Abstract
Background
Studies demonstrate that women physicians are less likely than men to be full professors. Comprehensive evidence examining whether sex differences in faculty rank exist in academic cardiology, adjusting for experience and research productivity, is lacking. Therefore, we evaluated for sex differences in faculty rank among a comprehensive, contemporary cohort of United States (US) cardiologists after adjustment for several factors that impact academic advancement, including measures of clinical experience and research productivity.
Methods
We identified all US cardiologists with medical school faculty appointments in 2014 using the American Association of Medical Colleges (AAMC) faculty roster, and linked this list to a comprehensive physician database from Doximity, a professional networking website for doctors. Data on physician age, sex, years since residency, cardiology sub-specialty, publications, National Institutes of Health (NIH) grants, and registered clinical trials were available for all academic cardiologists. We estimated sex differences in full professorship, adjusting for these factors and medical school-specific fixed effects in a multivariable regression model.
Results
Among 3810 cardiologists with faculty appointments in 2014 (13.3% of all US cardiologists), 630 (16.5%) were women. Women faculty were younger than men (mean age: 48.3 years vs 53.5 years, p<0.001), had fewer total publications (mean number: 16.5 publications vs. 25.2 publications, p<0.001), were similarly likely to have NIH funding (proportion with at least one NIH award: 10.8% vs. 10.4%, p=0.77), and were less likely to have a registered clinical trial (percentage with at least one clinical trial: 8.9% vs. 11.1%, p=0.10). Among 3180 men, 973 (30.6%) were full professors compared to 100 (15.9%) of 630 women. In adjusted analyses, women were less likely to be full professors than men (adjusted OR: 0.63, 95% CI: 0.43, 0.94, p = 0.02; adjusted proportions 22.7% vs. 26.7%, absolute difference −4.0%; 95% CI: −7.5% to −0.7%).
Conclusions
Among cardiology faculty at US medical schools, women were less likely than men to be full professors after accounting for several factors known to influence faculty rank.
Keywords: women, academic cardiology, professional development, workforce policy
Subject Terms: Health Services, Ethics and Policy
INTRODUCTION
Over the last half century, medicine has made important progress towards mitigating sex disparities in access to medical training, employment, academic advancement, and promotion. Currently, about half of all United States (US) medical school graduates and 38% of all US medical school faculty are women—proportions that have increased dramatically since 1970, when approximately 8% of medical school graduates and faculty were female.1–3 Despite this progress, important sex differences persist in medicine generally, and in academic medicine in particular. For example, previous work has identified sex differences in salary among, and institutional support for, early career physician-investigators.4–6 Moreover, a recently published analysis of sex differences in academic rank in the US—which included more than 90,000 physicians with academic appointments at US medical schools—found significant sex disparities in full and associate professorship even after adjusting for age and several measures of research productivity.1 The proportion of female cardiologists has more than doubled over the last twenty years—from 5% in 1996 to 12.3% in 2013.2,7 Nevertheless, cardiology continues to have the lowest proportion of women of any medical specialty.2 Women are particularly underrepresented in cardiology’s procedural subspecialties, and account for less than 10% of the physician workforce in both interventional cardiology and electrophysiology.8 Female cardiologists also face several professional and personal challenges that do not impact men, including minimizing radiation exposure prior to and during pregnancy, and taking maternity leave to have children.7–11 Moreover, 69% of female cardiologists surveyed by the American College of Cardiology (ACC) in 2006 reported experiencing some form of sex-related discrimination.8 Recent research has also identified sex differences in cardiologists’ salaries which persist after accounting for numerous potential confounders.9 Unconscious sex bias is an important enabler of these persistent sex differences.12,13
These sex disparities in cardiology extend to professional advancement as well. The 2006 ACC survey revealed marked sex differences in the perceived speed of professional advancement vis-à-vis professional contemporaries.8 However, to our knowledge no previous work has specifically examined sex differences in academic rank among US academic cardiologists. Using a unique, comprehensive database of physicians with faculty appointments at US medical schools in 2014, we evaluated sex differences in academic rank among academic cardiologists. Our database included detailed information on several factors known to influence academic rank in medicine, including age, years of experience, sub-specialty, research funding, publications, participation in clinical trials, and clinical volume.4,6,14
METHODS
Data Sources
We obtained and analyzed data from a comprehensive cross-sectional database of US physicians developed by Doximity, a company which provides an online networking service for US physicians. The database contains information about 1,029,088 US physicians as of July 7, 2015.
Doximity uses several mechanisms to identify physicians for inclusion in the database. First, it automatically creates accounts for all physicians included in the National Plan and Provider and Numeration System (NPPES) National Provider Identifier (NPI) registry. These physicians may then register as users. Second, physicians without active NPIs may self-register with Doximity and use its services for free. As of July 7, 2015, 24.0% of all US doctors were registered members (246,786 of 1,029,088).
The company obtains several types of information about each physician, independent of member status, including: age; sex; allopathic (MD) versus osteopathic (DO) training; year of graduation from medical school and residency; medical school name; location of residency training; American Board of Internal Medicine (ABIM) certification, including in internal medicine (IM), IM specialties (e.g., cardiology, gastroenterology, etc.), and sub-specialties (interventional cardiology and electrophysiology, for example); number of publications (including first, last, and total), number of National Institute of Health (NIH) grants for which the physician was a principle investigator (PI); and number of clinical trials for which the physician was a PI or sub-investigator. These data are obtained from several sources, including: The American Board of Medical Specialties, state licensing boards, PubMed, the NIH RePORT database, ClinicalTrials.gov, and through partnerships with collaborating hospitals and medical schools. A detailed explanation of the database and validation of its accuracy has been published previously.1 We augmented this database by adding each physician’s Medicare revenue in 2013 (which is publicly available from the Centers for Medicare and Medicaid Services (CMS)) and by identifying physicians with academic appointments at medical schools ranked in the top 20 for research by US News & World Report in 2013.15
Study Population
Our study population included all cardiologists who were on the list of physician faculty (e.g. assistant, associate, and full professors) in the 2014 Association of American Medical Colleges (AAMC) faculty roster. The AAMC faculty roster is a comprehensive database of US physician faculty, and contains more than 160,000 active faculty. All accredited US medical schools participate voluntarily in the database, and regularly update the faculty roster.16 Thus, the study population represented a comprehensive sample of US cardiologists who were assistant, associate, or full professors at accredited US medical schools in 2014. Each of these cardiologists was matched with their information in the Doximity database. The human subjects review committee at Harvard Medical School approved these data for study and waived participant consent.
Data Validity
The accuracy of the data set was assessed in two ways. First, we evaluated the subgroup of cardiologists who were registered members of Doximity (e.g had logged in to activate their accounts). We presumed that the profiles of these registered users might be more complete then those of non-registered users, and sought to assess whether any differences in profile completeness resulted in differences in outcomes. Second, in a previous analysis, we performed manual audits of the profiles of a random sample of 200 physicians with faculty appointments at US medical schools. We manually confirmed faculty rank (through review of institutional websites); publications in PubMed; clinical trial participation through manual review of ClinicalTrials.gov; and NIH funding through manual review of NIH RePORT database. This validation analysis has been described previously.1
Statistical Analysis
We began by performing unadjusted comparisons of the characteristics of men and women in our cohort using 2-sided t tests and chi-square tests. Next, we constructed a multivariable logistic regression model to predict the probability of full professorship as a function of physician sex. This multivariable regression analysis adjusted for several other variables which could affect academic advancement among cardiologists and confound sex differences in faculty rank, including: age, years since residency completion, sub-specialty within cardiology (binary variables for each of the following: interventional cardiology, electrophysiology, non-invasive cardiology), number of publications (first author plus last author, and total), NIH grants (binary variable indicating whether a cardiologist had ever been a principal investigator on an NIH grant), clinical trial participation (binary variable), employment at US medical school ranked in the top 20 US medical schools for research by US News & World Report,15 and Medicare reimbursements in 2013. This model also included medical school-level fixed effects to assist with identifying sex differences in faculty rank among cardiologists within the same school. We used robust standard errors to account for correlations due to physician clustering by medical school.
