Participants of the Expert group on CPG for management of sexual dysfunction
Murgesh Vaishnav, G Prasad Rao, Neelanjana Paul, Mukesh P Jagiwala, Roop Sidana, M S Bhatia
INTRODUCTION
Sexual functioning is a complex bio-psycho-social process, coordinated by the neurological, vascular and endocrine systems. In addition to the biological factors, the psychosocial factors like societal and religious beliefs, health status, personal experience, ethnicity and socio-demographic conditions, and psychological status of the person/couple play an important role in adequate sexual functioning of a person. In addition, sexual activity incorporates interpersonal relationships, each partner bringing unique attitudes, needs and responses into the coupling. A breakdown in any of these areas may lead to sexual dysfunction.
Prevalence of sexual dysfunction in general population is very high. It is suggested that about 43% of women and 31% of men have one or other kind of sexual dysfunction. Among men, premature ejaculation is the most common male sexual dysfunction. There is lack of consensus with regards to the most common sexual dysfunction in women with some studies reporting hypoactive sexual desire disorder to be the most common entity, followed by orgasmic and arousal disorders; whereas other studies suggest that difficulty achieving orgasm and vaginal dryness to be the most common type of sexual dysfunction in women. Problems of sexual dysfunction may be lifelong or acquired, general or situational.
Although sexual problems are highly prevalent, these are frequently under-recognized and under-diagnosed in clinical practice. It is also noted that clinicians also have lack of understanding about the approach for identification and evaluation of sexual problem. It is often recommended that the treating psychiatrists and collaborating specialists need to possess broad knowledge and appropriate attitude towards human sexuality.
The essential concepts underlying the management of sexual problems are adoption of a patient-centered framework for evaluation and treatment. Principles of evidence-based medicine may be followed in both men and women in diagnostic and treatment planning and adoption of common management approaches for sexual dysfunction. The purpose of these guidelines is to present a framework for the evaluation, treatment, and follow-up of the patient/couple, who presents with sexual dysfunction. We hope that these guidelines would help in facilitating proper management of patients presenting with various types of sexual dysfunction. These guidelines are to be read along with the earlier version of Indian Psychiatric Society Guidelines.
CLASSIFICATION OF SEXUAL DISORDERS
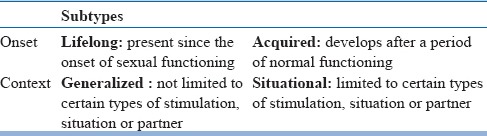
Compared to DSM-IVTR, DSM-5 has fewer categories for describing sexual dysfunction and has provided gender-specific sexual dysfunctions (Table-1). Other major change in DSM-5 includes the duration criteria. According to DSM-5 the minimum duration for making the diagnosis of sexual dysfunction is 6 months (except substance-/medication-induced sexual dysfunction) for almost all the disorders and also specifies the frequency of dysfunction to be 75-100%. DSM-5 has also done away with the categories of sexual aversion disorder and sexual dysfunction due to a general medical condition. The category of substance induced sexual dysfunction is now labelled as Substance/Medication induced sexual dysfunction. The Not Otherwise Specified (NOS) category has also been removed. The substance or medication-induced sexual dysfunction has been retained as such. Various types of sexual dysfunctions are categorized on the basis of onset and context (Table-2).
Table 1.
Comparison of diagnostic categories of ICD-10 & DSM-5 of sexual disorders
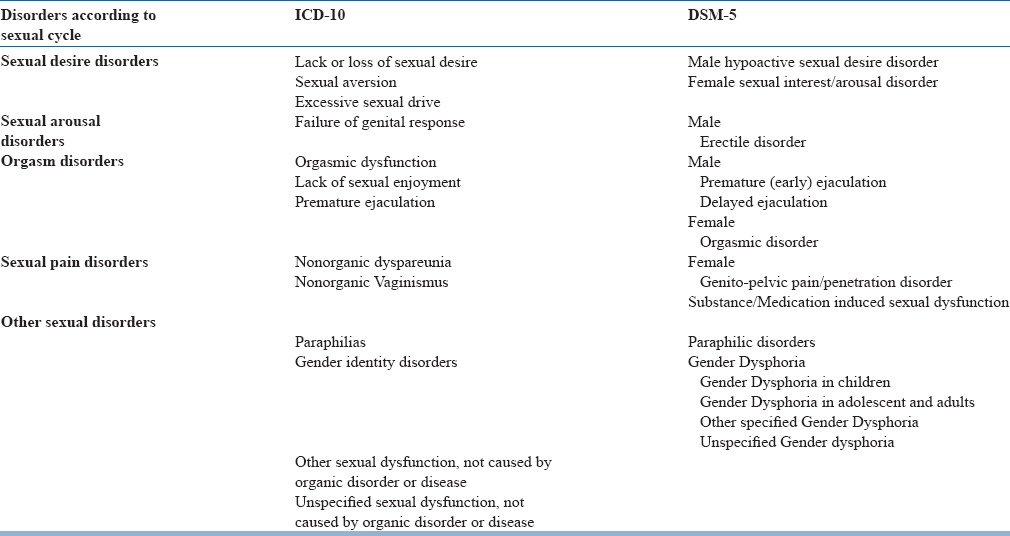
Table 2.
Subtypes of sexual dysfunctions according to DSM-5
ICD-10 describes sexual disorders under the headings of: Sexual dysfunction, not caused by organic disorder or diseases (F52) under the broad heading of Behavioral syndromes associated with physiological disturbances and physical disorders, Gender Identity disorders (F64), Disorder of sexual preferences (F65), Psychological and behavioral disorders associated with sexual development and orientation (F66), under the broad heading of Disorders of adult personality and behavior.
Other sexual disorders/dysfunctions in Indian context
Although both the nosological systems have classified sexual disorders, but they don’t include certain sexual disorders commonly seen by Indian clinicians. Indian researchers have consistently alluded to the existence of certain unique socio-culturally determined sexual clinical conditions such as, Dhat syndrome and Apprehension about potency. Dhat syndrome has been coded in ICD-10 under other neurotic disorders (F48.8), but the diagnosis of apprehension about potency doesn’t find mention. The clinical entity of apprehension about potency is related to the commonly held belief in most of the Indian sub-cultures that masturbation and night emissions before marriage result in loss of potency in marital conjugal relations. Masturbation is considered to be responsible for shrinkage or sideward curvature of penis and watery semen. Thus, there are exaggerated apprehensions in males centered on sexual performance on “First wedding night (Suhaag raat)”. Some of the studies have also shown that many females who have leucorrhoea, for which no infective or pathological cause could be found have psychasthenic syndrome or female Dhat syndrome, similar to Dhat syndrome in males.
Sexuality is understood as a broader concept which goes beyond sexual dysfunctions. These guidelines are applicable for management of sexual dysfunctions and some of the disorders, like Dhat syndrome which are seen in the Indian context and are associated with high rates of comorbid sexual dysfunctions.
ASSESSMENT OF PATIENTS WITH SEXUAL DYSFUNCTIONS
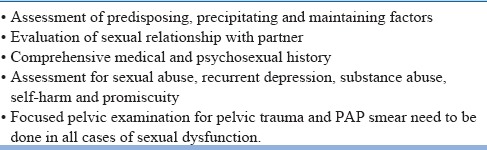
Evaluation of any patient with sexual dysfunction requires thorough understanding about the type of sexual dysfunction, factors associated with or contributing to sexual dysfunction and factors maintaining the sexual dysfunction. Accordingly, proper evaluation includes detailed history taking (sexual, medical and psychosocial), focused physical examination, laboratory tests (routine and specific) and consultation with appropriate specialists. Careful attention always be paid to the presence of significance comorbidities or underlying etiologies (e.g., cardiovascular disease, diabetes, depression).
Important aspects of evaluation of patients with sexual dysfunctions
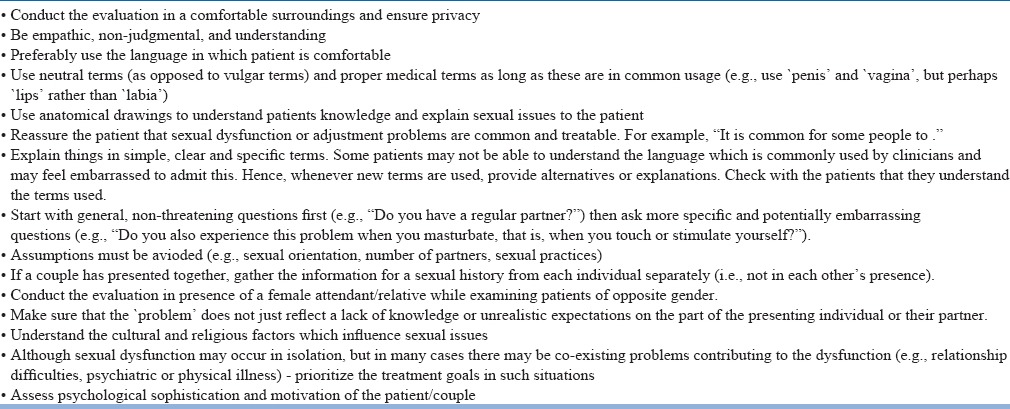
Discussing sex-related issues can be embarrassing both for the clinician and the patient. Patients often carry the feeling of failure or that they are abnormal. Clinicians should anticipate the embarrassment of patient and acknowledge that it could be difficult talking about such issues. For example, the clinician may say, “Most people find it difficult to talk about these things and may feel a bit embarrassed. I’d just like to reassure you that everything you say is confidential and that I’d like to help you if I can. The first step is to find out exactly what's going on so that we can figure out how to make things right again. Please feel free to be open with me and to ask questions whenever you have any doubt.” Some of the other important issues for evaluation are given in Table-3.
Table 3.
Important aspects in evaluation of sexual dysfunctions
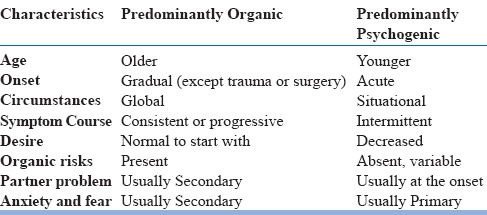
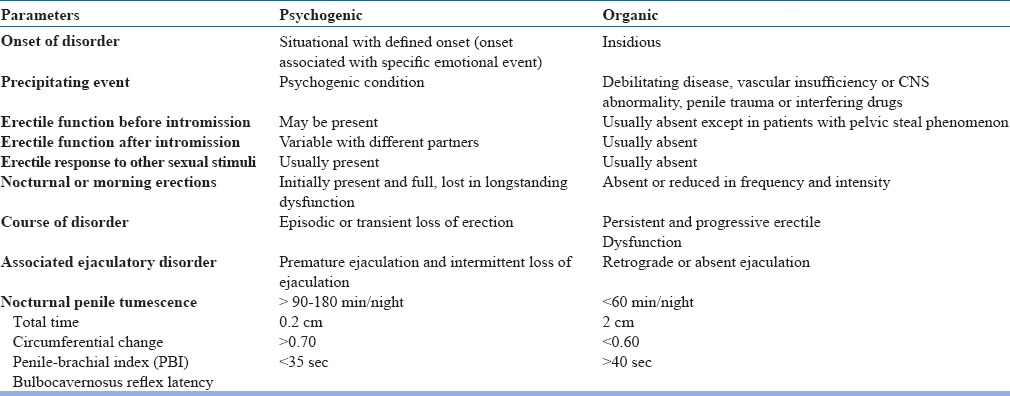
The basic principles of sexual history taking are given in table-4. The patient needs to be asked to describe their problem in terms of time and manner of onset, its course over the period, its current status, and associated medical or psychological problems. While taking history, attention must be given to features which can help in distinguishing predominantly psychogenic from predominantly organic sexual dysfunctions (Table-5). But, it is important to note that, in many cases, organic and psychogenic factors may coexist, particularly in individuals or couples with long-standing or chronic sexual dysfunction. In such cases, clinicians need to assess the independent and interactive role of both organic and psychogenic factors.
Table 4.
