Abstract
Background:
This study aimed to compare the effects of the schema along with mindfulness-based therapies in the psoriasis patients.
Materials and Methods:
This semi-experimental study with post- and pre-tests was conducted on the psoriasis patients in the Dermatology Clinic of the Isfahan Alzahra Hospital, Iran using the convenience sampling in 2014. The patients had a low general health score. The experimental groups included two treatment groups of schema-based (n = 8) and mindfulness (n = 8). Both groups received eight 90-min sessions therapy once a week; they were compared with 8 patients in the control group. To evaluate the psoriasis patients’ maladaptive schema, Young schema questionnaire was used. Data were analyzed through the covariance analysis test.
Results:
There was a significant difference between the schema-based therapy and mindfulness groups with the control group. There was also a significant difference between the schema-based therapy groups consisting of the defeated schema, dependence/incompetence schema, devotion schema, stubbornly criteria schema, merit schema, restraint/inadequate self-discipline schema, and the control group. Moreover, a significant difference existed between the maladaptive schema of mindfulness therapy group and the controls. There was a significant difference concerning the improvement of the psychopathologic symptoms between the mindfulness therapy group and the control group.
Conclusions:
This study showed similar effects of both the schema and mindfulness-based therapies on the maladaptive schemas in improving the psoriasis patients with the psychopathologic symptoms.
Keywords: General public health, maladaptive schemas, mindfulness, psoriasis
Introduction
Psoriasis is an immune system-related disease, which affects nearly 0.2% of the individuals in society. Skin lesions in 0.5–20% of cases are accompanied with arthritis. The most common form of the disease is psoriasis vulgaris, which is exhibited in the form of annular plaques in the body extensors such as elbows, lower waist, and around the umbilicus.[1] Psoriasis may last for several years and in some patients it recurs and some patients recover.[2] It may be so modest that is not diagnosed or it may be so severe that covers much of the body surface.[3] Psoriasis is a common skin disease, which is more common in the north of Iran.[4]
Psoriasis does not seriously disturb the patients’ physical capabilities; however, it has crucial effects on their psychological status.[1] Thus, patient's social and psychological problems mainly result from the physical problems and cause a negative picture and self-image; therefore, it leads to attenuation in the individual's position in family and his/her self-confidence. Such problems gradually lead to lethargy and sometimes depression. Finally, the patient cannot continue his/her life normally, and this may exacerbate the psychological complications in these patients.[2]
Psoriasis patients have exhibited a high risk for depression, anxiety, and suicide.[5] From cognitivists’ view, physical problems emerge under the effect of interpersonal problems and their imagination of themselves and others, which results in forming the schema.[6] Some of the schemas especially the ones formed due to childhood bitter experiences-may be the main focus of personality disorders, cognitive character problems, and many I-axis disorders. When people surround to the schema, they accept its accuracy. Inefficiency of schemas is revealed when individuals’ schemas are confirmed in their routine style of life and their interactions with others, even if their initial impression is untrue and they would never try to fight the schema or avoid it, but they accept them as true.[7] Initial maladaptive schemas are inefficient mechanisms that directly or indirectly end in the psychological affliction.[8]
Schema, particularly the ones mainly formed owing to the childhood unpleasant experiences, are deep and widespread patterns or themes comprised of memories, excitements, cognitions, and corporal emotions that persist throughout life. They are about self and relation with others and completely inefficient.[7] Initial maladaptive schema is the result of the human tendency for “cognitive harmonization.” Although the individual knows that the schema bothers him/her, he/she is convenient with it, and this comfort leads him/her to the conclusion that his/her schema is right. The outcome of such a perspective is that the schema affects processing of subsequent experiences. Schema plays a fundamental role in the patient's reflection, emotion, behavior, and communication with others and in an inevitable and conflicting way drag the adulthood life to childhood unpleasant condition, which is generally harmful for the patient.[9]
Through distortion, the person puts his finger on data consistent with schema and ignores or disvalues the ones contradicting the schema. Emotionally, the person may block the excitements related to a schema; once an emotion is blocked, the schema will not reach consciousness. Thus effective steps cannot be taken to change or improve it.[10] Behaviorally, the person is involved in self-defeating patterns, unconscious selection, and staying in relations and situations that drive and continue the schema while he/she avoids making relationships that improve the schema. Interpersonally, patients communicate with others in such a manner that stimulates their negative responses, thus reinforcing their own schema.[11]
