Abstract
Anterior cruciate ligament (ACL) tears are among the most common sports-related injuries. Although studies have reported reliable outcomes with allograft tissue, several studies have shown a higher failure rate in younger patients. Although ACL graft augmentation has been met with varying levels of success, internal bracing of an allograft represents a promising area in ACL reconstruction. The purpose of this article is to detail allograft preparation involving a collagen-coated, ultrahigh-molecular-weight polyethylene/polyester suture tape as an internal brace augmentation for ACL reconstruction using the all-inside ACL GraftLink Technique (Arthrex, Naples, FL).
Given the prevalence of anterior cruciate ligament (ACL) injury and the continual need for improved reconstructive techniques, surgeons are constantly looking for possible surgical technique advancements. Although several studies have shown good success with use of allograft tissue for ACL reconstruction,1, 2 many authors have shown a higher failure rate in younger patients.3, 4, 5 A possible clinical solution to improving outcomes with allograft ACL reconstruction would be adding augmentation to the allograft. Historically, there has been a negative connotation surrounding the usage of artificial devices for ACL substitution based on past experience.6, 7 However, review of the literature suggests that ACL augmentation through the addition of a synthetic device to a soft tissue graft for ACL reconstruction can yield positive outcomes.8, 9, 10 Batty et al.8 noted in their systematic review that short-term results for newer-generation devices generated lower reported rates of revision, failure, and sterile synovitis/effusion than older synthetic grafts. Likewise, the editor-in-chief of Arthroscopy penned an editorial commentary discussing the potential benefits of utilizing second-generation synthetic ACL grafts as a structural tie when used in combination with promising scaffold technologies.9 Finally, Lubowitz, MacKay, and Gilmer discuss their successes in augmenting medial cruciate ligament reconstructions with a FiberTape (Arthrex, Naples, FL).10
This article presents a unique ACL augmentation reconstructive technique utilizing an ultrahigh-molecular-weight polyethylene/polyester tape that serves as an internal brace. The tape integrates seamlessly into a quadrupled tendon graft construct. This construct theoretically adds strength to the biomechanical properties of the ACL graft through the addition of the tape, yet maintains the other properties of a natural graft. The major advantage with this approach for a soft tissue allograft would be for protection of the allograft during the revascularization and remodeling phase as biologic incorporation of allograft tissue has been shown to be slower than with autograft.11 The ACL reconstruction in this case follows the all-inside ACL GraftLink technique (Arthrex) initially described by Lubowitz et al.12
Surgical Technique
For this procedure, an anterior tibialis allograft with the addition of a FiberTape (Arthrex) for internal brace augmentation was used to complete an ACL reconstruction. A collagen-coated FiberTape is preferred for increased tissue integration. Similar to the graft preparation demonstrated by Lubowitz, this procedure uses a GraftLink construct for the graft.12
Graft Preparation
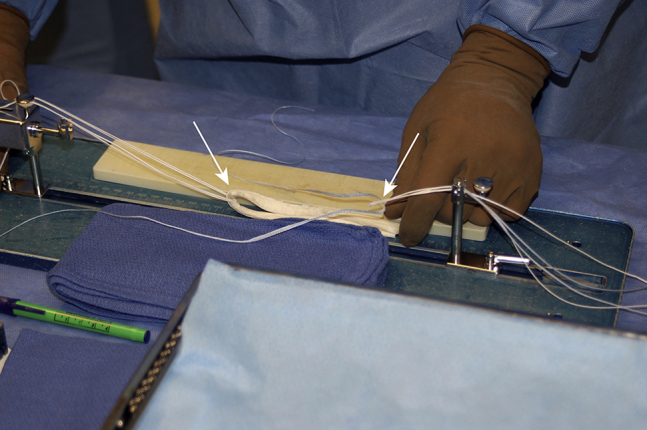
A graft-prep station assists preparation and tensioning of the graft construct. In this case, the tendon was pretensioned at approximately 70 N for 15 minutes to eliminate creep. For graft fixation, a TightRope RT loop (Arthrex) is placed on the femoral side, and a No-Button TightRope loop (Arthrex) is placed on the tibial side (Fig 1, Video 1).
