Abstract
Objective
U.S. hospitals that care for vulnerable populations, “safety-net hospitals” (SNHs), are more likely to incur penalties under the Hospital Readmissions Reduction Program (HRRP), which penalizes hospitals with higher-than-expected readmissions. Understanding whether SNHs face unique barriers to reducing readmissions or whether they underuse readmission-prevention strategies is important.
Design
We surveyed leadership at 1,600 U.S. acute care hospitals, of whom 980 participated, between June 2013–January 2014. Responses on 28 questions on readmission-related barriers and strategies were compared between SNHs and non-SNHs, adjusting for non-response and sampling strategy. We further compared responses between high-performing SNHs and low-performing SNHs.
Results
We achieved a 62% response rate. SNHs were more likely to report patient-related barriers, including lack of transportation, homelessness, and language barriers compared to non-SNHs (p-values<0.001). Despite reporting more barriers, SNHs were less likely to use e-tools to share discharge summaries (70.1% vs. 73.7%, p<0.04) or verbally communicate (31.5% vs. 39.8%, p<0.001) with outpatient providers, track readmissions by race/ethnicity (23.9% vs. 28.6%, p<0.001), or enroll patients in post-discharge programs (13.3% vs. 17.2%, p<0.001). SNHs were also less likely to use discharge coordinators, pharmacists, and post-discharge programs. When we examined the use of strategies within SNHs, we found trends to suggest that high-performing SNHs were more likely to use several readmission strategies.
Conclusions
Despite reporting more barriers to reducing readmissions, SNHs were less likely to use readmission-reduction strategies. This combination of higher barriers and lower use of strategies may explain why SNHs have higher rates of readmissions and penalties under the HRRP.
Keywords: Readmissions, Safety-Net Hospitals, Vulnerable Populations
INTRODUCTION
Hospital readmissions are common and costly(1) and have become a major focus for U.S. policymakers and clinical leaders.(2) One compelling strategy is the use of penalties to improve quality of care. The U.S. federal government has made significant efforts to shift towards value-based payments after passage of the Affordable Care Act (ACA) in 2010. One key program under this Act is the Hospital Readmissions Reduction Program (HRRP) implemented in 2011, which penalizes U.S. hospitals with higher-than-expected readmission rates up to 3% of their base Medicare payments. In fiscal year 2016, CMS penalized 2,592 hospitals, of which over 90% were also penalized the year before.(3) Early evidence shows that the introduction of HRRP is associated with improvements in readmission rates over time.(4)
One major concern regarding penalty programs is that they will disproportionately affect hospitals serving vulnerable populations and/or under financial constraints. For example, one group of U.S. hospitals that have fared particularly poorly under the HRRP are safety-net hospitals (SNHs).(5) Safety-net hospitals are typically the hospitals in communities that disproportionately care for the poor and racial/ethnic minorities. Currently, we know little about why SNHs have higher readmission rates. It is possible that these hospitals face unique barriers to reducing readmissions. Prior research shows that poor and minority patients are at much higher risk of readmissions regardless of the hospitals from which they are discharged.(6–10) This then contributes to higher rates of penalties for SNHs under the new Medicare penalty rules.(6, 11–13) However, it is also possible that SNHs are simply doing less to prevent readmissions, whether due to their limited resources or because they haven’t made it a priority. Understanding whether SNHs are facing specific barriers to readmission prevention or whether they are underusing readmission strategies is critically important in determining how best to design policy or clinical interventions to reduce readmission rates in these hospitals, but to our knowledge, there are currently no national data available to inform this question.
Therefore, through a national survey of U.S. hospital leaders, we sought to answer three questions. First, what are the barriers that hospitals face in their efforts to reduce readmissions, and do these barriers vary between safety-net hospitals and other hospitals? Second, is there a difference in the strategies used to reduce readmissions between SNHs and non-SNHs? Finally, given known wide variation in readmission rates within SNHs alone, do high-performing SNHs employ a different set of strategies to reduce readmissions than low-performing SNHs?
