A 23-year-old Caucasian woman developed simultaneous onset longitudinally extensive transverse myelitis (LETM; figure, A.a) and left optic neuritis. She had no significant neurologic history, but her brother had MS. At nadir, she had Medical Research Council grade 2/5 power in the lower limbs and a sensory level at T4. MRI of the brain identified lesions within the right middle cerebellar peduncle (figure, A.b) and adjacent to the posterior horn of the left lateral ventricle (figure, A.c). Oligoclonal bands were present in the CSF, and serum autoantibodies to aquaporin-4 and myelin oligodendrocyte glycoprotein were absent on repeated testing 2 months apart. Visual evoked potentials were abnormal only on the left. Seronegative neuromyelitis optica spectrum disorder (NMOSD) was diagnosed1 and treated with corticosteroids, but she relapsed 2 months later. Azathioprine was added to steroids but she relapsed again 4 months later. Repeat MRI showed fragmentation of the LETM into multiple short cord lesions (figure, B.a) and 2 new juxtaventricular lesions in the brain (figure, B.b and c), more in keeping with MS than NMOSD. She was initiated on natalizumab and has remained without new clinical events for the last 12 months. MRI was repeated 8 months into treatment with natalizumab and confirmed that there were no new lesions.
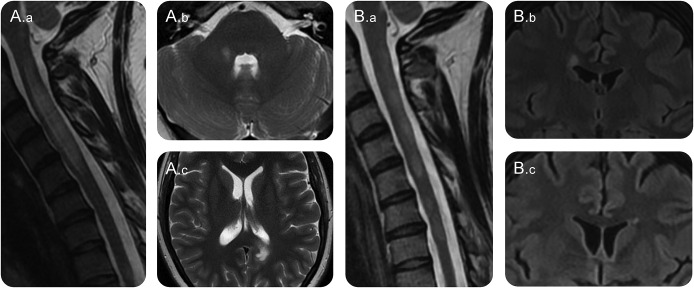
Figure. Sequential cervical cord and brain MRIs at presentation (A.a–c) and 6 months later (B.a–c).
(A.a) Longitudinally extensive T2-hyperintensity within the spinal cord from C1 to the lower border of C5. (A.b) Lesion within the right middle cerebellar peduncle. (A.c) Lesion adjacent to the posterior horn of the left lateral ventricle. (B.a) Longitudinally extensive transverse myelitis has fragmented into multiple discrete short lesions within the cervical cord. (B.b) New lesion adjacent to the body of the right lateral ventricle. (B.c) New lesion adjacent to the body of the left lateral ventricle.
Discussion.
LETM (myelitis extending over 3 or more vertebral segments) with optic neuritis is considered the sine qua non of NMOSD. By contrast, spinal cord lesions in MS are usually less than 1 vertebral segment in length. However, long myelitis can occur in MS too. It was present in approximately 3% of patients in 2 large case series2,3 and was the presenting demyelinating episode in only 0.7% of cases.3 Contiguous multiple short lesions with edema can also give the appearance of LETM.
In this case, the presentation of optic neuritis and long myelitis led to the diagnosis of NMOSD, but in hindsight, there were several features that could support the diagnosis of MS had it not been for the LETM: Caucasian ethnicity, family history of MS, CSF oligoclonal bands, MS-typical brain lesions, and poor response to azathioprine combined with high-dose corticosteroids. Lesions adjacent to the body of the lateral ventricles (as in the figure, panels B.b and c) are highly sensitive and specific for MS over NMOSD.4 The prompt remission on natalizumab, a drug that is known to be associated with worsening of NMOSD,5 is also supportive of the diagnosis of relapsing-remitting MS.
This case demonstrates a rare radiologic manifestation of MS mimicking a classical presentation of the much rarer NMOSD. The correct diagnosis became clear with time and sequential imaging. In the absence of aquaporin-4 autoantibodies, accurate differentiation between these 2 disorders is not always straightforward, and given that many disease-modifying treatments for MS can exacerbate NMOSD, it is sometimes reasonable to treat with conventional immunosuppressant medications until more certain of the diagnosis.6 While neurologists have become sensitive about the possibility of NMO mimicking MS over the last decade, the possibility of MS masquerading as NMO needs to be periodically considered in all cases of seronegative NMOSD, particularly those remaining unresponsive to treatments.
Acknowledgments
Acknowledgment: The UK NMO Service is funded by the highly specialized commissioning group of NHS England.
Footnotes
Author contributions: Daniel Whittam, Maneesh Bhojak, and Kumar Das: drafting and revising the manuscript. Anu Jacob: study concept and drafting and revising the manuscript.
Study funding: No targeted funding.
Disclosure: D. Whittam, M. Bhojak, and K. Das report no disclosures. A. Jacobs served on the scientific advisory board for Shire Pharmaceuticals; received travel funding and/or speaker honoraria from Biogen Idec, Shire, and Terumo BCT; consulted for Shire Pharmaceuticals; and received research support from Biogen, Alexion Pharmaceuticals, NHS, and University of Liverpool. Go to Neurology.org/nn for full disclosure forms. The Article Processing Charge was paid by the authors.
References
- 1.Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology 2006;66:1485–1489. [DOI] [PubMed] [Google Scholar]
- 2.Bot JC, Barkhof F, Polman CH, et al. Spinal cord abnormalities in recently diagnosed MS patients: added value of spinal MRI examination. Neurology 2004;62:226–233. [DOI] [PubMed] [Google Scholar]
- 3.Qiu W, Wu JS, Zhang MN, et al. Longitudinally extensive myelopathy in Caucasians: a West Australian study of 26 cases from the Perth Demyelinating Diseases Database. J Neurol Neurosurg Psychiatry 2010;81:209–212. [DOI] [PubMed] [Google Scholar]
- 4.Matthews L, Marasco R, Jenkinson M, et al. Distinction of seropositive NMO spectrum disorder and MS brain lesion distribution. Neurology 2013;80:1330–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacob A, Hutchinson M, Elsone L, et al. Does natalizumab therapy worsen neuromyelitis optica? Neurology 2012;79:1065–1066. [DOI] [PubMed] [Google Scholar]
- 6.Palace J, Leite I, Jacob A. A practical guide to the treatment of neuromyelitis optica. Pract Neurol 2012;12:209–214. [DOI] [PubMed] [Google Scholar]