Highlights
-
•
There are currently no available prostheses that can be used for extremely small femurs or tibias of adult patients.
-
•
Our novel technique can be used with conventional prostheses.
-
•
Our novel technique is simple and easy solution in skeletally immature adult patients requiring the resection of distal femur malignant tumors.
Keywords: Surgical technique, Distal femur replacement, Osteosarcoma, Bone tumor
Abstract
Introduction
There are currently no available prostheses that can be used for extremely small femurs or tibias of adult patients in countries where allograft is unavailable.
Case report
We report the case of a 17-year-old girl requiring special limb salvage technique for distal femur reconstruction following resection of malignant tumor. This technique was needed because of a very narrow canal of the tibia. We split bilateral tibial cortices longitudinally with osteotomies to enlarge tibial canal enough to insert conventional endoprosthesis. After insertion of the implant, split tibia reduced with titanium cables and bands, and the split clefts were filled with cancellous bone. Fifteen months after the operation, proper fixation was achieved with bony fusion of bilateral split clefts and ambulation without assistance was achieved.
Discussion
Any proper surgical procedure for our patient were reported previously. We developed a conventional non-expandable endoprosthesis for distal femur replacement using the double longitudinal split technique as a solution to this difficult problem.
Conclusion
Our longitudinal split technique should be applicable to adult patients with skeletal immaturity requiring resection of juxta-articular malignant tumors and in other situations complicated by the presence of a narrow canal.
1. Introduction
