know, they get it put in there.” (patient access representative, clinic 1). Interestingly, the physical environment was not associated with any barriers or facilitators. One barrier was attributed to the external environment - HIPAA regulations dictating what sort of information might be left in a voice message for a patient, which an interviewee speculated leads to fewer return calls from patients (step 7 in clinic 2 panel management, Figure 3).
7. Discussion
The SEIPS-based modeling method represents how HFE can advance beyond task analysis to process description and analysis. The maps and accompanying tables describe the process, as do other modeling methods (Jun et al., 2010; 2009). Our maps and accompanying tables systematically consider all work system elements (Carayon, 2009; Smith & Carayon-Sainfort, 1989).
Our method facilitates process analysis of the complex sociotechnical systems characterizing healthcare delivery, including how the system responds to the variation inherent in health care. We present the process at a general level that accommodates variation, such as by patient type. For instance, the variation related to insurance status of patients is embedded in box 3 of table 3. The different ways or variations of this task are not explicitly described: it is possible that patients with different insurance would produce different instantiations of the task in box 3. Our method not only produces descriptive outputs but also supports process evaluation, filling a gap of many currently utilized methods, which focus on describing tasks and processes. For example, the identification of barriers and facilitators within a process is useful to direct improvement efforts. Sometimes, this exposes relatively low-cost process facilitators that could be leveraged more widely. For example, one facilitator in the previsit planning process highlights the usefulness of dual monitors. Therefore, when we presented our analysis and findings to the healthcare system, we recommended adding a second computer monitor for others involved in these processes at other clinics. Improvements identified in process analysis can result in safer, more efficient processes, improve patient safety and care quality care and reduce frustration and improve satisfaction of healthcare workers.
Accurate, complete description of a process is key to building organizational awareness, the state of knowledge individuals and teams have regarding the process (Schultz et al., 2007); this can help to ensure that participants in the process and other stakeholders fully understand the process and develop common ground, especially regarding potential barriers and issues that need to be addressed in a redesign. Our method provides a visual representation of all work system elements in a process and the connections between these elements, providing a tool to facilitate understanding and communication among stakeholders. Because our method maps the entire process, denoting the contributions of all roles, it helps people involved in the process to not only understand or clarify their specific contributions, but also to understand the linkages between their role and the contribution of others to the process.
One important feature of our method is that it supports the identification of all work system elements by visually representing them in a process map. The fit, or lack thereof, between work system elements creates barriers and facilitators in the work system, as described in the supplementary tables. The barriers and facilitators can be proximal and immediate or more distant and further up the causal chain (Holden et al., 2013). For example, the external environment may create the need for a task, such as reporting health maintenance activity completion, and the tools and technologies might not support this task, resulting in a work system barrier. In this case, the misfit of the tools and technology with the task is the proximal interaction leading to the barrier. While the external environment does not immediately impact this tool and technology misfit, it is involved in the interaction distally. Another example of this may be required use of technology that does not support the process of providing safe, high-quality health care creating a barrier and resulting in a work around, for example to meet reporting requirements or to receive national funding (Eason et al., 2012). While this barrier is immediately caused by the technology, the external environment requiring the use of that technology is involved distally. The analysis reported in this paper focuses on immediate or proximal barriers and facilitators; however, it is important to understand that this local context is embedded in a larger organization that interacts with the external environment (Carayon et al., 2013). In fact, two of the processes we analyzed are direct consequences of the external environment – the emphasis on population health management in the US Affordable Care Act, which makes it increasingly important for health systems to encourage patients to see their primary care physician regularly. Contacting patients who have not been seen in a year is one way to reconnect patients with their primary care physician; pre-visit planning makes the time spent in physician-patient encounters as efficient as possible. Ultimately, when examining the web of factors leading to a barrier or facilitator, most work system elements will be involved. Therefore, moving forward, we must examine these multi-level system interactions between distal and proximal factors (Carayon et al., 2013; Holden et al., 2013). We must develop methods for conceptualizing, describing and measuring these interactions, or the “system-ness” of the system (Carayon et al., 2013; Hettinger et al., 2015; Robertson et al., 2015).