METHODS
Survey Development
We initially conducted a set of case studies examining hospitals’ efforts to reduce readmission rates; this work has been described previously.(14) As part of this work, we developed a survey instrument that was tested with survey experts, hospital personnel, and leaders. The survey instrument asked questions related to 1) barriers hospitals face in reducing readmissions, including patient-, community-, and hospital-related barriers and 2) strategies hospitals use to reduce readmissions (Supplemental Digital Content 2).(15)
Survey Administration
We began in mid-2012 with a list of all 3,172 acute-care hospitals that were eligible for penalties under the HRRP. We excluded Critical Access Hospitals and other facilities not paid under the Inpatient Prospective Payment System (IPPS), and, therefore, ineligible for participation in the penalty program. Based on calculations performed prior to survey administration, we anticipated needing 1,000 survey responses to have adequate power to address our hypothesis. To achieve a response rate of at least 60%, our final sample consisted of 1,600 hospitals.
Furthermore, we designed our survey sample to enable us to pursue secondary analyses that focused on: differences between hospitals that care for a large proportion of black patients (which have previously been shown to have particularly high readmission rates) and other hospitals and differences between hospitals that had high, average, or low 30-day readmission rates. We calculated the overall proportion of Medicare patients at each hospital that are identified as black in the Medicare beneficiary file. We then calculated 30-day risk-adjusted readmission rates for acute myocardial infarction (AMI), congestive heart failure (HF), and pneumonia (PN) in 2008–2010 (the years used to assign hospital penalties during the first year of the HRRP) using the 100% Medicare inpatient file for each hospital using methods previously described.(16) We then selected all of the top 900 hospitals in terms of their proportion black for inclusion in our sample. We divided the remaining 2,272 acute care hospitals into three groups based on performance on readmissions in 2008–2010: top (best) quintile, middle three quintiles, and bottom quintile. We selected 266 hospitals from each of these groups using random number generation. There were a small number of hospitals in our sample that had closed, merged with other hospitals, or become critical access hospitals or long-term care facilities; we replaced these using random selection from the same group.
To identify clinical leaders, we first obtained the hospital leadership list of Chief Medical Officers (CMOs) from the American Hospital Association. Study staff called each hospital leader to verify contact information, and once a recipient was verified, his or her hospital was moved into the active fielding stage. The survey was then fielded in two phases. The first phase (June 2013 to June 2014) was conducted by Datastat (Ann Arbor, MI). Hospitals were mailed a hard copy of the survey, along with a cover letter explaining the intent of the survey and the consent process. This was followed by follow-up phone calls and a second mailing. If requested, recipients were sent a version of the survey as a portable document format (PDF) file. The second phase (June to December 2014) was conducted by research staff at our university and followed a similar protocol – a mailing followed by follow-up phone calls – but also gave hospital leaders the option of completing a web-based version of the survey instrument. The second phase was instituted to ensure an adequately high response rate given the difficulty of completing and mailing the paper-based survey. Throughout the survey, though the initial point of contact was the office of the CMO, we encouraged that individual to reach out to other leaders within the hospital best equipped to help either provide assistance or actually complete the survey. We offered a $100 Amazon gift card as an incentive to complete the survey, which we believe was appropriate for the time required to complete the survey and average level of compensation for the hospital leaders’ time.
Variables
We defined “safety-net hospital” using the Medicare disproportionate share hospital (DSH) patient percentage, which is a measure of hospitals that serve a large number of Medicaid and uninsured individuals, both of which are typically individuals of low socioeconomic status. We considered SNHs to be in the top quartile with the highest DSH percentage and the remaining 75% of hospitals as non-safety-net hospitals (non-SNHs). We then ranked SNHs by composite readmission rate for pneumonia, heart failure, and acute myocardial infarction using 2012 and 2013 Medicare inpatient data and categorized the SNHs in the lowest tertile of readmission rates as “high-performing SNHs” and the other two tertiles as “low-performing SNHs.”
Analysis
For the purposes of analysis, we computed summary statistics both overall and stratified by safety-net hospital status. Responses were tabulated for each question. For multiple-choice or Likert-scale questions, responses were summed within groups as they were defined on the survey (i.e. “never,” “rarely,” “sometimes,” “usually,” and “always”; or “not a challenge,” “moderate challenge,” or “great challenge”).
