Abstract
Study objective
The emergency department (ED) is an inherently high-risk setting. Our objective is to identify the factors associated with the combined poor outcome of either death or an ICU admission shortly after ED discharge in older adults.
Methods
We conducted chart review of 600 ED visit records among adults older than 65 years that resulted in discharge from any of 13 hospitals within an integrated health system in 2009 to 2010. We randomly chose 300 patients who experienced the combined outcome within 7 days of discharge and matched case patients to controls who did not experience the outcome. Two emergency physicians blinded to the outcome reviewed the records and identified whether a number of characteristics were present. Predictors of the outcome were identified with conditional logistic regression.
Results
Of 1,442,594 ED visits to Kaiser Permanente Southern California in 2009 to 2010, 300 unique cases and 300 unique control records were randomly abstracted. Characteristics associated with the combined poor outcome included cognitive impairment (adjusted odds ratio [AOR] 2.10; 95% confidence interval [CI] 1.19 to 3.56), disposition plan change (AOR 2.71; 95% CI 1.50 to 4.89), systolic blood pressure less than 120 mm Hg (AOR 1.48; 95% CI 1.00 to 2.20), and pulse rate greater than 90 beats/min (AOR 1.66; 95% CI 1.02 to 2.71).
Conclusion
We found that older patients discharged from the ED with a change in disposition from “admit” to “discharge,” cognitive impairment, systolic blood pressure less than 120 mm Hg, and pulse rate greater than 90 beats/ min were at increased risk of death or ICU admission shortly after discharge. Increased awareness of these high-risk characteristics may improve ED disposition decisionmaking.
INTRODUCTION
The elderly have the highest rate of emergency department (ED) use among all adults.1 A poor outcome such as death or an ICU admission shortly after discharge from the ED can be considered a catastrophic event. Although such poor outcomes after discharge have important patient safety, quality improvement, and medicolegal implications, there is insufficient understanding of factors leading to such events, especially in older adults. To our knowledge, this is the first case-control chart review analysis using clinical records to identify factors associated with poor outcomes after ED discharge in older patients. Identifying these factors is an important first step toward improvement in ED or follow-up care.
Previous studies conducted by our study team,2–5 as well as other authors,6,7 used clinical data to identify predictors of poor outcomes after ED discharge and were an important first step in understanding this association. Yet these studies were limited in that they were qualitative and were hypothesis generating or the researchers did not have direct access to patient records and could not identify patient and process-of-care characteristics that were inherent to the encounter.2,3,6,7 The objective of this study was to extract data from patient records by using a matched case-control review analysis and identify patient and process-of-care factors that may be associated with early death or ICU admission within 7 days of discharge from the ED visit.
MATERIALS AND METHODS
Study Design
We conducted a matched case-control study of patients older than 65 years who died or experienced an ICU admission within 7 days of an ED evaluation and discharge. Such studies can have increased power at a fraction of the cost of cohort studies and are particularly valuable for studying relatively rare outcomes. The study protocol was approved by the institutional review boards of Kaiser Permanente Southern California and the University of California at Los Angeles.
Setting
Study subjects were members of Kaiser Permanente Southern California, an integrated health system that provides comprehensive care to 3.7 million members throughout Southern California. Health care was delivered at approximately 200 outpatient clinics, and emergency services were provided at 13 medical centers at the study.
All health plan members had similar health care benefits, including coverage of emergency services both within and outside the health system. Electronic health records tracked all health care encounters within the health system and provided access to notes, vital signs, laboratory results, pharmacy, imaging, and many other clinical care data. A claims reimbursement system tracked health care encounters at outside facilities. A specialized administrative database provided information on the use of hospice services.
Selection of Participants
Potentially eligible subjects were patients older than 65 years who were treated and discharged from any of 13 Kaiser Permanente Southern California EDs between January 1, 2009, and December 31, 2010 (n=1,552,594 visits of n=922,005 patients). Death within 7 days of the ED discharge was identified with the California Vital Statistics files and the Social Security Death Index. ICU admission was identified through the Kaiser Permanente Southern California electronic health record. We chose the 7-day time frame because of its clinical relevance, implications for health policy decisions, and use in previous related studies.3,6–9
Each subject had to be a member of the health plan at the ED visit; no minimum health plan enrollment period was required. Non–Kaiser Permanente Southern California member visits (n=286,484) were excluded, as well as patient visits with missing sex and birth date (n=59 visits) and visits of patients younger than 65 years (n=955,845). Visits by patients who received hospice care were also excluded (n=12,414 visits) on the assumption that this status implies an intention to provide end-of-life comfort therapy rather than prolong life and that death would not be considered necessarily an adverse outcome. Patients transferred from the ED to outside hospitals were also excluded (n=3,621 visits). Patient ED visits that resulted in death in the ED during the visit were excluded (n=3,581 visits). In addition, patient ED visits involving direct admission from the ED to an inpatient bed or to observations care were excluded (n=109,817 visits). After application of all exclusion criteria electronically, the eligible study sample was n=180,773 visits of n=104,025 members.