Schema therapy is an influential treatment in reducing the emotional reactions and symptoms and elevating the patient's quality of life (QoL). Another treatment is mindfulness, which has been expanded in therapeutic works by others.[12] Considering mindfulness-based cognitive therapy (MBCT), individual created mindfulness-based stress reduction and for chronic pains he/she suggested mindfulness exercises such as body search, mediation while walking, yoga exercise, and awareness of every day's life, the individual also taught the participants how to do their work consciously. The individual took major steps in controlling stress through exercises, lectures, educational videotapes, and workshops.[10]
Various mechanisms have been considered to define how mindfulness skills can decrease symptoms and change behaviors. These mechanisms include exposure, cognitive alterations, self-regulation, body relaxation, and acceptance. MBCT group instruction accompanied by concentrating skills in 10 sessions during the second half of pregnancy was influential on the pregnant women's stress, pain, fear, and pregnancy-induced anxiety, which lead to the positive emotions.[12,13] Some investigators showed that the patients with psoriasis, who underwent ultraviolet therapy and simultaneously mindfulness-based intervention (mediation), experienced reduced stress and increased wound healing. Psychological and physical treatment of psoriasis is mutually interactive. On one hand, negative psychological aspects of psoriasis have a direct effect on the patient's mental health.[1]
Moreover, it potentially affects the disease desperation and this psychological status affects treatment motivation and the expectancy for recovery and it intervenes with treatment trend; on the other hand, control or improvement in psoriasis symptoms plays a crucial role in enhancing the patients’ QoL and their mental wellbeing.[14] However, sectional treatments of psoriasis such as topical treatment, light therapy, systemic and biologic medication, and other complementary therapies merely prevent disease recurrence, and they have not managed to provide recovery until now.[14] Several studies have proved that the mindfulness-based therapy has a positive effect on hypertension, stress, anxiety of the pregnant women, QoL, chronic skeletal pains, physical symptoms of the patients with irritable bowel syndrome, and depression of the multiple sclerosis patients.[15,19] In addition, these studies have proved that the schema-based therapy and primary maladaptive schemas have positive effects on the social anxiety and widespread anxiety disorder in the women, respectively.[16,17,18,19] Furthermore, one recent study has shown that the patients with psoriasis, who received mindfulness as an adjunct to their usual therapy, experienced a significant improvement in both psoriasis severity and QoL.[20]
This study aimed to compare the effects of the schema and mindfulness-based therapies on the maladaptive schemas in the psoriasis patients with the psychopathological symptoms. The innovation of this study is the effectiveness of the schema therapy on the maladaptive schemas of chronic diseases. Since no information is available which shows that patients with psoriasis are classified into the class of chronic diseases, who more likely to have personality disorders? Therefore, this conception needs further investigations.
Materials and Methods
A useful consort flowchart is attached [Flowchart 1].
Flowchart 1.
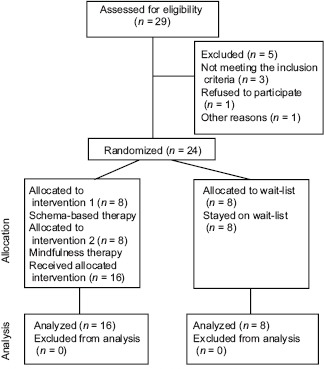
The sample template for the consort diagram showing the flow of participants through each stage of a randomized trial
Patients
The design of this study was semi-experimental with the post- and pre-tests. The statistical populations were all the patients with psoriasis (n = 24, 11 males, 13 females, age range 20–50 years), who referred to the Isfahan Al-Zahra Hospital in Iran, Dermatology Clinic, from February to September 2014. Twenty-four patients with the low general health and pathological criteria were chosen using the available sampling method. The patients were diagnosed with psoriasis symptoms through a clinical interview and the dermatologist's diagnosis. Subsequently, the patients were divided into three groups of the schema-based therapy (n = 8), mindfulness therapy (n = 8) and control (n = 8). The inclusion criteria were as follows: Patients with psoriasis according to the dermatologist diagnosis, not being detected with the psychotic disorders, based on the clinical interview and criteria of the diagnostic and statistical manual of mental disorders (DSM), having mental disorders, based on the general health questionnaire (GHQ), not taking the psychiatric medicines. The exclusion criteria were also as follows: Patients with physical diseases, being stressed after an accident during the current month, and consumption of alcohol and narcotics.