Survey responses were adjusted for both non-response and sampling strategy. To adjust for non-response, we constructed a logistic regression model in which returning the survey was the primary outcome and hospital characteristics, including size, teaching status, ownership, urban location, and region were predictors. Each hospital received a likelihood of response based on this model; responses were then weighted with the inverse of this likelihood. To adjust for sampling strategy, we assigned sample weights to each group as well. We then compared responses between SNHs and non-SNHs using chi-square tests. Next, we used logistic regression models to adjust for hospital structural characteristics, as described above. We also adjusted for whether the survey was completed in phase 1 versus phase 2. Finally, only within SNHs, we compared the responses between “high-performing SNHs” and “low-performing SNHs.” P-values <0.05 were considered statistically significant.
All responses were de-identified before analysis. Informed consent was obtained within the survey itself; the introductory page to the survey included detailed information about privacy and data de-identification and stated, “Completion of this survey implies informed consent.” The study was approved by the University’s Office of Human Research Administration.
RESULTS
Hospital and Leader Characteristics
Of the 1,600 hospitals contacted, we received completed surveys from 992, for a 62% response rate. Compared with non-respondents, respondents were more often leaders from large hospitals, non-profit hospitals, and teaching hospitals; respondents were also more likely to be located in urban locations and regionalized in the Northeast and Midwest (Supplemental Digital Content 1, Table 1).(17)
Table 1.
Hospital Characteristics
| Hospital Characteristics | Safety-Net Hospital (N=334) |
Non-Safety- Net Hospital (N=646) |
P-value |
|---|---|---|---|
| Size | (%) | (%) | |
| Small [1–99 beds] | 18.3 | 31.7 | <0.001 |
| Medium [100–399 beds] | 53.0 | 53.3 | |
| Large [400+ beds] | 28.7 | 15.0 | |
| Teaching Status | |||
| Teaching | 49.1 | 31.1 | <0.001 |
| Non-teaching | 50.9 | 68.9 | |
| Ownership | |||
| For-profit | 20.7 | 16.7 | <0.001 |
| Non-profit | 79.3 | 83.3 | |
| Region | |||
| Northeast | 15.0 | 13.2 | 0.001 |
| Midwest | 15.3 | 26 | |
| South | 51.8 | 47.2 | |
| West | 18.0 | 13.6 | |
| Type of Location | |||
| Rural | 30.2 | 34.1 | 0.009 |
| Suburban | 0.6 | 3.9 | |
| Urban | 69.2 | 62.1 | |
| Race/Ethnicity | |||
| Black | 25.2 | 10.8 | <0.001 |
| Hispanic | 4.3 | 0.9 | <0.001 |
| Type of Insurance | |||
| Medicare | 39.1 | 49.4 | <0.001 |
| Medicaid | 28.9 | 16.4 | <0.001 |
| Mean Readmission Rate (CHF, PNA, MI) | 22.5 | 20.3 | <0.001 |
CHF=congestive heart failure; PNA=pneumonia; MI=myocardial infarction.
Of those hospitals that completed our survey, 980 had data on DSH index from the AHA survey and comprise our analytic sample. Of these 980 hospitals, 334 (34.1%) were identified as SNHs and 646 (65.9%) were non-SNHs. SNHs were more likely to be large hospitals, teaching hospitals, for-profit, located in the South, and in urban locations compared to non-SNHs (Table 1). Additionally, SNHs cared for more blacks and Hispanics. The mean composite readmission rate for congestive heart failure, pneumonia, and acute myocardial infarction was also higher in SNHs compared to non-SNHs (22.5% vs. 20.3%, p<0.001).
Of survey respondents, 29.6% identified themselves as Directors of Case Management or equivalent, 27.1% as Chief Quality Officers or equivalent, 26.3% as Chief Medical Officers or Chiefs of Staff, 4.6% as Chief Nursing Officers, 2.5% as Chief Executive Officers, and 9.8% as “other,” including Vice President for Medical Affairs and Chief Operating Officer.