The primary outcome of this analysis was the adjusted odds of full professorship (versus associate and assistant professorship) among women relative to men. We calculated adjusted odds ratios to determine associations between each model variable and full professorship. In addition, we calculated the adjusted proportions of full professorship for men and women, as well as the absolute adjusted difference in proportions, assuming population mean values for all other model variables. We used analogous methods to characterize associations between each model variable and the probability of being a full professor. We considered a two tailed p-value </= 0.05 to be statistically significant.
In secondary analyses, and using the same variables included in the primary analysis, we estimated new multivariable logistic regression models to evaluate the odds of associate or full professorship (a combined outcome) versus assistant professorship among faculty of all ranks, and full professorship versus associate professorship among faculty with the titles of associate or full professor (e.g. excluding assistant professors). We then used these models to calculate adjusted odds ratios of men and women who achieve these outcomes, and to assess odds ratios for secondary outcomes as a function of the other model variables. We also used the models to calculate adjusted differences in proportions for each of these outcomes.
We compared sex differences in full professorship among cardiologists and cohorts of U.S. academic physicians practicing in seven other internal medicine (IM) sub-specialties: gastroenterology, infectious diseases, pulmonology, rheumatology, oncology, nephrology, and endocrinology. To do so, we identified all physicians in the Doximity database from each of these specialties who were assistant, associate, or full professors at a U.S. medical school and used our multivariable logistic regression model from the primary analysis to estimate adjusted odds ratios of full professorship between men and women for each IM subspecialty.
We assessed for variation in sex differences in academic rank between medical schools in two ways: First, we stratified our cohorts of cardiologists and other IM sub-specialists into: those affiliated with medical schools ranked in the top 20 for research by U.S. News & World Report in 2013,15 and those affiliated with all other medical schools. We then compared adjusted sex differences in full professorship across IM sub-specialties within each stratified level.
Second, we evaluated adjusted sex differences in full professorship for each individual US medical school in the following way: Using the multivariable regression model from our primary analysis, we predicted for each medical school the difference in adjusted proportions of full professorship between men and women if all cardiologists in our cohort were affiliated with that medical school. For each school, we calculated the difference between the observed and predicted sex differences in full professorship (with more negative differences representing greater sex disparities in full professorship).
Our dataset was missing information on the year of residency completion for a small number of physicians (287; 6.5% of total), but was otherwise complete. To address this issue, we compared characteristics of physicians with and without missing data and confirmed that non-missing characteristics were similar between the two groups (eTable 1). We then excluded all physicians with missing data from our analyses.
Sensitivity Analyses
We performed sensitivity analyses to better understand how NIH funding status, and different definitions of cardiology sub-specialties influenced our outcomes of interest. First, while we hypothesized that physicians with NIH funding were likely to be on full time research tracks, it is possible that sex differences in full professorship may differ among those on research vs. clinical tracks. To investigate our hypothesis, we added an interaction term between sex and NIH funding status to our model to understand whether sex differences in academic rank were different for research vs. non-research tracks. Sex was not interacted with any other variables in the model. The outcomes of this analysis were the regression coefficient of the new interaction term and predicted sex differences in full professorship according to NIH funding status using this newly estimated regression model. In addition, repeat research funding may predict academic advancement and previous work suggests that women are less likely than men to obtain repeat NIH funding.17,18 We therefore evaluated the adjusted odds of having at least two NIH awards (among cardiologists with at least one award) as a function of physician sex and the above covariates and also evaluated whether repeat research funding (defined as two or more NIH grants among cardiologists with at least one grant) was associated increased adjusted odds of full professorship.
Second, because some practicing interventional cardiologists and electrophysiologists are not ABIM-board certified in these specialties, we assessed whether identifying subspecialists through billing for sub-specialty procedures in Medicare claims data affected our results.19,20 To do so, we estimated our multivariable regression analysis three times, using three different methods for identifying interventional cardiologists and electrophysiologists (See Appendices A–B for description of these methods and list of CPT Codes used for definitions, respectively). All analyses were performed in STATA, version 14.0 (College Station, TX).
RESULTS
Characteristics of Study Population
Our study included 3,810 cardiologists with faculty appointments at US Medical Schools in 2014 (13.3% of 28,650 cardiologists in the overall database), of whom 16.5% (630/3810) were women (descriptive characteristics for 287 cardiologists excluded from analyses due to missing data are available in eTable 1). Overall, 28.2% (1074/3810) of all cardiologists were full professors. Female cardiologists were less likely than male cardiologists to be full professors (15.9% [100/630] vs. 30.6% [973/3180]; absolute difference 14.7%, p<0.001; Table 1). Women were more likely than men to be assistant professors (60.2% vs. 46.8%; absolute difference, 13.4%, p<0.001) and similarly likely to be associate professors (24.0% vs. 22.6%; absolute difference, 1.4%, p=0.47). On the whole, women were younger, less likely to practice an invasive specialty, and had completed residency more recently than their male colleagues. Women were also more likely than men to be faculty at a school ranked highly in research (37.0% vs. 31.9%; absolute difference 5.1%, p=0.02). Female cardiologists had fewer total and first- or last-author publications (mean total, 16.5 vs. 25.2; difference −8.7, p<0.001; mean first- or last-author; 9.5 vs. 16.4; difference −6.9, p<0.001), and fewer NIH grants (median number of grants among those with at least one NIH award; 3 vs. 4, p=0.08). Similar proportions of female and male cardiologists had at least one NIH grant (10.8% vs. 10.4%; difference 0.4%, p=0.77), or helped conduct at least one clinical trial (8.9% vs. 11.1%, difference −2.2%, p=0.10). On average, women received lower total Medicare payments than men in 2013 ($70,258 vs. $95,902; difference −$25,644, p <0.001).
TABLE 1.