Instrumentation
General health questionnaire
Goldberg GHQ contained 28 questions and evaluated four minor scales of corporal signs, anxiety, social function, and depression symptoms which assessed the person's general health during the last month. In this questionnaire, Likert scoring method was employed which was in the form of. A Likert scale is a psychometric scale usually involved in research that uses questionnaires. It is the most extensively used approach to scaling responses in survey research, such that the term is often employed interchangeably with rating scale, or more accurately the Likert-type scale, even though the two are not synonymous. The highest testing score in this method was 84. A lower score in this questionnaire indicated a higher level of general health. The score of 23 was the cutting score that was if the examinee's score equals 23 or more, it would be screened as suspected. In the Goldberg and Wiliams questionnaire, the final coefficient for having the whole questionnaire is reported to be 0.95. The Williams questionnaire, components of the longer patient health questionnaire, offers psychologists concise, self-administered tools for assessing depression. It incorporates the DSM-IV depression criteria with other leading significant depressive symptoms into brief self-report instruments that are usually employed for screening and diagnosis, as well as selecting and monitoring treatment.
Young schema questionnaire
Young schema questionnaire-short form with 75 articles evaluates 15 initial maladaptive schemas. Each question was marked, based on a 6° scale. If the average of each minor scale surpassed 25, that schema was inefficient. Stability of this scale for the whole test is reported to be 0.96 and above 0.80 for all minor scales. The stability of this questionnaire for the Iranian society is 0.94.[21]
General framework of the mindfulness therapy
General framework of mindfulness therapy was as follows: The program consisted of eight 90 min sessions and a briefing session was intended before the beginning of the program. Overall emphasis of the program was on learning to direct attention towards the inner experience and seeing what happens during this process and then on the application of those things that have been achieved through performing mindfulness practices in dealing with real-life challenges. The general trend was that each session began with the completion of an emotion scale and doing a breathing exercise. After that, a brief overview of the previous session was articulated, and agenda of the current meeting was expressed. Next, the assignments of the previous session were reviewed and then mindfulness exercises and activities related to each session were done. The session continued with breathing exercise and refilling the emotion scale. Finally, the session ended with the distribution of compendium of tips and learning materials that had been prepared in sessions and a review of the assignments. Application of MBCT intervention programs is among the most important programs in the year of 1992 by Teasdale.
The formulating mindfulness training sessions
Session one – Getting to know members of the group and their expectations, making a group policy, (explaining about psoriasis), practice of eating raisins, and body checking practice,
Session two – Body checking practice, 10 min of mindful breathing, practice of thoughts and feelings (learning that emotions are resulted from the position and its interpretation),
Session three – Seated meditation with focus on awareness of breathing and body, investigating pleasant events of the week and body feelings, thoughts, emotions and temper associated with the pleasant event,
Session four – 5 min of mindful seeing or hearing, seated meditation with focus on breathing, body, sounds, thoughts and nonelection based awareness, 3 min breathing space (the use of this method in difficult situations), examining unpleasant experiences and physical sensations, thoughts, feelings and temper related those experiences,
Session five – Seated meditation with awareness of breathing and body, practice of discovering habitual patterns of reaction, and the use of mindfulness skills to facilitate greater responding to the present time,
Session six – Seated meditation with awareness of breathing and body, 3 min breathing space, practice of temper, thought, and alternative perspectives with emphasis on this fact that thoughts are not facts, preparation for the end of the period,
Session seven – Seated meditation with awareness of breathing, body, sounds, thoughts and emotions, 3 min breathing space, investigation of the relationship between activity and temper,
Session eight – Body checking practice, discussion on the continuation of exercises, and problems that prevent duties to be carried out.[22]
Treatment outline of the schema therapy group
