Abstract
In Germany, a biennial preventive health check-up has been available for individuals aged 35 and older since 1989. The check-up includes identification of cardiovascular disease risk factors and examinations for diabetes mellitus type 2 and kidney disease. Participation in preventive health check-ups among 19,351 women aged 35 to 74 in Germany in 2004 was investigated. Logistic regression was performed to examine associations between participation and age, marital status, education, socio-economic status (SES) and region of residence. In total, 53.4% of women attended at least every two years, 23.4% attended irregularly and 23.2% never attended. In adjusted models, single, divorced, separated or widowed women were less likely to have a preventive health check-up at least every two years compared to married women (OR 0.63, 95% CI 0.57–0.71), while women in eastern Germany were less likely to participate (OR 0.80, 95% CI 0.75–0.86) than women in western Germany. Education showed no association with having a preventive health check-up at least every two years; however, women with low SES were less likely to participate compared to those with high SES (OR 0.82, 95% CI 0.74–0.92). About half of eligible women reported participating in health check-ups at least every two years, with participation varying according to socio-demographic characteristics. Women who are less likely to participate may benefit from receiving invitation letters within the framework of an organised programme. The benefits of general health checks, however, need to be evaluated.
Keywords: Preventive health check-up, Survey, Socio-economic status, Education, Germany
1. Introduction
A biennial preventive health check-up covered by the health insurance companies has been available for all men and women aged 35 and older in Germany since 1989 (Kahl et al., 1999). The health check-up includes identification of cardiovascular disease risk factors, such as raised cholesterol levels and high blood pressure, as well as examinations for diabetes mellitus type 2 and kidney disease. This includes blood glucose, cholesterol as well as urine tests. There is no organised invitation system for eligible individuals in Germany; rather, check-ups are performed on an opportunistic basis, largely on the patients' own initiative and usually at a general practitioner's (GP) office.
General health checks are regularly performed in the USA and UK, with the National Health Service Health Check programme being introduced in the UK in 2009 (Holland, 2009). Health Check programmes have also been initiated in the Netherlands and Australia, while Denmark has recently abandoned plans to introduce such a programme for the general population (Si et al., 2014, Gotzsche et al., 2014).
Previous studies have shown that participation in the preventive health check-up has been low in Germany. The two-year participation among women in a 2002–2003 study was reported to be 43% (Bergmann et al., 2005). In a 2003–2004 Telephone Health Survey in Germany, 46.8% of women reported having had a health check-up in the previous two years (Ellert et al., 2006). A Finnish study investigated participation in an invitational occupational health check-up in specified age groups and found that 38% of women participated, with the highest income quartile being more likely than the lowest quartile to participate (Laaksonen et al., 2008). Other studies have found participation rates in programmes with a personal invitation to be much higher. Since 2005, an invitational programme aimed at preventing cardiovascular disease in a Swedish county has reported participation rates of 66% (Norberg et al., 2010). Another Swedish study reported that 71.2% of individuals aged 32 to 51 who were invited to a comprehensive check-up for cardiovascular disease risk factors, detection of breast cancer, diabetes and alcohol abuse, chose to participate (Berglund et al., 2000).
Our study analysed data from a nationwide population-based survey to investigate the participation of women in Germany in opportunistic preventive health check-ups, and to determine social, demographic and economic factors influencing participation.
2. Methods
2.1. Study population
Data from the 2004 Healthcare Access Panel, an established population-based household panel were analysed. The panel consisted of 49,890 households, which included 47,796 women between the ages of 20 and 74.
2.2. Questionnaire
A comprehensive questionnaire was sent via the postal service. Participants were asked to indicate whether and how often they participated in preventive health check-ups. The questionnaire also assessed various socio-demographic factors.