Characteristics of the Study Population
| Faculty
|
P-value for Comparison by Sex* | ||||||
|---|---|---|---|---|---|---|---|
| All (n = 3810) | Male (n = 3180) | Female (n = 630) | |||||
| Count | % | Count | % | Count | % | ||
| Faculty Rank | |||||||
|
| |||||||
| Assistant | 1866 | 49.0 | 1487 | 46.8 | 379 | 60.2 | <0.001 |
|
| |||||||
| Associate | 871 | 22.9 | 720 | 22.6 | 151 | 24 | 0.47 |
|
| |||||||
| Full | 1073 | 28.2 | 973 | 30.6 | 100 | 15.9 | <0.001 |
|
| |||||||
| Sub-Specialty† | |||||||
|
| |||||||
| Non-Invasive‡ | 2598 | 68.2 | 2057 | 64.7 | 541 | 85.9 | <0.001 |
|
| |||||||
| Electrophysiology | 497 | 13.0 | 443 | 13.9 | 54 | 8.6 | <0.001 |
|
| |||||||
| Interventional Cardiology | 715 | 18.8 | 680 | 21.4 | 35 | 5.6 | <0.001 |
|
| |||||||
| Faculty at Top 20 Med School§ | 1248 | 32.8 | 1015 | 31.9 | 233 | 37.0 | 0.02 |
|
| |||||||
| Age (SD) | 52.7 | 11.6 | 53.5 | 11.8 | 48.3 | 9.4 | <0.001 |
|
| |||||||
| Age Groups | |||||||
|
| |||||||
| Age <40 | 526 | 14.2 | 404 | 13.4 | 122 | 20.4 | <0.001 |
|
| |||||||
| Age 40–44 | 582 | 15.8 | 463 | 14.9 | 119 | 19.9 | |
|
| |||||||
| Age 45–49 | 497 | 13.5 | 395 | 12.8 | 102 | 17.1 | |
|
| |||||||
| Age 50–54 | 537 | 14.5 | 439 | 14.2 | 98 | 16.4 | |
|
| |||||||
| Age 55–59 | 483 | 13.1 | 404 | 13.0 | 79 | 13.2 | |
|
| |||||||
| Age 60–64 | 464 | 12.6 | 411 | 13.3 | 53 | 8.9 | |
|
| |||||||
| Age 65+ | 607 | 16.4 | 583 | 18.8 | 24 | 4.0 | |
|
| |||||||
| Years since Residency|| | 22.2 | 12.0 | 23.1 | 12.2 | 17.6 | 9.4 | <0.001 |
|
| |||||||
| Publications | |||||||
|
| |||||||
| Total (SD) | 23.8 | 36.7 | 25.2 | 38.2 | 16.5 | 27.5 | <0.001 |
|
| |||||||
| First/Last Author (SD) | 15.2 | 28.9 | 16.4 | 30.5 | 9.5 | 18.2 | <0.001 |
|
| |||||||
| NIH Grants | |||||||
|
| |||||||
| At least one | 399 | 10.5 | 331 | 10.4 | 68 | 10.8 | 0.77 |
|
| |||||||
| Median, at least one (25–75 pctile) | 4 | 2–9 | 4 | 2–9 | 3 | 1–7 | 0.08 |
|
| |||||||
| Clinical Trials | |||||||
|
| |||||||
| At least one | 410 | 10.8 | 354 | 11.1 | 56 | 8.9 | 0.10 |
|
| |||||||
| Median, at least one (25–75 pctile) | 1 | 1–2 | 1 | 1–2 | 1 | 1–2 | 0.65 |
|
| |||||||
| Total Medicare Payments, 2013--$ (SD) | 91,674 | 101,150 | 95,902 | 106,295 | 70,258 | 65,470 | <0.001 |
Abbreviation: NIH= National Institutes of Health
P values reflect 2-sided t tests and X2 comparisons where appropriate. P value for age reflects comparison of age distributions.
Sub-specialty classification was based on American Board of Internal Medicine (ABIM) sub-specialty board certification.
All cardiologists without ABIM certification in electrophysiology or interventional cardiology.
Top 20 school refers to whether a physician was on faculty at a medical school ranked among the top 20 US medical schools for research by US News & World Report in 2013.15
Calculations excluded 287 cardiologists for whom data on years since residency was unavailable.
Multivariable Analysis
After adjusting for age, sub-specialty, years since residency, publication number, NIH funding, clinical trial participation, affiliation with a medical school ranked highly in research, and 2013 Medicare payments, female cardiologists were less likely than male cardiologists to be full professors (OR 0.63; 95% CI: 0.43, 0.94; p=0.02; Table 2; absolute difference in proportion, −4.0%; 95% CI: −7.5% to −0.7%, eTable 2). In addition to male sex, full professorship was positively associated with age, sub-specialization in electrophysiology or interventional cardiology, years since residency completion, total publication number, NIH funding, and conducting at least one clinical trial, and negatively associated with total Medicare payments.
Table 2.
Multivariable Analysis of Sex Differences in Full Professorship Among U.S. Academic Cardiologists
| Full Professor (vs. Assistant and Associate)*
|
|||
|---|---|---|---|
| No./ Total (%) of Professors | Adjusted Odds Ratio (95% CI)† | P-Value | |
| Sex | |||
|
| |||
| Men | 973 / 3180 (30.6) | 1.00 | — |
|
| |||
| Women | 100 / 630 (15.9) | 0.63 (0.43, 0.94) | 0.02 |
|
| |||
| Age | |||
|
| |||
| Age <50 | 51 / 1605 (3.2) | 1.00 | — |
|
| |||
| Age 50–54 | 146 / 537 (27.2) | 5.67 (3.4, 9.5) | <0.001 |
|
| |||
| Age 55–59 | 217 / 483 (44.9) | 8.53 (4.6, 15.9) | <0.001 |
|
| |||
| Age 60–64 | 242 / 464 (52.2) | 6.03 (2.9, 12.6 | <0.001 |
|
| |||
| Age 65+ | 375 / 607 (61.8) | 3.24 (1.3, 8.2) | 0.01 |
|
| |||
| Sub-Specialty‡ | |||
|
| |||
| Non-Invasive | 772 / 2598 (29.7) | 1.00 | — |
|
| |||
| Electrophysiology | 125 / 497 (25.2) | 1.96 (1.3, 2.9) | 0.001 |
|
| |||
| Interventional | 176 / 715 (24.6) | 1.39 (1.0, 1.9) | 0.05 |
|
| |||
| Years Since Residency (per 1 yr) | 1.17 (1.1, 1.2) | <0.001 | |
|
| |||
| Publication (per 1 pub)§ | |||
|
| |||
| Total | 1.03 (1.02, 1.03) | <0.001 | |
|
| |||
| First/Last Author | 1.00 (1.00, 1.01) | 0.20 | |
|
| |||
| NIH Grant|| | |||
|
| |||
| None | 827 / 3411 (61.7) | 1.00 | — |
|
| |||
| At least one | 246 / 399 (28.2) | 1.86 (1.2, 2.9) | 0.004 |
|
| |||
| Clinical Trial Investigator | |||
|
| |||
| None | 871 /3400 (25.6) | 1.00 | — |
|
| |||
| At least one | 202 / 410 (49.3) | 2.10 (1.4, 3.1) | <0.001 |
|
| |||
| Top 20 Med School Faculty | |||
|
| |||
| No | 673 / 2440 (27.6) | 1.00 | — |
| Yes | 364 / 1248 (29.2) | 0.36 (0.04, 3.5) | 0.38 |
|
| |||
| 2013 Medicare Payment (per $10,000) | 0.02 (0.00, 0.13) | <0.001 | |
Abbreviation: NIH, National Institutes of Health
Factors associated with full professorship among faculty of all ranks.
Each model estimated the association between faculty rank and physician sex, adjusted for age, years since residency, Cardiology sub-specialty (e.g. non-invasive vs. electrophysiology vs. interventional cardiology), publications (total, first & last author), whether a physician was ever principal investigator on an NIH grant, whether a physician had conducted a clinical trial, whether a physician was faculty at a top 20 US medical school in terms of US News & World Report 2013 medical school research ranking,15 each physician’s annual Medicare revenue in 2013, and medical school-level fixed effects.