After the application of exclusion criteria, we identified 1,055 eligible cases, defined as visits of patients older than 65 years who were treated at a Kaiser Permanente Southern California ED and either died or had an ICU admission within 7 days of discharge. In accordance with previous literature2,4,5 and clinical judgment, we then matched all case patients to eligible controls 1:1, using a daisy cluster algorithm that allows all variable types to be matched, not just numeric variables,10 without replacement according to the following parameters: age, sex, Emergency Severity Index11 score, Charlson comorbidity index score,12 and discharge diagnosis. Sex, Emergency Severity Index score, and discharge diagnosis were perfect matches. Age (in years) and the Charlson comorbidity index score were allowed to match at 1 integer above or below. There were 171,108 eligible controls, defined as patients treated in an ED and discharged but who did not experience death or an ICU visit within 7 days. There were a total of 1,027 case-control visit pairs.
Of the 1,027 case-control visit pairs, a research assistant manually reviewed randomly selected ones until she arrived at 300 eligible case-control pairs. We chose to limit the analysis to 300 pairs because of a power calculation explained below.
Although they were randomly selected, case-control visit pairs were manually excluded if they met any of the following criteria: transfer from the ED to a different facility (7 pairs), presence of do not resuscitate or do not intubate orders (40 pairs), no emergency physician note (4 pairs), and duplicate patients (6 pairs). After the manual exclusion, we generated a list of 300 case patients and 300 controls accessible only by the research assistant.
The candidate abstraction instrument measures were developed by members of the study team (G.Z.G., M.K.G., and C.A.S.) according to previous work conducted by G.Z.G.2,3 and to previous literature.13–16 We considered only measures that could be ascertained reliably by the 2 chart abstractors through the review of clinical records and that had a κ>0.6.17,18 Measures addressed the patient’s presentation, such as cognition or location or level of pain; or the care that was delivered, such as the use of a consultant or change in disposition plan. Vital signs were recorded for patients electronically and not abstracted manually. Vital signs chosen for the analysis were those closest to discharge.
Methods of Measurement
We used standard chart review methods described by Gilbert et al.19 Two attending emergency physicians (N.P. and K.A.D.) who worked at a Kaiser Permanente Southern California hospital and had access to its computers during the study period performed the chart abstraction. Before initiation of the project, the chart abstractors met with the principal investigator (G.Z.G.) multiple times to train in chart review methodology, as well as how to use the standardized abstraction instrument. During these training sessions, they reviewed 20 sample Kaiser Permanente Southern California cases with the principal investigator (G.Z.G.) to confirm that they evaluate records reliably and in an organized manner. Throughout the training and study itself, the abstractors remained blinded to the study objectives and whether records were of case patients or controls.
The data were collected by a research assistant who was not aware of the study objectives. The research assistant created PDFs of deidentified ED records void of patient identifying information that did not include information about whether records were of case patients or controls. Bimonthly, the research assistant sent electronic PDFs to the chart abstractors through the Kaiser Permanente intranet.
Chart abstractors were advised to ascertain measures from the ED provider note in either the chief complaint, history of present illness, and physical examination section or the portion on physician decisionmaking. For questions involving pain (abdominal or chest pain) or a sign-out of care, chart abstractors were also asked to evaluate the nurse’s note to obtain more information. For all measures, chart abstractors were asked to indicate whether the measure was present or absent. If there was no mention of a complaint or condition, then the chart abstractors documented that the complaint or condition was not present. For example, if a chart did not contain mention of a change in cognition, then the reviewer recorded that there was no change. If a chart had conflicting information such that the nurse’s note or the consultant note provided differing information about the patient’s presentation, complaint, or examination, the abstractors were trained to use only information provided in the ED provider note.
If chart abstractors were unable to answer the questions of the standardized abstraction measure questionnaire, they were given the following additional training about how to interpret the chart:
Cognitive Impairment or Change in Mental Status: Present if the provider mentioned an acute or chronic change in cognition or personality
Fall: Present if there was an unintentional ground impact from a seated or standing position
Vital Signs: Present if there was any discussion or documentation of vital signs within the note
Chest Radiograph: Present if, on ordering of a radiograph, a “different” reading required different ED management. If one part of the management was a portion of the other, then that was considered a “same” reading. A same reading also included whether either reading consisted of a portion of the other.
Chest Pain: Present if there was any complaint of pain, pressure, or discomfort in the area underlying the ribs
Abdominal Pain: Present if there was any complaint of pain, pressure, or discomfort in the area below the ribs and above the pelvis, excluding leg pain of any kind
Disposition Change: Present if there was any notation of the consideration or plan to admit the patient to an inpatient bed
Ill: Present if there was mention of “ill appearing,” “distressed,” or “toxic” in the physical examination section or remainder of the provider note
Sign-out: Present if there was any mention of a physician-to-physician sign-out or communication or conveying the care of the patient to another emergency physician provider. This was also present if there were 2 or more provider names on the ED provider note.