The treatment plan of the second experimental group (schema therapy) treats a patient in form of 8 weekly sessions, in which in each session, patients receive schema therapy individually for 90 min. In the first session, some explanations about the treatment method and how it works were given to the patient, and the patient was clinically interviewed according to the criteria of DSM. After the interview, Young's schema therapy test was given to the patient. In the case of diagnosis, the patient was asked to participate in seven individual sessions if he/she wishes to continue the treatment. In later sessions, with presenting assignments and homework review, the patient was asked to express any disadvantages and his/her views during the treatment. He/she was talked to about the recurrence of the problem and some guidance was given to him/her. Young's schema therapy questionnaire was given as the post-test and the test result was announced to the patient. At the end of the session, the patient was thanked, and the end of the meeting was announced. In this study, sessions were implemented, based on the schema therapy method, which was designed and developed by Young et al. (2001). The outline of the therapy session is given in the detailed stages of the schema therapy in appendix two.[23]
The formulating schema therapy sessions
Session one – Explaining the schema model to the patient in the plain and clear language and how schemas and coping styles are formed, completing the questionnaire, assessing the patient's problems,
Session two – Hypothesis making about schemas and identifying and naming them, identifying patient's coping styles and mood and temper and mental imagery in the evaluation phase,
Session three – Conceptualizing the patient's problem according to the schema approach and collecting all the information obtained during the evaluation stage, investigating objective evidence approving or rejecting schemas on the basis of evidence of the past and current life of the patient,
Session four – Assigning the evidence confirming the schemas to childhood experiences and dysfunctional parenting styles, the interaction between the schema aspect and the healthy aspect and learning responses of the healthy aspect by the patient,
Session five – Developing the schema educational cards when facing with the schema provoking situation, writing the schema registration form during everyday life and provoking time of schemas,
Session six – Providing a rationale for using experimental techniques and the implementation of an imaginary dialog, strengthening the concept of a “healthy adult” in the patient's mind and identifying unfulfilled emotional needs and fighting against schemas,
Session seven – Creating an opportunity for the patient to identify his feelings about his parents and these unmet needs by them, helping the patient to send out his blocked emotions by traumatic events and providing support for the patient, finding new ways to communicate and stopping avoidance and excessive compensation coping styles,
Session eight – Providing a comprehensive list of problematic behaviors and determining change priorities and identifying therapeutic targets, mental imaging of problematic situations, and dealing with the most problematic behavior, practicing healthy behaviors through role-playing, reviewing the benefits and disadvantages of unhealthy and healthy behaviors, and overcoming behavior change obstacles.[23]
Treatment sessions were held by a clinical psychologist licensed for the schema and mindfulness therapies. Of course, these sessions were under the surveillance of the psychology organization consisting of a supervisor and dermatologist, who controlled the intervening variables regularly.
Statistical analysis
Statistical analysis was done through the Statistical package for social science (SPSS-20) software and in order to analyze data, descriptive and inferential statistics were employed for data analysis. Co-variance analysis test was used to evaluate the hypothesis. The control variables were pretest scores in measuring instruments and demographic variables. The independent variables were group membership in two-intervention presentation of the three levels (mindfulness and schema therapy) and not presenting intervention. The dependent variables were the Young's posttest scores and the psoriasis patients’ general public health.
One of the assumptions of the parametric tests application is the assumption of normality of the scores distribution of the sample group or groups in the community. The default assumption is that the distribution of scores is in the normal range in the community using the Kolmogorov–Smirnov-Z-statistic test. This test showed that the P value was >0.05, and accordingly, there was insignificant difference between the normal distribution and variable distribution. Thus, the distribution of variable was normal. At first, the presumption of normality of scores’ distribution was assessed through the Kolmogorov–Smirnov test. The statistics Levene's test is an inferential statistic used to evaluate the equality of variances for a variable, calculated for two or more groups. Therefore, the right statistical path (parametric or nonparametric, which determines the test type using the Kolmogorov–Smirnov-Z test) would be revealed. The latter test also does the same. The P ≤ 0.05 were considered significant. The two groups’ variances were equal and they were insignificant.
Ethical consideration
This study was carried out in accordance with the ethical guidelines of the 1975 declaration of Helsinki as reflected in a prior approval by the Institution's Human Research Committee. Accordingly, a moral code of 493032 was obtained from the Ethical Committee of the Isfahan University of Medical Sciences. The participants were safe from any probable physical and mental hazards. Furthermore, the participants gave written informed consent forms after explaining the purposes and protocol of the study.