Sub-specialty classification was based on ABIM sub-specialty board certification as of November 10, 2014.
The reported association between faculty rank and publication count reflects the marginal effect of an additional publication on the probability of a given faculty rank.
NIH grant information was obtained from the NIH RePORT grants database. Clinical trial information was obtained from ClinicalTrials.gov database.
In additional adjusted analyses, we found no sex differences in the proportions of associate and full professors, as compared to assistant professors, (OR 1.07; 95% CI: 0.8, 1.5; p=0.67; Table 3; adjusted difference, 0.8%; 95% CI: −2.8% to 4.3% eTable 3). However, among associate and full professors, women remained significantly less likely than men to be full professors after multivariable adjustment (OR 0.62; 95% CI: 0.40, 0.94, p=0.03; adjusted difference, −7.6%; 95% CI: −13.5% to −0.9%).
Table 3.
Multivariable Analyses of Sex Differences in Secondary Outcomes Among U.S. Academic Cardiologists
| Associate & Full Professor (vs. Assistant)* | Full Professor (vs. Associate)† | |||||
|---|---|---|---|---|---|---|
| No./ Total (%) of Professors | Adjusted Odds Ratio (95% CI)‡ | P-Value | No./ Total (%) of Professors | Adjusted Odds Ratio (95% CI)‡ | P-Value | |
| Sex | ||||||
| Men | 1693 / 3180 (53.2) | 1.00 | — | 973 / 1693 (57.5) | 1.00 | — |
| Women | 251 / 630 (39.8) | 1.07 (0.8, 1.5) | 0.67 | 100 / 251 (39.8) | 0.62 (0.40, 0.94) | 0.03 |
| Age | ||||||
| Age <50 | 348 / 1605 (21.7) | 1.00 | — | 51 / 348 (14.7) | 1.00 | — |
| Age 50–54 | 348 / 537 (64.8) | 1.72 (1.2, 2.5) | 0.005 | 146 / 348 (42.0) | 3.74 (2.2, 6.4) | <0.001 |
| Age 55–59 | 342 / 483 (70.8) | 0.88 (0.5, 1.4) | 0.62 | 217 / 342 (63.5) | 6.10 (3.2, 11.5 | <0.001 |
| Age 60–64 | 341 / 464 (73.5) | 0.37 (0.20, 0.7) | 0.001 | 242 / 341 (71.0) | 5.05 (2.3, 10.9) | <0.001 |
| Age 65+ | 498 / 607 (82.0) | 0.15 (0.07, 0.33) | <0.001 | 375 / 498 (75.3) | 2.33 (0.9, 6.2) | 0.09 |
| Sub-Specialty‡ | ||||||
| Non-Invasive | 1323 / 2598 (50.9) | 1.00 | — | 772 / 1323 (58.4) | 1.00 | — |
| Electrophysiology | 264 / 497 (53.1) | 1.94 (1.4, 2.7) | <0.001 | 125 / 264 (47.3) | 1.44 (0.96, 2.2) | 0.08 |
| Interventional | 357 / 715 (49.9) | 1.25 (0.95, 1.7) | 0.11 | 176 / 357 (49.3) | 1.38 (0.96, 2.0) | 0.09 |
| Years Since Residency (per 1 yr) | 1.25 (1.21, 1.29) | <0.001 | 1.16 (1.1, 1.2) | <0.001 | ||
| Publication (per 1 pub)§ | ||||||
| Total | 1.04 (1.03,1.05) | <0.001 | 1.02 (1.01,1.02) | <0.001 | ||
| First/Last Author | 1.00 (1.00, 1.01) | 0.18 | 1.00 (1.00, 1.01) | 0.32 | ||
| NIH Grant|| | ||||||
| None | 1611 / 3411 (47.2) | 1.00 | — | 827 / 1611 (51.3) | 1.00 | — |
| At least one | 333 / 399 (83.5) | 1.09 (0.7, 1.7) | 0.73 | 246 / 333 (73.9) | 1.76 (1.1, 2.7) | 0.01 |
| Clinical Trial Investigator | ||||||
| None | 1621 / 3400 (47.7) | 1.00 | — | 871 / 1621 (53.7) | 1.00 | — |
| At least one | 323 / 410 (78.8) | 2.64 (1.8, 3.9) | <0.001 | 202 / 323 (62.5) | 1.66 (1.1, 2.5) | 0.01 |
| Top 20 Med School Faculty | ||||||
| No | 1236 / 2440 (50.7) | 1.00 | — | 673 / 1236 (54.4) | 1.00 | — |
| Yes | 658 / 1248 (52.7) | 1.41 (0.2, 10.2) | 0.73 | 364 / 658 (55.3) | 0.35 (0.04, 3.2) | 0.35 |
| 2013 Medicare Payment (per $10,000) | 0.11 (0.03, 0.35) | <0.001 | 0.08 (0.01, 0.5) | 0.009 | ||
Abbreviation: NIH, National Institutes of Health
Factors associated with associate or full professorship among faculty of all ranks.
Factors associated with full professorship among faculty at the associate or full professor rank.
Each model estimated the association between faculty rank and physician sex, adjusted for age, years since residency, cardiology sub-specialty (e.g. non-invasive vs. electrophysiology vs. interventional cardiology), publications (total, first and last author), whether a physician was ever principal investigator on an NIH grant, whether a physician had conducted a clinical trial, whether a physician was faculty at a top 20 US medical school in terms of US News & World Report 2013 medical school research ranking,15 each physician’s annual Medicare revenue in 2013, and medical school-level fixed effects.
Sub-specialty classification was based on ABIM sub-specialty board certification.
The reported association between faculty rank and publication count reflects the marginal effect of an additional publication on the probability of a given faculty rank.
NIH grant information was obtained from the NIH RePORT grants database. Clinical trial information was obtained from ClinicalTrials.gov database.
Across US medical schools we observed sizeable variation in sex differences in full professorship among cardiologists (Figure 1). In adjusted analyses, all medical schools in our analysis had negative gaps in full professorship. The adjusted absolute school-specific gaps ranged from approximately −1.4% to −5.2%, and the median gap was −4.8 % (interquartile range −4.2% to −5.1%).
Figure 1.
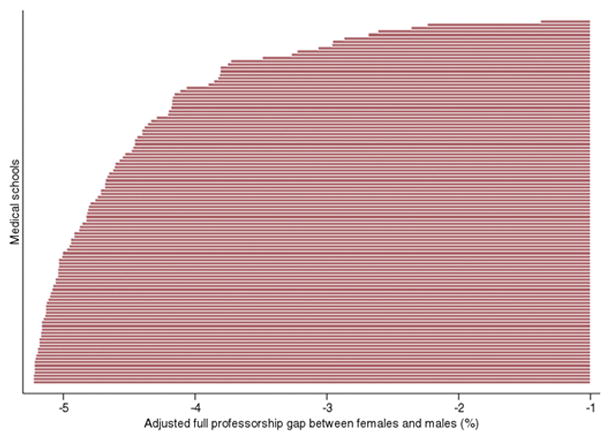
Medical School Level Variation in Actual Versus Expected Sex Differences in Full Professorship
This figure presents the results of an analysis of adjusted sex differences in full professorship across 109 US medical schools in this analysis. Each bar corresponds to a single US medical school and represents the adjusted difference in proportion of full professors among women versus men. Adjusted sex differences in proportion for each medical school were calculated in the following way: Using the multivariable regression model from the primary analysis, the difference in adjusted proportions of full professorship between women and men for each medical school were estimated as if all cardiologists in the study were affiliated with that medical school. Then, the difference between the observed and predicted sex differences in full professorship for each school was calculated. More negative differences representing greater sex disparities in full professorship.
