Abstract
We report a typical case of “tennis leg”, in which the main finding was a fluid collection between the medial head of the gastrocnemius and soleus muscles. Since the first clinical description of this entity in 1883, the injury has been attributed to rupture of the plantaris tendon. However, recent studies of this condition with sonography and magnetic resonance imaging have shown that most of these cases are actually due to injury to the gastrocnemius and/or soleus muscles, and up to 10% are due to deep venous thrombosis masquerading as muscle injury. The plantaris muscle and tendon are only rarely involved in this injury.
Keywords: Tennis leg, Plantaris tendon, Gastrocnemius, Deep vein thrombosis
Introduction
“Tennis leg” refers to acute mid-calf pain, which is a common sports-associated injury, usually experienced by middle-aged persons, incurred with extension of the knee and forced dorsiflexion of the ankle [1]. This entity can occur during many activities, but was first described in a tennis player in 1883, where it was attributed to rupture of the plantaris tendon [2]. The plantaris tendon has continued to be implicated in this injury for many years [1], [2]. However, more recent research suggests that far more common causes of tennis leg are rupture of the medial head of the gastrocnemius, fluid between the gastrocnemius and soleus muscles without evidence of muscle injury, and even deep vein thrombosis [1]. Determining the cause of symptoms affects clinical management and patient prognosis, especially in patients with deep vein thrombosis. We report a typical case of tennis leg, in which the main finding was a fluid collection between the medial head of the gastrocnemius and soleus muscles.
Case report
A 57-year-old male experienced acute mid-calf pain, while throwing a Frisbee. He reported hearing and feeling a “snapping” sensation posterior to his knee, followed by immediate swelling and an inability to bear weight. He was initially seen at an outside emergency department, where he was placed in a cam boot. The patient was seen in clinic 3 weeks after the initial injury, where he reported an improvement in pain and a decrease in swelling. During this visit, the clinician noted ecchymosis tracking down his right lower extremity associated with mild swelling. On physical examination, there was no limitation in flexion or extension of the knee, and ankle range of motion was appropriate in all planes. There was an increased pain in the mid-calf with dorsiflexion, as well as on palpation.
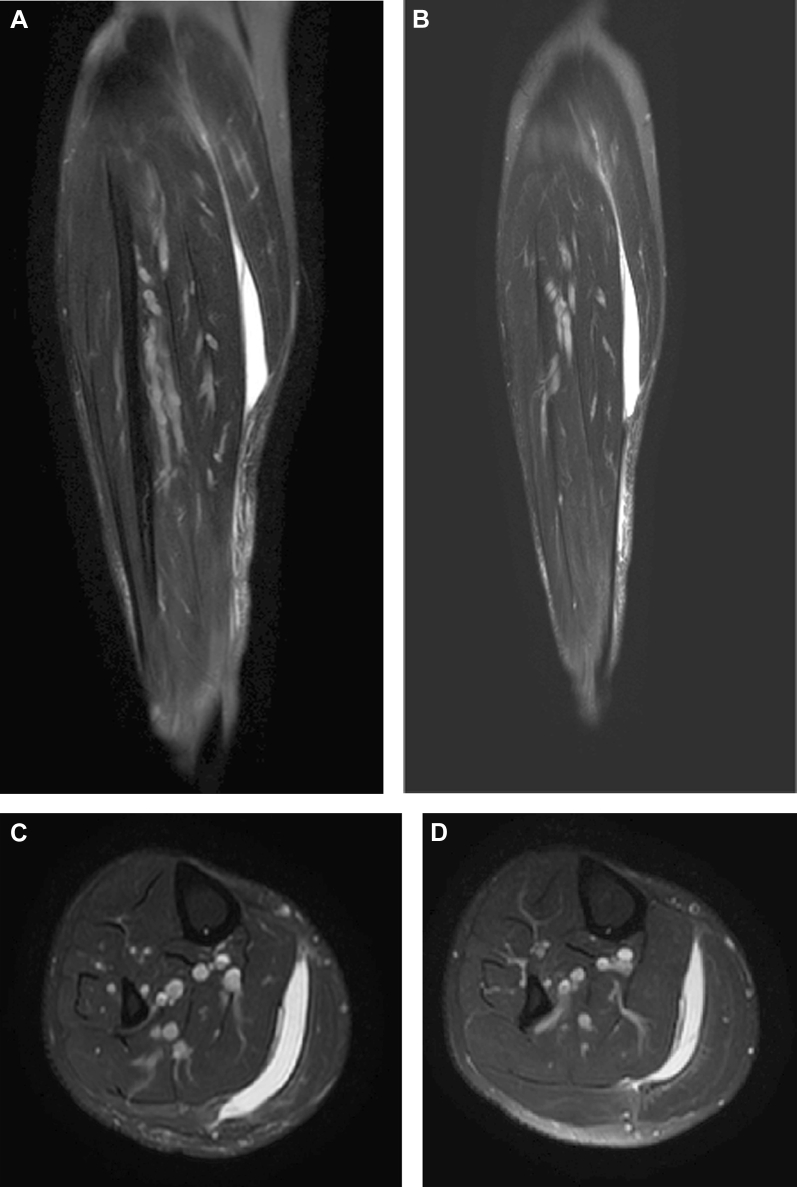
A magnetic resonance imaging (MRI) of the right tibia and fibula was performed, without contrast (Fig. 1). This demonstrated crescentic T1-hypointense and T2-hyperintense fluid collection, located between the medial head of the gastrocnemius and soleus. Mildly increased subcutaneous T2 signal was noted along the lower leg. There was no evidence of plantaris or gastrocnemius muscle rupture.
Fig. 1.