Fig 1.

Graft prep station with the NoButton TightRope loop for the tibial fixation seen on the right, and the TightRope RT loop for femoral fixation seen on the left. The anterior tibialis allograft (red arrow) to be prepared is on the white board in the foreground.
A collagen-coated FiberTape is passed through the femoral TightRope loop with the 2 free ends of the tape on the tibial TightRope side. The allograft tendon is then passed through the tibial TightRope loop, and the 2 free graft ends are passed in opposite directions through the femoral TightRope loop (Fig 2, Video 1). The 2 free ends of the graft are then sutured together on the tibial side with a no. 2 FiberLoop (Arthrex) in a SpeedWhip fashion.13
Fig 2.
The anterior tibialis graft is first passed through the tibial NoButton TightRope loop (left arrow). The collagen-coated FiberTape is next passed through the femoral TightRope loop (right arrow).
The quadrupled construct is then placed under tension at approximately 70 N, and the 4 limbs are linked together using 4 wraparound type no. 2 FiberWire sutures (Arthrex). It is important that each limb of the graft is captured with this wrapping suture and the internal brace FiberTape. The 4 sutures are placed close to the TightRope loops while avoiding incorporating the loops in the process. This ensures no suture will be in the joint space. This suturing technique is done on both the femoral and tibial side. The FiberTape, now functioning as an internal brace within the middle of the construct, is not visualized because it is completely surrounded by the graft. Use of the small internal FiberTape does not add to overall graft diameter (Fig 3, Video 1). Marks are made on the graft denoting the expected length in the tibial and femoral sockets.
Fig 3.
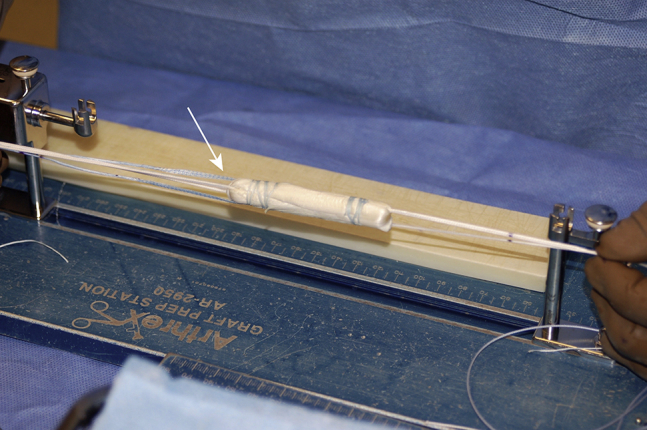
The final construct of the quadrupled anterior tibialis allograft secured by the 4 wrap-around no. 2 Fiberwire sutures. The internal brace collagen-coated FiberTape is only visible with the 2 free ends exiting out the tibial end of the graft (left, arrow).
ACL Reconstruction
All-inside ACL reconstruction is performed as described by Lubowitz.12, 14 The graft is first passed into the femoral socket and fixated with the TightRope RT suspensory button (Arthrex). Once the button passes the depth of the measured femoral intraosseous distance (as marked with methylene blue on the loop), the button flips on the lateral femoral cortex. The shortening sutures are pulled in an alternating fashion to hoist the graft into this femoral socket for secure fixation. The tibial end of the graft with the NoButton TightRope and graft sutures, along with the free ends of the internal brace FiberTape, are then passed into the tibial socket by way of a passing suture. An Attachable Button System (ABS) (Arthrex) is applied to the NoButton TightRope, and the knee is brought into full hyperextension by holding the foot. The shortening sutures from the NoButton TightRope are then secured to the ABS button for final fixation. The knee is cycled several times to additionally tension the construct, and then both the femoral and tibial TightRope shortening sutures are firmly pulled with the knee in full hyperextension for final tendon graft fixation (Fig 4). The shortening sutures from the TightRope and the 2 ends of the no. 2 FiberLoop sutures on the tibial side of the graft are tied to the button for backup fixation.