History taking for sexual disorders
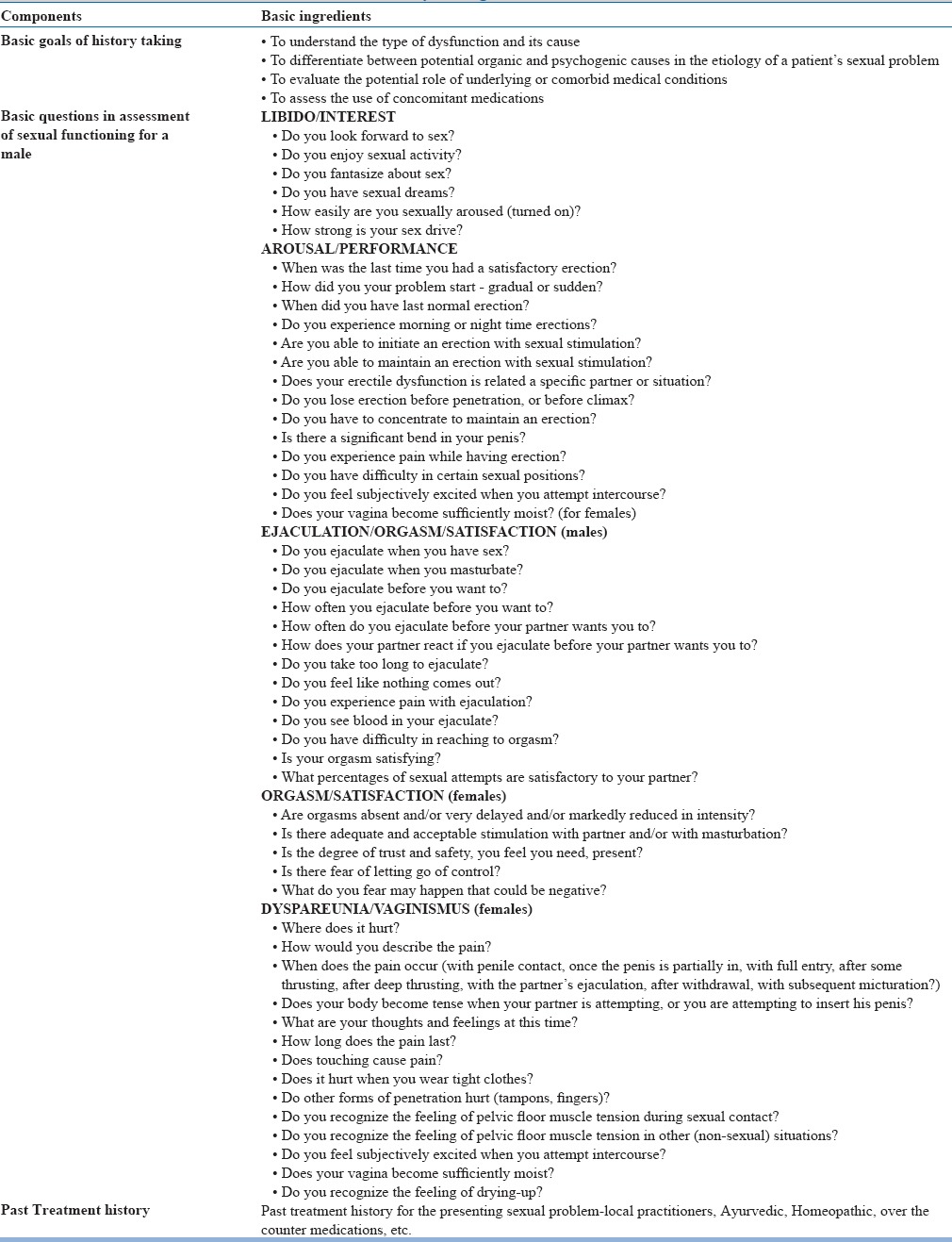
Table 5.
Differentiating features between psychogenic and organic sexual dysfunction
An important aspect of sexual history taking in females is to remember that women play different roles at different times in their life. Many women have several roles-the professional or worker, housewife, mother, daughter, friend, and lover. It is often seen that the over the years as the demands of other roles increase, lover role fades away. Paying attention to these issues can be very useful, and this information can be collected by using a process called the “timetable of life.” Both partners can be asked to fill in a timetable representing a typical week from their initial interaction to the time of presentation. Various aspects which can be covered during the assessment of a week during a typical time frame may include, family time (that is, with children and partners), work time (both at work and work in the house), extended family time (with parents and relations), social time, personal time, and relationship time (time spent together as a couple). The relationship time must also include information about the sexual activity. A timetable almost always brings forward various elements missing in the relationship and personal time. Repeating the “timetable” for different times in life and comparing it during courtship, when sexual desire was probably good, with the timetable for a time when sexual desire was low is useful and can show how priorities change and how this influences desire for sexual activity. Looking at what happens in a sexual situation often gives much information about the defenses used when a patient engages in sexual activity. Clinician may also note what turns a patient on and off, how engorged he/she becomes in the sexual experience, and whether loss of desire occurs every time or it is situational. Other important aspects which can enhance the understanding about the problem include sexual fantasy, masturbation, genital functioning, and contraception.
Psychosocial history: Psychological factors associated with sexual dysfunction can be divided into three categories: predisposing factors, precipitating factors, and maintaining factors (See table-6), which can co-exist with each other. The areas to be explored in psychosocial history are enlisted in table-7. It is to be remembered that the existence of an organic disease does not rule out the possibility of a coexisting psychogenic factor. Conversely, the presence of psychogenic conditions, such as anxiety, anger, guilt, or marital discord, need not be considered as evidence for a sole primary causation.
Table 6.
Psychological factors associated with sexual dysfunctions
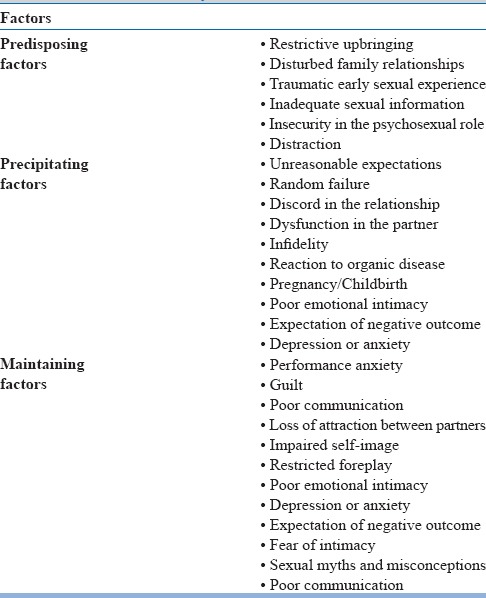
Table 7.
Psychosocial assessment of sexual dysfunctions
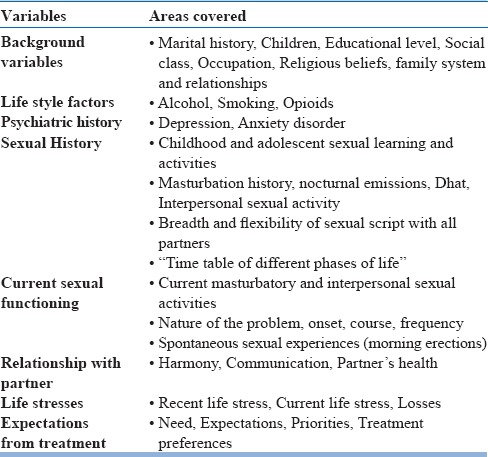
The current psychological state need to be assessed with special focus on symptoms of anxiety or depression, low self-esteem and coping skills, previous and current partner relationships, history of sexual trauma/abuse, occupational and social stresses, socioeconomic status, and educational level. Sexual dysfunction may affect the patient's self-esteem and coping ability, as well as his or her social relationships and occupational performance. These aspects need to be assessed in each case. Clinicians need not assume that every patient is involved in a monogamous, heterosexual relationship.
Considering the fact that sexual problems arise in the interpersonal context, the clinician need to carefully assess past and present partner relationships. Another important aspect of psychosexual history is inquiring specifically about the quality of the relationship between the couple with respect to nonsexual factors, i.e., how to they get along on most issues, communication patterns, gender equality/inequality, level of commitment, dealing with stress, etc. While interviewing the couple together it is important to note the dynamics between the partners. Relationship problems may be due to intrinsic differences between the two, and expectations about sexual fulfillment may also vary. Many a times, lack of proper communication between the couple, which may be due to embarrassment, may be mistaken as lack of caring.
Another important aspect of psychosocial evaluation is the identification of patient/couple needs, expectations from each other, priorities and treatment preferences. These may be significantly influenced by cultural, social, ethnic and religious perspectives. Patient education about the problem is also important in enhancing therapeutic relationship, communication between patient and physician and ensuring patient compliance. Partner involvement is important. On the first visit, it is not always possible to involve the partner but efforts need to be made to involve the patient's partner early in the treatment process at the earliest. If the psychosocial assessment reveals the presence of significant psychological distress or conflict between the couple, further evaluation and management may be carried out either prior to, or along with treatment of sexual dysfunction.
Medical history: Historical events related to the presence of chronic disease, use of pharmacological agents, endocrine disorders, prior surgeries and trauma is to be carefully evaluated. While evaluating women careful medical history is to be obtained about any health problem that might affect sexual anatomy, the vascular system, the neurological system, and the endocrine system. Indirect causes i.e., factors that cause chronic pain, fatigue, and malaise may also contribute to dyspareunia.
Substance use History: Excessive use of alcohol or use of other recreational drugs may cause sexual dysfunction, either by a direct effect on the penile neurovascular system or by causing increased secretion of prolactin, reduction in production of testosterone, or both.
Treatment/Medication History: Clinicians should also enquire about the medication intake, including prescription drugs, over the counter medications and culturally sanctioned aphrodisiacs. Medications commonly associated with sexual dysfunction include diuretics (thiazides, spironolactone), sympatholytics agents (Central agents like methyldopa, clonidine and peripheral agents like reserpine), alpha blockers, beta blockers (particularly nonselective agents), angiotensin-converting enzyme inhibitors, calcium channel blockers, antipsychotics, antidepressants, benzodiazepines, buspirone, lithium, disulfiram, digoxin, histamine H2-receptor blockers, ketoconazole, niacin, phenobarbital, phenytoin, allopurinol, gemfibrozil, clofiberate, phenobarbital, phenytoin, danazol, GnRH agonists, oral contraceptives etc.
Physical Examination
Every effort be made to ensure the privacy, confidentiality and personal comfort of the patient while conducting the physical examination. Careful physical examination not only corroborates the medical history but at times also reveals unsuspected physical findings (e.g., decreased peripheral pulses, vaginal atrophy, atrophic testes, penile plaque).
In addition, to the general and systemic evaluations, detailed assessment of gonadal function, vascular competence, neurological integrity, and genital organ normalcy is to be performed on every patient. Patients suspected of hypogonadism need to be assessed for evidence of muscle development, size and structure of the penis, normal urethral opening, hypospadias, size and consistency of the testes and the prostate. Alcohol swabs can be used to test penile temperature sensation. Bulbo-cavernosus reflex can be elicited by squeezing the glans penis and assessing the evoked contractions of external anal sphincter or bulbo-cavernosus muscles. This reflex response is clinically detectable in 70% of normal males. The penis also needs to be examined for evidence of any masses or plaque formation, angulation, unprovoked persistent erection, or tight unretractable foreskin.
Similarly in females genital examination is often highly informative, especially in cases of dyspareunia, vaginismus, with a history of pelvic trauma and with any disease potentially affecting genital health. If there are indications from history, the opportunity for pap smear/sexually transmitted disease investigation is to be taken.
Recommended Laboratory Testing
Recommended laboratory tests for men and women with sexual problems typically include blood glucose levels, cholesterol, lipids, hormonal profile and X-ray spine for spina bifida. Additional laboratory tests (e.g., thyroid function) may be performed at the discretion of the clinician, based on the medical history and clinician's judgment. When an infective etiology for dyspareunia remains a possibility- vaginal, cervical and vulval discharge microscopy/cultures need to be performed.
Assessment of Knowledge and Attitude towards sex
Few patients may not actually have sexual dysfunction, but may perceive the same, because of poor knowledge and negativistic attitude towards sex. Further, in some patients the sexual problems may be attributed to the beliefs and cultural practices. Some of the scales like Sexual Knowledge and Attitude Questionnaire and Dhat syndrome Questionnaire, which have been validated in the Indian context, may be used for structured assessment and documentation. These scales can also help in determining the area to be focused in sex education and psychoeducation.
Specialist Consultation and Referral
Patients with history of medical problems be referred to appropriate specialty to evaluate the severity and state of disease control (See table-8). Sometimes there may not be a need for referral, but if patient requests for the same, it is to be done. Further diagnostic evaluation also needs to be conducted in case of lifelong or primary sexual dysfunction, in the presence of specific anatomic or endocrine factors and failure of initial therapy. Patients with hyposexual desire and absent or retarded emission or anorgasmia may need to be evaluated for the presence of diseases involving the nervous system. Patients with prolonged or painful erection need to be evaluated for the possibility of primary penile disease, hematological disorder, or other systemic diseases associated with penile complication.