Sex Differences in Full Professorship Across Internal Medicine Sub-specialties and by Medical School Ranking
Cardiology and infectious disease were the only two internal medicine specialties in which women had significantly lower odds of full professorship than men (adjusted OR for infectious disease: 0.33, 95% CI: 0.19, 0.57, p <0.001) (Table 4). In analyses stratified by medical school ranking within, or outside of, the top 20 for research by U.S. News & World Report,15 female cardiologists had non-significantly lower odds of full professorship than men in both sub-groups (Top 20 medical schools: OR 0.65, 95% CI: 0.34, 1.22; p=0.18; Non-top 20 medical schools: OR 0.62, 95% CI: 0.37, 1.04; p=0.07). Infectious disease was the only specialty studied which had significant sex differences in full professorship in both medical school strata (Top 20 medical schools: OR 0.10, 95% CI: 0.03, 0.33; p <0.001; Non-top 20 medical schools: OR 0.47, 95% CI: 0.24, 0.93; p=0.03).
Table 4.
Sex Differences in Full Professorship Across Internal Medicine Subspecialties
| Subspecialty | Adjusted OR * (95% CI) | P-value |
|---|---|---|
| ALL MEDICAL SCHOOLS† | ||
| Cardiology (N=3810) | 0.63 (0.43, 0.94) | 0.02 |
| Endocrinology (N=1270) | 0.98 (0.48, 1.97) | 0.95 |
| Gastroenterology (N=1891) | 0.67 (0.38, 1.20) | 0.18 |
| Infectious Disease (N=1910) | 0.33 (0.19, 0.57) | < 0.001 |
| Nephrology (N=1518) | 0.66 (0.35, 1.25) | 0.20 |
| Oncology (N=1374) | 1.09 (0.61, 1.94) | 0.77 |
| Pulmonology (N=1587) | 0.99 (0.47, 2.09) | 0.99 |
| Rheumatology (N=810) | 1.00 (0.33, 3.00) | 1.00 |
| TOP 20 MEDICAL SCHOOLS‡ | ||
| Cardiology (N=1248) | 0.65 (0.34, 1.22) | 0.18 |
| Endocrinology (N=454) | 1.07 (0.35, 3.27) | 0.91 |
| Gastroenterology (N=579) | 1.09 (0.41, 2.91) | 0.86 |
| Infectious Disease (N=583) | 0.10 (0.03, 0.33) | < 0.001 |
| Nephrology (N=443) | 0.87 (0.33, 2.26) | 0.77 |
| Oncology (N=589) | 0.69 (0.28, 1.71) | 0.42 |
| Pulmonology (N=469) | 1.23 (0.43, 3.54) | 0.70 |
| Rheumatology (N=301) | 0.60 (0.12, 3.04) | 0.54 |
| NON-TOP 20 MEDICAL SCHOOLS§ | ||
| Cardiology (N=2562) | 0.62 (0.37, 1.04) | 0.07 |
| Endocrinology (N=816) | 1.06 (0.39, 2.84) | 0.91 |
| Gastroenterology (N=1312) | 0.48 (0.22, 1.05) | 0.07 |
| Infectious Disease (N=1327) | 0.47 (0.24, 0.93) | 0.03 |
| Nephrology (N=1075) | 0.62 (0.25, 1.54) | 0.30 |
| Oncology (N=785) | 1.72 (0.77, 3.82) | 0.18 |
| Pulmonology (N=1118) | 0.88 (0.28, 2.78) | 0.83 |
| Rheumatology (N=509) | 4.50 (0.64, 31.70) | 0.13 |
This table presents the results of comparisons of sex differences in full professorship in 2014 in cardiology and seven other internal medicine subspecialties.
OR = odds ratio.
The top third of the table presents adjusted odds ratios of full professorship among women versus men at all US medical schools (odds ratios < 1 are consistent with lower rates of full professorship among women relative to men). Odds ratios are adjusted for: age, years since residency, publications (total and first/last author), NIH grant awards (yes/no), serving as principal or co-investigator on at least one clinical trial (yes/no), affiliation with Medical school ranked in top 20 for research in 2013 by US News & World Report,15 and total Medicare payments in 2013. For cardiologists, odds ratios are also adjusted for cardiology subspecialty practice (non-invasive, electrophysiology, or interventional cardiology).
Adjusted odds ratios of female versus male full professors by internal medicine subspecialty at US medical schools ranked in top 20 for research in 2013 by US News & World Report.15
Sensitivity Analyses
The presence of NIH funding did not modify the relationship between physician sex and full professorship (p=0.99 for interaction term), indicating that similar sex differences in full professorship were present among academic cardiologists with and without NIH funding. Among cardiologists with at least one NIH grant, women had non-significantly lower adjusted odds of having two or more funding awards (OR 0.55, 95% CI: 0.21, 1.5) (Table 5). Compared to cardiologists with one NIH grant, those with two or more funding awards had significantly greater adjusted odds of being full professors, though the confidence intervals around the odds ratio estimate were wide and approached one (OR 5.38, 95% CI: 1.03, 28.2).
Table 5.
Sensitivity of Differences in Full Professorship to NIH Funding Among U.S. Cardiologists with at Least One NIH Award
| OR (95% CI)* | |
|---|---|
| Adjusted odds of having more than one NIH award among women versus men (N=399)† | 0.55 (0.2, 1.5) |
| Adjusted odds of full professorship from multiple NIH awards versus one award (N=399)‡ | 5.38 (1.03, 28.2) |
This table presents the results of sensitivity analyses of the impact of NIH funding status on the probability of full professorship among 399 academic cardiologists with at least 1 NIH grant award as of November, 2014.
OR = odds ratio; CI = confidence interval;
Odds ratio represents the adjusted odds of being a full professors among all female cardiologists with at least one NIH award divided by the adjusted odds of being a full professor among all men with at least one NIH award.
Odds ratio represents the adjusted odds of being a full professor among all cardiologists with two or more NIH awards divided by the adjusted odds of being a full professor among all cardiologists with one NIH award. Analyses were adjusted for adjusted for age, years since residency, publications (total and first/last author), serving as principal or co-investigator on at least one clinical trial (yes/no), cardiology subspecialty practice (non-invasive, electrophysiology, or interventional cardiology), affiliation with US medical school ranked in top 20 for research in 2013 by US News & World Report,15 and total Medicare payments in 2013.
Identifying interventional cardiologists and electrophysiologists using Medicare reimbursements alone, or a combination of ABIM board certification and Medicare reimbursements, did not affect our findings regarding sex differences in full professorship (Appendices A–B).