Fig 4.

The patient is lying supine with the knee flexed at 90°. The right knee is shown with the completed quadrupled anterior tibialis allograft anterior cruciate ligament construct after suspensory TightRope fixation on the femur and tibia. Again, the internal brace collagen-coated FiberTape is fully contained within the graft such that no part of the FiberTape is visible inside the joint space.
Internal Brace Fixation
Importantly, the FiberTape internal brace is tensioned independently after the graft. Once the allograft ACL has been secured on the femur and tibia, attention is directed toward final fixation of the internal brace. This is accomplished with a 4.75-mm absorbable BioComposite SwiveLock (Arthrex) (Fig 5). A guide pin is drilled 1.5 cm distal to the ABS tibial fixation button to a depth of 20 mm and reamed with a 4.5-mm reamer to a depth of 20 mm because of the SwiveLock length of 19 mm. This hole is then tapped with a 4.75-mm tap. First, making sure the 2 free ends of the FiberTape are free from the ACL graft tibial fixation button, a hemostat is placed under the FiberTape limbs, so it will not be tighter than the graft. Then, the FiberTape is fixated with the knotless SwiveLock to a depth of 19 mm in the tibia, which should always be done in full hyperextension to avoid “capturing” the joint and limiting extension. The knee should be checked at this time to ensure that full range of motion is present.
Fig 5.
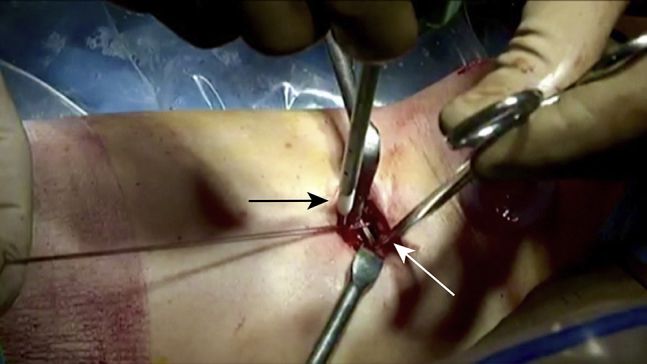
The patient remains in the supine position, and the knee is held in full hyperextension. The collagen-coated FiberTape internal brace is independently tensioned and fixated on the tibia after the anterior cruciate ligament graft fixation is completed on the tibial side. First, a hemostat is placed underneath the 2 free ends of the collagen-coated FiberTape (white arrow). Next the FiberTape ends are secured to the tibia with a biocomposite SwiveLock (Arthrex, Naples, FL) (black arrow) in full hyperextension.
Postoperatively, range of motion is instituted with use of a CPM machine, and weight-bearing is progressed as tolerated once the patient demonstrates a well-functioning quadriceps muscle and good leg control. Closed-chain strengthening is emphasized, and return to sport is typically allowed 6 to 9 months after surgery.