Results
The demographic characteristic of the groups regarding the mean age ± standard deviation (SD) for the patients with psoriasis under the schema and mindfulness-based therapies was 37.25 ± 3.06 and 35.75 ± 3.26, respectively. Furthermore, for the patients, who were not under no intervention (controls), the mean ± SD of 31.25 ± 3.5 was obtained [Table 1]. To control the scores of pretest and the presumed demographic variables, applying covariance analysis was considered. Tables 2 and 3 show the results of the covariance analysis of the pretest scores on the mental health and incompetence schema among the psoriasis patients (P ≤ 0.05). The findings revealed significant difference between the schema-based therapy and mindfulness with the control group consisting of the defeated schema, dependence/incompetence schema, devotion schema; stubbornly criteria schema, merit schema, restraint/inadequate self-discipline schema and general health the control group revealed significant difference (P ≤ 0.05), but for the defect/schema, the difference between the three groups were insignificant [Table 2].
Table 1.
Demographic characteristics of the groups
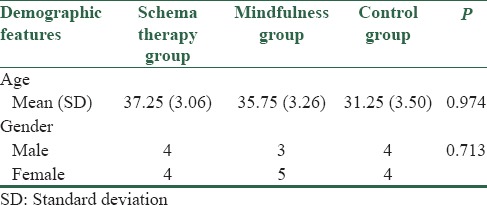
Table 2.
Comparison of the maladaptive schemas between the groups
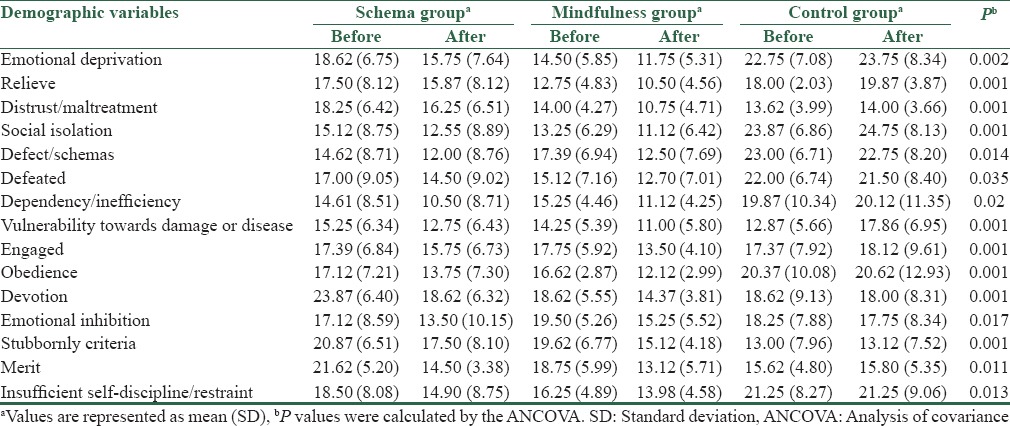
Table 3.
Comparison of the general public health between the groups
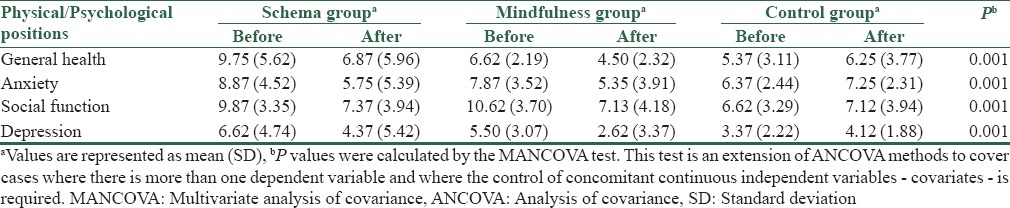
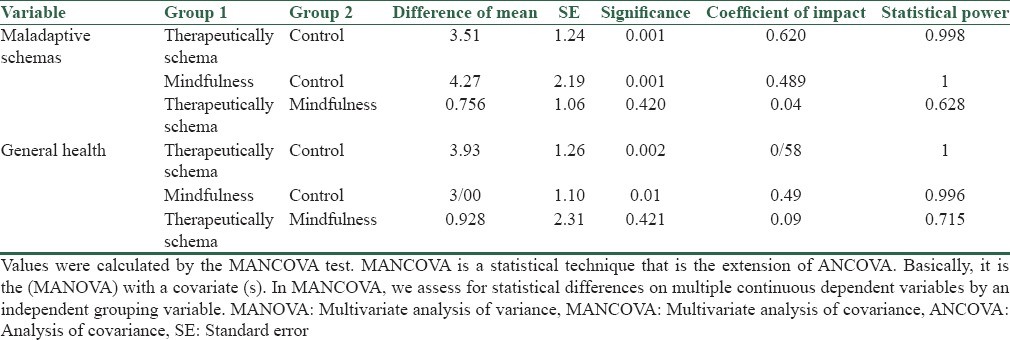
The results of the paired comparison of the multivariate analysis of covariance demonstrated that there was no difference between the maladaptive schemas and the general health of the schema therapy group and the mindfulness therapy group. However, the difference of the scores between the schema therapy group and the control group was significant. In addition, the difference of the scores between the mindfulness therapy group and the control group was significant [Table 4, P ≤ 0.05].