MRI of the right calf. (A and B) Coronal T2-weighted fat-suppressed images show a hyperintense fluid collection between the medial head of the gastrocnemius and soleus. Increased subcutaneous T2 signal is noted along the lower leg. (C and D) Axial T2-weighted fat-suppressed images show a hyperintense fluid collection between the medial head of the gastrocnemius and soleus.
Discussion
The plantaris is an accessory muscle, absent in 7%-20% of the population [1]. It assists with plantar flexion of the calf muscle and is commonly harvested by surgeons for tendon grafts [3]. The plantaris composes part of the posterosuperficial compartment of the calf. In association with the gastrocnemius and soleus muscles, it forms the triceps surae unit [1]. The plantaris muscle belly is approximately 7-13 cm in length [4]. It originates from the lateral supracondylar line of the femur and inserts onto the calcaneus [1]. The muscle belly originates superior to both the medial and lateral heads of the gastrocnemius and lies deep to the lateral head of the gastrocnemius [1]. The plantaris myotendinous junction occurs at the level of origin of the soleus muscle [4]. The plantaris tendon courses toward the medial aspect of the lower extremity, running between the medial head of the gastrocnemius and the soleus muscle [1]. It courses near the medial border of the Achilles tendon (in some cases fusing with it) and inserts onto the calcaneus, anteromedially to the Achilles tendon [1]. Because it spans 2 joints, the knee and the ankle, the plantaris may have an increased likelihood of injury [3].
The gastrocnemius is the most superficial muscle of the calf and is composed of 2 muscle heads. The medial head originates from the posterior medial femoral condyle and the lateral head originates from the posterior lateral femoral condyle. The 2 heads unite and form an aponeurosis, which combines with the soleus aponeurosis to form the Achilles tendon. The Achilles inserts onto the posterior calcaneus [5].
“Tennis leg” was first described by Powell in 1883 [2]. The classic presentation is acute mid-calf pain in a middle-aged person. This is most often a sports-associated injury, incurred during extension of the knee and forced dorsiflexion of the ankle. Often, a “snapping” sensation is both felt and heard by the patient [1], [6]. For many years, the pathophysiology of tennis leg was attributed to rupture of the plantaris tendon [1]. Although rupture of the plantaris is possible, injury to the medial head of the gastrocnemius or injury to the gastrocnemius-soleus aponeurosis are far more common causes of tennis leg.
Delgado et al presented the sonographic findings in 141 patients with the clinical diagnosis of tennis leg. These findings were retrospectively reviewed to determine the underlying pathology. Partial rupture of the medial head of the gastrocnemius was noted in 66.7% of patients. Fluid collection, without evidence of muscle rupture, was noted between the aponeuroses of the gastrocnemius and the soleus in 21.3% of patients. Deep vein thrombosis was seen in conjunction with another finding in 5% of patients and as a solitary finding in 9.9% of patients. Actual plantaris tendon rupture occurred in 1.4% of patients and partial rupture of the soleus was seen in 0.7% of patients [1].