DISCUSSION
We used a comprehensive national database of US physicians to evaluate sex differences in academic rank among US cardiologists with faculty appointments at a US medical school in 2014. After adjusting for physician age, sub-specialty training in interventional cardiology or electrophysiology, years since residency training, and several measures of research and clinical productivity, we found that female cardiologists were significantly less likely than their male colleagues to be full professors. Our findings are consistent with recent and older work examining sex differences in academic rank in medicine—including a recent analysis of more than 90,000 US academic physicians which utilized the same database that we employed for this study, and a 20 year old, survey-based study of sex disparities in academic advancement among US pediatricians.1,14
To our knowledge, this study is the first such analysis to investigate sex differences in academic rank among US cardiologists. Previous work has identified several drivers of sex differences in academic rank in medicine, including asymmetric home and childcare responsibilities between men and women,21,22 lack of effective mentorship and role models for women,23–25 lack of institutional support—particularly for early career female researchers5—inconsistent offering of alternative, and part-time tenure tracks for non-researchers,26–29 sex bias favoring men in the NIH award application review process generally, and for RO1 awards and repeat funding in particular,17,18 attrition of female academics at higher levels in the academic hierarchy,30 overt sex discrimination, and unconscious sex bias.8,12,13,25,30 Female cardiologists report having to contend with many of these challenges. For example, female cardiologists are more likely to delay getting married or starting a family in order to focus on their training.8,31 Despite the fact that women in cardiology are significantly more likely than men to modify their training or career plans to avoid radiation exposure, 30% of women in cardiology report having performed procedures with radiation risk while pregnant. Female cardiologists are also more likely than men to rely on multiple sources of childcare, and to pay for a fulltime caregiver—in large part because the majority of male cardiologists with children have spouses who provide fulltime childcare.8 Overall, more women than men in cardiology perceive that their personal commitments conflict with their work, and hinder their professional advancement.8 In addition, female cardiologists are paid less than men even after accounting for several factors known to impact salary, and the majority of women—69% in a recent survey, versus 22% of men—report having experienced workplace discrimination during their careers.8,9 While this same study found that women and men were similarly satisfied with the availability and quality of mentors, several other studies have found that women in medicine generally, and cardiology in particular, struggle more than men to find effective mentorship and role models.7,8,14,32,33
While the proportion of US female cardiologists practicing in academic settings is increasing,7,8 we are aware of only two survey-based studies—both performed by the ACC’s Women in Cardiology Council—which report results specifically about women in academic cardiology. The more recent of these two analyses found that women in academic cardiology were significantly more dissatisfied with their careers than men; importantly, this finding did not generalize to analyses of cardiologists in non-academic practices.8 Academic and non-academic female cardiologists may have different career goals and priorities, and may face different combinations of barriers to professional advancement. Therefore, studies focused on the experiences of women in academic cardiology would be extremely helpful for understanding the particular forces that influence career advancement for these women.
We also found that while female and male cardiologists were similarly likely to be associate or full professors (a combined outcome), women were less likely than men to hold the title of full professors than associate professor. Because these analyses do not control for cardiologists who exited each of these academic tiers in 2014, no firm conclusions can be drawn from our work about the presence of sex disparities in promotion among academic cardiologists. However, if sex disparities in promotion in academic cardiology do exist, these differences may exist at one or multiple levels in the academic hierarchy. Moreover, because disparities at different academic levels may have different root causes, disparate approaches may be necessary to effectively address them.1
Our retrospective cross-sectional study design limits our ability to identify causal mechanisms underlying our findings. Nonetheless, we identified multiple independent predictors of cardiologists’ academic rank which have implications for future efforts to identify causal links between physician sex and academic rank generally, and within cardiology in particular. For example, physician age and experience (as determined by years since residency) were strongly and independently associated with academic rank, and the female cardiologists in our analysis were younger, and had fewer years of experience. It is possible that age and experience afford professional opportunities—including promotion to local and national leadership positions, the receipt of awards, or simply time to cultivate a reputation—which increase the likelihood of promotion, but which we could not measure. Experience may be particularly important for individuals who are promoted on clinical tracks, and the fact that we did not identify an independent association between academic rank and the number of first and last author publications—which are widely viewed to impact academic advancement among researchers—raises the possibility that many of the cardiologists in our study were being promoted on clinical tracks. Furthermore, the fact that women had fewer total publications than men, and that total publications were positively associated with academic rank, raises the possibility that our results could reflect sex differences in access to resources necessary to generate high publication volumes—including mentorship, time, funding (particularly early career funding), and research networks and teams. Previous work has demonstrated sex differences in physicians’ access to each of these resources.4,7–10,24 In addition, sub-specialization in interventional cardiology and electrophysiology—cardiology sub-specialties in which women are relatively underrepresented—was also independently and positively associated with academic rank. While the mechanisms underlying this association are unclear, they could reflect one or more of several factors—including population-level demand for invasive services, greater revenue generation by invasive relative to non-invasive specialists, and greater likelihood of participation in one of the many clinical trials of invasive cardiovascular disease treatments.
The significant heterogeneity in sex differences in full professorship across internal medicine specialties that we observed are generally consistent with findings from a previous study demonstrating sex differences in academic rank across medical specialties.1 Importantly, this finding suggests that “local,” specialty-specific elements—including access to mentorship, research time protection, and decisions about whom to recommend for promotion—may contribute as much, if not more, to sex disparities in rank as institutional and systems-level policies. These findings also highlight that additional efforts to understand and compare promotion practices across internal medicine specialties may help to elucidate mechanisms underlying sex differences within cardiology.
Several factors may contribute to the variation across US medical schools in the adjusted full professorship gap for female cardiologists observed in this study. First, different promotion practices and criteria across medical schools—including variations in the types of tenure tracks offered,27,28 thresholds for promotion,29,34 work life balance and part-time tenure-track policies,21,35 and the length of probationary periods prior to achieving a tenure-track position,26 may influence male and female academic cardiologists differently. For example, there exists significant heterogeneity across medical schools in the presence and design of clinician educator tracks (CET) and in the eligibility of physicians on CET tracks for tenure.28 CETs—which have proliferated in the past twenty years—were available at roughly 75% of US Medical schools in 2011.28 While more than 75% of CETs contain more women than men, physicians in CETs are often promoted more slowly than those in tenure and research tracks. Even though medical schools use objective criteria to assess faculty performance, the promotion process remains heavily influenced by subjective assessments by divisional and departmental leaders. Indeed, at up to one half of medical schools, department and promotion committee chairs disagree significantly on the relative importance of different CET promotion criteria.29 Second, medical schools, and their cardiology divisions, may vary in terms of their focus on recruiting, supporting, and retaining female cardiologists. Third, cardiology training programs vary widely in their missions, and in their capacity to prepare trainees for successful careers in academic cardiology. Importantly, sex differences in full professorship among cardiologists were consistent across medical schools ranked highly and less highly in research, arguing against effect modification due to differential prioritization of research success across schools. Nonetheless, we do not know the degree to which these, and other factors, account for our findings. Thus, further research is necessary to understand the origins of variation across medical schools in sex differences in academic rank. This finding also intimates that efforts to rectify national disparities should include interventions at the medical school level. Efforts to widely disseminate information about the experiences of those schools with the smallest sex differences in academic rank might help leaders of schools with larger (e.g. “more negative”) sex-based professorship gaps to learn how to more effectively mitigate them.