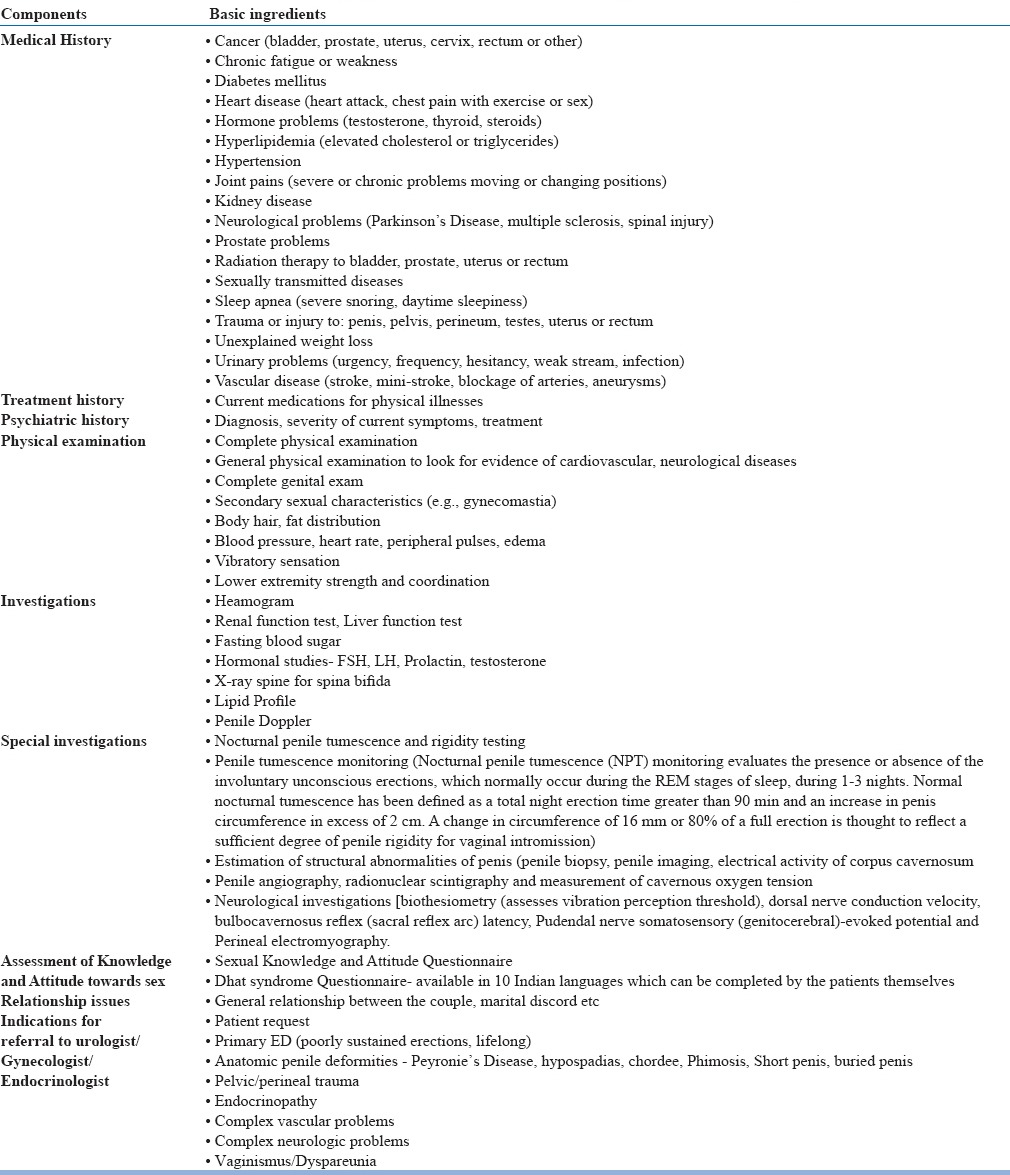
Table 8.
Medical history, physical examination and investigations for sexual dysfunctions
By the end of assessment the clinician should be able to answer the following questions for themselves to plan management:
Does patient/couple actually have sexual dysfunction?
Whether the dysfunction is primarily psychogenic or primarily organic?
If the dysfunction has organic etiology, then is there a psychological overlay too?
If there are more than one dysfunction, then which is the primary?
Does patient has any comorbid psychiatric disorder?
If subject has a psychiatric disorder, then is the sexual dysfunction secondary to it?
If subject has a psychiatric disorder, then how severe it is?
Is there a marital discord between the couple, which needs to be addressed?
What is the motivation of the patient/couple to seek treatment?
What is the level of psychological sophistication?
MANAGEMENT OF SEXUAL DYSFUNCTION
Principles of management
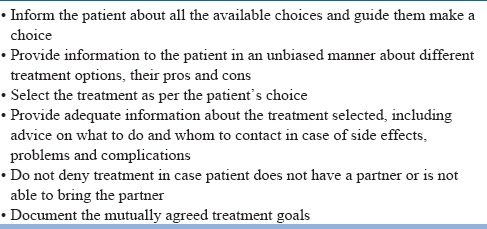
Management of sexual dysfunction involves patient centered approach and clinicians are expected to consciously adopt the patient's perspective and respect the ideas, feelings, expectations and values of their patients. Some of the basic principles of patient centered approach are given in Table-9.
Table 9.
Principles of treatment
Formulation: After complete assessment, the first step in the management is to provide the patient/couple a brief and simple account of the nature of their problems and possible contributory factors. The aims of the formulation are threefold. First, it helps the couple to understand their difficulties. This can be a source of encouragement, especially if the therapist also explains how common such problems are. Second, the therapist point out the likely contributory factors, particularly the maintaining factors which will be the focus of therapy, and thus establish a rationale for the treatment approach. Finally, providing a formulation also helps to check that the information obtained during the assessment has been correctly interpreted. So the couples need to be always asked to give a feedback of the formulation.
Balancing the partners: It is important for the therapist to understand the contribution of individual partner to the problem and need to strike a balance between individual partners. The therapist must emphasize the need of collaboration between the partners for the success of the therapy. The therapist needs to emphasize positive aspects of the couple's relationship.
Treatment options: Treatments for various sexual dysfunctions can be broadly classified into general and specific measures. The general measures include sex education and relaxation exercises. The specific measures can be either pharmacological measures, non-pharmacological measures or a combination of both.
Among the non-pharmacological measures, many types of psychotherapies like psychodynamic, interpersonal, rational emotive therapy, Master Johnson's behavioural therapy or its modifications, systematic desensitization, ban on sexual intercourse and skill training in communication of sexual preferences etc have been used. Unfortunately there are no well designed studies which have evaluated the effectiveness of these psychotherapies. Most of the studies done have used convenience sampling, don’t describe their sample adequately, have not used standard definitions for various disorders and are silent about the therapist variables. Hence the results cannot be generalized. Among all the techniques, which have been used, cognitive behavioural measures of Master Johnson or its modifications are the most popular and have been found to be most useful.
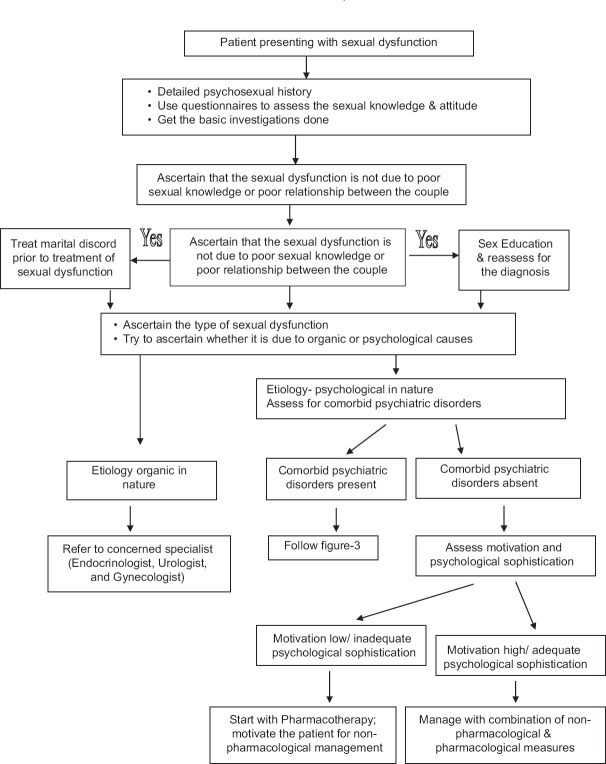
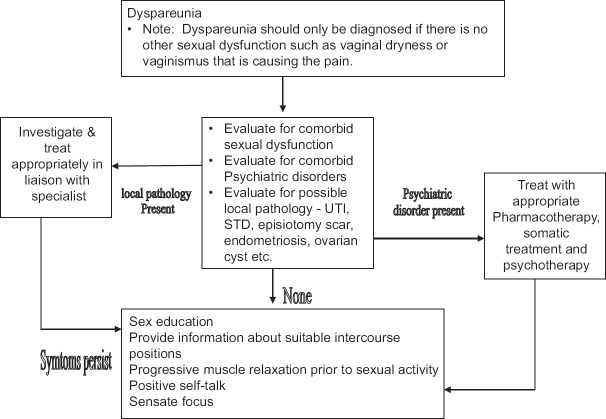
Selection of treatment: The final selection of treatment is to be according to patient/couple's choice. The therapist needs to inform the patient/couple about the available modalities and help them to make a reasoned choice. Agreed treatment goals need to be established at the start of treatment. Figure-1 and 2 shows the general outline for management of cases of sexual dysfunction presenting with or without psychiatric comorbidity. Initial evaluation involves detailed psychosexual history and getting the basic investigations. Besides taking a proper history, screening questionnaires can be used to assess the sexual knowledge and attitude. The initial evaluation will help in ascertaining the type(s) of sexual dysfunction. The next step involves establishing the probable etiological basis of the dysfunction, i.e., whether the dysfunction is organic in origin, psychological in origin or has components of both. If the dysfunction is organic in origin the patient is to be referred to the concerned specialists and need to be investigated and treated accordingly. It is often seen that some patients may have sexual dysfunction of organic origin, but would also have psychological factors contributing to its maintenance. Such patients are the most difficult to treat and require very good liaison between the psychiatrist and the physicians. In patients who have psychogenic sexual dysfunction, the next step involves evaluation for sexual knowledge, relationship issues, presence of comorbid psychiatric disorder, motivation and psychological sophistication of the patient for treatment.
Figure 1.
Treatment Algorithm for Evaluation & Management of a case of Sexual dysfunction
Figure 2.
Assessment and Management Algorithm for a case of sexual dysfunction with psychiatric comorbidity
Assessing the sexual knowledge and relationship issues are important aspect of treatment of sexual dysfunction as many a time the patient/couple may not have any sexual dysfunction per se but the reported complaints may be arising due to faulty beliefs or relationship issues. If any of these two factors are found to be contributing to the sexual dysfunction, these need to be focused and once they have been adequately addressed, the sexual dysfunction is to be reassessed and if present needs to be treated adequately.
If comorbid psychiatric disorder is present, the next step involves ascertaining – is it primary or secondary (primary- psychiatric disorder causing sexual dysfunction; secondary - psychiatric disorder is secondary to sexual dysfunction). The patient who have primary comorbid psychiatric dysfunction or those who have prominent psychiatric symptoms (may be secondary in origin), the psychiatric disorders is to be treated first and adequately before focusing on the treatment of sexual dysfunctions. While treating these disorders adequate care needs to be taken in selecting the pharmacological agent, so that the dysfunction is not worsened. In some cases the side effects of the drugs can in fact help in decreasing/ameliorating the sexual dysfunction, for example, for a case of depression with premature ejaculation selective serotonin reuptake inhibitors like paroxetine may be beneficial. If the psychiatric disorder is secondary and not prominent then the sexual dysfunction is to be treated first. An important aspect of treatment involves understanding the motivation and psychological sophistication. If the motivation for treatment is low or if patient has poor psychological sophistication, then the primary mode of treatment is pharmacotherapy. Patients who are highly motivated and/or have good psychological sophistication are to be treated with combination of non-pharmacological and pharmacological therapies.
General Non-pharmacological measures: Education about sexuality
The first step in the treatment of any sexual dysfunction is sex education/psychoeducation. The sex education needs to aim at normalization of the individual's experiences and reduce anxiety about sex by providing accurate information. The various components of sex education are shown in Table-10. Although all the areas are to be covered, special emphasis needs to be given to those areas, which are directly related to the patient's problem. Where ever possible figures and diagrams are to be used for reference and illustrations. In some cases the reading material can also be provided to the couple/patient. Sex education and teaching relaxation is to be carried out over about four sessions.
Table 10.