Another area of future work is clearly showing how SEIPS can be used to describe the work of clinicians and patients, as well as the collaborative work between them. SEIPS 2.0 represents a first step in this direction, by explicitly considering the simultaneous interaction of multiple work system components and offering suggestions for diagramming active and interacting components (Holden et al., 2013). The intentional inclusion of the patient within the SEIPS 2.0 framework indicates that process mapping based on SEIPS 2.0 would include modeling the patient’s work and the collaborative work between the patient and clinician(s). This requires the development of a new method to represent these two dimensions; this new method could be based on the method we present here.
Limitations of this study include data collection in a single healthcare organization, necessarily limiting generalization beyond the two clinics studied. However, insights about the proposed SEIPS-based process modeling method can still be gleaned. The involvement of multiple researchers and use of multiple methods were helpful to minimize bias and to triangulate data. The proposed method needs further refinement and testing. Future research could formally collect feedback from potential end users of the method and its output to assess usability and usefulness of this method, similar to research conducted by Jun et al. (2009). Based on this feedback, we can continue to refine the process analysis method and further integrate HFE and quality improvement science for the benefits of patient safety and healthcare quality (Hignett et al., 2015).
8. Conclusion
The need to shift to process analysis in order to address major patient safety and healthcare quality problems has been established (Walker & Carayon, 2009), but health care continues to grapple with how it can be accomplished. The SEIPS-based process modeling method represents a significant step in addressing the question of how to accomplish greater focus on processes. We integrate the SEIPS model, already understood and used in health care, with process modeling methods to ensure that all work system elements are considered (Carayon, Wetterneck, et al., 2014). The method can be used to analyze processes and evaluate specific areas of interest, i.e. barriers and facilitators, workload, patient safety, health IT, etc. As Waterson et al. (2015) indicate, we, the HFE community, already perform task analyses. Walker and Carayon (2009) issued the call to shift to process analysis. Now we as the HFE community must develop and disseminate innovative methods to accomplish this in order to continue our positive impact on health care.
Highlights.
The proposed SEIPS-based process modeling method identifies all work system elements involved in care processes.
The SEIPS-based process maps provide a visual representation useful to build organizational awareness.
Describing all work system elements and barriers and facilitators in a care process map can help to identify opportunities for redesign and improvement.
Acknowledgments
Funding for this research was provided by the US Office of the National Coordinator through the Beacon award program [award No. 90BC001301]. This research was also supported by the National Center for Advancing Translational Sciences (NCATS) [grant UL1TR000427]. We would like to thank Sarah Kianfar, Randi Cartmill and the study participants.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adobe Systems Incorporated. Illustrator CC. 2014. [Google Scholar]
- Agency for Healthcare Research and Quality. 2014 National Healthcare Quality & Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; 2015. [Google Scholar]
- Asan O, Chiou E, Montague E. Quantitative ethnographic study of physician workflow and interactions with electronic health record systems. International Journal of Industrial Ergonomics. 2014 doi: 10.1016/j.ergon.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beasley John, Escoto Kamisha, Karsh Ben-Tzion. Human Factors and Ergonomics in Primary Care. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 1. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2007. [Google Scholar]