Currently, 90–95% of patients with primary musculoskeletal malignant tumors involving the extremities are treated safely with wide resection and limb-salvage surgery with a low risk of recurrence and the same disease-free survival rate as with amputative surgery [1], [2], [3]. Limb salvage increases patient satisfaction since it provides immediate mobility, stability, weight bearing, and an improved quality of life due to a more acceptable cosmetic appearance and greater emotional acceptance.
The distal femur has a predilection for developing skeletal sarcomas. A frequently performed distal femur tumor treatment involves distal femur reconstruction with a total knee arthroplasty (TKA) system following tumor resection [4]. However, there are currently no available prostheses that can be used for extremely small femurs or tibias of adult patients.
We report that our novel longitudinal split technique can be used with conventional prostheses in skeletally immature adult patients requiring the resection of distal femur malignant tumors.
2. Case report
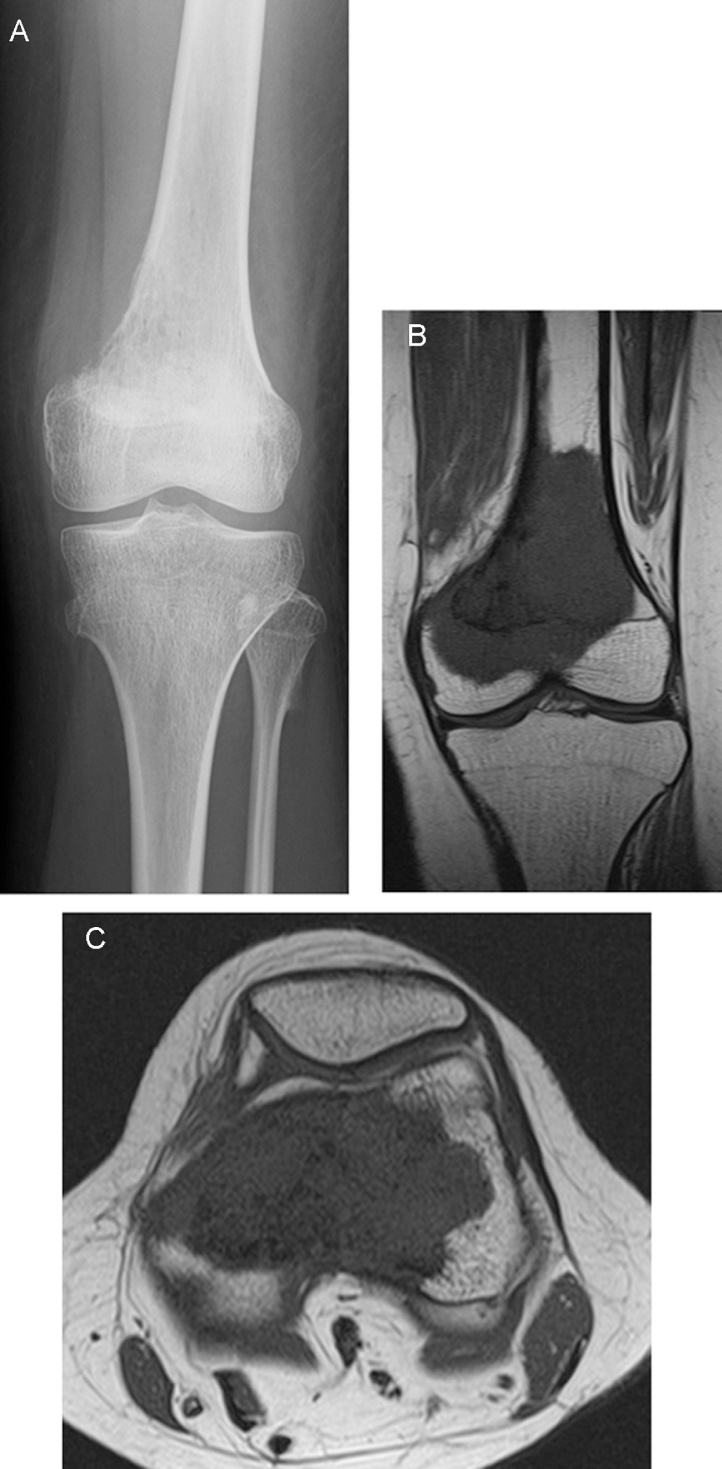
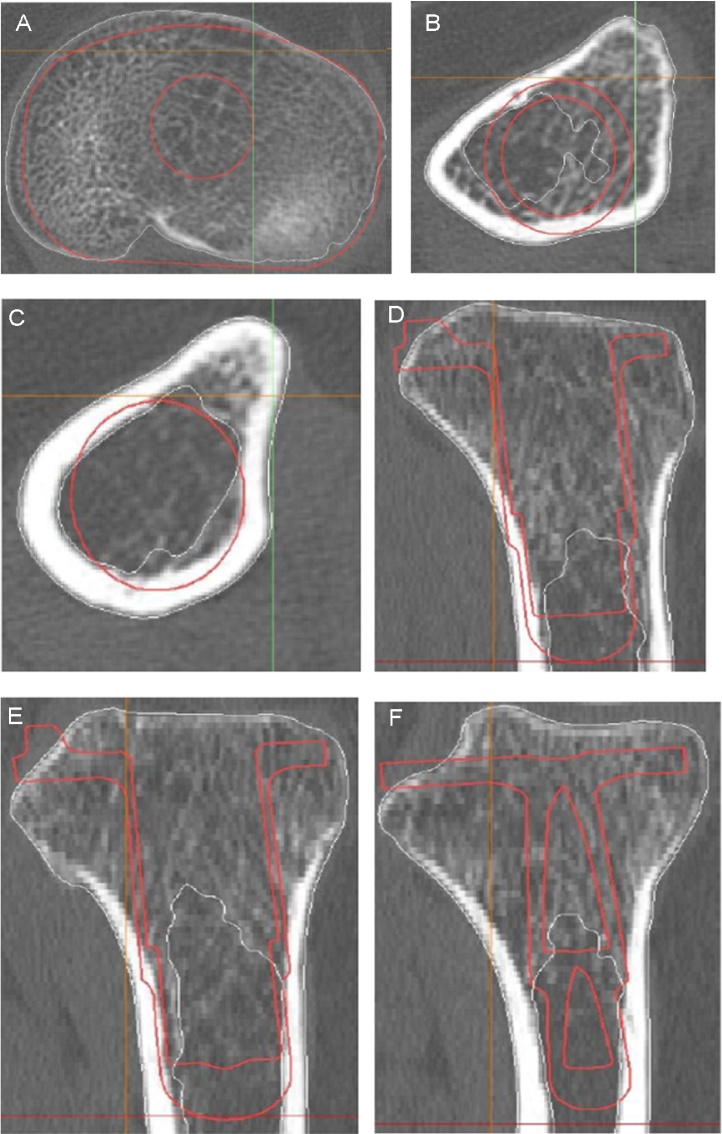
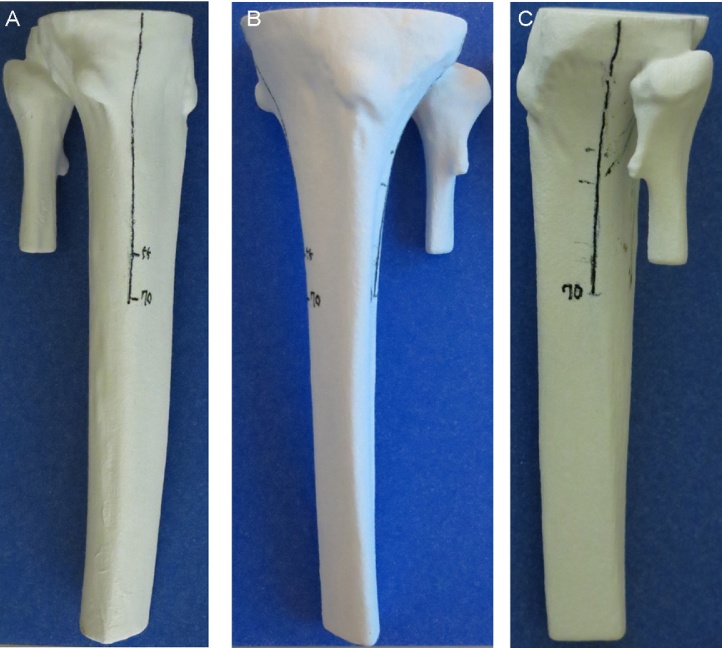
A 17-year-old girl was referred to our hospital for the treatment of a left distal femoral bone tumor. Her gait was normal although she suffered from knee pain. Her height was 138 cm, and her body weight was 32 kg at the time of her first visit. She had been treated between the ages of 3 months and 3 years with chemotherapy and whole body radiation for malignant lymphoma. The skull base radiation for this treatment resulted in growth disturbances. She was treated with growth hormone and thyroid hormone for secondary growth hormone deficiency and secondary hypothyroidism. Radiographs of the knee demonstrated periosteal reaction, an osteolytic lesion in the medial part of the distal femur, and that the growth plate was closed (Fig. 1a). An MRI at the time of presentation demonstrated that the medial part of the articular capsule and one-fourth of the medial part of the patella were invaded by the tumor. Pathology of an open biopsy specimen showed conventional osteosarcoma. Preoperative chemotherapy was administered, and a wide resection of the distal femoral tumor with a distal