Aims and Components of education about sexuality
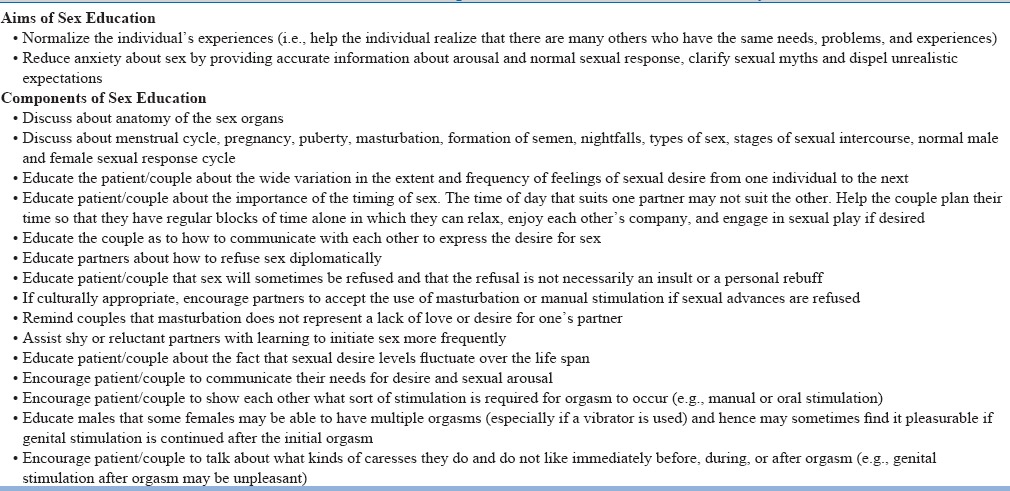
Understand and clarify sexual myths: For some individuals, inappropriate sexual beliefs or myths can cause problems within a relationship. Individuals acquire expectations about what sex should be like and how they or their partner should behave. One of the components of sex-education is to help the individual and his or her partner alter any sexual beliefs that interfere with the individual's enjoyment of sex. Some of these apply equally to both men and women, while others will be more relevant to one gender than the other. Some of the common myths are given in Table-11.
Table 11.
Common Myths about Sex
General Non-pharmacological measures: Relaxation exercises
Relaxation therapy should be taught to patient using Jacobson's Progressive Muscular Relaxation Technique or Benson Henry Relaxation Technique. This can be combined with the biofeedback machine so as to facilitate objective evidence and mastering of anxiety by the patient.
Specific Non-pharmacological management of Sexual Dysfunction
The specific non-pharmacological measures will vary according to the type of sexual dysfunction. However, one of the important components, of the specific measures includes home work assignment for the couple. It is important to remember that many of these measures are carried out simultaneously.
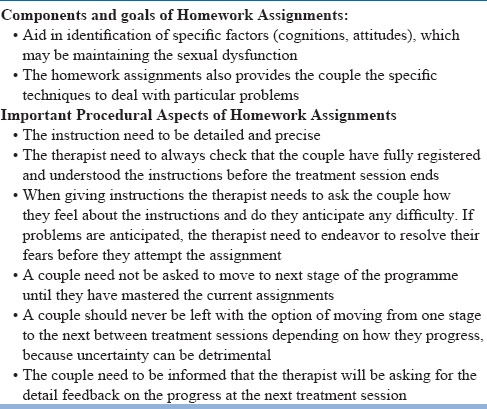
Homework assignment for the couple: The homework assignment provides a structured approach, which allows the couple to rebuild their sexual relationship gradually. The stages of this programme are labeled using the terminology introduced by Master and Johnson (1970) is: non-genital sensate focus, genital sensate focus and vaginal containment. There are some basic principles of giving and carrying out the homework assignments as shown in table-12.
Table 12.
Principles of giving and carrying out the homework assignments
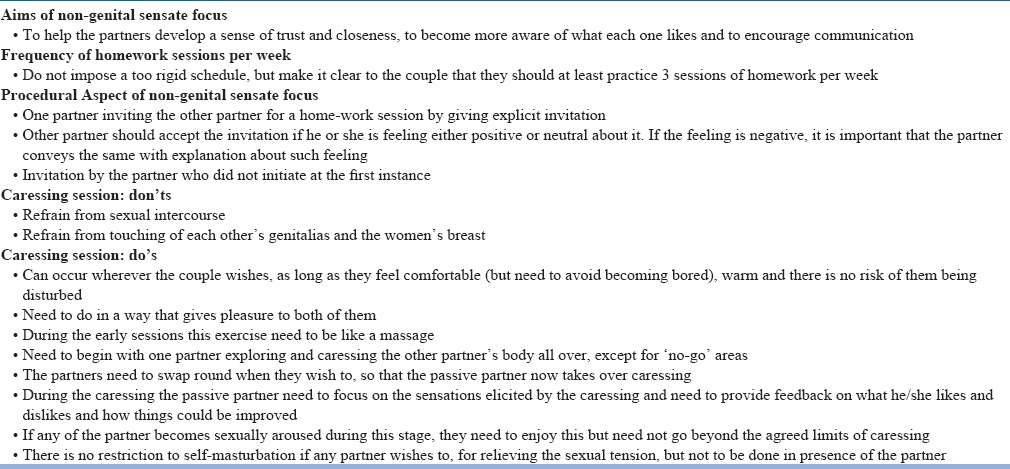
Non-genital sensate focus: This assignment is particularly helpful for a couple to establish physical intimacy in a comfortable and relaxed fashion, and allows open communication about feelings and desires. The basis aim of this stage is to help the partners develop a sense of trust and closeness, to become more aware of what each one likes and to encourage communication. Details of the procedural aspect of non-genital sensate focus session are given in Table-13. It is to be explained to the couple that they need to “refrain from sexual intercourse and touching of each other's genitalia and the women's breast” to ensure that they are not continually confronted by those aspects of sexuality that is most likely to cause anxiety, and to enable them to concentrate on rebuilding their physical relationship by first learning to enjoy general physical contact. Initial reactions to these sessions vary according to the nature of the couple's problem. Some couple's may find this enjoyable and others may react negatively. In some cases it will be appropriate for the therapist to just acknowledge the problem and reassure and encourage the couple. In some cases therapist have to explain that this is understandable and expected, but that in order to overcome a sexual problem like theirs it is necessary to approach it in a systemic fashion and with due course of time they will begin to get pleasure out of their sessions and these would come as spontaneous behaviour.
Table 13.
Non-Genital Sensate Focus
Some couples will have more serious difficulties in the form of negative responses to homework assignments, persistent breaking of the ban on sexual intercourse, or cessation of homework assignments. In such cases the focus of therapy might have to be changed temporarily and sessions may be required to help the partners express their feelings and anxieties. In occasional cases no progress can be made in developing understanding of why couple is encountering difficulties. In such cases it is worth seeing the partners separately to find out whether important information is being withheld by one of them.
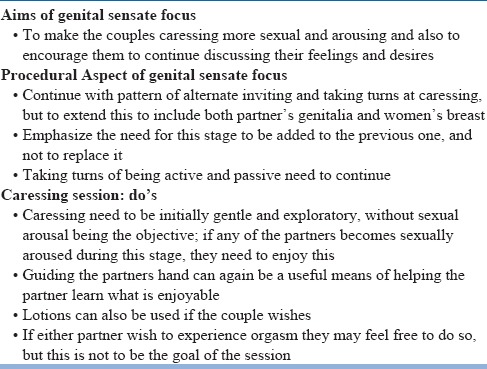
Genital sensate focus: The couples, who go through the non-genital sensate focus sessions successfully, need to be told to move to the genital sensate focus sessions. The aim and procedural aspect of genital sensate focus are given in Table-14. As with the non-genital sensate focus, some couples immediately find these sessions pleasurable while others would react adversely. This stage is particularly likely to generate anxiety, especially about sexual arousal or intimacy, so it is very important that the therapist specifically encourages partners to focus on pleasurable sensations. Some of the techniques for dealing with specific dysfunctions also need to be introduced at this stage.
Table 14.
Genital Sensate Focus
Vaginal Containment: This stage is an intermediate one in the introduction of sexual intercourse to the therapy programme. It is relatively minor stage for couples whose difficulties have by now largely resolved. For others it is extremely important, especially when vaginal penetration is the key step (e.g. ED, PME, and vaginismus). The couple is instructed that when they both are feeling relaxed and sexually aroused the women can introduce her partner's penis into her vagina and the partner to then lie still, concentrating on any pleasant genital sensations. The best position to attempt vaginal containment is female superior position or a side to side position. The couple be asked to maintain containment as long as they wish, and then they can return to genital and non-genital pleasuring. The couple can repeat the containment up to three times in any one session. Once this stage is well established the couple to introduce movement during containment, with preferably women starting the movements first. With this the general programme of sex therapy is completed and now the treatment need to include superimposition of treatment for specific sexual dysfunctions.
It is important to remember that during the whole therapy feedback be taken after every session and any doubts/misconceptions be clarified.
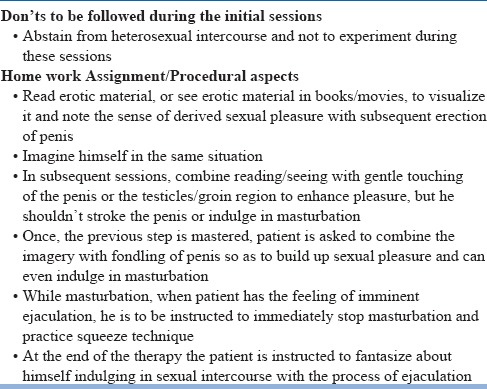
Home work assignments for single male
Management of sexual dysfunctions in single males also involves same principles. The subject be provided with sex education and thought relaxation exercises. The principles of home work assignments for single male with erectile dysfunction and premature ejaculation are given in Table-15 and Table-16. At the end the patient be counseled and reassured that he can now indulge in heterosexual experience without difficulty. However, he be cautioned that it should be done after few days, not in a hurry, and to be carried out in familiar surroundings without guilt or fear and anxiety.
Table 15.
Home work assignments for Single Male with Erectile Dysfunction
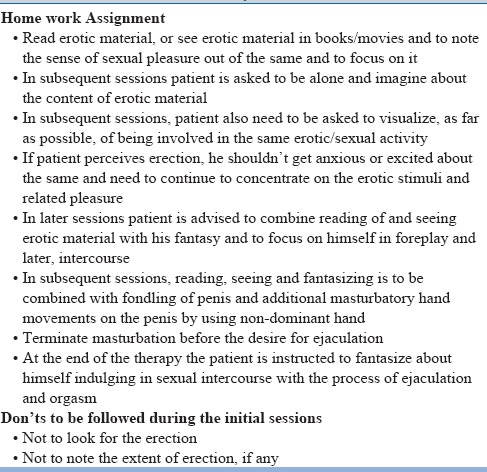
Table 16.
Home work assignments for Single Male with Premature Ejaculation
ERECTILE DYSFUNCTION
An important aspect of assessment of erectile dysfunction is to distinguish between psychogenic and organic erectile dysfunction (See table-17). Non-pharmacological measures are to be used in patients with psychogenic or mixed erectile dysfunction along with pharmacological agents.
Table 17.
Differentiating features between psychogenic and organic erectile dysfunction
Specific Non Pharmacological treatment for erectile dysfunction
Men with psychogenic erectile dysfunction will usually start experiencing erections during either non-genital or genital sensate focus. If the therapist suggests that during the initial phase the man tries not to have an erection this can have the opposite effect. Men with erectile dysfunction often have difficulty attending to erotic stimuli, especially when an erection develops, tending instead to think about the quality of their erection or whether they will be able to maintain it. The therapist need to specifically encourage the man to focus his attention on the pleasurable sensations he experiences during the partner's genital caressing (the use of a lotion can often heighten these sensations), areas of his partner's body that he finds arousing, and the pleasure of witnessing his partner's sexual arousal.
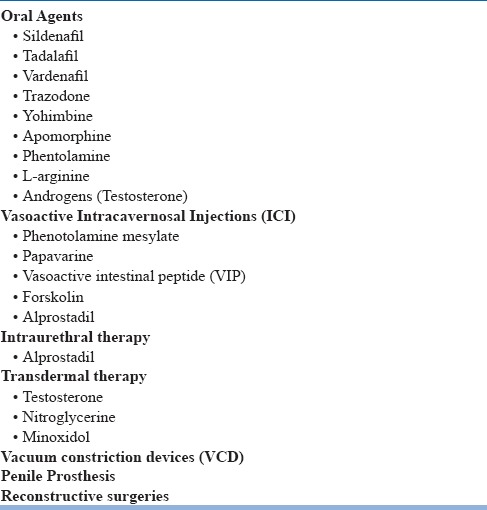
Pharmacological treatment for erectile dysfunction
Besides the psychological measures, other therapeutic options for erectile dysfunction includes medications, constriction ring, vacuum constriction devices, intra-cavernosal injections, intra-uretheral medication devices, penile prosthesis and reconstructive surgery (Table-18).
Table 18.
Treatment options for erectile dysfunction
Oral erectogenic agents
Oral therapy with vasoactive agents has emerged as the first line treatment and has transformed the management of erectile dysfunction.