Discussion
This surgical technique describes the use of FiberTape as an internal brace augmentation for an allograft ACL reconstruction. The concept behind the addition of the small-diameter FiberTape relates to the additional protection the internal brace provides for the allograft during its initial revascularization and remodeling phase, which has been shown to take 12 months by Arnoczky et al. and 18 months by Shino et al.15, 16 Lubowitz et al.10 described the use of a FiberTape internal brace for medial ligament repair with a good outcome. Similarly, recent studies have shown potential biomechanical improvements involving the use of internal bracing for both a modified Broström and ulnar collateral ligament repairs.17, 18, 19
The concept of internal bracing has been described in the ankle for augmentation of a Broström repair.19, 20 The touted advantage in the ankle was to allow early range of motion and early weight-bearing to enhance functional return to normal activities. The internal brace also protects the Broström primary ligament repair so as to not compromise ultimate ankle stability during the accelerated rehabilitation process. This was validated through the significantly improved biomechanical strength that was shown in an experimental model of the Broström repair.19 Similarly, successful internal bracing for an open medial collateral ligament reconstruction has also been described.10
Allograft tissue is appealing for ACL reconstruction relative to avoidance of autograft harvest, less operative time, and less postoperative pain.1, 3 However, it has been biologically shown that allograft ACL constructs are slower to revascularize and remodel compared with autograft tissue.15, 16 Numerous studies have shown a higher failure rate for allograft reconstruction, particularly in young patients.3, 4, 5 Through the addition of an internal strut or brace, perhaps allograft tissue could be enhanced to minimize tissue elongation during the longer biologic incorporation process. In turn, this could potentially minimize ACL allograft retears. Another potential advantage of use of the FiberTape internal brace relates to augmenting small-diameter grafts, or providing additional support in a revision ACL reconstruction situation.
To be an ideal augmentation tool for intra-articular use, the internal brace device needs to be strong, low-profile, biocompatible, and nonreactive. Potential complications of artificial ligaments have been well documented with Gore-Tex grafts.7, 8 The difference with use of FiberTape as an internal brace is that it is only a small part of the soft tissue allograft construct and is not being used alone for ACL replacement. This becomes a key distinction between a FiberTape internal brace construct and the Ligament Advanced Reinforcement System (LARS). The LARS is a nonabsorbable, synthetic ligament device made of terephthalic polyethylene polyester fibers and is too ineffective when used as a stand-alone graft.21 Many previous attempts at ACL repair using synthetic grafts have used materials that have failed because of poor integration or the buildup of synthetic material within the joint space.22, 23 FiberTape has been used extensively for rotator cuff repair and has been very well tolerated.24
A major advantage in the use of the internal brace is to inherently strengthen the overall construct to protect the graft during the revascularization and remodeling process (Table 1). This is particularly true in allograft tissue, which has a slower integration period.15, 16 Independent tensioning of the FiberTape separate from the graft tensioning is very important, so the graft itself experiences load. Another advantage is confidence with an accelerated rehabilitation program with early weight-bearing, with the internal brace providing increased joint support. Finally, given that its small size and overall flexibility make it an easy material to handle intraoperatively, it is simple to loop the Fibertape to the femoral TightRope device and fixate on the tibia with a SwiveLock.
Table 1.
Advantages and Disadvantages of Anterior Cruciate Ligament Reconstruction With Internal Brace Augmentation
| Advantages | Disadvantages |
|---|---|
| Independent tensioning from graft | Potential for overconstraining the joint |
| Protects graft during healing process | Possible stress shielding of graft |
| Allows for accelerated rehabilitation | |
| Small (only 3 mm in diameter) | |
| Flexible; easy fixation | |
| Biocompatibility (rotator cuff use) |
The primary disadvantage regarding use of an internal brace would be the risk of overconstraining the joint and leading to loss of motion if the internal brace is too tight (Table 2). For this reason, the internal brace is fixated separately from the graft and always at full hyperextension. Another concern would be potential stress shielding of the graft itself, but this also can be avoided by placing a hemostat tip underneath the FiberTape at the time of tibial fixation to build in a bit of slack with the internal brace. This ensures that the graft sees load, which is important in the tissue revascularization and remodeling process.
Table 2.