- Benyoucef M, Kuziemsky C, Rad A Afrasiabi, Elsabbahi A. Modeling healthcare processes as service orchestrations and choreographies. Business Process Management Journal. 2011;17(4):568–597. doi: 10.1108/14637151111149438. [DOI] [Google Scholar]
- Beuscart-Zéphir Marie-Catherine, Pelayo Sylvia, Anceaux Françoise, Maxwell David, Guerlinger Sandra. Cognitive analysis of physicians and nurses cooperation in the medication ordering and administration process. Int J Med Inform. 2007;76:S65–S77. doi: 10.1016/j.ijmedinf.2006.05.022. [DOI] [PubMed] [Google Scholar]
- Brixey JJ, Tang Z, Robinson DJ, Johnson CW, Johnson TR, Turley JP, … Zhang J. Interruptions in a level one trauma center: a case study. Int J Med Inform. 2008;77(4):235–241. doi: 10.1016/j.ijmedinf.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P. The Balance Theory and the work system model... Twenty years later. International Journal of Human-Computer Interaction. 2009;25(5):313–327. [Google Scholar]
- Carayon P, DuBenske LL, McCabe BC, Shaw B, Gaines ME, Kelly MM, … Cox ED. Work system barriers and facilitators to family engagement in rounds in a pediatric hospital. In: Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal G, Tartaglia R, editors. Healthcare Systems Ergonomics and Patient Safety 2011. Boca Raton, FL: CRC Press; 2011. pp. 81–85. [Google Scholar]
- Carayon P, Faye H, Hundt AS, Karsh B-T, Wetterneck T. Patient safety and proactive risk assessment. In: Yuehwern Y, editor. Handbook of Healthcare Delivery Systems. Boca Raton, FL: Taylor & Francis; 2011. p. 12-11.p. 12-15. [Google Scholar]
- Carayon P, Gurses AP, Hundt AS, Ayoub P, Alvarado CJ. Performance obstacles and facilitators of healthcare providers. In: Korunka C, Hoffmann P, editors. Change and Quality in Human Service Work. Vol. 4. Munchen, Germany: Hampp Publishers; 2005. pp. 257–276. [Google Scholar]
- Carayon P, Hancock P, Leveson N, Noy I, Sznelwar L, van Hootegem G. Advancing a sociotechnical systems approach to workplace safety - developing the conceptual framework. Ergonomics. 2015;58(4):548–564. doi: 10.1080/00140139.2015.1015623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Hancock P, Leveson N, Noy I, Sznelwar L, Van Hootegem G, Hettinger L. Sociotechnical systems for occupational safety – New research directions. 2013 doi: 10.1080/00140139.2015.1015623. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Hundt A, Hoonakker P, Kianfar S, Alyousef B, Salek D, … Tomcavage J. Perceived impact of care managers’ work on patient and clinician outcomes. European Journal for Person Centered Healthcare. 2015;3(2):158–167. doi: 10.5750/ejpch.v3i2.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Hundt AH, Karsh BT, Gurses AP, Alvarado CJ, Smith M, Brennan PF. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(Suppl 1):i50–58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Li Y, Kelly MM, DuBenske LL, Xie A, McCabe B, … Cox ED. Stimulated recall methodology for assessing work system barriers and facilitators in family-centered rounds in a pediatric hospital. Appl Ergon. 2014;45(6):1540–1546. doi: 10.1016/j.apergo.2014.05.001. doi: http://dx.doi.org/10.1016/j.apergo.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Schultz K, Hundt AS. Righting wrong site surgery. Jt Comm J Qual Saf. 2004;30(7):405–410. doi: 10.1016/s1549-3741(04)30046-8. [DOI] [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, Gurses AP. Human factors systems approach to healthcare quality and patient safety. Appl Ergon. 2014;45(1):14–25. doi: 10.1016/j.apergo.2013.04.023. S0003-6870(13)00096-3 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eason K, Dent M, Waterson P, Tutt D, Hurd P, Thornett A. Final report. NIHR Service Delivery and Organisation Programme, Department of Health; London: 2012. Getting the benefit from electronic patient information that crosses organisational boundaries. [Google Scholar]