Phospho-diaesterase inhibitors (PDE-5 inhibitors), i.e., sildenafil, tadalafil, vardenafil have proven efficacy and safety in men with erectile dysfunction and are considered as first line pharmacotherapy for management of erectile dysfunction. The profile of these drugs is shown in table-19. Among the available PDE-5 inhibitors, sildenafil and vardenafil have short half-life, whereas tadalafil have relatively longer half-life. Available data also suggests the safety of some of these PDE-5 inhibitors in patients with erectile dysfunction associated with diabetes mellitus, spinal cord injury, chronic renal failure, Parkinson's disease, antidepressant use and following radical prostatectomy. It is important to remember that action of PDE-5 inhibitors is dependent on androgens. Hence, in patients with hypogonadism management with PDE-5 inhibitors may not be effective and use of androgens may be an effective choice. Adverse effects of PDE-5 inhibitors are generally mild and dropout rates due to side effects are similar to placebo. PDE-5 inhibitors are metabolized by the cytochrome P450 3A4 and as a result may affect metabolism of protease inhibitors and antifungal medications. In general PDE-5 inhibitors have been shown to be safe and have not been associated with increased risk of myocardial infarction. However, it is important to remember that use of PDE-5 inhibitors is contraindicated in those receiving nitrate. Use of PDE-5 inhibitors along with antihypertensive medication like ACE inhibitors, angiotensin-receptor blockers, calcium channel blockers and diuretics can result in small additive decreases in blood pressure. Use of PDE-5 inhibitors along with alpha blockers can result in orthostatic hypotension.
Table 19.
Comparison of various PDE-5 inhibitors
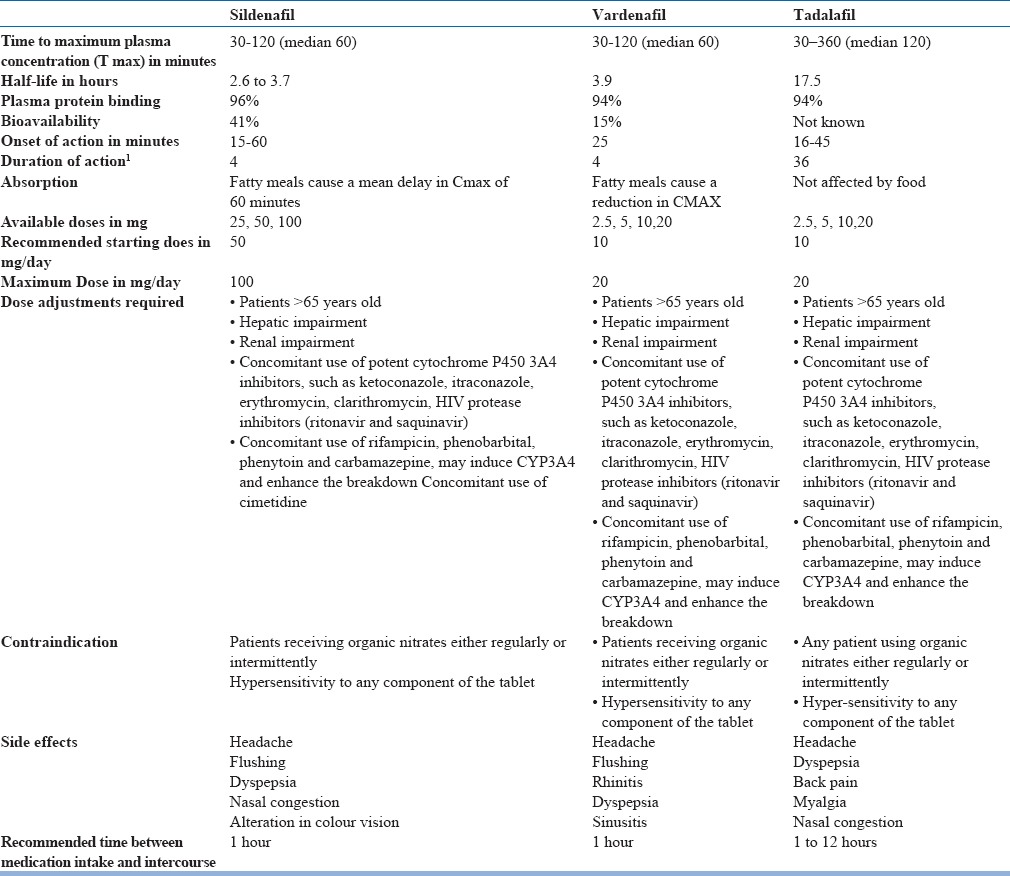
There are no comparative trials to suggest superiority of one PDE-5 inhibitor over the other. However, preliminary data from some of the cross-over trials suggest that some patients may respond better to one PDE-5 inhibitor than to another. Accordingly, it can be said that a patient who does not respond to one agent, may be shifted to another PDE-5 inhibitor. Some preliminary data also suggest that a proportion of patients who fail to respond to intermittent dosing, may respond to daily dosing.
The selection of medication is to be done on the basis of frequency of intercourse. Although very robust data is not available, but daily use of tadalafil is associated with improved endothelial function with a sustained effect after its discontinuation, whereas such effects are not seen with use of on-demand tadalafil.
A subject who does not respond to 6-8 doses of a PDE-5 inhibitor with sexual stimulation at maximum dose is considered as non-responder to a PDE-5 inhibitor. However, it is to be remembered that most often patients fail to respond due to incorrect use of PDE-5 inhibitors and these include failure to use adequate sexual stimulation, adequate dose and failure to wait for the adequate duration for the action of the medication to start. It is to be remembered that even though all the 3 PDE-5 inhibitors have onset of action within 30 minutes of oral ingestion, in most patients a lag of 60 minutes is required for sildenafil and verdenafil and 2 hours for tadalafil. Based on the half-life of the medication, the normal window of efficacy of sildenafil and verdenafil is 6-8 hours after ingestion, whereas the window of efficacy for tadalafil is about 36 hours. Patient prescribed PDE-5 inhibitors are to be adequately psychoeducated with respect to dose of medication, timing of medication, relationship of dosing with fatty meal, need for sexual stimulation and window during which desired effect will be perceived.
Other oral erectogenic agents
Trazodone: One of the earliest drugs used in erectile dysfunction was trazodone. Trazodone and its active metabolite have antagonistic effect on 5HT2C receptors and may also have adrenoceptor antagonistic action. Available data suggest that trazodone is more efficacious than placebo in mixed and psychogenic erectile dysfunction.
Yohimbine: It is a α2-adrenergic blocker. Before introduction of sildenafil, yohimbine was the most widely used oral medication for management of erectile dysfunction. Available evidence suggests that it is more efficacious than placebo.
Apomorphine: Apomorphine is a dopamine agonist (D1 & D2 receptors) and its sublingual form (Apo-SL) is a new central initiator of erection and has been found to be effective in various types of erectile dysfunction.. Recent studies show that sublingual apomorphine has a safe cardiovascular profile and thus making it a new treatment option for patients with concomitant disease including cardiovascular disease and diabetes mellitus.
Phentolamine: Oral phentolamine mesylate, is a competitive inhibitor of α- adrenergic receptor. It also has the advantage of lack of interaction with nitrates and hence has been suggested as an alternative to treatment of erectile dysfunction in patients with cardiac illness.
L-arginine: L-arginine is the precursor of Nitric Oxide (NO) and has been shown to improve erections in 40% of patients.
Androgens
Androgens are useful for erectile dysfunction in men with severe hypogonadism and may be useful as adjunctive therapy when other treatments are unsuccessful by themselves. Libido and an overall sense of well-being are likely to improve when serum testosterone levels are restored to the reference range. Some evidence suggests that combination of testosterone and PDE-5 inhibitors yields better results. Usually testosterone is used parenterally, either once a week or once in 2 weeks. Other methods of administration like skin patches, testosterone gel is also available, but this is to be used daily and is costly. Testosterone implants are also available, which can last for 3-6 months. However, it is to be remembered that use of exogenous androgens suppresses natural androgen production. Elevated serum androgen has the potential to stimulate growth of prostate gland and increase the risk of cancer. Use of exogenous testosterone is also known to be associated with erythrocytosis, elevated serum transaminase levels, exacerbation of untreated sleep apnea, benign prostatic hyperplasia, and an increased risk of adenocarcinoma of the prostate. Accordingly, periodic examination of prostate, estimation of prostate-specific antigen (PSA) and heamogram are recommended in all patients receiving supplemental androgens. Obtaining a testosterone level during therapy is necessary for optimizing the dosage.
Vasoactive Intracavernosal Injections (ICI)
Since early1980s, till advent of sildenafil, intracavernous injections were the mainstays of the treatment of erectile dysfunction. The agents which have been used for intracavernous injections include phentolamine mesylate, papavarine, vasoactive intestinal peptide (VIP), forskolin and alprostadil.
Phentolamine mesylate, an a - adrenoceptor antagonist acts via increasing cAMP and decreasing intracellular Ca2+ and also possibly via nitric oxide synthase (NOS) activation. Clinical efficacy and safety of intracavernosal mesylate has been well documented.
Papavarine is a non-selective inhibitor of phosphodiesterase (PDE) and acts by increasing cAMP thus decreasing intracellular smooth muscle. It is used in papavarine (20-80 mg) induced penile erection (PIPE) test to distinguish between psychogenic and organic ED. However, it has limited efficacy so it is used with other agents such as phentolamine and with phentolamine and prostaglandin E1.
VIP and Forskolin which increase cAMP, have been found to be efficacious in moderate to severe erectile dysfunction resistant to monotherapy and polypharmacotherapy. No pain at site of injection has been reported with VIP, which is an advantage to patients.
Alprostadil, a synthetic prostaglandin E1 is an adenylate cyclase activator and is now the drug of choice of intra-cavernosal pharmacotherapy. Intracavernous alprostadil in the dose of 5-40 µg is most efficacious as monotherapy. It leads to erection in 5-15 minutes and the duration of ejection depends on the dose of the medication used. It is reported have an efficacy of more than 70% and has also been found to be effective in patients with erectile dysfunction associated with diabetes mellitus and cardiovascular disease. Patient and partners also report high satisfaction rates. However, in long run use of intra-cavernosal alprostadil is associated with high dropout rates (41-68%), with most dropouts’ occuring during initial 3 months of therapy.
When used it is to be initially be given in the clinicians office at the lowest dose and gradually the dose need to be titrated to an adequate erectile response while monitoring for syncope. Intracavernosal alprostadil is considered to be more effective and better tolerated over the intraurethral form. Due to this Intracavernosal alprostadil is preferred over intraurethral alprostadil. Common side effects of intra-cavernosal alprostadil are penile pain, edema and hematoma, palpable nodules or plaques, and priapism. Patients are to be clearly informed about the chances of occurrence of priapism and what do in such situation. The patient is to be counseled that if the erections persists for more than 4 hours, they need to seek emergency medical help. Management of priapism in such situations involves aspiration of blood from corpus cavernosum under local anaesthesia. If this fails than intra-cavernosal phenylephrine injection is to be given with proper monitoring for severe hypertension, tachycardia and any arrhythmia.
Due to its synergistic action, it is often used with phentolamine and papavarine. Some studies have demonstrated that patients of erectile dysfunction preferred combination [Phentolamine (0.25-1.5 mg) + Papavarine (8-16 mg) + Prostaglandin E1 (10-20 µg)] to sildenafil, regardless of the etiology.
A meta-analysis of 25,000 patients showed that the advantage of mixing above agents is that lower doses of drugs are required thus leading onto synergistic effects with lesser side effect. Prominent side effects are pain, priapism, corporal fibrosis and scar tissue formation. Also, being an invasive procedure, many patients find it inconvenient to inject repeatedly. Procedural complicacy, bleeding and injury to urethra caused higher attrition rates at 1 year follow-up of patients being treated with intracavernous vasoactive drugs.
Intraurethral therapy
Medicated urethral system for erection (MUSE), which contains 500-1000 mg of alprostadil, has shown success rates varying from 43-69% in efficacy studies. It has advantages that it can be self-administered and has little systemic and local side effects.
Topical therapy (Transdermal delivery)
This option minimizes both systemic exposure and tissue traumatization and involves administration of vasoactive substances across skin of the penis. This has added benefit from the patient's perspective in being a less invasive option. Pilot studies using Soft Enhanced Percutaneous Absorption (SEPA) technology, give ground for optimism. Preliminary evidence suggests that prostaglandin-E1+ SEPA are effective in 80-90% of patients. Nevertheless, this option requires more intensive research before approval by regulatory authorities.
Testosterone therapy for ED is indicated only in confirmed cases of endocrinopathies and is to be reserved for patients with documented hypogonadism. Transdermal administration has been developed recently. Gel containing 2.5-5.0 mg of testosterone-applied daily to the abdomen, back, thighs or upper arms have shown to produce normal plasma testosterone levels. Patients using testosterone skin patches have reported improvements in libido, sexual function, energy and mood. Adverse skin reaction (9% of cases) can be treated with topical hydrocortisone or antihistamine cream. Serum prostate specific antigen (PSA) levels is to be measured before testosterone therapy is started.