2.3. Education and socio-economic status
Education was categorised as follows: 8–9 years (low), 10 years (medium), 12–13 years (high). For the assignment of women into SES categories, data on ‘highest education’, ‘occupational position and employment’, and ‘equivalent net household income’ were combined. The ‘equivalent net household income’ variable took the number of people living in the household into account (Klug et al., 2005). The variables were each awarded a maximum of 7 points, the highest possible score for SES being 21 (Winkler, 1998). The final SES categories were: low SES (< 8.5), medium SES (between 8.5 and < 14.5), or high SES (> = 14.5). In cases where there was a missing value for one of the three variables, this value was imputed by obtaining the mean of the two available variables (Winkler, 1998). No SES could be calculated for 512 women due to missing values in more than one of the three variables.
2.4. Statistical methods
Preventive health check-up participation rates among women aged 35 years and older were reported. Univariable and multivariable logistic regression models were used to examine the effect of age (reference: 35 to 44 years), marital status (reference: married), school education (reference: high education), SES (reference: high SES) and region (reference: western Germany) on participation in preventive health check-ups at least every two years. Because education data were included when constructing the SES variable, two separate logistic regression models were used. Odds ratios (OR) were estimated and 95% confidence intervals (CI) reported. All statistical procedures were performed with SAS 9.3 (Cary, North Carolina, USA).
3. Results
Of the 47,796 women who were contacted, 24,299 women returned the questionnaire (50.8%). A total of 19,351 women who answered the preventive health check-up question were aged 35 or older. The mean age in the study population was 50 years, with 70.5% being married and 8.3% being single. A total of 37.2% had a low level, and 20.2% had a high level of education. The majority of study participants had medium SES (66.4%), while 12.6% had low and 18.4% high SES. A total of 78.5% lived in western Germany and 21.5% lived in eastern Germany (data not shown).
Of the 19,351 women aged 35 or older included in the analysis, 53.4% reported participating in the preventive health check-up at least every two years, 23.4% participated irregularly, and 23.2% had never participated.
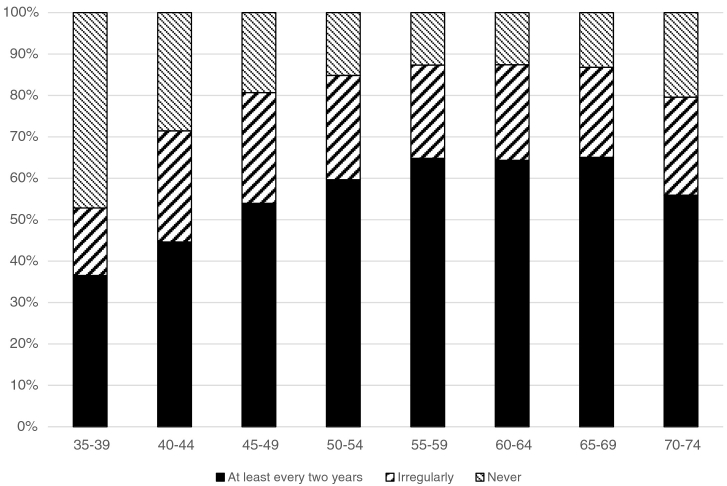
Fig. 1 shows participation rates in five-year age groups. Participation steadily increased in each of the age groups up to the age of 55. It then remained at a constant level up to the age of 69 and decreased again in the oldest age group (70–74 years). Participation at least every two years was highest in the age groups 55–59 (64.8%) and 65–69 years (65.0%). Only 36.5% of the 35–39 year-olds participated at least every two years.
Fig. 1.
Participation in preventive health check-ups as indicated by 19,351 women aged 35 to 74 in Germany in 2004.
Univariable logistic regression showed that older women were more likely to participate in preventive health check-ups at least every two years (OR65–74 2.58, 95% CI 2.30–2.89), while single (OR 0.52, 95% CI 0.47–0.57) as well as divorced, widowed and separated women (OR 0.90, 95% CI 0.84–0.96) were less likely to participate. Women with low education (OR 1.39, 95% CI 1.29–1.50) were more likely to participate, while participation among those with low SES (OR 0.87, 95% CI 0.78–0.96) as well as those living in eastern Germany (OR 0.84, 95% CI 0.78–0.90) was less likely (Table 1).
