Abstract
Introduction
To confirm the safety and feasibility of single-incision laparoscopically assisted appendectomy (SILA) performed by resident doctors.
Materials and methods
We retrospectively analyzed 86 consecutive patients who underwent SILA between August 2010 and August 2016 at Kinki Central Hospital. During this period, 9 residents and 6 board-certified attending surgeons performed SILA. Data on the patients' characteristics and perioperative complications were collected from their medical records.
Results
Resident doctors operated on 55% (47/86) of patients undergoing SILA. There were no significant differences between the groups with regard to patient characteristics. Mean operative time in the resident and staff surgeon groups was 74 min and 71 min, respectively (p = 0.5). Median blood loss in both the resident and staff surgeon groups was 0 mL (p = 0.3). The rate of conversion to a different operative procedure was 4% (2/47) in the resident group and 3% (1/39) in the staff surgeon group (p = 1). All three above-mentioned procedures, two (4%, 2/47) in the resident group and one (3%, 1/39) in the staff surgeon group, were converted to multi-port laparoscopic appendectomy. The mean postoperative hospital stay was 5 days for both the resident and staff surgeon groups (p = 0.7). Perioperative complications developed in 9% (4/47) of the patients in the resident group and 21% (8/39) of the patients in the staff surgeon group (p = 0.1).
Conclusions
SILA performed by residents under the guidance of a staff surgeon is safe and feasible.
Keywords: Appendectomy, Single-incision laparoscopically assisted appendectomy (SILA), Single-incision laparoscopic surgery (SILS), Surgical education
Highlights
-
•
Single-incision laparoscopically assisted appendectomy could be performed with acceptable morbidity by the residents.
-
•
Single-incision laparoscopically assisted appendectomy performed by residents under the guidance of a staff surgeon is safe and feasible.
1. Introduction
Appendectomy is one of the most commonly performed general surgical procedures. In recent years, laparoscopic appendectomy has been widely performed, and gradually, single-incision laparoscopically assisted appendectomy (SILA) has been implemented as a procedure with more favorable cosmetic outcomes than conventional laparoscopic appendectomy. However, resident training in single-incision laparoscopic surgery (SILS) techniques has been limited because of the specific difficulties of SILS, such as in-line positioning of the laparoscope, close proximity of the working instruments with limited triangulation, and limited range of motion of the laparoscope and instruments. Although there are some previous reports regarding resident training for conventional laparoscopic appendectomy [1], [2], [3], there are few reports regarding resident training for SILA [4], [5]. The aim of the present study was to evaluate the safety and feasibility of resident doctor-performed SILA, by comparing the outcomes with those of procedures performed by staff doctors.
2. Materials and methods
2.1. Study design
This study was designed as a single institution, retrospective case series [6]. This study was in accordance with the ethical standards of the institution and the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh 2000). Written informed consent was obtained from the patients for the information to be included in our manuscript.
2.2. Clinical settings
We retrospectively analyzed 86 consecutive patients who underwent SILA between August 2010 and August 2016 at Kinki Central Hospital. Appendicitis was diagnosed based on physical findings, blood tests, abdominal ultrasonography and CT scan.
2.3. Patients and surgeons
During the study period, 9 residents and 6 board-certified attending surgeons performed SILA. The staff surgeons in this study had completed fellowship training in advanced surgical techniques and had been routinely performing laparoscopic procedures. The resident doctors in the study were years 3–6 postgraduates. All SILAs performed by the residents were performed under the guidance of fully trained staff surgeons. The staff doctors were scrubbed in as camera operators and verbally directing the residents if necessary when the resident doctors performed SILAs.