Pearls and Pitfalls of Anterior Cruciate Ligament Reconstruction With Internal Brace Augmentation
| Pearls and Pitfalls |
| • Bury FiberTape within Graftlink construct. Loop FiberTape through femoral TightRope, with free ends on the tibial side, and then wrap graft tissue around it |
| • Fix anterior cruciate ligament graft on tibia first in full hyperextension and then fix FiberTape on tibia with SwiveLock in hyperextension using hemostat to ensure FiberTape is not too tight |
| • Make sure the free FiberTape ends on the tibial side do not get trapped underneath the tibial button used to fixate the graft here; otherwise, independent tensioning would be lost |
| • Do not fix with the knee flexed at all, as this could lead to loss of motion (i.e., extension) |
The authors believe a small-diameter FiberTape internal brace can safely protect an allograft during the remodeling and revascularization phase by facilitating tissue ingrowth and incorporation, potentially reducing the rate of retears in allograft reconstructions.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.A.B. received support from Arthrex for travel and accommodations for a mandatory coordinator meeting. P.A.S. serves as a consultant for and receives research support from Arthrex; receives royalties for a meniscus product from Arthrex; and has stock/stock options in Spinal Simplicity.
Supplementary Data
This video details the graft preparation and final fixation for a quadrupled GraftLink construct. The anterior tibialis allograft incorporates a collagen-coated FiberTape (Arthrex, Naples, FL) to provide additional strength and internal stability for the construct. The patient lies in a supine position with easy manipulation of the knee for the anterior cruciate ligament reconstruction as described by Lubowitz et al.12 The video includes a thoroughly narrated overview of the procedure and details as outlined in the manuscript.
References
- 1.Lawhorn K.W., Howell S.M. Scientific justification and technique for anterior cruciate ligament reconstruction using autogenous and allogeneic soft-tissue grafts. Orthop Clin North Am. 2003;34:19–30. doi: 10.1016/s0030-5898(02)00029-9. [DOI] [PubMed] [Google Scholar]
- 2.Shelton W.R., Papendick L., Dukes A.D. Autograft versus allograft anterior cruciate ligament reconstruction. Arthroscopy. 1997;13:446–449. doi: 10.1016/s0749-8063(97)90122-5. [DOI] [PubMed] [Google Scholar]
- 3.McGuire D.A., Hendricks S.D. Allograft tissue in ACL reconstruction. Sports Med Arthrosc. 2009;17:224–233. doi: 10.1097/JSA.0b013e3181c0cf8a. [DOI] [PubMed] [Google Scholar]
- 4.Barrett G.R., Luber K., Replogle W.H., Manley J.L. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy. 2010;26:1593–1601. doi: 10.1016/j.arthro.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 5.Bottoni C.R., Smith E.L., Shaha J. Autograft versus allograft anterior cruciate ligament reconstruction: A prospective, randomized clinical study with a minimum 10-year follow-up. Am J Sports Med. 2015;43:2501–2509. doi: 10.1177/0363546515596406. [DOI] [PubMed] [Google Scholar]
- 6.Waterman B.R., Johnson D.H. Synthetic grafts—Where is the common sense? Arthroscopy. 2015;31:1849–1850. doi: 10.1016/j.arthro.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 7.Dahlstedt L., Dalen N., Jonsson U. Goretex prosthetic ligament vs. Kennedy ligament augmentation device in anterior cruciate ligament reconstruction. A prospective randomized 3-year follow-up of 41 cases. Acta Orthop Scand. 1990;61:217–224. doi: 10.3109/17453679008993504. [DOI] [PubMed] [Google Scholar]
- 8.Batty L.M., Norsworthy C.J., Lash N.J., Wasiak J., Richmond A.K., Feller J.A. Synthetic devices for reconstructive surgery of the cruciate ligaments: A systematic review. Arthroscopy. 2015;31:957–968. doi: 10.1016/j.arthro.2014.11.032. [DOI] [PubMed] [Google Scholar]
- 9.Lubowitz J.H. Editorial commentary: Synthetic ACL grafts are more important than clinical nonbelievers may realize. Arthroscopy. 2015;31:969–970. doi: 10.1016/j.arthro.2015.02.039. [DOI] [PubMed] [Google Scholar]