Table 4.
The data of multivariate covariance analysis the effect of membership group on the scores rates of the maladaptive schemas among three groups
Discussion
This study aimed to study the effects of the schema and mindfulness therapies regarding the maladaptive schemas hold by the psoriasis patients, who had the pathophysiological symptoms. Naturally, by controlling the influence of the pretest, there was a difference among the three groups (schema therapy, mindfulness, and control groups). Findings imply that there was insignificant difference between two treatments of the schema and mindfulness therapies and effectiveness of both was evident on improving the psoriasis patients’ cognitive schema.
In addition, the schema-based therapy and mindfulness affected the patients’ maladaptive schemas other than defect schema and general health. To the best of our own knowledge, there is no corresponding study to the schema therapy group. Although, the findings of this study in some variables are consistent with the findings of Kameli et al. (2011), Bardack et al. (2014) Lisa et al., (2013) and Khorshid Zadeh et al. (2011), who found mindfulness focused on the cognitive therapy, had an impact in reducing stress, pain and fear and increased positive emotions and improved early maladaptive schemas.[24,13,25,19]
Psoriasis patients have schema behavior problems which are formed in childhood.[4] These highly inefficient schemas remain stable in life and cause bias in interpretation of events and show themselves as misunderstandings, distorted attitudes, wrong assumptions, unrealistic goals, and expectations and affect future understanding and evaluation of life. For describing persons with maladaptive schema, we should say that they think that people always mistreat them and others may abandon and ashamed them anytime, and they seek to take advantage of them. They have also maladaptive schemas/disfavor defect so that they think that they are incomplete, undesirable, bad, despised and worthless persons, or others consider them as hated and undesirable persons. People with this schema are too sensitive to the other people's criticism, rejection, blame, and improper comparisons.[26]
People with the maladaptive schema of emotional deprivation and social isolation think that desires and needs of emotional support from others will not be satisfied sufficiently, the possibility of undesirable interpersonal relationships are very high and should withdraw from relationships. Because they are different with others and not belonging to a particular person, thus they exclude themselves from family. They believe that they are unable to continue living or being happy without the support of others.[27]
Due to radical inhibition of actions, emotions and spontaneous communications in order to avoid rejection from others, they have an inhibition in anger, expression of positive momentum and vulnerability as well as having a sense of shame. These people have an excessive emphasis on rationality and ignoring the emotions and feelings. They have a maladaptive schema of obedience so that they feel forced towards excessive transferring of their control to another person that this often occurs for avoiding anger, withdrawal, or revenge and these behaviors lead to a kind of withdrawal in patients and make them be rejected by another party.[28]
In general, in patients with maladaptive schema failure in progress, entitlement/grandiosity, inadequate self-control and self-discipline, self-sacrifice, seeking confirmation/drawing attention, unrelenting standards, self-punishment, the possibility of disintegration and dissatisfaction of health will increase.[29] Patients with skin diseases because of faulty thinking pattern always may enter a new period of mental health problems such as anxiety, depression, and physical symptoms.[4]
Mindfulness is training people to get rid of cognitive processing that makes them vulnerable to periods of depression. Mindfulness tries to change consciousness and create a new relationship with thoughts instead of changing them to reduce rumination; this ability takes place by breeding two important skills of adoption of internal experiences (thoughts-emotions and unpleasant physical senses and not avoiding these experience). Mindfulness teaches patients to get out of the habitual skills of mind and prepare the conditions for change by directing information processing resources toward the goals of attention such as breathing or feeling the moment.[27]