Table 1.
Univariable and multivariable logistic regression results for preventive health check-up participation among 19,351 women in Germany in 2004.
| Socio-demographic characteristics | Participating at least every 2 yearsa |
|||||
|---|---|---|---|---|---|---|
| Univariable |
Multivariableb |
Multivariablec |
||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age | ||||||
| 35–44 (reference) | 1.00 | – | 1.00 | – | 1.00 | – |
| 45–54 | 1.90 | 1.78–2.04 | 1.87 | 1.74–2.00 | 1.88 | 1.76–2.02 |
| 55–64 | 2.65 | 2.45–2.86 | 2.63 | 2.43–2.86 | 2.63 | 2.43–2.85 |
| 65–74 | 2.58 | 2.30–2.89 | 2.55 | 2.27–2.87 | 2.68 | 2.38–3.01 |
| Marital status | ||||||
| Married (reference) | 1.00 | – | 1.00 | – | 1.00 | – |
| Single | 0.52 | 0.47–0.57 | 0.63 | 0.57–0.71 | 0.63 | 0.57–0.71 |
| Divorced, widowedd | 0.90 | 0.84–0.96 | 0.80 | 0.75–0.86 | 0.82 | 0.76–0.88 |
| School education | ||||||
| 12–13 years (High) (reference) | 1.00 | – | 1.00 | – | – | – |
| 10 years (Medium) | 1.05 | 0.97–1.13 | 1.04 | 0.96–1.13 | – | – |
| ≤ 8–9 years (Low) | 1.39 | 1.29–1.50 | 1.06 | 0.98–1.16 | – | – |
| SES | ||||||
| High (reference) | 1.00 | – | – | – | 1.00 | – |
| Medium | 0.99 | 0.92–1.07 | – | – | 1.03 | 0.95–1.11 |
| Low | 0.87 | 0.78–0.96 | – | – | 0.82 | 0.74–0.92 |
| Region | ||||||
| West (reference) | 1.00 | – | 1.00 | – | 1.00 | – |
| East | 0.84 | 0.78–0.90 | 0.80 | 0.75–0.86 | 0.80 | 0.75–0.86 |
Reference category: ‘irregularly’ or ‘not yet’.
Controlled for age, marital status, school education and region.
Controlled for age, marital status, SES and region.
Includes women who are separated but not divorced.
In the adjusted logistic regression (SES model), older women were more likely to participate at least every two years (OR65–74 2.68, 95% CI 2.38–3.01). Participation was less likely among divorced, widowed and separated women than married women (OR 0.82, 95% CI 0.76–0.88). Similarly women from eastern Germany were less likely to participate compared to women from western Germany (OR 0.80, 95% CI 0.75–0.86). Participation was also less likely among women with low SES (OR 0.82, 95% CI 0.74–0.92), while education had no statistically significant influence on participation in the adjusted model (Table 1).
4. Discussion
Our results showed that just over half of eligible women aged 35 or older in Germany underwent a preventive health check-up at least every two years as recommended by German health authorities. Participation was higher among women who were older, married, of higher SES and from western Germany.
The two-year preventive health check-up participation rate in our survey (53.4%) was higher than in the 2003–2004 German Telephone Health Survey, which reported a 46.8% participation rate over a two-year period (Ellert et al., 2006). Similarly, data from the German Central Institute for Statutory Health Insurance Care (ZI), found two-year participation to be 41.0% for 2007 and 2008 (Theimer, 2010). However, the latter source relied on a selection of billing data, and not on population-based data. The ZI reported a two-year participation rate of 48.5% among women for the years 2012–2013 (ZI, 2015). Data from the Robert Koch Institute's (RKI) 2009/2010 German Health Update (GEDA) showed that 49.8% of women surveyed had undergone a check-up in the two years before the survey (Hoebel et al., 2013). Almost a quarter of women in our study (23.2%) had never participated in the preventive health check-up, substantially less than the 47.8% reported in the 2003–2004 German Telephone Health Survey (Ellert et al., 2006).