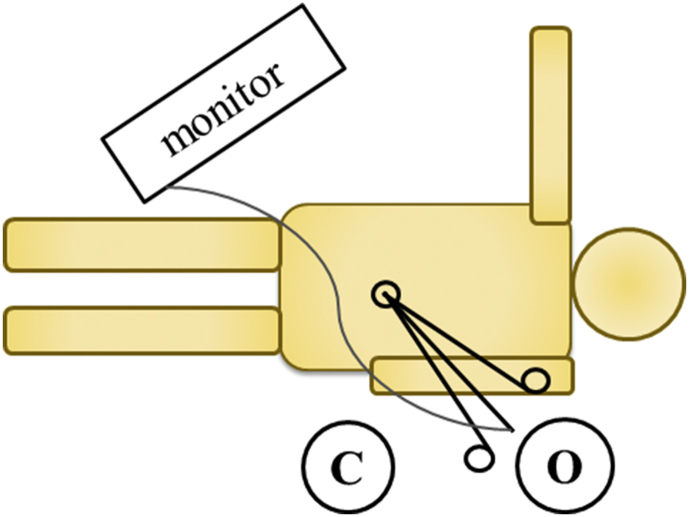
2.4. Surgical technique
Fig. 1 shows the operative settings. The skin incision was made intraumbilically. A single access system enclosing three working channels was introduced into the abdominal cavity via an incision in the muscular aponeurosis under visual control. Depending on the operating surgeon's choice and hospital supplies, several types of single access systems were used in this study, including: EZ access and Lap-Protector, Hakko Co., Ltd., Nagano, Japan; SILS™, Covidien, Dublin, Ireland; and a surgical-glove technique that involves the use of a small plastic wound retractor inserted transumbilically with an attached surgical glove to prevent CO2 leakage, with the fingers functioning as multiple ports. Typically, we used EZ access on the Lap Protector for insertion of trocars for the 5-mm flexible scope and instruments during the operations (Fig. 2). A carbon dioxide pneumoperitoneum was then created, and the pressure was maintained at 10 mmHg. After the operating table was positioned, the ileocecum was mobilized with conventional straight forceps and laparoscopic coagulation shears. The appendix or mesoappendix was grasped, and the pneumoperitoneum was deflated. The appendix was then delivered through the umbilical wound. In the extracorporeal portion of the procedure, the appendix and mesoappendix were dissected and ligated extracorporeally. The stump of the appendix was inverted with a purse-string suture, as in open appendectomy. Depending on the operating surgeon's choice and the surgical field, Endo GIA™ Universal Stapling System, Covidien, Dublin, Ireland, was used to resect the appendix intraperitoneally instead of the extracorporeal procedure. Drains were placed as required. The umbilical wound was closed in two layers in a routine fashion (Fig. 3).
Fig. 1.
Operative settings for SILA. O: operator, C: camera operator.
Fig. 2.
The three ports secured to the EZ access for the operation.
Fig. 3.
Postoperative scar.
2.5. Data collection
Data on the patients' age, sex, body mass index (BMI), American Society of Anesthesiologists-physical status (ASA-PS) grade, previous history of abdominal surgery, presence of a fecolith or abscess, operative time, blood loss, conversion rate, postoperative hospital stay, and perioperative complications were collected from their medical records. All patients were followed up at least until the day of discharge. When comparing resident-performed and staff surgeon-performed SILAs, the rates of appendicitis complicated by gangrenous appendicitis or perforation of the appendix were also evaluated, in addition to the baseline demographic data.
2.6. Statistical analysis
Student's t-test, Fisher's exact probability test, and the Mann-Whitney U test were used for analysis of parametric and non-parametric data, as appropriate. Differences of p < 0.05 were considered significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The Foundation for Statistical Computing). More precisely, it is a modified version of R commander, designed to add statistical functions frequently used in biostatistics [7].
3. Results
Table 1 lists the characteristics of the patients in each group. The resident doctors operated on 55% (47/86) of patients undergoing SILA at our hospital. There were no significant differences between the groups with regard to patient age, sex, BMI, ASA-PS grade, previous history of abdominal surgery, presence of a fecolith or abscess, and the rate of complicated appendicitis.
Table 1.