Barriers to Reducing Readmissions
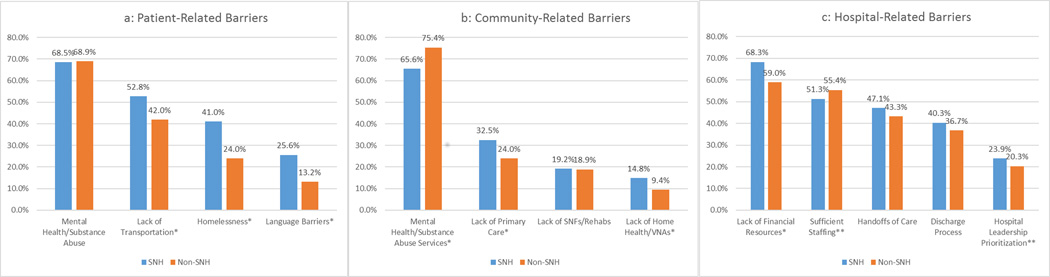
Mental health and substance abuse was equally cited by both SNHs and non-SNHs as the greatest patient-related barrier (68.5% vs. 68.9%, p=0.79). However, SNHs were overall more likely to report more patient-related barriers as great challenges compared to non-SNHs, including lack of transportation (52.8% vs. 42.0%, p<0.001), homelessness (41.0% vs. 24.0%, p<0.001), and language barriers (25.6% vs. 13.2%, p<0.001; Figure 1a).
Figure 1.
Availability of mental health and substance abuse services was again seen by both types of hospitals as the greatest community-related challenge, though SNHs were actually less likely to rate this as a great barrier compared to non-SNHs (65.6% vs. 75.4%, p<0.001). However, SNHs were more likely to report other community-related barriers, including availability of high-quality primary care services (32.5% vs. 24.0%, p<0.001) and home health/visiting nurses’ services (14.8% vs. 9.4%, p<0.001) (Figure 1b).
Finally, SNHs were more likely to identify availability of financial resources (68.3% vs. 59.0%, p<0.001) and prioritization of hospital leadership (23.9% vs. 20.3%, p=0.02) as great challenges (Figure 1c); there were no differences between hospital types in the prevalence of the remainder of the hospital-related barriers.
Strategies to Reduce Readmissions
With regards to tracking readmissions, the majority of hospitals reported having internal tracking systems, though SNHs were slightly less likely to have such systems (Table 2). SNHs were also much less likely to track readmissions by race and ethnicity. Hospital leadership at both types of hospitals were equally likely to receive readmission reports with the exception that individual physicians at SNHs were less likely to receive reports compared to non-SNHs (51.0% vs. 58.4%, p<0.001). With regards to incentives, few hospitals reward hospital leaders and individual physicians based on readmission performance, but to the extent that they did, non-SNHs were twice as likely to offer incentives as SNHs (Table 2).
Table 2.
Hospital Strategies: Tracking, Reporting, and Incentivizing Readmissions
| Hospital Strategies to Reduce Readmissions* | Safety-Net Hospital |
Non-Safety-Net Hospital |
Difference | P-value |
|---|---|---|---|---|
| Track Readmissions | ||||
| Internal Readmission Tracking System | 92.5% | 95.2% | −2.7% | 0.002 |
| Track Readmissions by Race/Ethnicity | 23.9% | 28.6% | −4.7% | 0.005 |
| Receive Feedback on Readmission Performance | ||||
| Hospital Board | 76.7% | 75.9% | 0.8% | 0.646 |
| Chief Executive Officer | 89.4% | 90.4% | −1.0% | 0.399 |
| Chief Medical Officer or Chief Quality Officer | 89.7% | 90.4% | −0.7% | 0.540 |
| Department Chairs/Division Chiefs | 72.1% | 68.8% | 3.3% | 0.060 |
| Individual Physicians | 51.0% | 58.4% | −7.4% | <0.001 |
| Receive Financial Incentives to Reduce Readmissions | ||||
| Chief Executive Officer | 7.2% | 14.7% | −7.5% | <0.001 |
| Chief Medical Officer or Chief Quality Officer | 7.1% | 14.8% | −7.7% | <0.001 |
| Department Chairs | 3.9% | 6.1% | −2.2% | 0.009 |
| Individual Physicians | 4.4% | 9.7% | −5.3% | <0.001 |
Percent of hospital leaders answering “Yes” to specified strategy.
Furthermore, SNHs were less likely to use a number of specific readmission strategies, including the use of health information technology tools to share discharge summaries with outpatient providers, or to provide patients access to mobile web technology or applications for management of disease (Table 3). SNHs were also less likely to use discharge coordinators, pharmacists, and formal discharge checklists. With regards to post-discharge programs, SNHs were also less likely to communicate discharge plans with primary care doctors or enroll patients in disease management or patient engagement programs (Table 3).
Table 3.