Nitroglycerine, a nitric oxide donor and minoxidil ointments have met with only minimal success. Although still under investigation, but these agents could acts as another tool in the armamentarium for treating erectile dysfunction.
Vacuum constriction devices (VCD)
Vacuum devices work by exerting a negative pressure on the penis, which results in an increase in corporeal blood flow and erection. A constriction ring placed around the base of the penis prolongs the erection by decreasing corporeal drainage. The erection obtained with a vacuum device is different from that obtained normally as there is no relaxation of the trabecular smooth muscle. Instead blood is trapped in the intra and extracorporeal regions of the penis. The time taken to achieve an erection varies, but is generally around 2-2.5 mins. The band need not be left in the place for more than 20 mins. Majority of the vacuum devices currently marketed use either a battery or a hand pump to generate vacuum. Overall success rate with VCD has been reported to be around 90%, with more than 80% of patients continuing with the device. Another study quoted that 53% patients reported satisfaction with only 23% continuing with the device. Drawbacks of VCDs include pain, petechiae, obstruction of ejaculation, penile pivoting, numbness and slight bluish colouration due to cyanosis. Almost all patients of ED can use VCDs. The vacuum devices are contraindicated in patients with severe Peyronie's curvature, sickle cell anaemia or blood dyscrasias and those on anticoagulants.
Penile Prosthesis
Since their introduction about 3 decades ago, penile implants are still a widely chosen treatment option, mostly after failure of all forms of therapy for erectile dysfunction. There are various forms of penile prosthesis, i.e., semi-rigid rod prosthesis consists of two rod like cylinders that are implanted into corpora cavernosum, mechanical rods (Dura II), malleable rods and inflatable penile prosthesis (Unitary, two-piece, and three-piece devices). Usually 3 piece inflatable penile prosthesis is preferred as it leads to more natural erections. Postoperative complications of penile implants include infection and mechanical malfunction. Peri-prosthetic infection requires immediate antibiotic therapy and removal of prosthesis.
Reconstructive surgery
Surgery for venous leakage involves penile venous ligation or embolization. Venous ligation restores spontaneous erections in only 50% of patients. Arterial revascularization is an experimental procedure used for treatment of vasculogenic ED. Upto 65% of patients report return of erectile function following arterial revascularization, but careful patient selection is necessary. Generally, good results are obtained only in young men with pure arteriogenic erectile dysfunction. A number of complications associated with arterial revascularization including arterial haemorrhage, glans-penis hyperemia, anastomotic occlusion, diminished penile sensation and fibrosis.
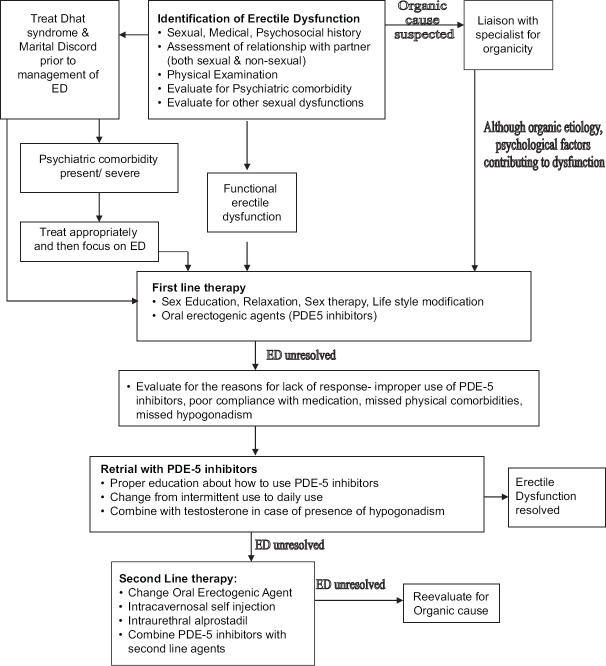
Steps in the Management of Erectile Dysfunction
First step is to confirm the diagnosis of erectile dysfunction as per the prevailing nosological system. The consensus is that inability to attain and maintain an erection sufficient to permit satisfactory sexual performance, lasting for more than 6 months, is considered to be an indicator of presence of erectile dysfunction. The general principles of evaluation of erectile dysfunction are shown in Table-20. The most important issue in management is evaluation for the organic factors, look for comorbid psychiatric conditions, comorbid sexual dysfunction and marital disharmony. However, it is to be remembered that although the cause may be organic, psychological causes can worsen the ED, so treating with behavioural measures in such cases is also an important step in the management. Once the evaluation is complete the patient/couple is to be explained about the potential beneficial and adverse effects of available treatment and guide them to make an informed choice. The selection of treatment strategy for erectile dysfunction is outlined in figure-3. If patient has Dhat syndrome along with erectile dysfunction, it is to be addressed first. Psychiatric disorders and marital harmony is to be addressed prior to treatment of erectile dysfunction and a similar protocol need to be followed.
Table 20.
General principles of evaluation of erectile dysfunction
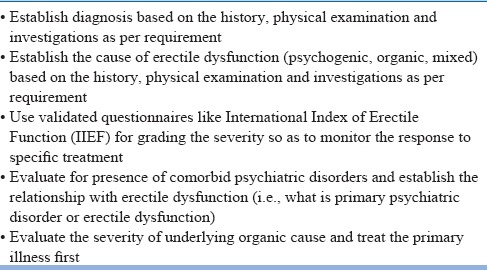
Figure 3.
Treatment algorithm for management of patients with ED
Initial treatment involves providing sex education, clarifying the myths, teaching relaxation exercises, and sensate focus training. After assessing coexistent problems, while providing formulation and sex education, education about factors that create a normal sexual response and erectile dysfunction can help patients and their partners cope with sexual difficulties. It is also important to change/remove/reduce the associated modifiable or reversible factors, including lifestyle or drug-related factors. Changes in lifestyle like smoking cessation, control of diabetes/ cholesterol, weight loss and reduction in stress are of prime importance. The success of psychosexual therapy is guided by the motivation of the patient, as this require him to work with the therapist to understand what prevents him from experiencing normal sexual arousal.
Follow-up plan is to be tailor made for the individual and there is no single follow-up regime. However, regular follow-up at 4 weeks for 6 months is usually recommended.
In terms of pharmacological treatments (see Table-21), PDE-5 inhibitors are considered to be the first line therapy in treatment of erectile dysfunction. The PDE-5 inhibitors available in India include sildenafil, vardenafil and tadalafil. Apomorphine sublingual has the advantage of quick onset of action. It is well tolerated and there is no interactive action with other medications, food and alcohol. This can be prescribed by physicians to patients with psychogenic and a mild organic impotence. It is also used when PDE-5 inhibitors are contraindicated. VCDs are better accepted by older patients especially who have a stable partner. Penile pain, numbness and delayed ejaculation are some of the side effects that treating psychiatrist need to be aware of. Psychosexual therapy is also the first line treatment and it is used in patients with significant psychological problems, though psychological component may be present in all cases of erectile dysfunction. It is used either alone or in combination with other first line therapies. The motivation of the patient is of utmost importance for any psychosexual therapy. The major advantages are that it is non-invasive, involves the partner, and leads to sustainable improvement in sexual function and satisfaction. However, it takes time, is associated with high dropout rates and is associated with variable results.
Table 21.
Management of Erectile dysfunction
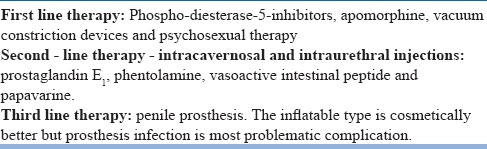
If the first line therapies fail or are contraindicated than the second line treatment includes use of intracavernosal and intraurethral injections. Patient's comfort and education is very important while using intracavernosal and intraurethral injections. Use of an automatic special pen that avoids the needle view can avoid fear of penile puncture. It is helpful in most cases of erectile dysfunction; however, it is contraindicated in patients with hypersensitivity to drug employed and priapism. Erection appears within 5-15 mins. The psychiatrist is to be aware of the side effects like priapism, penile pain and fibrosis. In cases where the penile erection lasts more than 4 mins aspiration of blood by a 19 gauge needle has been suggested. If it still does not resolve then 200mg of Phenylepherine intracavernosal injections every 5 mins is recommended. Intraurethral PGE1 as semisolid pellets is a less invasive procedure but success rates are lower. In case both first and second line therapies fail, use of inflatable penile prosthesis can be considered.
Premature Ejaculation (PME)
Specific Non Pharmacological for specific sexual dysfunctions
It is considered that behavioural management is to be the first line of therapy where ever possible. The specific behavioural techniques for PME involves stop- start or squeeze techniques, which are usually introduced during genital sensate focus.
The stop-start technique developed by Masters and Johnson is highly effective for the treatment of premature ejaculation with success rates of as high as 90%. The technique aims to increase the frequency of sexual contact and sensory threshold of the penis. It is best carried out in the context of sensate focus exercises because some males ejaculate so early that direct stimulation of the penis of any kind can trigger ejaculation straight away. Starting with non-genital caresses allows the male more time to identify the sensations that occur immediately prior to ejaculation. The stop-start technique consists of the man lying on his back and focusing his attention fully on the sensation provided by the partner's stimulation of his penis. When he feels himself becoming highly aroused he is to indicate this to her in pre-arranged manner at which point she need to stop caressing and allow his arousal to subside. After a short delay this procedure is repeated twice more, following which the woman stimulates her partner to ejaculation. At first the man may find himself ejaculating too early, but usually gradually develops control. Later a lotion can be applied to the man's penis during this procedure, which will increase his arousal and make genital stimulation more like vaginal containment.
The squeeze technique is an elaboration of the stop-start technique, and probably only needs to be used if the latter proves ineffective. The couple proceeds as with the stop-start procedure. When the man indicates he is becoming highly aroused his partner should apply a firm squeeze to his penis for about 15-20 seconds. During applying the pressure, the forefinger and middle finger are placed over the base of the glans and shaft of the penis, on the upper surface of the penis, with the thumb placed at the base of the undersurface of the glans. This inhibits the ejaculatory reflex. As with the stop-start technique this is repeated three times in a session and on the fourth occasion the man may ejaculate.
Both procedures appear to help a man develop more control over ejaculation, perhaps because he gradually acquires the cognitive techniques associated with ejaculatory control, or perhaps because he gradually becomes accustomed to experiencing sexual arousal without getting anxious (Hawton, 1989). Stop-Start technique and Squeeze technique have been documented to have anywhere between 60-95% success rates.
Pharmacological management of Premature Ejaculation (PME)
Pharmacological treatment of premature ejaculation includes use of topical anesthetic agent, tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs) (Table-22). There is preliminary data for use of sildenafil and some of the Chinese herbs. However, it is important to note that none of these agents have been approved.
Table 22.
Treatment options for premature ejaculation
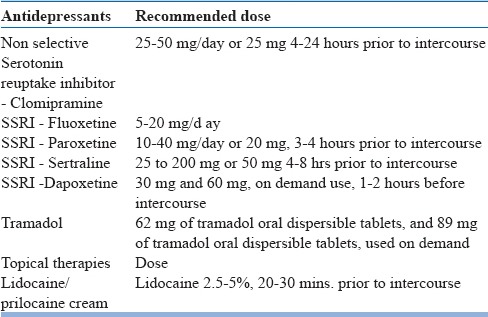
Over the last few years, dapoxetine, another non-selective SSRI, has been marketed specifically for management of PME. Dapoxetine has been found to be efficacious in both lifelong and acquired PME. Dapoxetine is associated with side effects like nausea, diarrhoea, headache and dizziness. Combining dapoxetine with PDE-5 inhibitors is associated with increased risk of syncope. It is generally recommended that patient's blood pressure is to be evaluated prior to starting of dapoxetine.
Among the SSRIs, paroxetine has been found to be useful. However, data also exist for the beneficial effect of sertraline. Studies which have compared various SSRIs suggest that paroxetine is superior to fluoxetine, clomipramine and sertraline. Data also suggest that sertraline is better than fluoxetine; however, the efficacy of clomipramine is not significantly different from fluoxetine and sertraline.
Chinese herbs like S-S cream, which are used as topical agents, have claimed good efficacy and favorable side effect profile.
PDE-5 inhibitors have also been evaluated for management of PME. Some of the available data suggests that using combination of SSRIs and PDE-5 inhibitors leads to better outcome than use of SSRIs alone.
SSRIs can be used on continuous basis or on situation basis, i.e. pre-intercourse. It is unclear as which of the two is more effective. There is no clear consensus as to whether SSRIs will effect an eventual cure of PME allowing for discontinuation of the medication, or whether SSRIs will be required for life. The general consensus is that PME usually returns upon discontinuation of therapy.