Patients with psoriasis commonly experience thoughts related to incomplete schemas, mindfulness encourages patients to increase acceptance for dealing with emotional pain and distress to pay attention to their experiences in a manner devoid of judgment and in the present time and thereby reducing the level of psychological discomfort. This awareness could lead to an improvement in the emotional processing and the manner of dealing with chronic diseases.[28]
In addition, a conscious mind targets useless processes such as rumination, worry and weak emotional regulation and promotes positive emotions. Reusing of attention in this way prevents increasing or survival of faulty thoughts and makes faulty processing cycles to be less available. People learn to see their thoughts and feelings without judgment and look at them as simple mental events that come and go instead of seeing them as their own part or reflection of the fact[28] This approach reduces the level of body and muscle tensions and by being aware of their body feelings, the patients increase their awareness of physical changes that this leads to a reduction in their reported physical symptoms in the long-term and distracting of attention and awareness toward thoughts, emotions, and desires.[12]
In general, we can say that increasing attention and awareness compared to thoughts, emotions, and desires in mindfulness causes internal consistency and adaptive behaviors lead to positive psychological states in people and even cause improving the individual ability towards personal and social activities and creating interest in these activities.[29]
Patients with psoriasis have mental schemas that underestimate their ability to cope, seeing active outer thoughts and emotions and trying to avoid or escape from them can be an example of facing that cause to shutdown the fear responses and avoidance behavior. In the approach of the schema therapy, disturbed schemas will be improved, and the rate of activation and accompanying emotional intensity will be reduced.[11] Improvement of the schemas will be followed by a series of behavioral changes so that patients respond to the schema's provocative incentives in healthier ways, and their attitude becomes more positive about themselves and their environment.[29]
Through the cognitive strategy in the schemas, patients create a healthy voice in their minds and empower their healthy mindset and plan a rational position against schema. These strategies help patients to distance from the schemas and evaluate their correctness, also by inciting emotions associated with early maladaptive schemas as well as reprinting; patients will be helped for improving relative satisfying of childhood excitement and unmet needs.[26]
The limitations of this study were the low sample size as well as focusing study to Isfahan city population in Iran. Nevertheless, the strength point is that in addition to the schema and mindfulness therapeutic interventions that affect emotions and cognition, other treatments such as behavioral therapy should be taken into account.
In conclusion, this study showed similar effects of both schema and mindfulness therapies on the maladaptive schemas in improving the psoriasis patients’ psychological symptoms. We also suggest that due to the roles of geographical and genetic predisposition factors in psoriasis prevalence, the roles of biological and psychological variables should be also examined. Subsequently, the study can be run in the other cities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gupta MA, Gupta AK. Quality of life of psoriasis patients. J Eur Acad Dermatol Venereol. 2000;14:241–2. doi: 10.1046/j.1468-3083.2000.00134.x. [DOI] [PubMed] [Google Scholar]
- 2.Henseler T. The genetics of psoriasis. J Am Acad Dermatol. 1997;37(2 Pt 3):S1–11. [PubMed] [Google Scholar]
- 3.Zaragoza V, Pérez A, Sánchez JL, Oliver V, Martínez L, Alegre V. Long-term safety and efficacy of etanercept in the treatment of psoriasis. Actas Dermosifiliogr. 2010;101:47–53. [PubMed] [Google Scholar]
- 4.Darjani A, Mohtasham-Amiri Z, Mohammad Amini K, Golchai J, Sadre-Eshkevari S, Alizade N. Skin disorders among elder patients in a referral center in Northern Iran (2011) Dermatol Res Pract 2013. 2013:193205. doi: 10.1155/2013/193205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurd SK, Troxel AB, Crits-Christoph P, Gelfand JM. The risk of depression, anxiety, and suicidality in patients with psoriasis: A population-based cohort study. Arch Dermatol. 2010;146:891–5. doi: 10.1001/archdermatol.2010.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rush AJ. At the research front: Cognitive therapy for depression. Aust N Z J Psychiatry. 1979;13:13–6. doi: 10.3109/00048677909159104. [DOI] [PubMed] [Google Scholar]