Hospital Strategies: Use of Health IT, Discharge Staff, and Post-Discharge Programs
| Hospital Strategy* | Safety- Net Hospital |
Non- Safety- Net Hospital |
Adjusted Difference |
p- value |
|---|---|---|---|---|
| Use of Health IT Tools | ||||
| Electronic Tools to Reconcile Discharge Medications | 76.7% | 77.4% | −0.7% | 0.69 |
| Electronic Tools to Share Discharge Summary | 70.1% | 73.7% | −3.6% | 0.04 |
| Mobile/Web Apps for Patients | 4.7% | 9.8% | −5.1% | <0.001 |
| Dedicated Staff/Resources | ||||
| Use Dedicated Discharge Planners/Coordinators | 72.2% | 76.1% | −3.9% | 0.02 |
| Use Formal Discharge Checklist | 53.9% | 59.5% | −5.6% | <0.01 |
| Use Pharmacists to Reconcile Discharge Meds | 34.6% | 42.8% | −8.2% | <0.001 |
| Use Transition Coaches | 27.8% | 25.2% | 2.6% | 0.13 |
| Post-Discharge Strategies/Programs | ||||
| Schedule follow-up appointments prior to patient leaving the hospital | 71.7% | 67.9% | 3.8% | 0.03 |
| Call Patients within 48 hours after discharge | 66.0% | 66.5% | −0.5% | 0.78 |
| Directly communicate discharge plan with primary care providers prior to discharge | 31.5% | 39.8% | −8.3% | <0.001 |
| Enroll Patients in a Disease Management Program | 13.3% | 17.2% | −3.9% | <0.01 |
| Enroll Patients in a post-discharge patient engagement program | 9.1% | 12.7% | −3.6% | <0.01 |
Percent of hospital leaders answering “usually” or “always” to the use of each specific strategy.
Comparing High-Performing SNHs versus Low-Performing SNHs
When comparing the responses of high-performing SNHs with low-performing SNHs, we found that high-performing SNHs had a mean readmission rate of 17.2% compared to 25.0% in low-performing SNHs for the three target conditions. High-performing SNHs were overall more likely to report the use of electronic tools to reconcile discharge medications (81.6% vs. 71.9%, p<0.04) and much more likely to use discharge coordinators (80.3% vs. 64.9%, p<0.01) (Table 4). There were also trends to suggest that high-performing SNHs report using electronic tools to share discharge summaries with outpatient providers, schedule follow-up appointments, and communicate discharge plans with primary care doctors, however, these differences were not statistically significant from low-performing SNHs (Table 4).
Table 4.
Comparing Strategies in Top-Performing SNHs vs. Low-Performing SNHs
| Hospital Strategy | High-Performing SNHs*† |
Low-Performing SNHs |
Difference | p-value |
|---|---|---|---|---|
| Use of Health IT Tools | ||||
| Electronic Tools to Reconcile Discharge Medications | 81.6% | 71.9% | 9.7% | 0.04 |
| Electronic Tools to Share Discharge Summary | 63.8% | 58.6% | 5.2% | 0.34 |
| Mobile/Web Apps for Patients | 5.4% | 3.7% | 1.7% | 0.98 |
| Dedicated Staff/Resources | ||||
| Discharge Planners/Coordinators | 80.3% | 64.9% | 15.3% | <0.01 |
| Use Formal Discharge Checklist | 52.7% | 53.1% | −0.4% | 0.95 |
| Pharmacists to Reconcile Discharge Medications | 33.3% | 36.3% | −3.0% | 0.58 |
| Transition Coaches | 24.8% | 24.3% | 0.5% | 0.92 |
| Post-Discharge Strategies/Programs | ||||
| Schedule follow-up appointments | 72.7% | 67.7% | 5.0% | 0.33 |
| Call Patients 48hrs after discharge | 59.5% | 59.2% | 0.3% | 0.96 |
| Communicate discharge plan with primary care providers | 34.4% | 31.4% | 3.0% | 0.57 |
Percent of hospital leaders answering “usually” or “always” to the use of each specific strategy.
We ranked SNHs by their risk-adjusted mean readmission rates for acute myocardial infarction, pneumonia, and heart failure. We then categorized the hospitals in the lowest tertile by readmission rates as high-performing SNHs and the remaining two-thirds as low-performing SNHs.