femoral reconstruction was planned by using a prosthetic replacement. Preoperative MRI showed the tumor involving most of the distal femur, but the previously seen contamination of the medial part of the articular capsule and the patella were no longer appreciable (Fig. 1b, c). Preoperative planning with the Mimics (Biomet Japan, LLC., Tokyo, Japan) computer simulation system revealed that the medullary cavity of the proximal part of the tibia was too narrow for insertion of the smallest diameter prosthesis available in Japan, although the femur component of the prosthesis was of appropriate size (Fig. 2a–f). We intentionally planned bilateral longitudinal splits on the proximal tibia, along the medial border of the tibia and the interosseous border, to allow bending of the posterior tibial cortex and insertion into the tibial component stem. The reconstruction prosthesis we selected was Biomet OSS (Orthopaedic Salvage System, Biomet Japan), a rotating hinge knee joint that allows a maximum flexion of 135°, a maximum extension of −3° and an internal/external rotation of 20°. We selected the Biomet OSS because the diameter of the stem of the tibial component was the smallest available in Japan. Preoperative planning demonstrated the need for 70 mm bilateral splits of the tibia. We made a 3D plaster model to confirm the split lines needed during the operation (Fig. 3).
Fig. 1.
Preoperative anteroposterior (A) radiograph of the left knee of the 17-year-old female patient showing periosteal reaction on the medial aspect of the distal femur. The coronal (B) and axial (C) preoperative MRI showed tumor localization in the distal diaphysis of the femur.
Fig. 2.
Computer simulation view of endoprosthesis implantation in the tibia (A–F). (A–C) axial section from proximal to distal, (D–F) sagittal views from center to medial. These sequential views showed the canal of the tibia was too narrow to allow for insertion of the endoprosthesis.
Fig. 3.
3-D plaster model (A–C). Bilateral lines were planned as split line.