- 10.Lubowitz J.H., MacKay G., Gilmer B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc Tech. 2014;3:e505–e508. doi: 10.1016/j.eats.2014.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheffler S.U., Schmidt T., Gangey I., Dustmann M., Unterhauser F., Weiler A. Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: Delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy. 2008;24:448–458. doi: 10.1016/j.arthro.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Lubowitz J.H., Ahmad C.S., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 13.White K.L., Camire L.M., Parks B.G., Corey W.S., Hinton R.Y. Krackow locking stitch versus locking premanufactured loop stitch for soft-tissue fixation: A biomechanical study. Arthroscopy. 2010;26:1662–1666. doi: 10.1016/j.arthro.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 14.Lubowitz J.H., Schwartzberg R., Smith P. Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy. 2013;29:1195–1200. doi: 10.1016/j.arthro.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 15.Arnoczky S.P., Tarvin G.B., Marshall J.L. Anterior cruciate ligament replacement using patellar tendon. An evaluation of graft revascularization in the dog. J Bone Joint Surg Am. 1982;64:217–224. [PubMed] [Google Scholar]
- 16.Shino K., Inoue M., Horibe S., Nagano J., Ono K. Maturation of allograft tendons transplanted into the knee. An arthroscopic and histological study. J Bone Joint Surg Br. 1988;70:556–560. doi: 10.1302/0301-620X.70B4.3403597. [DOI] [PubMed] [Google Scholar]
- 17.Dugas J.R., Walters B.L., Beason D.P., Fleisig G.S., Chronister J.E. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified jobe reconstruction. Am J Sports Med. 2016;44:735–741. doi: 10.1177/0363546515620390. [DOI] [PubMed] [Google Scholar]
- 18.Schuh R., Benca E., Willegger M. Comparison of Brostrom technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2016;24:1101–1107. doi: 10.1007/s00167-015-3631-7. [DOI] [PubMed] [Google Scholar]
- 19.Viens N.A., Wijdicks C.A., Campbell K.J., Laprade R.F., Clanton T.O. Anterior talofibular ligament ruptures, part 1: Biomechanical comparison of augmented Brostrom repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 2014;42:405–411. doi: 10.1177/0363546513510141. [DOI] [PubMed] [Google Scholar]
- 20.Cho B.K., Park K.J., Kim S.W., Lee H.J., Choi S.M. Minimal invasive suture-tape augmentation for chronic ankle instability. Foot Ankle Int. 2015;36:1330–1338. doi: 10.1177/1071100715592217. [DOI] [PubMed] [Google Scholar]
- 21.Tiefenboeck T.M., Thurmaier E., Tiefenboeck M.M. Clinical and functional outcome after anterior cruciate ligament reconstruction using the LARS system at a minimum follow-up of 10 years. Knee. 2015;22:565–568. doi: 10.1016/j.knee.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 22.Klein W., Jensen K.U. Synovitis and artificial ligaments. Arthroscopy. 1992;8:116–124. doi: 10.1016/0749-8063(92)90145-2. [DOI] [PubMed] [Google Scholar]
- 23.Prescott R.J., Ryan W.G., Bisset D.L. Histopathological features of failed prosthetic Leeds-Keio anterior cruciate ligaments. J Clin Pathol. 1994;47:375–376. doi: 10.1136/jcp.47.4.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hug K., Gerhardt C., Haneveld H., Scheibel M. Arthroscopic knotless-anchor rotator cuff repair: A clinical and radiological evaluation. Knee Surg Sports Traumatol Arthrosc. 2015;23:2628–2634. doi: 10.1007/s00167-014-3026-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video details the graft preparation and final fixation for a quadrupled GraftLink construct. The anterior tibialis allograft incorporates a collagen-coated FiberTape (Arthrex, Naples, FL) to provide additional strength and internal stability for the construct. The patient lies in a supine position with easy manipulation of the knee for the anterior cruciate ligament reconstruction as described by Lubowitz et al.12 The video includes a thoroughly narrated overview of the procedure and details as outlined in the manuscript.