Patients' characteristics.
| Residents (N = 47) | Staff surgeons (N = 39) | p value | |
|---|---|---|---|
| Mean age, years (range) | 34 (9–80) | 37 (9–86) | 0.7 |
| Male sex (%) | 19 (40) | 16 (41) | 1 |
| Mean BMI, kg/m2 (range) | 21 (14–28) | 21 (16–34) | 1 |
| ASA-PS grade ≥ 3 (%) | 0 | 1 (3) | 0.5 |
| Previous history of abdominal surgery (%) | 2 (4) | 2 (5) | 1 |
| Abscess (%) | 6 (13) | 7 (18) | 0.6 |
| Fecolith (%) | 16 (34) | 13 (33) | 1 |
| Complicated appendicitis (%) | 13 (28) | 13 (33) | 0.6 |
BMI, body mass index.
ASA-PS, American Society of Anesthesiologists physical status.
Table 2 shows the perioperative data of the patients undergoing SILA in each group. This study included 6 cases (13%, 6/47) in the resident group and 6 cases (15%, 6/39) in the staff surgeon group operated by single-incision laparoscopic appendectomy. Mean operative time in the resident and staff surgeon groups was 74 min (range 25–166 min) and 71 min (range 36–160 min), respectively (p = 0.5). Median blood loss in the resident and staff surgeon groups was the same, at 0 mL (range 0–50 mL and 0–63 mL, respectively) (p = 0.3). The rate of conversion to a different operative procedure was 4% (2/47) in the resident group and 3% (1/39) in the staff surgeon group (p = 1), all three procedures being converted to multi-port laparoscopic appendectomy. The mean postoperative hospital stay was 5 days (range 2–8 days) in the resident group and 5 days (range 3–15 days) in the staff surgeon group (p = 0.7). Perioperative complications developed in 9% (4/47) of the patients in the resident group and 21% (8/39) of the patients in the staff surgeon group (p = 0.1). A wound infection developed in 2% (1/47) of the patients in the resident group and 18% (7/39) of those in the staff-surgeon group (p < 0.05), while an intraabdominal abscess developed in 4% (2/47) of the patients in the resident group and 3% (1/39) of those in the staff-surgeon group (p = 0.1). Pseudomembranous colitis developed in 2% (1/47) of the patients in the resident group (p = 0.7). No other major complications, such as other organ injury, were noted in either group.
Table 2.
Perioperative data for single-incision laparoscopically assisted appendectomy cases.
| Residents (N = 47) | Staff surgeons (N = 39) | p value | |
|---|---|---|---|
| Single-incision laparoscopically assisted appendectomy (%) | 41 (87) | 33 (85) | 0.8 |
| Mean operative time, min (range) | 74 (25–166) | 71 (36–160) | 0.5 |
| Median blood loss, mL (range) | 0 (0–50) | 0 (0–63) | 0.3 |
| Conversion rate, total (%) | 2 (4) | 1 (3) | 1 |
| Multi-port surgery (%) | 2 (4) | 1 (3) | 1 |
| Open surgery (%) | 0 | 0 | 1 |
| Mean postoperative hospital stay, days (range) | 5 (2–8) | 5 (3–15) | 0.7 |
| Complications, total (%) | 4 (9) | 8 (21) | 0.1 |
| Wound infection (%) | 1 (2) | 7 (18) | <0.05 |
| Intra-abdominal abscess (%) | 2 (4) | 1 (3) | 1 |
| Pseudomembranous colitis (%) | 1 (2) | 0 | 1 |
4. Discussion
In this study, there were two important clinical observations. First, operative time and conversion rate of SILAs performed by resident doctors were comparable to those performed by staff surgeons. Second, SILA could be performed with acceptable morbidity by the residents.
First, the operative time and conversion rates of SILAs performed by resident doctors were comparable to those in procedures performed by staff surgeons. A number of studies have reported that operative times tend to be longer with the participation of residents, which is contrary to the results of this study [8]. The conversion rate for surgeries performed by the residents was 4%, which is comparable to that reported in previous literature (Table 3) [1], [2], [3], [4], [5]. Furthermore, there were no conversions to open surgery in this study. This might be explained by the fact that all teaching procedures were overseen by experienced laparoscopic surgeons, and, therefore, intraoperative complications with the potential to prolong operative time and to lead to conversions could be avoided.