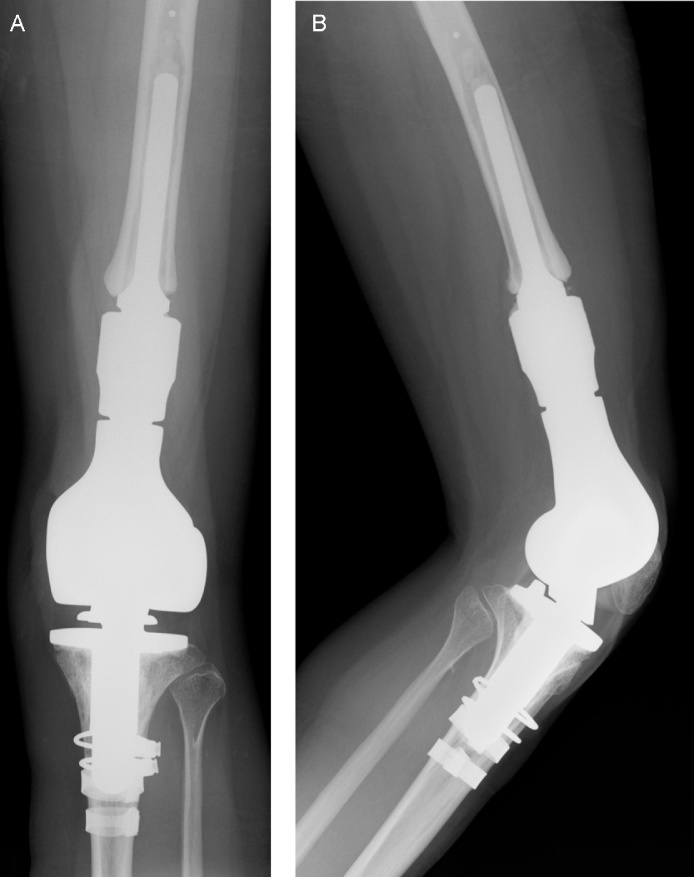
After wide resection of the distal femoral tumor with inclusion of the medial part of the patella and the articular capsule through a medial incision, distal femoral reconstruction was performed. The resection length of the femur and tibia were 11 and 1.2 cm, respectively, as planned. After resection of both bones, split lines were made along the medial border of the tibia and the interosseous border of the tibia with a 1-cm width osteotome. The length of each split line was 70 mm. We referred to the 3D plaster model made preoperatively to ensure appropriate split lines. Both split lines were prepared simultaneously, 5 mm at a time on alternating sides of the bone. To check the length of the split lines and to ensure that the tibial component would insert at the proper angle, femoral and tibial trial insertions were performed. For our patient, the reduced OSS Tibial Plate Short 51 mm, 12 mm tibial bearing was selected for the tibia and the OSS segmental femoral component 7 cm (diameter 9 mm) and OSS diaphyseal segment 4 cm were selected. Then, 2 Dall-Miles cables (Stryker, Mahwah, NJ) and titanium Compression Cerclage Gundolf (CCG) bands (Smith & Nephew Orthopaedics KK, Tokyo, Japan) were applied loosely. The femoral component was implanted first, and then, the tibial component was inserted as recommended by the manufacturer. In order to avoid leaking of the cement from the bilateral cleft, the cement was attached to the tibial implant prior to insertion into the cavity. After tightening the cables and bands, excess cement was removed. Fragments of tibial cortex and cancellous bone were collected from the resected tibia and inserted into the clefts. Cobalt High Contrast Bone Cement (Biomet Japan, Tokyo, Japan) was used because of its high viscosity, which prevents leaking. The medial gastrocnemius muscle was transposed to the medial part of the patella to reconstruct the medial articular capsule. The intraoperative passive range of motion (ROM) of the knee achieved was extension to 0° and flexion to 120°. Postoperative radiographs showed bilateral split lines (Fig. 4a, b). One week after operation, necrosis of the skin on the patella and medial gastrocnemius flap occurred. Debridement of the necrotic tissue was performed, and a vacuum-assisted closure (VAC®, KCI, Tokyo, Japan) device was applied for 4 weeks. After granulation of the wound a free full-thickness skin graft was performed. The operated knee was immobilized for 8 weeks following distal femur replacement with an elastic knee brace. The patient was allowed partial weight bearing (25%) for 2 weeks, and weight-bearing was increased by 25% every fortnight. Twelve weeks after distal femur replacement, the patient was able to walk without any assistance and tolerated full weight bearing.