In our analyses, women with low SES were less likely to participate than women with high SES. Findings from the GEDA study were similar, with eligible women of low SES also being less likely to attend health checks than women of high SES (OR 0.63, 95% CI 0.55–0.72) (Hoebel et al., 2013). The German Telephone Health Survey, however, found the opposite effect (Ellert et al., 2006).
Previous studies have suggested that preventive health check-up participation involves the self-selection of more health conscious individuals, meaning that those with more risk factors may choose not to participate. Those who attend health checks tend to have higher socio-economic status, lower cardiovascular risk, less cardiovascular morbidity, and lower mortality than others, thus reducing the potential cost-effectiveness of preventive health care (Krogsboll et al., 2012, Huber et al., 2009). If this is the case, programmes to encourage participation among those who are unlikely to attend could be beneficial. A British study by Chamnan and colleagues concluded that a programme model that used a score based on a risk factor assessment to select patients for a cardiovascular check-up, would have similar sensitivity and specificity for cardiovascular events as mass invitation (Chamnan et al., 2010). Additionally, Swedish studies have shown that participation rates increase when eligible individuals are personally invited to attend (Norberg et al., 2010, Berglund et al., 2000).
The benefits of preventive health checks have recently been called into question, with a Cochrane systematic review concluding that general health checks are not effective in terms of reducing morbidity or mortality (Krogsbøll et al., 2012). No effect was found overall, nor for cardiovascular or cancer causes. The review did however find that general health checks increased the number of new diagnoses (Krogsbøll et al., 2012). The most recent randomized trial investigating general health checks, the Danish Inter99 trial, investigated the effect of systematic screening for ischaemic heart disease risk factors. This trial also failed to find an effect on total mortality (Gøtzsche et al., 2014). Plans to implement a preventive health check programme in Denmark have recently been abandoned in light of these findings (Gøtzsche et al., 2014).
Although health checks may contribute towards reducing patient anxiety, it is questionable whether the net clinical benefit justifies the substantial cost involved. Potentially the health check may even be harmful by leading to over-diagnosis (Mehrotra & Prochazka, 2016). Some have argued that it should be replaced with a new type of visit, which focusses on establishing a trusting therapeutic relationship between the physician and patient, and not exclusively on the physical exam or screening laboratory tests (Mehrotra & Prochazka, 2016). Other suggestions include calls for improving the health check by allowing for a multidisciplinary-team-based approach (Goroll, 2016).
Limitations of our study include the self-reporting nature of the questionnaire, with women possibly underestimating or overestimating their participation.
5. Conclusions
Our study showed evidence for lower preventive health check-up participation at least every two years among women who were younger, single, divorced or widowed, women with low SES and women from eastern Germany. These groups might benefit from reminders or invitation letters to attend. This should ideally occur within the framework of an organised, quality-controlled, evaluated programme. However, since the effectiveness of preventive health check-ups has recently been questioned, the benefits of such a programme should first be carefully evaluated before such an organised programme is implemented.
Conflict of interest
None.
Funding
This work was supported by the German Research Foundation (DFG) and the Technical University of Munich within the funding programme Open Access Publishing.
Acknowledgments
The authors would like to thank Dagmar Lautz for her assistance with data preparation.