Steps in management of Premature Ejaculation (PME)
Firstly, the diagnosis of premature ejaculation be made as per the prevalent nosological system. The working diagnosis of PME is made if ejaculation occurs sooner than desired either before or soon after penetration causing distress to either or both partner for more than 3 months. The general principles of management are shown in Table-23.
Table 23.
General principles of evaluation of premature ejaculation
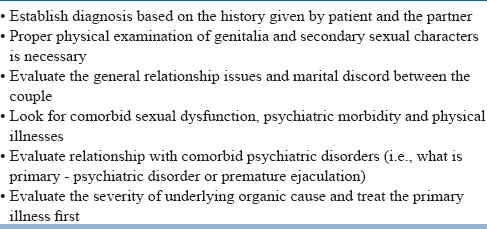
The general guideline for selection of mode of treatment is given in figure-4. The first step for treatment involves evaluation for presence of comorbid sexual dysfunctions, comorbid psychiatric disorders and marital discord. If patient has erectile dysfunction or Dhat syndrome along with PME, these is to be addressed first. If patient has a psychiatric disorder it needs to be carefully evaluated – is it primary or secondary to sexual dysfunction, and how severe it is. If the psychiatric comorbidity is primary and/or severe, it is to be addressed first. Sometimes the PME is secondary to the poor interpersonal relationship between the couple, so it needs to be addressed prior to treatment of PME.
Figure 4.
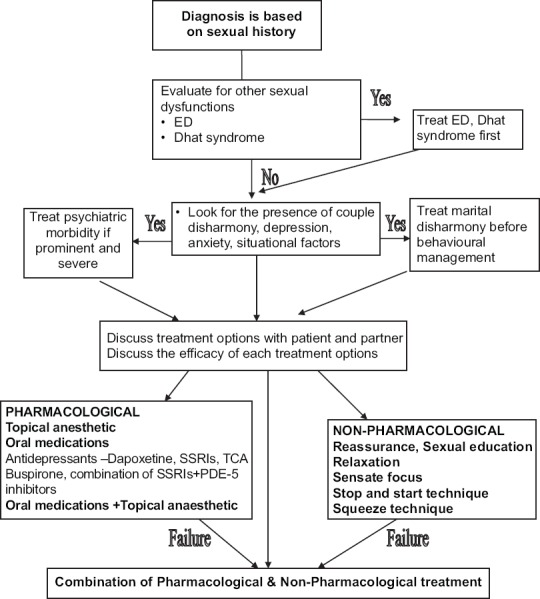
Guidelines for Premature ejaculation
Initial treatment involves providing sex education, clarifying the myths, relaxation and correction of situational factors (if present) contributing/causing the dysfunction and following the sensate focus training. It is considered that behavioural management is the first line of therapy wherever possible. But some authors suggest that men with lifelong premature ejaculation need to be managed with a combination of pharmacotherapy and behavioural management, while those with acquired or situational PME can be treated with pharmacotherapy and/or behavioral therapy according to patient/partner preference. The specific behavioural techniques for PME involves stop- start or squeeze techniques, which are usually introduced during genital sensate focus. The pharmacotherapy involves use of Dapoxetine, SSRIs, TCAs, Buspirone and topical agents. If either of the therapeutic measure fails then a combination of both may be tried. Combination of SSRIs and PDE-5 inhibitors has also been reported to lead to better outcome than use of SSRIs alone.
Selection of specific treatment modality is to be made based on physician judgment and patient's informed choice. The primary outcome measure is to be the patient's and partner satisfaction.
Risk and benefits of all treatment options are to be discussed with patient prior to any intervention.
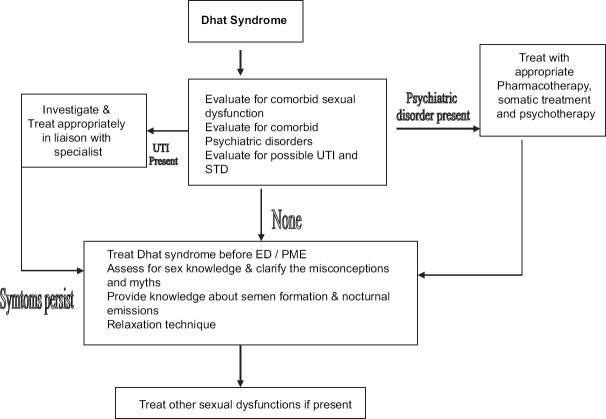
Dhat syndrome
The first step in the management of Dhat syndrome involves evaluation for comorbid sexual dysfunctions, psychiatric disorders and presence of possible urinary tract infection (UTI) and sexually transmitted diseases (STD). Where ever there is a suspicion, local examination, appropriate investigations for infective pathology and phosphaturia need to be done and adequate treatment is to be provided. Even after appropriate treatment, if the symptoms persist then the subject is to be provided adequate sexual knowledge.
Whenever patient has comorbid Dhat syndrome along with PME or ED, Dhat syndrome is to be treated first. If the psychiatric comorbidity is primary and/or severe, it need to be addressed first (See figure-5).
Figure 5.
Treatment Algorithm of Dhat syndrome
The most important aspect of treatment of Dhat syndrome is providing adequate sex knowledge and clarifying sexual myths. Sex education mainly focuses on anatomy and physiology of sexual organs and their functioning with reference to masturbation, semen formation, nocturnal emissions and their functioning with genitourinary system independent of gastro-intestinal tract etc. If there is the presence of associated anxiety or depressive symptoms that impede the process of therapy, anxiolytics or/and antidepressants can be added for the least possible time and in the least possible doses.
Impaired sexual interest in men or women:
Besides the general measures, no particular procedures are used in the treatment of this problem. The main emphasis is on setting the right circumstances for sexual activity, reducing anxiety, establishing satisfactory fore play, focusing attention on erotic stimuli and cognitions and resolving the general issues of relationship between the couple. It is generally agreed that desire disorders have a substantially poorer response to psychotherapy (<50%) than other forms of sexual dysfunction (≥ 70%). In addition, therapy tends to be more difficult and the conventional sex therapy techniques (e.g., sensate focus) are generally inadequate. Hence, a more flexible and person centric approach to treatment is required. Many authors have tried approaches like cognitive-behavioral therapy, systems approach, script modification, clinical hypnosis, guided fantasy exercises, and sexual assertiveness training. Cognitive-behavioral therapy emphasizes the role of thoughts and beliefs in perpetuating the maladaptive behavior and is useful when beliefs held by the patient or couple about norms or responses is contributing to the sexual problem. The “systems” approach, targets dynamics between the couple and allows assessing the extent to which sexual dysfunction is used by the couple to maintain a “sexual equilibrium” within the relationship (i.e., the way sexual dysfunction is used to regulate intimacy or to allow the share of blame between partners for the failure of the relationship).
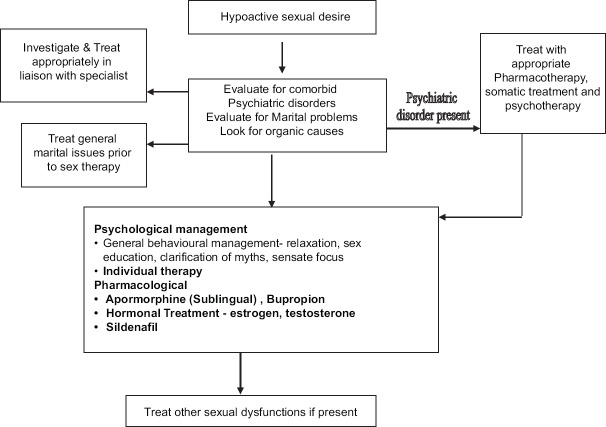
Steps in the management of impaired sexual interest in men or women:
The most important issue in management is evaluation for the organic factors, evaluation for presence of comorbid psychiatric conditions, comorbid sexual dysfunction and marital disharmony. But it is to be remembered that although the cause may be organic, psychological causes can decrease the sexual interest, these also need to be focused adequately. Many couples have marital disharmony associated with decrease sexual interest and treating the same would be the only thing which is required.
Besides the general measures, no particular procedures are used in the treatment of this problem. The main emphasis is on setting the right circumstances for sexual activity, reducing anxiety, establishing satisfactory fore play, focusing attention on erotic stimuli and cognitions and resolving the general issues of relationship between the couple. More flexible and individualistic approach to treatment is required. The general outline of management is shown in figure-6.
Figure 6.
Treatment Algorithm of Hypoactive sexual desire
Female sexual Dysfunction
Formulation of a treatment plan
Firstly female sexual disorders need to be diagnosed as per the current definitions. Initial treatment planning requires a thorough assessment of the patient, with the goals of support, normalization, permission giving, sex education, stress reduction, symptom alleviation, improve communication skills (sexual & others) and attitude change. The thorough assessment includes a comprehensive medical and psychological history of the patient and her partner. Like in male sexual dysfunction, psychiatrist treating female sexual dysfunction is to be aware of the etiology including genitourinary, endocrinological, vascular and neurological systems. The general principles of assessment of female patients with sexual dysfunction are given in Table-24. A multidisciplinary approach is of paramount importance in female sexual dysfunction.
Table 24.
General principles of evaluation of female sexual dysfunction
Vaginismus
It is important to remember that many women who present with vaginismus have negative attitude towards sex and quite a few are victim of sexual assault. Some may also have the belief that premarital sex is wrong or sinful. This belief may be so ingrained that, even when intercourse is sanctioned by marriage, it may be difficult to relax physically or mentally during sexual intercourse. Some times the cause of vaginismus may be a fear that is instilled by friends or family by suggesting that the first experience of intercourse is likely to be painful or bloody. Another important cause of vaginismus is fear of pregnancy.
The sex education needs to focus on clarifying normal sexuality and reducing negative attitude for sex. Besides the use of general relaxation exercises, the relaxation procedure also needs to focus on teaching the women to relax muscles around the inner thigh and pelvic area.
The specific management involves the following stages:
Helping the woman develop more positive attitudes towards her genitals. After fully describing the female sexual anatomy, the therapist need to encourage the woman to examine herself with a hand mirror on several occasions. Extremely negative attitudes (especially concerning the appearance of the genitals, or the desirability of examining them) may become apparent during this stage, possibly leading to failure to carry out the homework. Some women find it easier to examine themselves in the presence of the partners; others may only get started if the therapist helps them do this first in the clinic. If this is necessary a medically qualified female therapist is to be involved.
Pelvic muscle exercises. These are intended to help the woman gain some control over the muscles surrounding the entrance to the vagina. If she is unsure whether or not she can contract her vaginal muscles she may be asked to try to stop the flow of urine when she next goes to the toilet. The woman can later check that she is using the correct muscles by placing her finger at the entrance to her vagina where she need to be able to feel the muscle contractions. Subsequently she is advised to practice firmly contracting these muscles for an agreed number of times (e.g. 10) several times a day.
Vaginal penetration. Once the woman has become comfortable with her external genital anatomy she is advised to explore the inside of her vagina with her fingers. This is partly to encourage familiarity and partly to initiate vaginal penetration. Negative attitudes may also become apparent at this stage (e.g. concerning the texture of the vagina, its cleanliness, fear of causing damage, and whether it is ‘right’ to do this sort of thing). The rationale for any of these objections is to be explored. At a later stage the woman might try using two fingers and moving them around. Once she is comfortable inserting a finger herself, her partner need to begin to do this under her guidance during their homework sessions. A lotion (e.g. K-Y or baby lotion) can make this easier. Graded vaginal dilators can be used. However, clinical experience has shown that the use of fingers is just as effective.
Vaginal containment. When vaginal containment is attempted the pelvic muscle exercises and the lotion are used to assist in relaxing the vaginal muscles and making penetration easier. This is often a difficult stage and the therapist therefore needs to encourage the woman to gain confidence from all the progress made so far. Persisting concerns about possible pain may need to be explored, including how the woman might ensure that she retains control during this stage.
Movements during containment: Once containment is well established the couple is asked to introduce movement during containment, with preferably women starting the movements first. With this the general programme of sex therapy is completed and now the treatment needs to include superimposition of treatment for specific sexual dysfunctions.
Steps in the management of vaginismus: Treatment is to be individualized for each woman and/or partner, whenever possible with their input. Psychological issues as well as interpersonal issues need to be addressed first. The sex education needs to focus on clarifying normal sexuality and reducing negative attitude for sex. Besides the use of general relaxation exercises, the relaxation procedure needs to focus on teaching the women to relax muscles around the inner thigh and pelvic area. The specific behavioural management is to be followed.
Dyspareunia
Besides the general measures and sensate focus, treatment of dyspareunia involves sex education. The sex education need to focus on the importance of adequate arousal and the couple may also be helped by specific suggestions for modifying their usual intercourse positions. Couple may be helped by avoiding positions that lead to deep penetration (such as vaginal entry from the rear) and by adopting positions in which the woman is in control of the depth of penetration (woman on top) or in which penetration is not too deep (side by side or ‘spoons’ position). Another important aspect of treatment of dyspareunia due to psychological causes is helping the woman become aroused by teaching the sensate focus programme.
