Abstract
A 71-year-old man, with history of plasmacytoma in relapse since one year, was hospitalized for a initial presentation of acute pancreatitis and hepatitis. Although there was a heterogeneous infiltration around the pancreas head, the diagnosis of an extramedullary localization of his plasmacytoma was not made until later. This delayed diagnosis was due to the lack of specific radiologic features and the lack of dilatation of biliary ducts at the admission. A diagnosis was made with a simple ultrasound guided paracentesis of the low abundance ascites after a transjugular hepatic biopsy, an endoscopic ultrasound-guided fine needle aspiration of the pancreatic mass, and a failed attempt of biliary drainage through endoscopic retrograde cholangiopancreatography. In order to document the difficulty of this diagnosis, characteristics of 63 patients suffering from this condition and diagnosis were identified and discussed through a systematic literature search.
Keywords: Plasmacytoma, Pancreas, Diagnosis, Ultrasound endoscopy, Review
Core tip: We wrote an interesting case report about a pancreatic plasmacytoma for which diagnosis, including endoscopic diagnosis, was a challenge. In a second part, a systematic pubmed search was performed from 1950 to June 2016, reporting characteristics and route to diagnosis of 63 similar cases reports! Strengths of our paper are the original route to diagnosis (by a simple ultrasound guided paracentesis, after failed of the endoscopic route) and our literature search which is particularly exhaustive: we are first to identify more 20 case similar reports (63!!) and their characteristics.
INTRODUCTION
Here we describe the case of a pancreatic plasmacytoma and difficulties to establish the diagnosis. Characteristics of patients and routes to diagnosis in this condition will be identified through a systematic literature search, in a second part.
CASE REPORT
A 71-year-old man was hospitalized for a clinical and biological presentation of acute pancreatitis. Pain occurred suddenly and was associated with an increased level of lipase above 2000 UI/L, a cholestatic icterus (bilirubin: 103 µmol/L) and a hepatic cytolysis (ALT: 154 UI/L; AST: 131 UI/L). An initial computerized tomography (CT) scan showed a significant but unspecific infiltration around the pancreas head, without dilatation of biliary ducts. A first endoscopic ultrasound (EUS) (Pentax, EG 3670 URK, France) showed similar data. The hypoechoic infiltration of the pancreas head was heterogeneous and extended to the hepatic hilum, in contact with portal vein. There was no biliary lithiasis, nor context of alcohol consumption during the last days before the admission. However, the patient was treated with Lenalidomide plus dexamethasone for a Immunoglobulin A (IgA) plasmacytoma diagnosed 3 years ago [t(4;14) positive, del(17p) negative; at baseline: LDH: 173 UI/L, monoclonal immunoglobulin peak: 40.5 g/L, Kappa and Lambda serum free light chain: 11.7 and 18.6 mg/L, respectively], without hypercalcemia nor kidney failure. He relapsed dramatically one year ago, with an extramedullar localization (L4 lumbar spine). Based on hematotoxicity (platelets: 41000 G/mm3) and lake of specific radiologic features, the initial diagnosis suspected was a dual hepatic and pancreatic toxicity of Lenalidomide. Indeed, acute pancreatitis and hepatitis had been occasionally reported as a side effect of Lenalidomide[1,2]. Common hepatitis viral serologies were tested before carrying out a transjugular hepatic biopsy which showed a histological aspect compatible with the diagnosis of drug hepatitis or hepatitis related to a biliary obstruction (centrilobular and portal infiltrate of polymorphs inflammatory cells including eosinophils). Although an empirical treatment with 500 mg intravenous methylprednisolone daily was started, bilirubin level increased at 345.8 μmol/L within the following ten days. Hence, a new CT-scan was performed and showed the occurrence of a mild to moderate dilatation of biliary ducts and a low abundance ascites. At the moment of admission, the infiltration of the pancreas