- Engström S, Foldevi S, Borgquist L. Is general practice effective? A systematic literature review. Scandinavian Journal of Primary Health Care. 2001;19(2):131–144. doi: 10.1080/028134301750235394. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Carayon P. Performance obstacles of intensive care nurses. Nursing Research. 2007;56(3):185–194. doi: 10.1097/01.NNR.0000270028.75112.00. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Ozok AA, Pronovost PJ. Time to accelerate integration of human factors and ergonomics in patient safety. BMJ quality & safety. 2011 doi: 10.1136/bmjqs-2011-000421. [DOI] [PubMed] [Google Scholar]
- Hallock ML, Alper SJ, Karsh B. A macroergonomic work system analysis of the diagnostic testing process in an outpatient health care facility for process improvement and patient safety. Ergonomics. 2006;49(5–6):544–566. doi: 10.1080/00140130600568832. [DOI] [PubMed] [Google Scholar]
- Hettinger LJ, Kirlik A, Goh YM, Buckle P. Modelling and simulation of complex sociotechnical systems: Envisioning and analysing work environments. Ergonomics. 2015;58(4):600–614. doi: 10.1080/00140139.2015.1008586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hignett S, Jones EL, Miller D, Wolf L, Modi C, Shahzad MW, … Catchpole K. Human factors and ergonomics and quality improvement science: Integrating approaches for safety in healthcare. BMJ Qual Saf. 2015;24(4):1–5. doi: 10.1136/bmjqs-2014-003623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Carayon Pascale, Gurses Ayse P, Hoonakker Peter, Hundt Ann Schoofs, Ozok A Ant, Rivera-Rodriguez A Joy. SEIPS 2.0: A human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–1686. doi: 10.1080/00140139.2013.838643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- ISO. ISO 9000: Quality Management Systems. Genève, Switzerland: International Organization for Standardization; 2015. [Google Scholar]
- Johnson KB, Fitzhenry F. Case report: activity diagrams for integrating electronic prescribing tools into clinical workflow. J Am Med Inform Assoc. 2006;13(4):391–395. doi: 10.1197/jamia.M2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jun GT, Ward J, Clarkson P. Systems modelling approaches to the design of safe healthcare delivery: ease of use and usefulness perceived by healthcare workers. Ergonomics. 2010;53(7):829–847. doi: 10.1080/00140139.2010.489653. [DOI] [PubMed] [Google Scholar]
- Jun GT, Ward J, Morris Z, Clarkson J. Health care process modelling: which method when? International Journal for Quality in Health Care. 2009;21(3):214–224. doi: 10.1093/intqhc/mzp016. [DOI] [PubMed] [Google Scholar]
- Kaplan G, Bo-Linn G, Carayon P, Pronovost P, Rouse W, Reid P, Saunders R. Bringing a systems approach to health. Institute of Medicine; 2013. [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington, D.C: National Academy Press; 1999. [PubMed] [Google Scholar]
- Kummerow Broman K, Kensinger C, Hart H, Mathisen J, Kripalani S. Closing the loop: a process evaluation of inpatient care team communication. BMJ Qual Saf. 2015 doi: 10.1136/bmjqs-2015-004580. [DOI] [PubMed] [Google Scholar]
- Laxmisan Archana, Hakimzada Forogh, Sayan Osman R, Green Robert A, Zhang Jiajie, Patel Vimla L. The multitasking clinician: Decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2007;76(11–12):801–811. doi: 10.1016/j.ijmedinf.2006.09.019. doi: http://dx.doi.org/10.1016/j.ijmedinf.2006.09.019. [DOI] [PubMed] [Google Scholar]
- Microsoft Office. Microsoft Visio. 2013. [Google Scholar]
- Ozkaynak M, Brennan P. An Observation Tool for Studying Patient-oriented Workflow in Hospital Emergency Departments. Methods Inf Med. 2013;52(6):503–513. doi: 10.3414/ME12-01-0079. [DOI] [PubMed] [Google Scholar]
- Pentecost MJ. Wither primary care? Journal of the American College of Radiology. 2006;3(6):394–397. doi: 10.1016/j.jacr.2006.03.002. [DOI] [PubMed] [Google Scholar]
- President’s Council of Advisors on Science and Technology. Report to the President, better health care and lower costs: accelerating improvement through systems engineering. Vol. 2014 Washington, District of Columbia: Executive Office of the President, President's Council of Advisors on Science and Technology; 2014. [Google Scholar]
- Puentes John, Roux Michèle, Montagner Julien, Lecornu Laurent. Development framework for a patient-centered record. Comput Methods Programs Biomed. 2012;108(3):1036–1051. doi: 10.1016/j.cmpb.2012.06.007. doi: http://dx.doi.org/10.1016/j.cmpb.2012.06.007. [DOI] [PubMed] [Google Scholar]