DISCUSSION
In a national survey of U.S. hospital leaders, we found meaningful differences between the perceived barriers and reported use of strategies for hospital readmission reduction between safety-net hospitals and non-SNHs. Not surprisingly, hospitals that care for vulnerable populations were more likely to report patient barriers, including homelessness and lack of transportation, community barriers, including lack of primary care in the community, and hospital-related barriers, specifically availability of financial resources. However, SNHs were also less likely to employ specific strategies to help reduce readmissions, including use of electronic tools, financial incentives, discharge checklists, discharge coordinators, and post-discharge programs. Taken together, the combination of higher barriers and lower use of strategies may explain why SNHs have higher rates of readmissions and higher penalties under the HRRP.
Our study has important implications for policy makers and healthcare providers. First, although it is not surprising that SNHs are generally more likely to report barriers to readmission reduction given the populations they serve, our survey quantifies the extent and type of challenges these hospitals face in their effort to reduce readmissions, including homelessness, transportation issues, and language barriers. However, even among non-SNHs, we found that that barriers related to socioeconomic status were highly prevalent. These findings reflect the significant concern raised by U.S. organizations about the importance of accounting for socioeconomic factors when judging hospital performance under the HRRP. Given the broad consensus on this issue, at least two bipartisan bills have been proposed in Congress to alter the HRRP to take social factors into account.(18, 19)
Our findings point to specific issues that will need to be addressed if we want to comprehensively address hospital readmissions, including mental and behavioral health, which was cited by nearly 70% of hospital leaders as a significant challenge. Given the perceived lack of availability of mental health services in the community, there are serious concern about our ability to effectively treat mental health disorders – with negative resultant effects on our ability to effectively address preventable readmissions.(20) Of course, the effects of our inadequate mental health system are felt far more widely than just readmissions but our findings underscore the importance of tackling this critical issue for the U.S. healthcare system.
Despite reporting more barriers, SNHs were less likely to use several strategies or interventions to reduce readmissions. Critics of SNHs might point to these data as evidence that lack of effective leadership and inadequate attention to readmissions is the primary cause of SNHs being penalized under the U.S. penalty programs. Defenders of SNHs might point out that these hospitals generally have worse baseline financial health and increased fiscal stress,(21, 22) findings reaffirmed by our survey, which may make it more difficult to employ these readmission reduction strategies. Which of these two scenarios – inadequate attention versus focusing on other priorities – is more dominant is unclear and likely varies from organization to organization.
Our work adds to a growing body of literature that illustrates the struggles faced by SNHs in providing care to a patient population with a unique set of needs and challenges. Prior studies have shown that SNHs tend to have worse processes and outcomes of care, as well as poorer performance on patient experience.(6, 10, 22–24) Therefore, our finding that these hospitals employ a significantly lower number of readmission reduction strategies provides some explanation for why these patterns might exist. While much of the concern regarding differences in outcomes between SNHs and non-SNHs is around inadequate risk adjustment for socioeconomic status or medical complexity,(8) differences in the use of strategies to prevent readmissions is less controversial. The finding that high-performing SNHs were more likely to use some of the key strategies we identified suggests that it is possible for SNHs to employ some key strategies to reduce readmissions; however, many of these strategies did not meaningfully differ between high and low performers, which may speak to the fact that many commonly used tactics do not address the social and behavioral determinants that may underlie many readmissions.
These findings have important policy implications. In the U.S., as the federal government continues to develop value-based payment programs in other care settings, including Skilled Nursing and Home Health Value-Based Purchasing programs, the End-Stage Renal Disease Quality Incentive program, and the Medicare Shared Saving Program, similar readmission metrics are being used to assess performance. Therefore, policymakers should be cautious to ensure that performance metrics allow for fair comparisons between hospitals and providers. While providers should not get a pass for providing worse care for poor patients, they should also not be penalized for simply taking care of more poor patients. Another important concern is that the ACA mandates cuts to the DSH subsidies for caring for the nation’s poor, which, combined with HRRP and other programs that penalize SNHs, raises important questions about the viability of these institutions.(11) Providing care for the poor is an important societal goal, and we should ensure that policies support institutions that do so while still holding them accountable for high quality care.