head significantly resembled a tumor (Figure 1) and the diagnosis of a pancreatic localization of the plasmacytoma was suspected. After platelets support, EUS (Pentax, EG 3670UTK, France) guided fine needle aspiration (FNA) was carried out with a 22-gauge needle. Tumor infiltration appeared to be growing due to portal vein invasion. Linear EUS passage through the pylorus was drastically limited, so that FNA was performed from the gastric antrum. Then, an endoscopic retrograde cholangiopancreatography was attempted to place a biliary stent for palliative treatment, but the cannulation of the bile duct had failed due to a major parietal oedema of the duodenum which was easily bleeding due to the contact of the sphincterotome. A percutaneous biliary drainage was considered, but an ultrasound-guided paracentesis was preferred, taking into account technical difficulties of the biliary drainage. Cytology of the FNA was not contributory (epithelial cells of pancreas without malignity signs) while the analysis of ascites showed plasmacytosis with severe atypia enabling the diagnosis of pancreatic plasmacytoma (Figure 2). Bone marrow was exempted from dystrophic plasma cells, proving an extramedullar relapse. The increase of the monoclonal spike (from 2.3 g/L to 8.1 g/L within 4 mo) and LDH (259 UI/L) was compatible with this diagnosis. Kappa and Lambda free light chain, at this time of the disease, were 0.4 mg/L and 24.8 mg/L, respectively, without hypercalcemia, Bence Jones proteinuria, nor kidney failure. Hence, after contacting the referral hematologist of the patient, a cure of 40 mg dexamethasone daily was started inciting a drastic decrease of bilirubin level within the next three days (183.1 μmol/L). Then, a second line of chemotherapy (Bortezomib + Cyclophosphamide) was started with a good short-term safety. Although a biological response, especially for monoclonal peak (2.1 g/L), at one month, the patient died 4 mo after the diagnosis of pancreatic plasmacytoma.
Figure 1.
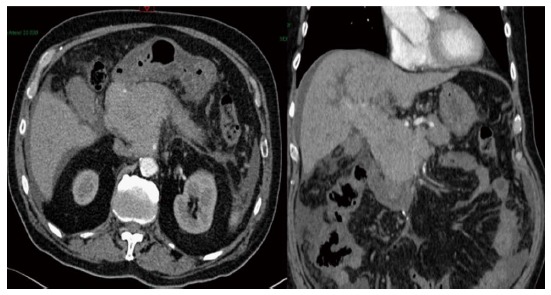
Abdominal computerized tomography scan showing a head pancreas mass extended to the hepatic hilum with mild to moderate dilatation of biliary ducts and a low abundance ascites.
Figure 2.
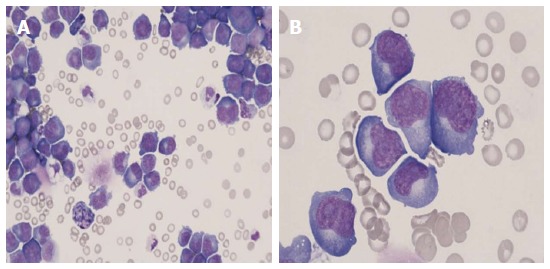
Peritoneal fluid Cytology, May-Grünwald-Giemsa stain. A: An almost pure population of myeloma cells (× 40); B: Malignant plasma cells exhibiting severe atypia (× 100).
DISCUSSION
Extramedullary plasmacytoma involvement is not an uncommon presentation, occurring in 10 %-15 % of patients[3]. They are commonly identified after the diagnosis of multiple myeloma. The most commonly involved organs are those located around skeletal lesions, and less frequently, skin, liver, kidney, or central nervous system. Regarding the digestive system, liver and spleen are classically the organs which could be damaged by disease through deposits of amyloid proteins[4]. Extramedullary plasmacytomas involving the pancreas is a very rare condition with a prevalence rate estimated at 2.3%, based on autopsy studies[5].
After conducting a systematic Pubmed search, we identified 63 case reports of pancreatic plasmacytoma and collected a set of clinical and diagnostic data which were reported in Table 1. About half of them were male, with a median age of 58.5 years old, and presented jaundice in 70.0% with (36%) or without pain. About 2/3 of patients (68.4%) had a known history of plasmacytoma since 1 year (0-13) (median, interquartile ranges 25%-75%), before the involvement of the pancreas head. Only two cases involved the body or the tail of the pancreas[6,7]. Only 1/3 of patients (32.6%) were diagnosed by EUS-guided FNA vs 1/5 (20.9%) by CT-guided percutaneous FNA. About ¼ of patients (25.6%) have needed for a surgical biopsy, including situation involving bowel obstruction. A direct biopsy of the mass was possible in 16.3% during an upper gastrointestinal endoscopy. Most of patients were treated with chemotherapy (56.0%) and/or radiotherapy (52.0%), providing a 100% tumor response rate. A biliary stent was placed in half of patients with jaundice (46.7%).