One commonly proposed explanation for apparent sex differences in promotion or achievement is that women, but not men, may take several months-years off from work for childbearing. It is certainly plausible that maternity leave could delay the attainment of a given academic rank. However, the ACC Women in Cardiology council’s most recent Professional Life Survey found that fewer than 25 % of female and male cardiologists interrupted training or clinical practice for three or more months, only 11% of female and male cardiologists interrupted clinical practice for six or more consecutive months, and that female trainees were significantly less likely than male trainees to interrupt training for twelve or more months.8 It therefore seems improbable that our findings could be attributed solely to the fact that women take off more time than men to bear children. Furthermore, more than three quarters of female cardiologists with children have one or two children, suggesting that the cumulative amount of maternity leave taken by female cardiologists is similarly unlikely to explain our findings.
Importantly, our results may partially assuage legitimate concerns that the constellation of challenges faced by women in cardiology are dissuading young female trainees from pursuing careers in cardiology generally, and academic cardiology in particular.7,10,31 Indeed, more than half of the female cardiologists in this study were under the age of 50, and 37.2% were less than 45 years. While longitudinal data are necessary to determine if and how these demographics are changing over time, this finding is nonetheless encouraging.
Our study has several limitations. First, we lacked information about faculty career track, which could confound our results if women are less likely to be full professors because they disproportionately pursue non-research tracks, in which full professorship is less common.28 We partially addressed this issue by adjusting for total Medicare reimbursement, which should correlate with total clinical volume, and being on a non-research track. In addition, we performed a sensitivity analysis which demonstrated that sex differences in full professorship did not differ significantly between those with NIH funding—who presumably are more likely to be on full-time research tracks—and those without it. Second, we lacked data on whether cardiologists in our cohort worked full time or part time, which could also potentially confound our results if women are more likely to work part time. However, previous work demonstrates that the vast majority of female and male cardiologists—at-least 80% of women and 80–90% of men—work full time.8,9 Thus, any sex differences in full time employment among academic cardiologists which do exist are likely modest in size, and unlikely to single-handedly explain our findings. Third, our database did not include information about non-NIH grant awards. Many clinician-researchers in cardiology rely on grant support from non-governmental organizations, including the American Heart Association (AHA) and private businesses, and early career investigators may receive institutional support for their work.4,5 It is therefore likely that using NIH awards as the sole measure of external financial support for research underestimates the number of cardiologists with research support. Nonetheless, by also examining publications and clinical trials—two of the major products of funded research—we likely capture, and adjust for, much of the individual variation in research productivity and non-NIH research funding. Fourth, because clinical trial registration on clinicaltrials.gov attributes each clinical trial to a single principal investigator, our approach may therefore underestimate cardiologists’ involvement in clinical trials. Fifth, we did not adjust for administrative and leadership roles—such as division chair or fellowship director—that could impact academic rank. Sixth, because our study was cross sectional, we could not assess for sex differences in promotion. Longitudinal data are needed to evaluate promotion practices. Seventh, our measures of research and clinical productivity do not account for several factors that may impact academic advancement—including teaching awards, presentations, committee service, and peer evaluations. However, these factors may have a greater impact on the promotion of physicians on non-research tracks, including CET, which include more women than men. Thus, adjusting for these factors could increase sex disparities in academic rank. Eighth, academic cardiologists likely vary widely in their career priorities and interest in becoming full professors. Our analyses do not control for this heterogeneity of values and priorities. Finally, we cannot rule out residual confounding due to unmeasured variables.
CONCLUSION
Among more than 3800 academic cardiologists with faculty appointments at US medical schools in 2014, women were less likely than men to be full professors, even after accounting for age, years since residency, sub-specialty practice, Medicare reimbursements, and several measures of research productivity.
Supplementary Material
Clinical Perspective.
What is New?
This analysis investigated sex differences in academic rank among 3810 cardiologists affiliated with 109 US medical schools in 2014.
After adjusting for age, clinical experience, cardiology subspecialty, and multiple measures of research and clinical productivity, the authors found that the odds of being a full professor were 37% lower among women than men (adjusted OR: 0.63, 95% CI: 0.43, 0.94), p = 0.02).
In comparisons of sex differences in full professorship across 8 internal medicine specialties, cardiology and infectious disease were the only two subspecialties in which women had significantly lower odds of full professorship than men.
Clinical Implications
Significant sex differences in academic rank exist among cardiology faculty at US medical schools, and these sex differences are not explained by a number of factors that influence academic rank, including several measures of research and clinical productivity.
Additional efforts to understand the mechanisms underlying these disparities, and to develop targeted interventions to correct them, are urgently needed.
In particular, further investigations of the heterogeneity in sex differences in academic rank across internal medicine specialties may help to elucidate factors that propagate these disparities within cardiology.
Acknowledgments
FUNDING SOURCES
The authors report funding grant 1DP50D017897-01 Early Independence Award from the Office of the Director, National Institutes of Health (Dr. Jena).
Footnotes
DISCLOSURES
None.
References
- 1.Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex Differences in Academic Rank in US Medical Schools in 2014. JAMA. 2015;314:1149–1158. doi: 10.1001/jama.2015.10680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Magrane D, Jolly P. The Changing Representation of Men and Women in Academic Medicine. Annals in Brief (Association of American Medical Colleges) [Internet] 2005:1–2. [cited 2013 April 10] Available from: http://www.aamc.org.
- 3.Association of American Medical Colleges. Total Graduates by US Medical School, Sex, and Year, 2010–2011 through 2014–2015. [Internet] 2015 [cited 2016 Aug 18]; Available from: https://www.aamc.org/
- 4.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender Differences in Salary in a Recent Cohort of Early-Career Physician-Researchers. Acad Med. 2013;88 doi: 10.1097/ACM.0b013e3182a71519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sege R, Nykiel-Bub L, Selk S. Sex Differences in Institutional Support for Junior Biomedical Researchers. JAMA. 2015;314:1175–1177. doi: 10.1001/jama.2015.8517. [DOI] [PubMed] [Google Scholar]