Limitations
There are limitations to our study. First, it is possible that the hospital leaders that responded to our survey were different than those who did not. While we used appropriate techniques to deal with non-response, these statistical techniques are imperfect and our results may not generalize beyond our sample. Second, though we believe that hospital leaders answered survey questions to their best of their ability, it is possible that the strategies and barriers identified by the responders may reflect their personal views rather than those of the larger communities within the hospitals they represent. In addition, there is a risk that hospital leaders are likely to reflect hospital efforts more favorably and avoid criticism of leadership and management, due to social desirability bias. However, we have no reason to believe that this bias would be different across SNHs and non-SNHs. Third, there is no universal approach to define safety-net hospitals, though our approach has been used frequently in the past and represents a group of hospitals that serve a high proportion of poor individuals.(12, 25) Fourth, we used two different phases for survey recruitment; phase 1 was predominantly paper-based, and phase 2 was predominantly an online-survey. Controlling for the recruitment phase did not alter our findings, though we cannot be certain that phase did not impact responses in any way. Fifth, survey responses were based on efforts in 2013–2014. Our classification of “high” and “low” performing SNHs was based on performance in 2012–2013 (the most recent patient-level data available at this time of analysis), which may introduce potential misclassification given the one-year lag; however, given prior findings that hospitals that were penalized in the first years of the program continue to be penalized,(3) we suspect that this issue has a relatively small impact and would likely bias our findings to the null. Finally, our study was cross-sectional, and we did not assess changes in behavior or strategies over time nor their association with improvements in readmission rates, though this represents an important area for future research; we suspect that any misclassification introduced by changes in performance over time would bias our study to the null.
CONCLUSION
In a national survey of U.S. hospital leaders, we found that, in addition to reporting more barriers to reduce readmissions, hospitals that care for large proportions of vulnerable populations were less likely to use a number of promising readmission reduction strategies. Together, these two factors may shed light on why readmission rates are higher at SNHs. In addition to promoting the use of proven strategies to reduce readmissions at SNHs, interventions that address the unique needs of SNHs, particularly in terms of mental health and substance abuse as well as primary care services, may have the potential to reduce readmission rates and improve outcomes for vulnerable populations.
Supplementary Material
Acknowledgments
Disclosure of Funding: The National Heart, Lung, and Blood Institute funded this work (R01HL113567-02). The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the article.
Footnotes
Conflicts of Interest: All authors do not have any conflicts of interest to disclose for the past three years.
Contributor Information
Jose F. Figueroa, Department of Health Policy and Management, Harvard T.H. Chan School of Public Health, Division of General Internal Medicine, Department of Medicine, Brigham and Women’s Hospital, 42 Church Street, Cambridge, MA 02138, Tel: 617-384-5367, Fax: 617-264-6346, jfigueroa@hsph.harvard.edu.
Karen E. Joynt, Department of Health Policy and Management, Harvard T.H. Chan School of Public Health, Division of Cardiovascular Medicine, Department of Medicine, Brigham and Women’s Hospital, 75 Francis Street, Boston, MA 02115, Tel: 617-432-1816, Fax: 617-432-4494, kjoynt@hsph.harvard.edu.
Xiner Zhou, Department of Health Policy and Management, Harvard T.H. Chan School of Public Health, 42 Church Street, Cambridge, MA 02138, Tel: 617-384-5367, Fax: 617-264-6346, xzhou@hsph.harvard.edu.
E. John Orav, Department of Biostatistics, Harvard T.H. Chan School of Public Health, Division of General Internal Medicine, Department of Medicine, Brigham and Women’s Hospital, 1620 Tremont Street 3rd Floor, Boston, MA 02115, Tel: 617-732-5899, orav@hsph.harvard.edu.
Ashish K. Jha, Department of Health Policy and Management, Harvard T.H. Chan School of Public Health, Division of General Internal Medicine, Department of Medicine, Brigham and Women’s Hospital, Division of Medicine, Veterans Affairs Boston Healthcare System, 42 Church Street 2nd Floor, Cambridge, MA 02138, Tel: 617-384-5367, Fax: 617-264-6346, ajha@hsph.harvard.edu.