- 7.Young JE. Cognitive Therapy for Personality Disorders: A Schema-focused Approach (Rev ed) Practitioner’ Resource Series) (3rd Edition) 1999:Professional Resource Exchange in. [Google Scholar]
- 8.Turner HM, Rose KS, Cooper MJ. Parental bonding and eating disorder symptoms in adolescents: The meditating role of core beliefs. Eat Behav. 2005;6:113–8. doi: 10.1016/j.eatbeh.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Lindeman S. Personality disorders can be treated by a schema focused approach. Duodecim. 2004;120:2889–96. [PubMed] [Google Scholar]
- 10.Hawke LD, Provencher MD, Parikh SV. Schema therapy for bipolar disorder: A conceptual model and future directions. J Affect Disord. 2013;148:118–22. doi: 10.1016/j.jad.2012.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Teasdale JD, Segal Z, Williams JM. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behav Res Ther. 1995;33:25–39. doi: 10.1016/0005-7967(94)e0011-7. [DOI] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J, Hanh TN. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. by unified Buddhist. 2013 [Google Scholar]
- 13.Bardacke N, Duncan LG. Mindfulness-based childbirth and parenting: Cultivating inner resources for the transition to parenthood and beyond. Mindfulness-Based Treatment Approaches: Clinician's Guide to Evidence Base and Applications. London: Academic Press; 2014. p. 213. [Google Scholar]
- 14.Nanda A, Al-Fouzan AS, El-Kashlan M, Al-Sweih N, Al-Muzairai I. Salient features and HLA markers of childhood psoriasis in Kuwait. Clin Exp Dermatol. 2000:147–51. doi: 10.1046/j.1365-2230.2000.00598.x. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y, Yang X, Wang L, Zhang X. A randomized controlled trial of the effects of brief mindfulness meditation on anxiety symptoms and systolic blood pressure in Chinese nursing students. Nurse Educ Today. 2013;33:1166–72. doi: 10.1016/j.nedt.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Davoudi I, Nasimi N. The efficacy of mindfulness-based stress reduction on pain relief and the approach to encounter with devastating factors in women with chronic pains of muscular skeletal. New findings in Psychology. 2012;7:45–62. [Google Scholar]
- 17.Moghtadaei K. The efficacy of mindfulness based cognitive therapy group training on the physical symptoms of women with irritable bowel syndrome. J Behavioral Sci Res. 2012;10:698–708. [Google Scholar]
- 18.Bagheri H, Mirzaeayan B, MohammadGhani P, Omrani S. The efficacy of mindfulness-based cognitive therapy (MBCT) on the reduction of depression in patients with multiple sclerosis (MS) Thought and Behavior. 2012;6:75–82. [Google Scholar]
- 19.Khorshidzadeh MB, A. Sohrabei F. The effectiveness of schemetherapy on the reduction of early maladaptive schemes in women with social anxiety disorder. Culturecounseling and Psych J. 2011;2:1–34. [Google Scholar]
- 20.Fordham B, Griffiths CE, Bundy C. A pilot study examining mindfulness-based cognitive therapy in psoriasis. Psychol Health Med. 2015;20:121–7. doi: 10.1080/13548506.2014.902483. [DOI] [PubMed] [Google Scholar]
- 21.Oei TP, Baranoff J. Young schema questionnaire: Review of psychometric and measurement issues. Aust J Psychol. 2007;59:78–86. [Google Scholar]
- 22.Segal Z, Williams J, Teasdale J. Mindfulness-based Cognitive Therapy for Depression: A New Approach to Relapse Prevention. New York: Guilford; 2002. [Google Scholar]
- 23.Young JE, Weinberger AD, Beck AT. Cognitive therapy for depression. Clinical Handbook of Psychological Disorders: A Step-by-step Treatment Manual. Vol. 3 Guilford. 2014:264–308. [Google Scholar]
- 24.Kameli ZG, B. Aghamohamadian H. The effectiveness of Scheme -Focused Therapy On the adjustment of the basic incompatible scheme ongirls of irresponsible and un supervised. Clinical Psychology Research and Consulting J. 2011;1:83–98. [Google Scholar]
- 25.Lisa D, Hawke MDP, Sagar V. Schema therapy for bipolar disorder: A conceptual model and future directions. Journal of Affective Disorders. 2013;148:118–22. doi: 10.1016/j.jad.2012.10.034. [DOI] [PubMed] [Google Scholar]
- 26.Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin Psychol. 2013;10:125–43. [Google Scholar]
- 27.Thimm JC. Personality and early maladaptive schemas: A five-factor model perspective. J Behav Ther Exp Psychiatry. 2010;41:373–80. doi: 10.1016/j.jbtep.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 28.Van Vlierberghe L, Braet C, Bosmans G, Rosseel Y, Bögels S. Maladaptive schemas and psychopathology in adolescence: On the utility of Young's schema theory in youth. Cognit Ther Res. 2010;34:316–32. [Google Scholar]
- 29.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]