Fig. 4.
Two months after distal femur replacement. Anteroposterior (A) and lateral (B) radiographs. Lateral radiograph demonstrates split lines below band.
At the 15-month postoperative follow-up, the patient was able to walk with full weight bearing and without any support. The active ROM was extension to −5° and flexion to 120°. Radiographs demonstrated shortening of the bilateral longitudinal splits (Fig. 5a, b). The bilateral clefts were healing spontaneously evident by comparing the CT from 2 months after operation and the CT from 15 months after the operation (Fig. 6a–h). There were no soft tissue deformities at this point.
Fig. 5.
15 months after distal femur replacement. Anteroposterior (A) and lateral (B) radiographs. Lateral radiograph demonstrates healing split lines.
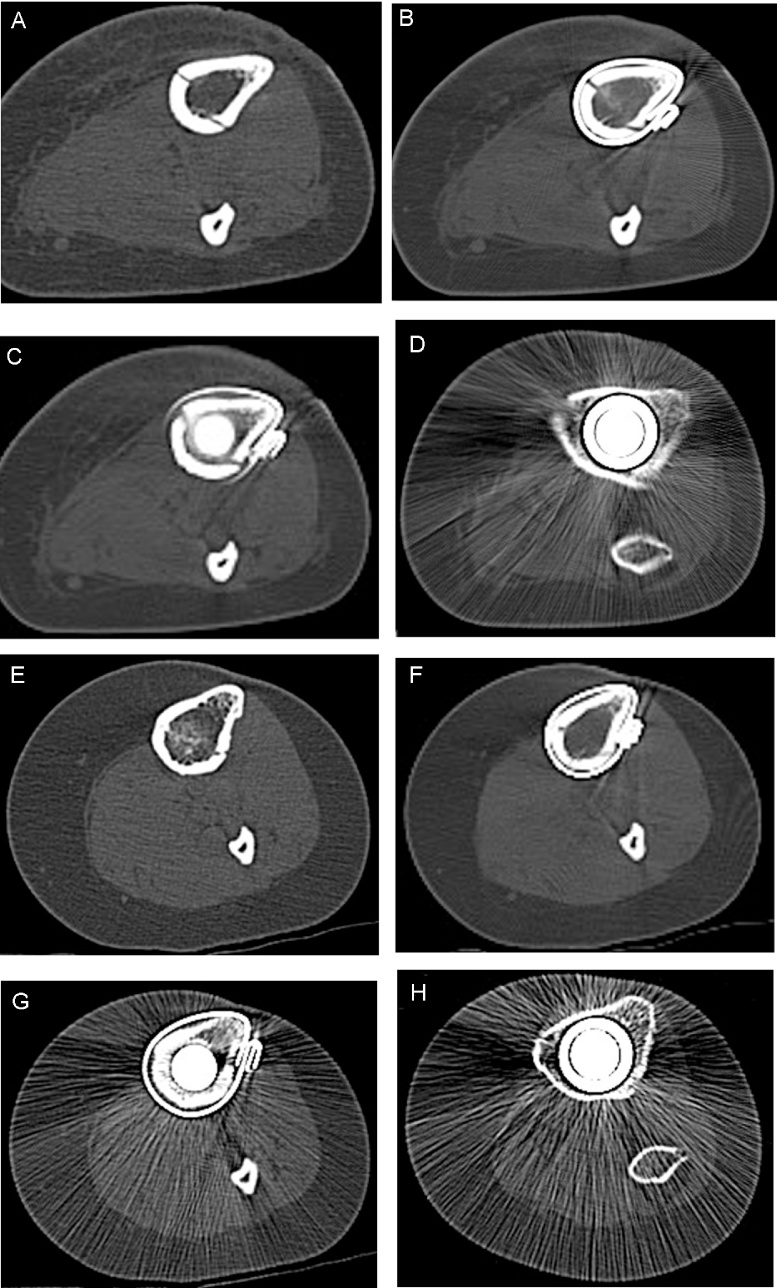
Fig. 6.
CT views of bilateral split lines 2 months after operation (A–D) and 15 months after operations (E–H). Each section shows bony union of the bilateral split clefts.