REFERENCES
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Burwell SM. Setting Value-Based Payment Goals — HHS Efforts to Improve U.S. Health Care. New England Journal of Medicine. 2015;372(10):897–899. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 3.Rau J. Half of nation’s hospitals fail again to escape Medicare’s readmission penalties. Kaiser Health News. 2015 [Google Scholar]
- 4.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. New England Journal of Medicine. 2016;374(16):1543–1551. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 5.Figueroa JF, Wang DE, Jha AK. Characteristics of hospitals receiving the largest penalties by US pay-for-performance programmes. BMJ Qual Saf. 2016 doi: 10.1136/bmjqs-2015-005040. [DOI] [PubMed] [Google Scholar]
- 6.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 7.Joynt KE, Orav E, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnett ML, Hsu J, McWilliams J. Patient characteristics and differences in hospital readmission rates. JAMA Internal Medicine. 2015;175(11):1803–1812. doi: 10.1001/jamainternmed.2015.4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greysen S, Stijacic Cenzer I, Auerbach AD, Covinsky KE. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015;175(4):559–565. doi: 10.1001/jamainternmed.2014.7756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jha AK, Orav EJ, Epstein AM. Low-quality, high-cost hospitals, mainly in south, care for sharply higher shares of elderly black, hispanic, and medicaid patients. Health Aff (Millwood) 2011;30(10):1904–1911. doi: 10.1377/hlthaff.2011.0027. [DOI] [PubMed] [Google Scholar]
- 11.Kahn CN, Ault T, Potetz L, Walke T, Chambers JH, Burch S. Assessing Medicare’s hospital pay-for-performance programs and whether they are achieving their goals. Health Aff (Millwood) 2015;34(8):1281–1288. doi: 10.1377/hlthaff.2015.0158. [DOI] [PubMed] [Google Scholar]
- 12.Chatterjee P, Joynt KE, Orav E, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Archives of Internal Medicine. 2012;172(16):1204–1210. doi: 10.1001/archinternmed.2012.3158. [DOI] [PubMed] [Google Scholar]
- 13.Figueroa JF, Wang DE, Jha AK. Characteristics of hospitals receiving the largest penalties by US pay-for-performance programmes. BMJ Qual Saf. 2016 doi: 10.1136/bmjqs-2015-005040. [DOI] [PubMed] [Google Scholar]
- 14.Joynt KE, Sarma N, Epstein AM, Jha AK, Weissman JS. Challenges in reducing readmissions: lessons from leadership and frontline personnel at eight minority-serving hospitals. Jt Comm J Qual Patient Saf. 2014;40(10):435–437. doi: 10.1016/s1553-7250(14)40056-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Supplemental Digital Content. Reducing Hospital Readmissions: A Survey of U.S. Hospital Leaders
- 16.Grady JN, Bhat KR, Desai MM, Grosso L, Lin Z, Parzynski C, et al. Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Readmission Measure. Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE) New Haven, CT: 2012. 2012. [Google Scholar]
- 17.Supplemental Digital Content. Appendix Table 1: Hospital Characteristics, Respondents vs. Non-Respondents
- 18.Establishing Beneficiary Equity in the Hospital Readmission Program Act of 2015, 114th Congress(2015).
- 19.Smith MW, Stocks C, Santora PB. Hospital readmission rates and emergency department visits for mental health and substance abuse conditions. Community Ment Health J. 2015;51(2):190–197. doi: 10.1007/s10597-014-9784-x. [DOI] [PubMed] [Google Scholar]
- 20.Andrulis DP, Siddiqui NJ. Health reform holds both risks and rewards for safety-net providers and racially and ethnically diverse patients. Health Aff (Millwood) 2011;30(10):1830–1836. doi: 10.1377/hlthaff.2011.0661. [DOI] [PubMed] [Google Scholar]
- 21.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. JAMA. 2008;299(18):2180–2187. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- 22.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 23.Goldman LE, Vittinghoff E, Dudley RA. Quality of care in hospitals with a high percent of Medicaid patients. Med Care. 2007;45(6):579–583. doi: 10.1097/MLR.0b013e318041f723. [DOI] [PubMed] [Google Scholar]
- 24.Wakeam E, Hevelone ND, Maine R, Swain J, Lipsitz SA, Finlayson SR, et al. Failure to rescue in safety-net hospitals: availability of hospital resources and differences in performance. JAMA Surg. 2014;149(3):229–235. doi: 10.1001/jamasurg.2013.3566. [DOI] [PubMed] [Google Scholar]
- 25.Hospital Readmissions Program Accuracy and Accountability Act of 2014, 113th Congress(2014).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.