- Reid PR, Compton WD, Grossman JH, Fanjiang G. Building a Better Delivery System. A New Engineering/Health Care Partnership. Washington, D.C: The National Academies Press; 2005. [PubMed] [Google Scholar]
- Rivera-Rodriguez AJ, McGuire K, Carayon P, Kleiner B, Wears R, Robertson M, … Waterson P. Multi-Level Ergonomics Determining How To Bound Your System. Paper presented at the Proceedings of the Human Factors and Ergonomics Society Annual Meeting.2013. [Google Scholar]
- Robertson MM, Hettinger LJ, Waterson PE, Noy YI, Dainoff MJ, Leveson NG, … Courtney TK. Sociotechnical approaches to workplace safety: Research needs and opportunities. Ergonomics. 2015;58(4):650–658. doi: 10.1080/00140139.2015.1011241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz K, Carayon P, Hundt AS, Springman SR. Care transitions in the outpatient surgery preoperative process: facilitators and obstacles to information flow and their consequences. Cognition, Technology & Work. 2007;9(4):219–231. [Google Scholar]
- Schultz K, Carayon P, Hundt AS, Springman SR. The Human Factors and Ergonomics Society, editor. Proceedings of the Human Factors and Ergonomics Society 49th Annual Meeting. Santa Monica, CA: The Human Factors and Ergonomics Society; 2005. Patient care process and information flow in outpatient surgery; pp. 1469–1473. [Google Scholar]
- Sepulveda MJ, Bodenheimer T, Grundy P. Primary care: can it solve employers’ health care dilemma? Health Aff (Millwood) 2008;27(1):151–158. doi: 10.1377/hlthaff.27.1.151. [DOI] [PubMed] [Google Scholar]
- Siemieniuch CE, Sinclair MA. Evaluation of Human Work. 3. CRC Press; 2005. The analysis of organisational processes; pp. 977–1008. [Google Scholar]
- Sinsky CA, Willard-Grace R, Schutzbank AM, Sinsky TA, Margolius D, Bodenheimer T. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;11(3):272–278. doi: 10.1370/afm.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MJ, Carayon-Sainfort P. A balance theory of job design for stress reduction. International Journal of Industrial Ergonomics. 1989;4(1):67–79. [Google Scholar]
- Unertl KM, Johnson KB, Lorenzi NM. Health information exchange technology on the front lines of healthcare: workflow factors and patterns of use. J Am Med Inform Assoc. 2012;19(3):392–400. doi: 10.1136/amiajnl-2011-000432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unertl KM, Novak LL, Johnson K, Lorenzi N. Traversing the many paths of workflow research: developing a conceptual framework of workflow terminology through a systematic literature review. Journal of the American Medical Informatics Association. 2010;17(3):265–273. doi: 10.1136/jamia.2010.004333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unertl KM, Weinger MB, Johnson KB, Lorenzi NM. Describing and Modeling Workflow and Information Flow in Chronic Disease Care. J Am Med Inform Assoc. 2009;16(6):826–836. doi: 10.1197/jamia.M3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Tilburg CM, Leistikow IP, Rademaker CMA, Bierings MB, van Dijk ATH. Health care failure mode and effect analysis: a useful proactive risk analysis in a pediatric oncology ward. Qual Saf Health Care. 2006;15(1):58–63. doi: 10.1136/qshc.2005.014902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker J, Carayon P. From tasks to processes: The case for changing health information technology to improve health care. Health Affairs. 2009;28(2):467. doi: 10.1377/hlthaff.28.2.467. [DOI] [PubMed] [Google Scholar]
- Waterson P, Robertson MM, Cooke NJ, Militello L, Roth E, Stanton N. Defining the methodological challenges and opportunities for an effective science of sociotechnical systems and safety. Ergonomics. 2015;58(4):565–599. doi: 10.1080/00140139.2015.1015622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie A, Carayon P. A systematic review of human factors and ergonomics (HFE)-based healthcare system redesign for quality of care and patient safety. Ergonomics. 2015;58(1):33–49. doi: 10.1080/00140139.2014.959070. [DOI] [PMC free article] [PubMed] [Google Scholar]