3. Discussion
In our case, the challenge was to devise a way to treat a distal femur osteosarcoma in the setting of very small bones due to acquired growth impairment. There is a paucity of guidance in the English literature on techniques to accomplish distal femur replacement for primary malignant bone tumors in the setting of very small mature bone. There are several surgical approaches described for cases of malignant bone tumors in children with extraordinarily small bone [5]. These procedures include: (1) amputation, (2) rotationplasty, (3) osteoarticular allograft, (4) arthrodesis techniques using a combination of allograft and autograft (vascularized or not), and (5) standard expanding endoprostheses for children.
Limb-sparing surgery preserves more physical function than amputation [3]. Limb salvage should offer the same chance of cure as amputation. Functional and cosmetic outcomes should be equal to, or better than, that from amputation [6]. In our country, allograft is not available. Standard expanding endoprostheses are available, but these have to be replaced with a conventional non-expanding endoprosthesis after skeletal maturity is complete [5]. All of the expanding systems have a high complication rate [5]. Rotationplasty is a rare surgical procedure in which the diseased part of the femur and knee are removed and the lower leg is re-attached to the thigh by a rotation of 180°. The ankle then acts as a knee joint while the foot is facing posteriorly. With this surgery, the sciatic nerve is preserved, but the cosmetic appearance of the rotated foot can lead to psychological problems [6].
Thus, for our patient, the best way to preserve the affected limb was limb salvage surgery with a non-expanding conventional endoprosthetic reconstruction, if possible. We used a conventional non-expandable endoprosthesis for distal femur replacement using the double longitudinal split technique as a solution to this difficult problem. A similar concept was reported as a solution for a complication during femoral broaching in total hip arthroplasty [7].
In conclusion, our longitudinal split technique should be applicable to adult patients with skeletal immaturity requiring resection of juxta-articular malignant tumors and in other situations complicated by the presence of a narrow canal.
Conflicts of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Funding
Authors declare there is no funding resources for this paper.
Ethical approval
Institutional review board approval was not required because all data were collected from clinical records and imaging systems for routine preoperative planning and follow-up.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
TA wrote this paper. All authors attended the surgery and read this paper.
Guarantor
Toru Akiyama, the corresponding author of this paper.
Contributor Information
Toru Akiyama, Email: toruakiyama827@jichi.ac.jp.
Shotaro Kanda, Email: panda714@hotmail.co.jp.
Kazuo Saita, Email: saita-k@jichi.ac.jp.
References
- 1.Mavrogenis A.F., Coll-Mesa L., Gonzalez-Gaitan M., Ucelay-Gomez R., Fabri N., Ruggieri P. Criteria and outcome of limb salvage surgery. J. BUON. 2011;16(4):617–626. [PubMed] [Google Scholar]
- 2.Sim I.W., Tse L.F., Ek E.T., Powell G.J., Choong P.F. Salvaging the limb salvage: management of complications following endoprosthetic reconstruction for tumours around the knee. Eur. J. Surg. Oncol. 2007;33(6):796–802. doi: 10.1016/j.ejso.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Aksnes L.H., Bauer H.C., Jebsen N.L., Folleras G., Allert C., Haugen G.S. Limb-sparing surgery preserves more function than amputation: a Scandinavian sarcoma group study of 118 patients. J. Bone Joint Surg. Br. 2008;90(6):786–794. doi: 10.1302/0301-620X.90B6.19805. [DOI] [PubMed] [Google Scholar]
- 4.Akiyama T., Kanda S., Maeda A., Endo M., Saita K. Patella dislocation following distal femoral replacement after bone tumour resection. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-205006. (29/Jul/2014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dotan A., Dadia S., Bickels J., Nirkin A., Flusser G., Issakov J. Expandable endoprosthesis for limb-sparing surgery in children: long-term results. J. Child. Orthop. 2010;4(5):391–400. doi: 10.1007/s11832-010-0270-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimer R.J. Surgical options for children with osteosarcoma. Lancet Oncol. 2005;6(2):85–92. doi: 10.1016/S1470-2045(05)01734-1. [DOI] [PubMed] [Google Scholar]
- 7.Waldstein W., Boettner F. A complication during femoral broaching in total hip arthroplasty: a case report. Open Orthop. J. 2013;7:272–274. doi: 10.2174/1874325001307010272. [DOI] [PMC free article] [PubMed] [Google Scholar]