Table 1.
Main characteristics of the 63 patients who had been reported to date with a pancreas plasmacytoma: Results of a PubMed search from 1950 to June 2016
| Demographic characteristics | n (%) |
| Male | 22 (56.4) |
| Age (years, median, IQR) | 58.5 [51.2-82] |
| Symptom(s) at diagnosis | |
| Jaundice | 35 (70.0) |
| Pain | 18 (36.0) |
| Myeloma | |
| Known history of myeloma | 26 (41.3) |
| Disease duration at diagnosis of pancreas plasmacytoma (years, median, IQR) | 1 [0-13] |
| Type Kappa | 13 (71.4) |
| Immunoglobulin | A (36%), G (52%), M (12%) |
| Diagnosis process of the pancreas plasmacytoma | |
| Endoscopic ultrasound FNA | 14 (32.6) |
| Percutaneous FNA | 9 (20.9) |
| Endoscopic biopsy | 7 (16.3) |
| Surgical biopsy | 11 (25.6) |
| Paracentesis | 0 (0.0) |
| Postmortem biopsy | 3 (7.0) |
| Management of the pancreas plasmacytoma | |
| Chemotherapy | 14 (56.0) |
| Radiotherapy | 13 (52.0) |
| Biliary stent in patients with jaundice | 10 (40.0) |
| Surgery | 8 (32.0) |
| Biliodigestive derivation | 3 (37.5) |
| Duodenopancreatectomy cephalic | 2 (25.0) |
FNA: Fine needle aspiration; IQR: Interquartile range.
Hence, to the best our knowledge, this is the first case report of a pancreatic plasmacytoma which was diagnosed by ascites analysis. Diagnosis by noninvasive procedures and rapid response to conservative therapy were important in this patient’s care. It is very difficult to radiologically differentiate extramedullary plasmacytoma of the pancreas from other pancreatic tumors. EUS guided FNA provides the easiest and most safe route to diagnosis of pancreatic plasmacytoma. Studies have shown that the overall accuracy of EUS-guided FNA ranges between 71% and 90% in case of pancreatic tumor[8]. However, there is no corresponding data in case of pancreatic plasmacytoma.
In our case, the missed diagnosis of pancreas plasmacytoma through EUS-guided FNA may be due to a sampling bias. Furthermore, we made only one diagnostic EUS attempt while in few cases reported, authors specified the need for repeating EUS-guided FNA[9-13].
This case highlights that a pancreatic mass in patients with plasmacytoma should be systematically considered as an extramedullary extension of the disease until proven otherwise. Ascites analysis could be a simple route to diagnosis, even in low abundance. Finally, in case of jaundice, excluding angiocholitis, potential risks of biliary stenting should be taken into account, regarding safety and the drastic efficacy of radiotherapy or medical treatment (dexamethasone and chemotherapy).
COMMENTS
Case characteristics
A 71-year-old man with history of plasmacytoma in relapse since one year, and treated with Lenalidomide.
Clinical diagnosis
The initial diagnosis suspected was a dual hepatic and pancreatic toxicity of Lenalidomide.
Differential diagnosis
An adenocarcinoma of the pancreas, or other less frequent pancreatic tumor such as a non Hodgkin’s lymphoma, or endocrine tumor.
Laboratory diagnosis
An increased level of lipase above 2000 UI/L, a cholestatic icterus and a hepatic cytolysis.
Imaging diagnosis
Computerized tomography showed a significant but unspecific infiltration around the pancreas head, without dilatation of biliary ducts, extended to the hepatic hilum, and evolving as a pseudotumor within few days.
Cytological diagnosis
A (pancreatic) plasmacytoma.
Treatment
An empirical corticotherapy followed by a second line of chemotherapy (Bortezomib + Cyclophosphamide).
Related reports
Cytology of the mass was not contributory in contrast with the very low abundance ascites located around the liver.
Terms explanation
Extramedullary plasmacytoma involvement is not an uncommon presentation, and occurres preferentially in located around skeletal lesions, or less frequently in, skin, liver, kidney, or central nervous system.
Experiences and lessons
A pancreatic mass occurring in a patient with history of plasmacytoma and with an uncommon presentation should make suspecting an extramedullar site of the disease. No diagnostic way should be forgot, even a simple analysis of an ascites sample.