Table 3.
Evaluations of the feasibility and safety of laparoscopic appendectomy performed by residents.
| Author [reference] | Jaffer [1] | Perry [2] | Fahrner [3] | Wakasugi [4] | Endo [5] | Wakasugi |
|---|---|---|---|---|---|---|
| Publication year | 2008 | 2010 | 2012 | 2016 | 2016 | 2017 |
| Number of patients operated on by residents | 40 | 184 | 684 | 156 | 103 | 47 |
| Patient characteristics | ||||||
| Age, years | 24 | 36 | 32 | 38 | 32 | 34 |
| Male gender | 11 (28) | NA | 380 (55) | 89 (57) | 47 (46) | 19 (40) |
| BMI, kg/m2 | NA | NA | NA | 21 | 22 | 21 |
| ASA-PS grade ≥ 3 | NA | NA | 19 (3) | 3 (2) | NA | 0 |
| Complicated appendicitis | 19 (48) | 24 (13) | 42 (6) | 62 (40) | NA | 13 (28) |
| Surgical features | ||||||
| Approach (multi/single- port) | multi | multi | multi | single | single | single |
| Operative time, minutes | 78 | 39 | 61 | 76 | 86 | 74 |
| Mean blood loss, mL | NA | NA | NA | 16 | 23 | 2 |
| Conversion rate | 8 (20) | 4 (2) | 0 | 5 (3) | 16 (16) | 2 (4) |
| Postoperative hospital stay, days | NA | 2 | 4 | 6 | 4 | 5 |
| Complications | NA | 15 (8) | 15 (2) | 14 (9) | 5 (5) | 4 (9) |
Data are given as numbers (%), unless otherwise specified.
NA, not applicable.
Second, SILA could be performed with acceptable morbidity by the residents. In the present study, the complication rate in patients who were operated on by resident doctors was 9% (4/47), which was comparable to that in patients operated on by staff surgeons and similar to that previously reported (Table 3) [1], [2], [3], [4], [5]. Most of the complications observed in this study were wound infections, all of which were treated conservatively. The staff surgeons operated on more patients with complicated appendicitis than the residents, although the difference was not statistically significant, which might have led to the worse operative outcomes for the staff surgeons compared to the residents.
SILA performed under the guidance of an experienced staff surgeon could be recommended as a teaching procedure for residents. In general, surgical training begins with simple open procedures, such as appendectomy, hernioplasty and cholecystectomy, and progresses to more complex procedures. However, many simple open procedures have now been replaced by laparoscopic procedures, including SILS, because of their minimal invasiveness and good cosmesis [8]. This raises two issues in surgical education: (i) reduced opportunity for training in open surgical skills; and (ii) lack of a standardized approach to laparoscopic surgical training for some procedures. Wakasugi et al. reported in their studies at Osaka Police Hospital that SILS for appendectomy and hernioplasty are safe and feasible, and could be useful teaching procedures for surgical residents to perform on selected patients under the guidance of an experienced staff surgeon [4], [9]. SILA requires basic and simple skills that are used in laparoscopic surgery, and offers a good opportunity for surgical residents to put learned skills into practice.
The present study has several limitations. First, it was a single center study that was retrospective in nature. There might have been a selection bias between the SILA patients treated by the resident doctors and those treated by the staff doctors, with no strict criteria for selecting which patients were operated on by the residents and which were operated on by the staff doctors. Second, the sample size was relatively small. Third, the difference of operative outcomes of SILA between the two groups might not be detected because a simple univariate analysis was carried out in this study. Despite these limitations, we are convinced that the present analysis demonstrates that SILA is safe and feasible when performed by resident doctors, and could be a teaching procedure for them.