- 6.Ash AS, Carr PL, Goldstein R, Friedman RH. Compensation and advancement of women in academic medicine: Is there equity? Ann Intern Med. 2004;141:205–212. doi: 10.7326/0003-4819-141-3-200408030-00009. [DOI] [PubMed] [Google Scholar]
- 7.Limacher M, Zaher C, Walsh M, Wolf W, Douglas P, Schwartz J, Wright J, Bodycombe D. The ACC professional life survey: career decisions of women and men in cardiology: A report of the Committee on Women in Cardiology. J Am Coll Cardiol. 1998;32:827–835. doi: 10.1016/s0735-1097(98)00319-2. [DOI] [PubMed] [Google Scholar]
- 8.Poppas A, Cummings J, Dorbala S, Douglas PS, Foster E, Limacher MC. Survey Results: A Decade of Change in Professional Life in Cardiology; A 2008 Report of the ACC Women in Cardiology Council. J Am Coll Cardiol. 2008;52:2215–2226. doi: 10.1016/j.jacc.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Jagsi R, Biga C, Poppas A, Rodgers GP, Walsh MN, White PJ, McKendry C, Sasson J, Schulte PJ, Douglas PS. Work Activities and Compensation of Male and Female Cardiologists. J Am Coll Cardiol. 2016;67:529–541. doi: 10.1016/j.jacc.2015.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warnes CA, Fedson SE, Foster E, Jessup M, Limacher MC, O’Donnell JA, Walsh MN. Working group 2: How to encourage more women to choose a career in cardiology. J Am Coll Cardiol. 2004;44:238–241. doi: 10.1016/j.jacc.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 11.Rodgers GP, Conti JB, Feinstein JA, Griffin BP, Kennett JD, Shah S, Walsh MN, Williams ES, Williams JL. ACC 2009 Survey Results and Recommendations: Addressing the Cardiology Workforce Crisis; A Report of the ACC Board of Trustees Workforce Task Force. J Am Coll Cardiol. 2009;54:1195–1208. doi: 10.1016/j.jacc.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Carnes M, Bland C. Viewpoint: A Challenge to Academic Health Centers and the National Institutes of Health to Prevent Unintended Gender Bias in the Selection of Clinical and Translational Science Award Leaders. Acad Med. 2007;82:202–6. doi: 10.1097/ACM.0b013e31802d939f. [DOI] [PubMed] [Google Scholar]
- 13.Steinpreis RE, Anders KA, Ritzke D. The Impact of Gender on the Review of the Curricula Vitae of Job Applicants and Tenure Candidates: A National Empirical Study. Sex Roles. 1999;41:509–528. [Google Scholar]
- 14.Kaplan SH, Sullivan LM, Dukes KA, Phillips CF, Kelch RP, Schaller JG. Sex Differences in Academic Advancement — Results of a National Study of Pediatricians. N Engl J Med. 1996;335:1282–1290. doi: 10.1056/NEJM199610243351706. [DOI] [PubMed] [Google Scholar]
- 15.U.S. News & World Report. Best Medical Schools: Research [Internet] [cited 2014 Sep 9]; Available from: http://grad-schools.usnews.rankingsandreviews.com/best-graduate-schools/top-medical-schools/
- 16.Association of American Medical Colleges. US Medical School Faculty, 2015 [Internet] 2016 [cited 2016 Aug 8]; Available from: https://www.aamc.org/data/facultyroster/reports/
- 17.Kaatz A, Magua W, Zimmerman DR, Carnes M. A Quantitative Linguistic Analysis of National Institutes of Health R01 Application Critiques from Investigators at One Institution. Acad Med. 2015;90:69–75. doi: 10.1097/ACM.0000000000000442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaatz A, Lee Y-G, Potvien A, Magua W, Filut A, Bhattacharya A, Leatherberry R, Zhu X, Carnes M. Analysis of NIH R01 Application Critiques, Impact and Criteria Scores: Does the Sex of the Principal Investigator Make a Difference? Acad Med. 2016;91:1080–1088. doi: 10.1097/ACM.0000000000001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zipes DP, Downing SM, Kangilaski R, Norcini JJ. The First Cardiac Electrophysiology Examination for Added Qualifications. J Cardiovasc Electrophysiol. 1994;5:641–644. doi: 10.1111/j.1540-8167.1994.tb01186.x. [DOI] [PubMed] [Google Scholar]
- 20.Fiorilli PN, Minges KE, Herrin J, Messenger JC, Ting HH, Nallamothu BK, Lipner RS, Hess BJ, Holmboe ES, Brennan JJ, Curtis JP. Association of Physician Certification in Interventional Cardiology with In-Hospital Outcomes of Percutaneous Coronary Intervention. Circulation. 2015;132:1816–24. doi: 10.1161/CIRCULATIONAHA.115.017523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Welch JL, Wiehe SE, Palmer-Smith V, Dankoski ME. Flexibility in Faculty Work-Life Policies at Medical Schools in the Big Ten Conference. J Womens Health. 2011;20:725–732. doi: 10.1089/jwh.2010.2553. [DOI] [PubMed] [Google Scholar]
- 22.Fox G, Schwartz A, Hart KM. Work-Family Balance and Academic Advancement in Medical Schools. Acad Psychiatry. 2006;30:227–234. doi: 10.1176/appi.ap.30.3.227. [DOI] [PubMed] [Google Scholar]
- 23.Yedidia MJ, Bickel J. Why Aren’t There More Women Leaders in Academic Medicine? The Views of Clinical Department Chairs. Acad Med. 2001;76:453–65. doi: 10.1097/00001888-200105000-00017. [DOI] [PubMed] [Google Scholar]
- 24.Mayer AP, Files JA, Ko MG, Blair JE. Academic Advancement of Women in Medicine: Do Socialized Gender Differences Have a Role in Mentoring? Mayo Clin Proc. 2008;83:204–207. doi: 10.4065/83.2.204. [DOI] [PubMed] [Google Scholar]
- 25.Bickel J, Wara D, Atkinson BF, Cohen LS, Dunn M, Hostler S, Johnson TRB, Morahan P, Rubenstein AH, Sheldon GF, Stokes E. Increasing Women’s Leadership in Academic Medicine: Report of the AAMC Project Implementation Committee. Acad Med. 2002;77:1043–1061. doi: 10.1097/00001888-200210000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Bunton SA, Mallon WT. The Continued Evolution of Faculty Appointment and Tenure Policies at U.S. Medical Schools. Acad Med. 2007;82:281–9. doi: 10.1097/ACM.0b013e3180307e87. [DOI] [PubMed] [Google Scholar]
- 27.Coleman MM, Richard GV. Faculty Career Tracks at U.S. Medical Schools. Acad Med. 2011;86:932–7. doi: 10.1097/ACM.0b013e3182222699. [DOI] [PubMed] [Google Scholar]
- 28.Mayer AP, Blair JE, Ko MG, Hayes SN, Chang Y-HH, Caubet SL, Files JA. Gender Distribution of U.S. Medical School Faculty by Academic Track Type. Acad Med. 2014;89:312–7. doi: 10.1097/ACM.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 29.Atasoylu AA, Wright SM, Beasley BW, Cofrancesco J, Macpherson DS, Partridge T, Thomas PA, Bass EB. Promotion Criteria for Clinician-educators. J Gen Intern Med. 2003;18:711–716. doi: 10.1046/j.1525-1497.2003.10425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carr PL, Ash AS, Friedman RH, et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132:889–896. doi: 10.7326/0003-4819-132-11-200006060-00007. [DOI] [PubMed] [Google Scholar]
- 31.Sanghavi M. Women in Cardiology. Circ Cardiovasc Qual Outcomes. 2014;7:188. doi: 10.1161/CIRCOUTCOMES.113.000449. [DOI] [PubMed] [Google Scholar]
- 32.Jagsi R, Guancial EA, Worobey CC, Henault LE, Chang Y, Starr R, Tarbell NJ, Hylek EM. The “Gender Gap” in Authorship of Academic Medical Literature — A 35-Year Perspective. N Engl J Med. 2006;355:281–287. doi: 10.1056/NEJMsa053910. [DOI] [PubMed] [Google Scholar]
- 33.Carr PL, Ash AS, Friedman RH, et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129:532–538. doi: 10.7326/0003-4819-129-7-199810010-00004. [DOI] [PubMed] [Google Scholar]
- 34.Beasley BW, Wright SM, Cofrancesco J, Jr, Babbott SF, Thomas PA, Bass EB. Promotion Criteria for Clinician-Educators in the United States and Canada: A Survey of Promotion Committee Chairpersons. JAMA. 1997;278:723–728. [PubMed] [Google Scholar]
- 35.Bristol MN, Abbuhl S, Cappola AR, Sonnad SS. Work-Life Policies for Faculty at the Top Ten Medical Schools. J Womens Health. 2008;17:1311–1320. doi: 10.1089/jwh.2007.0682. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