References
- Berglund G., Nilsson P., Eriksson K.F. Long-term outcome of the Malmö Preventive Project: mortality and cardiovascular morbidity. J. Intern. Med. 2000;247:19–29. doi: 10.1046/j.1365-2796.2000.00568.x. [DOI] [PubMed] [Google Scholar]
- Bergmann E., Kalcklösch M., Tiemann F. Public health care utilization. Initial results of the Telephone Health Survey 2003. Bundesgesundheitsbl. Gesundheitsforsch. Gesundheitsschutz. 2005 Dec;48(12):1365–1373. doi: 10.1007/s00103-005-1167-6. [DOI] [PubMed] [Google Scholar]
- Chamnan P., Käser L., Simmons R., Griffin S. Estimating the population impact of screening strategies for identifying and treating people at high risk of cardiovascular disease: modelling study. BMJ. 2010;340:c1693. doi: 10.1136/bmj.c1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellert U., Wirz J., Ziese T. Robert Koch Institut; Berlin: 2006. Telephone Health Survey from the Robert Koch Institute (2nd Wave) [Google Scholar]
- Goroll A. Toward trusting therapeutic relationships - in favor of the annual physical. N. Engl. J. Med. 2016;373(16):1487–1489. doi: 10.1056/NEJMp1508270. [DOI] [PubMed] [Google Scholar]
- Gøtzsche P.C., Jørgensen K.J., Krogsbøll L.T. General health checks don't work. BMJ. 2014;348:g3680. doi: 10.1136/bmj.g3680. [DOI] [PubMed] [Google Scholar]
- Hoebel J., Richter M., Lampert T. Social status and participation in health checks in men and women in Germany: results from the German Health Update (GEDA), 2009 and 2010. Dtsch. Arztebl. Int. 2013 Oct;110(41):679–685. doi: 10.3238/arztebl.2013.0679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland W. Periodic health examination – a brief history and critical assessment. Eurohealth. 2009;15(4):16–20. [Google Scholar]
- Huber C., Käser L., Rosemann T., Senn O. Medical check-ups on the ‘Gesundheitsschiff’. Benefit for population at risk, or self-selection of healthy and health-conscious people? Praxis. 2009;98:1421–1427. doi: 10.1024/1661-8157.98.24.1421. [DOI] [PubMed] [Google Scholar]
- Kahl H., Hölling H., Kamtsiuris P. Utilization of health screening studies and measures for health promotion. Gesundheitswesen. 1999 Dec;61(2):S163–S168. [PubMed] [Google Scholar]
- Klug S.J., Hetzer M., Blettner M. Screening for breast and cervical cancer in a large German city: participation, motivation and knowledge of risk factors. Eur. J. Pub. Health. 2005 Feb;15(1):70–77. doi: 10.1093/eurpub/cki118. [DOI] [PubMed] [Google Scholar]
- Krogsbøll L.T., Jørgensen K.J., Grønhøj Larsen C., Gøtzsche P.C. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ. 2012;345 doi: 10.1136/bmj.e7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laaksonen M., Aittomäki A., Lallukka T. Register-based study among employees showed small nonparticipation bias in health surveys and check-ups. J. Clin. Epidemiol. 2008 Sep;61(9):900–906. doi: 10.1016/j.jclinepi.2007.09.010. [DOI] [PubMed] [Google Scholar]
- Mehrotra A., Prochazka A. Improving value in health care - against the annual physical. N. Engl. J. Med. 2016;373(16):1485–1487. doi: 10.1056/NEJMp1507485. [DOI] [PubMed] [Google Scholar]
- Norberg M., Wall S., Boman K., Weinehall L. The Västerbotten Intervention Programme: background, design and implications. Glob. Health Action. 2010;3 doi: 10.3402/gha.v3i0.4643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si S., Moss J.R., Sullivan T.R., Newton S.S., Stocks N.P. Effectiveness of general practice-based health checks: a systematic review and meta-analysis. Br. J. Gen. Pract. 2014 Jan;64(618):e47–e53. doi: 10.3399/bjgp14X676456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theimer C. Krankheitsfrüherkennung. Zu wenig genutzt. Dt Ärztebl. 2010 Feb 12;107(6):A232. [Google Scholar]
- Winkler J. The measurement of social status using an index in the health surveys of the DHP. In: Ahrens W., Bellach B.M., Jöckel K.H., editors. Measurement of Socio-Demographic Characteristics in Epidemiology. Medizin Verlag; München: 1998. pp. 69–74. [Google Scholar]
- German Central Institute for Statutory Health Insurance Care (ZI) 2015. Utlization of Statutory Health Check-Ups. www.gbe-bund.de Accessed: 18.08.2015. [Google Scholar]