In conclusion, our analysis of SILA procedures performed in Kinki Central Hospital demonstrates that SILA is safe and feasible when performed by resident doctors, and would be useful as a teaching procedure for resident doctors under the guidance of an experienced staff surgeon. Further powerful randomized controlled trials or multivariable analysis might be needed to confirm the present results.
Ethical approval
This protocol for the research project were in accordance with the ethical standards of the institution and the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh 2000). Written informed consent was obtained from the patients for the information to be included in our manuscript.
Sources of funding
No sources of funding.
Author contribution
Study design: MW.
Data collection: MW, NT, YN.
Data analysis/interpretation: MW.
Paper writing: MW, SO.
Data interpretation: All.
Review: HT, KT, KN, SO.
Conflict of interest
No conflict of interest to declared.
Research registry
researchregistry1752.
Guarantor
Masaki Wakasugi.
References
- 1.Jaffer U., Cameron A.E. Laparoscopic appendectomy: a junior trainee's learning curve. JSLS. 2008;12:288–291. PMID: 18765054. [PMC free article] [PubMed] [Google Scholar]
- 2.Perry Z.H., Netz U., Mizrahi S., Lantsberg L., Kirshtein B. Laparoscopic appendectomy as an initial step in independent laparoscopic surgery by surgical residents. J. Laparoendosc. Adv. Surg. Tech. A. 2010;20:447–450. doi: 10.1089/lap.2009.0430. PMID: 20518691. [DOI] [PubMed] [Google Scholar]
- 3.Fahrner R., Schöb O. Laparoscopic appendectomy as a teaching procedure: experiences with 1,197 patients in a community hospital. Surg. Today. 2012;42:1165–1169. doi: 10.1007/s00595-012-0163-3. PMID: 22426772. [DOI] [PubMed] [Google Scholar]
- 4.Wakasugi M., Tei M., Omori T., Anno K., Mikami T., Tsukada R., Koh M., Gakuhara A., Furukawa K., Suzuki Y., Masuzawa T., Kishi K., Tanemura M., Akamatsu H. Single-incision laparoscopic surgery as a teaching procedure: a single-center experience of more than 2100 procedures. Surg. Today. 2016;46:1318–1324. doi: 10.1007/s00595-016-1315-7. PMID: 26922213. [DOI] [PubMed] [Google Scholar]
- 5.Endo K., Kujirai D., Maeda H., Ishida T., Terauchi T., Kimata M., Shinozaki H., Lefor A.K., Sata N. Transumbilical laparoscopic appendectomy performed by residents is safe and feasible. Asian J. Endosc. Surg. 2016;9:270–274. doi: 10.1111/ases.12303. PMID: 27349207. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Fowler A.J., Rajmohan S., Barai I., Orgill D.P. PROCESS Group. Preferred reporting of case series in surgery; the PROCESS guidelines. Int. J. Surg. 2016;36(Pt A):319–323. doi: 10.1016/j.ijsu.2016.10.025. PMID: 27770639. [DOI] [PubMed] [Google Scholar]
- 7.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richards M.K., McAteer J.P., Drake F.T., Goldin A.B., Khandelwal S., Gow K.W. A national review of the frequency of minimally invasive surgery among general surgery residents: assessment of ACGME case logs during 2 decades of general surgery resident training. JAMA Surg. 2015;150:169–172. doi: 10.1001/jamasurg.2014.1791. PMID: 25548997. [DOI] [PubMed] [Google Scholar]
- 9.Wakasugi M., Tei M., Anno K., Mikami T., Tsukada R., Koh M., Furukawa K., Suzuki Y., Masuzawa T., Kishi K., Tanemura M., Akamatsu H. Single-incision totally extraperitoneal inguinal hernia repair as a teaching procedure: one center's experience of more than 300 procedures. Surg. Today. 2016;46:1039–1044. doi: 10.1007/s00595-015-1273-5. PMID: 26563226. [DOI] [PubMed] [Google Scholar]