Peer-review
This is an interesting case about pancreas involvement in a case with relapsed myeloma.
Footnotes
Institutional review board statement: This case report was exempt from the internal Review Board standards of the Hepato-gastroenterology department managed by Pr Jean-Marc Phelip, at University of Saint-Etienne in Saint-Priest en Jarez.
Informed consent statement: The patient who is involved in the present case report gave his verbal informed consent before his death, authorizing use and disclosure of his protected health information.
Conflict-of-interest statement: None.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country of origin: France
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: October 11, 2016
First decision: November 30, 2016
Article in press: December 28, 2016
P- Reviewer: Bramhall S, Kyrtsonis MC, Mezalek ZT, Paydas S S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Nojkov B, Signori C, Konda A, Fontana RJ. Lenalidomide-associated hepatotoxicity--a case report and literature review. Anticancer Res. 2012;32:4117–4119. [PubMed] [Google Scholar]
- 2.FDA. Revlimid: highlights of prescribing informations (Federal Drugs Administration 2012) Available from: http: //www.accessdata.fda.gov/drugsatfda_docs/label/2012/021880s028lbl.pdf.
- 3.Pinto-Marques P, Martins C, Mendonça E, Castro H, Serra D. Pancreatic head mass of unusual etiology: multiple myeloma diagnosed by endoscopic ultrasound-guided fine needle aspiration. Endoscopy. 2010;42 Suppl 2:E263–E264. doi: 10.1055/s-0030-1255659. [DOI] [PubMed] [Google Scholar]
- 4.Michopoulos S, Petraki K, Petraki C, Dimopoulos MA. Light chain deposition disease of the liver without renal involvement in a patient with multiple myeloma related to liver failure and rapid fatal outcome. Dig Dis Sci. 2002;47:730–734. doi: 10.1023/a:1014773512707. [DOI] [PubMed] [Google Scholar]
- 5.Fischer A, Suhrland MJ, Vogl SE. Myeloma of the head of the pancreas. A case report. Cancer. 1991;67:681–683. doi: 10.1002/1097-0142(19910201)67:3<681::aid-cncr2820670325>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 6.Hirata S, Yamaguchi K, Bandai S, Izumo A, Chijiiwa K, Tanaka M. Secondary extramedullary plasmacytoma involving the pancreas. J Hepatobiliary Pancreat Surg. 2002;9:111–115. doi: 10.1007/s005340200012. [DOI] [PubMed] [Google Scholar]
- 7.Deguchi Y, Nonaka A, Takeuchi E, Funaki N, Kono Y, Mizuta K. Primary pancreatic plasmacytoma. Am J Clin Oncol. 2004;27:247–249. doi: 10.1097/01.coc.0000092613.05046.28. [DOI] [PubMed] [Google Scholar]
- 8.Harris MD, Buscaglia JM. How to do pancreatic mass FNA. Gastrointest Endosc. 2010;71:825–826. doi: 10.1016/j.gie.2010.01.068. [DOI] [PubMed] [Google Scholar]
- 9.Hue SS, Azhar R. Plasmacytoma of the pancreas: an unusual manifestation of multiple myeloma. Singapore Med J. 2013;54:e105–e107. doi: 10.11622/smedj.2013066. [DOI] [PubMed] [Google Scholar]
- 10.Gupta P, Rice GD, Abraham K, Ghole V, Ketkar M. Extramedullary plasmacytoma of the pancreas and jejunum. Clin Imaging. 2009;33:240–243. doi: 10.1016/j.clinimag.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Jaubert D, Hauteville D, Verdier M, Houdelette P, Gisserot D, Dupin-Nizard B, Sahel J. Plasmacytoma of the head of the pancreas: a rare cause of cholestatic jaundice. Gastroenterol Clin Biol. 1985;9:532–534. [PubMed] [Google Scholar]
- 12.Scheiman J, Elta G, Francis I. Biliary obstruction secondary to an extramedullary plasmacytoma of the pancreas: confusion with pancreatitis on computed tomography. Pancreas. 1987;2:237–239. doi: 10.1097/00006676-198703000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Sánchez Acevedo Z, Pomares Rey B, Alpera Tenza MR, Andrada Becerra E. Primary pancreatic plasmacytoma. Radiologia. 2014;56:e17–e20. doi: 10.1016/j.rx.2011.10.010. [DOI] [PubMed] [Google Scholar]