In woman with repeated pain experience on intercourse, it is likely that they will tense up on future occasions in anticipation of further pain. Such tension may actually increase pain as the muscles may be more resistant to penetration. Due to this, relaxation exercises prior to or during intercourse may be helpful. Progressive muscle relaxation prior to sexual activity may allow the women to reduce the body tension, while more specific relaxation exercises just prior to intercourse may help to relax the muscles around the pelvic region and may enhance arousal. As a woman acquires a number of coping techniques for minimising the likelihood of pain, positive self-talk may be helpful. Such self-talk can involve the woman reminding herself that she is in control of the situation and she will be the one to determine when penetration is to occur and how deep penetration will be.
Steps in the management of Dyspareunia: As with most of the other sexual dysfunctions, the first step is to rule out other causes/factors that can cause pain. Also the assessment needs to rule out vaginismus and dryness of vagina. Treatment of dyspareunia includes sex education and teaching sensate focus (Figure-7). In particular, it may be helpful for the couple to avoid deep penetration positions (such as vaginal entry from the rear) and to assume positions in which the woman is in control of the depth of penetration (woman on top) or in which penetration is not too deep (side by side or ‘spoons’ position).
Figure 7.
Treatment Algorithm of Dyspareunia
Arousal disorder
It is very important to rule out comorbid desire disorders before treating arousal disorders. If there is comorbid desire disorder then it needs to be treated first before arousal disorders are treated. There is no empirically validated treatment available for arousal disorders due to the fact that this is a less researched area. Approach usually depends on the etiology of the arousal disorders. Sensate focusing, CBT, systematic desensitization, individual and couples therapy, directed masturbation and communication skills have been tried in arousal disorders with moderate results.
Desire disorders
Assessment regarding whether primary or secondary needs to be settled. Also, whether the desire disorder is generalized or partner specific needs to be explored. Although empirically validated non-pharmacological treatments are not available yet, individual/couples therapy and medical/ psychological treatment have been tried in desire disorders in females. In recent times, a pharmacological agent, flibanserin has been approved for the management of hypoactive sexual desire disorder in premenopausal women. The recommended dose0 is 100 mg per day at bed time. Data from metanalysis shows that compared to placebo, flibanserin is associated with higher satisfying sexual events per month. Its use is associated with side effects like dizziness, somnolence, nausea, and fatigue. If a patient does not show improvement, the drug needs to be discontinued after 8 weeks.
Aversion disorders
Sexual abuse or rape, trauma, relationship problem, marital problem can lead to sexual aversion disorder. Therefore, all clinicians treating sexual aversion disorders need to be aware of these causes. In Aversion disorders also no empirically validated treatment is available however the clinicians usually employ couple / individual therapy.
Termination of treatment
The termination of the treatment must be planned carefully. The various strategies and component of termination are:
Prepare for termination from the start of treatment: The patient/couple should be told about the likely duration of therapy at the beginning of the treatment. Setting the time frame will encourage the patient/couple to work on the homework assignments.
Towards the end of treatment extend the intervals between sessions: The intervals between the last two to three sessions need to be extended to two to three weeks.
Prepare for relapse: The therapist need to prepare the couple for relapse. About three-fourth of men will experience recurrence of their problem following treatment. Hence, treatment also needs to assist men to cope well with relapse. Most recurrences occur in a temporal pattern (i.e., will occur more at certain times than at others) and usually improve naturally or with self-initiated restart of treatment techniques. The understanding that relapses are normal expected helps to reduce the anxiety and sense of failure that may otherwise prolong erectile difficulties.
Follow-up assessments: Follow-up assignments help the therapist to evaluate the short-term effectiveness of treatment.
SUGGESTED READING
- 1.Abdel Hamid IA, El Naggar EA, ElGilany AH. Assessment of as needed use of pharmacotherapy and pause-squeeze technique in premature ejaculation. International Journal of Impotence Research. 2001;13:41–45. doi: 10.1038/sj.ijir.3900630. [DOI] [PubMed] [Google Scholar]
- 2.Abdel Hamid IA. Phosphodiesterase 5 inhibitors in rapid ejaculation: potential use and possible mechanisms of action. Drugs. 2004;64:13–26. doi: 10.2165/00003495-200464010-00002. [DOI] [PubMed] [Google Scholar]
- 3.Alberta Medical Association. The Guidelines for the Investigation and Management of Erectile Dysfunction. 2005 [Google Scholar]
- 4.Alberta Medical Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- 5.Anastasiadis AG, Salomon L, Ghafar MA, Burchardt M, Shabsigh R. Female sexual dysfunction: State of the art. Curr Urol Rep. 2002;3:484–91. doi: 10.1007/s11934-002-0102-8. [DOI] [PubMed] [Google Scholar]
- 6.Asimakopoulos AD, Miano R, Finazzi Agrò E, Vespasiani G, Spera E. Does current scientific and clinical evidence support the use of phosphodiesterase type 5 inhibitors for the treatment of premature ejaculation? A systematic review and meta-analysis. J Sex Med. 2012;9:2404–16. doi: 10.1111/j.1743-6109.2011.02628.x. [DOI] [PubMed] [Google Scholar]
- 7.Avasthi A, Gupta N. Manual for standardized Management of Single males with sexual Disorders. Marital and Psychosexual Clinic, Department of Psychiatry, PGIMER, Chandigarh. 2002 [Google Scholar]
- 8.Avasthi A, Rao TSS, Grover S, Biswas PS, Kumar S. Shiv Gautam, Ajit Avasthi, editors. Indian Psychiatric Society: Clinical Practice Guidelines for management of sexual dysfunctions. Published by Indian Psychiatric Society. 2006;II:144–231. [Google Scholar]
- 9.Avasthi AK, Varma VK, Nehra R, Das K. Construction and standardization of a sex knowledge and attitude questionnaire (SKAQ) in simple Hindi, for North Indian population. Indian Journal of Psychiatry. 1992;34:24–27. [PMC free article] [PubMed] [Google Scholar]
- 10.Bai Y, Pu C, Han P, Li J, Yuan H, Tang Y, Wang X, Wei Q. Selective Serotonin Reuptake Inhibitors Plus Phosphodiesterase-5 Inhibitors for Premature Ejaculation: A Systematic Review and Meta-analysis. Urology. 2015;86:758–64. doi: 10.1016/j.urology.2015.06.045. [DOI] [PubMed] [Google Scholar]
- 11.Choi HK, Jung GW, Moon KH, Xin ZC, Choi YD, Lee WH, Rha KH, Choi YJ, Kim DK. Clinical study of S-S cream in patients with lifelong premature ejaculation. Urology. 2000;55:257–261. doi: 10.1016/s0090-4295(99)00415-x. [DOI] [PubMed] [Google Scholar]
- 12.Cooper K, Martyn-St James M, Kaltenthaler E, Dickinson K, Cantrell A. Interventions to treat premature ejaculation: a systematic review short report. Health Technol Assess. 2015;19:1–180. doi: 10.3310/hta19210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grover S, Avasthi A, Aneja J, Gauri Shankar Ravi Mohan M, Nehra R, Padhy S. Comprehensive Questionnaire for assessment of Dhat syndrome: development and use in patient population. J Sexual Medicine. 2014;11:2485–95. doi: 10.1111/jsm.12241. [DOI] [PubMed] [Google Scholar]
- 14.Grover S, Avasthi A, Gupta S, Dan A, Neogi R, Behere PB, Lakdawala B, Tripathi A, Chakraborty K, Sinha V, Bhatia MS, Pattojoshi A, Rao TS, Rozatkar A. Comorbidity in patients with dhat syndrome: a nationwide multicentric study. J Sex Med. 2015;12:1398–401. doi: 10.1111/jsm.12899. [DOI] [PubMed] [Google Scholar]
- 15.Grover S, Avasthi A, Gupta S, Dan A, Neogi R, Behere PB, Lakdawala B, Tripathi A, Chakraborty K, Sinha V, Bhatia MS, Pattojoshi A, Rao TS, Rozatkar A. Phenomenology and beliefs of patients with Dhat syndrome: A Nationwide multicentric study. Int J Soc Psychiatry. 2016;62:57–66. doi: 10.1177/0020764015591857. [DOI] [PubMed] [Google Scholar]
- 16.Grover S, Avasthi A, Gupta S, Hazari N, Malhotra N. Do female patients with nonpathological vaginal discharge need the same evaluation as for Dhat syndrome in males? Indian J Psychiatry. 2016;58:61–9. doi: 10.4103/0019-5545.174376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grover S, Kate N, Avasthi A, Rajpal N, Umamaheswari V. Do females too suffer from Dhat syndrome: a case series and revisit of the concept?Indian J Psychiatry. 2014;56:388–392. doi: 10.4103/0019-5545.146537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatzichristou D, Rosen RC, Broderick G, Clayton A, Cuzin B, Derogatis L, Litwin M, Meuleman E, O’Leary M, Quirk F, Sadovsky R, Seftel A. Clinical evaluation and management strategy for sexual dysfunction in men and women. Journal of Sexual Medicine. 2004;1:49–57. doi: 10.1111/j.1743-6109.2004.10108.x. [DOI] [PubMed] [Google Scholar]
- 19.Hatzichristou DG, Hatzimouratidis K, Bekas M, Apostolidis A, Tzortzis V, Yannakoyorgos K. The diagnostic steps in the evaluation of patients with erectile dysfunction. J Urol. 2002;168:615–20. [PubMed] [Google Scholar]
- 20.Hatzimouratidis K, Eardley I, Giuliano F, Hatzichristou D, Moncada I, Salonia A, Vardi Y, Wespes E. Guidelines on Male Sexual Dysfunction: Erectile dysfunction and premature ejaculation. European Association of Urology Web site. http: //uroweb.org/guideline/male-sexual-dysfunction/. Updated 2015. [DOI] [PubMed]
- 21.Hawton K. Sex therapy: A Practical guide. New York: Oxford University Press; 1985. [Google Scholar]
- 22.Hawton K. Sexual dysfunctions. In: Hawton K, Salkovskis P M, Kirk J, Clerk D M, editors. Cognitive Behaviour Therapy for Psychiatric Problems A Practical Guide. New York: Oxford University Press; 1989. [Google Scholar]
- 23.Hoy SM, Scott LJ. Dapoxetine: in premature ejaculation. Drugs. 2010;70:1433–43. doi: 10.2165/11204750-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 24.Hutchinson K, Cruickshank K, Wylie K. A benefit-risk assessment of dapoxetine in the treatment of premature ejaculation. Drug Saf. 2012;35(5):359–72. doi: 10.2165/11598150-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Jaspers L, Feys F, Bramer WM, Franco OH, Leusink P, Laan ET. Efficacy and Safety of Flibanserin for the Treatment of Hypoactive Sexual Desire Disorder in Women: A Systematic Review and Meta-analysis. JAMA Intern Med. 2016;176:453–62. doi: 10.1001/jamainternmed.2015.8565. [DOI] [PubMed] [Google Scholar]
- 26.Markou S, Perimenis P, Gyftopoulos K, Athanasopoulos A, Barbalias G. Vardenafil (Levitra) for erectile dysfunction: a systematic review and meta-analysis of clinical trial reports. International Journal of Impotence Research. 2004;16:470–8. doi: 10.1038/sj.ijir.3901258. [DOI] [PubMed] [Google Scholar]
- 27.Masters WH, Johnson V. Human Sexual Inadequecy. London: Churchill; 1970. [Google Scholar]
- 28.Masters WH, Johnson V. Human Sexual Response. Boston: Little, Brown & Co; 1966. [Google Scholar]
- 29.McMahon CG. Dapoxetine for premature ejaculation. Expert Opin Pharmacother. 2010;11:1741–52. doi: 10.1517/14656566.2010.493174. [DOI] [PubMed] [Google Scholar]
- 30.Men C, Yu L, Yuan H, Cui Y. Efficacy and safety of phosphodiesterase type 5 inhibitors on primary premature ejaculation in men receiving selective serotonin reuptake inhibitors therapy: a systematic review and meta-analysis. Andrologia. 2016 Jan 21; doi: 10.1111/and.12540. doi: 10.1111/and.12540. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 31.Rosen C. Prevalence and risk factors of sexual dysfunction in men and women. Curr Psychiatry Rep. 2000;2:189–95. doi: 10.1007/s11920-996-0006-2. [DOI] [PubMed] [Google Scholar]
- 32.Smith-Harrison LI, Patel A, Smith RP. The devil is in the details: An analysis of the subtleties between phosphodiesterase inhibitors for erectile dysfunction. Transl Androl Urol. 2016;5:181–6. doi: 10.21037/tau.2016.03.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for Research. Geneva: World health organization; 1993. [Google Scholar]