In both plantaris and gastrocnemius rupture, fluid collection between the medial head of the gastrocnemius and the soleus is common [3], [5], [7]. However, with rupture of the plantaris tendon, it is suggested that the retracted muscle belly should be visualized on MRI and may appear as a mass-like structure [3], [4], [5].
Up to 10% of patients with the classic clinical presentation of tennis leg may have unsuspected deep vein thrombosis [1]. Thus, during sonography of tennis leg, it is essential to include Doppler to rule out a thrombosis [3]. If MRI is being performed, arterial and venous patency should be analyzed. Failing to identify and treat a deep vein thrombosis could result in a life-threatening pulmonary embolism. Another consideration with a clinical presentation similar to that of tennis leg is rupture of a popliteal cyst. In such cases, the documentation of fluid extending from the joint in between the medial head of the gastrocnemius and the semimembranosus can be a helpful diagnostic feature [3].
Patients with plantaris tendon rupture, or the far more common gastrocnemius rupture, are almost always treated conservatively [8]. Surgery is only indicated when associated with compartment syndrome, for which fasciotomy is necessary [3], [8]. Compartment syndrome in association with gastrocnemius rupture is most often a result of direct muscle trauma or heavy exercise [9].
In conclusion, the classic clinical presentation of tennis leg is only rarely associated with an actual rupture of the plantaris tendon. Far more common causes are rupture of the medial head of the gastrocnemius muscle or injury to the gastrocnemius-soleus aponeurosis, without evidence of muscle rupture, as seen in our patient. Finally, up to 10% of patients presenting with tennis leg may actually have deep vein thrombosis, a potentially life-threatening condition.
Footnotes
Acknowledgments: No funding source was used for this submission.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Delgado G.J., Chung C.B., Lektrakul N., Azocar P., Botte M.J., Coria D. Tennis leg: clinical US study of 141 patients and anatomic investigation of four cadavers with MR imaging and US. Radiology. 2002;224:112–119. doi: 10.1148/radiol.2241011067. [DOI] [PubMed] [Google Scholar]
- 2.Powell R.W. Lawn tennis leg. Lancet. 1883;122(3123):44. [Google Scholar]
- 3.Rohilla S., Jain N., Yadav R. Plantaris rupture: why is it important? BMJ Case Rep. 2013;2013:1–3. doi: 10.1136/bcr-2012-007840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Helms C.A., Fritz R.C., Garvin G.J. Plantaris muscle injury: evaluation with MR imaging. Radiology. 1995;195:201–203. doi: 10.1148/radiology.195.1.7892469. [DOI] [PubMed] [Google Scholar]
- 5.Pacheco R.A., Stock H. Tennis leg: mechanism of injury and radiographic presentation. Conn Med. 2013;77:427–430. [PubMed] [Google Scholar]
- 6.Russell A.S., Crowther S. Tennis leg – a new variant of an old syndrome. Clin Rheumatol. 2011;30:855–857. doi: 10.1007/s10067-011-1681-x. [DOI] [PubMed] [Google Scholar]
- 7.Kwak H.S., Han Y.M., Lee S.Y., Kim K.N., Chung G.H. Diagnosis and follow-up US evaluation of ruptures of the medial head of the gastrocnemius (‘tennis leg’) Korean J Radiol. 2006;7:193–198. doi: 10.3348/kjr.2006.7.3.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwak H.S., Lee K.B., Han Y.M. Ruptures of the medial head of the gastrocnemius (‘tennis leg’): clinical outcome and compression effect. Clin Imaging. 2006;30:48–53. doi: 10.1016/j.clinimag.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Tao L., Jun H., Muliang D., Deye S., Jiangdong N. Acute compartment syndrome after gastrocnemius rupture (tennis leg) in a nonathlete without trauma. J Foot Ankle Surg. 2016;55(2):303–305. doi: 10.1053/j.jfas.2014.09.022. [DOI] [PubMed] [Google Scholar]