Consultation: Present if there was any mention of discussion (either in person or on the telephone) with a consultant or the formal use of a consultant that resulted in a note’s being placed in the patient’s chart. A consultant was defined as a Kaiser Permanente Southern California physician of a specialty other than the ED providers themselves.
Symptomatic: If the physician note did not directly mention that the patient’s symptoms had improved, then he or she was considered to have the same symptoms at discharge
Throughout the chart abstraction period, the chart abstractors and the principal investigator met regularly to resolve disputes and review coding rules.
Primary Data Analysis
We first looked for an association between the candidate abstraction instrument measures and the combined poor outcome. We summarized the outcome as a function of patient characteristics. Using vital sign ranges for adults, we created preliminary models that assessed the association of vital signs with admission after discharge. Members of the project team (G.Z.G., M.K.G., and C.A.S.) dichotomized each vital sign into 2 categories: normal versus abnormal. No case patients or controls had missing systolic blood pressure or pulse rate recordings.
We tested the combined poor outcome within 7 days of discharge for independence with each measure, using McNemar’s test for discrete variables with 2 categories. We used a conditional logistic regression for race or ethnicity, vital signs, and radiograph, and paired t tests for continuous variables. Two patients with unknown race or ethnicity were included in the referent category of white.
All measures were included in a full conditional logistic regression model (“full model”) evaluating the association with death or ICU admission (combined poor outcome), death only, and ICU admission only. In addition, all measures that were statistically significantly related to the combined poor outcome at P<.05 in unadjusted analyses were included in a conditional logistic regression model (“selective model”) to assess the relationship between predictors and all 3 outcomes (the combined poor outcome of death or an ICU admission, death only, and ICU admission only). For patients who experienced both death and ICU admission, the visits were included in the model that evaluated characteristics associated with death only because we did not want to count these patient visits 2 times. All data management and analysis was performed with SAS (version 9.3; SAS Institute, Inc., Cary, NC).
Our power analysis was based on estimations from previous literature.20,21 The calculation assumed a simple bivariate relationship and did not account for multiple testing. The calculation was based on the following: if the true odds ratio for a poor outcome within 7 days in case subjects relative to controls was 1.8, we needed to study approximately 300 case-patient visits with 1 matched control per case to be able to reject the null hypothesis with a power of 0.8 and type I error of 0.5.
RESULTS
Characteristics of Study Subjects
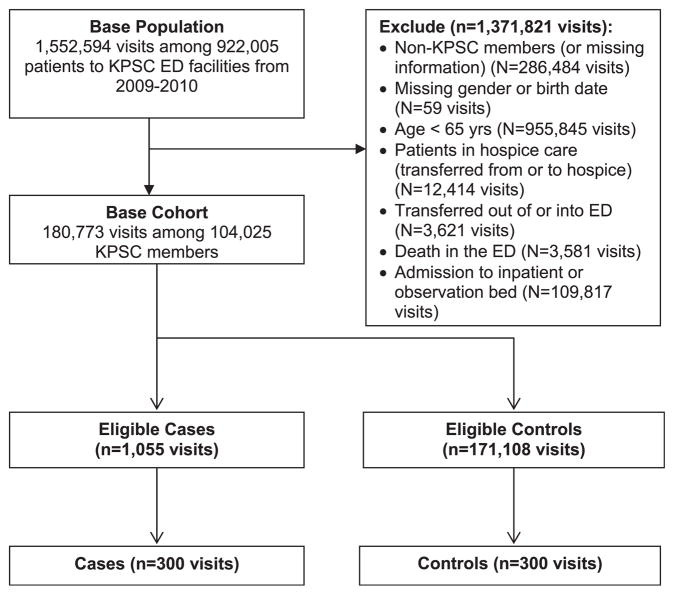
As illustrated in the Figure, the eligible sample included 180,773 visits among 104,025 patients, of whom 300 case patients were randomly selected and matched to 300 controls. Characteristics of the case patients and controls are presented in Table 1. There were statistically significant differences between case patients and controls in race or ethnicity, systolic blood pressure, and pulse rate. Of the combined poor outcome of death or ICU admission in the case-patient visits, there were 67 deaths, 211 ICU admissions, and 22 patient visits that resulted in both.
Figure.
Study cohort flowchart.
Table 1.
Descriptive characteristics of case patients and controls.
| Measure | Case Patients, No. (%) | Controls, No. (%) | Group Difference* |
|---|---|---|---|
| Race/ethnicity†‡ | |||
| White | 167 (55.7) | 164 (54.7) | [Reference] |
| Asian/Pacific Islander | 32 (10.7) | 15 (5.0) | 2.13 (1.09 to 4.15) |
| Black | 44 (14.7) | 69 (23.0) | 0.62 (0.40 to 0.98) |
| Hispanic | 57 (19.0) | 52 (17.3) | 1.05 (0.67 to 1.64) |
| Vital signs | |||
| BP, mean (SD) | 131.7 (21.3) | 136.2 (21.4) | −4.5 (−7.79 to −1.22) |
| Pulse rate, mean (SD) | 78.6 (15.0) | 75.3 (12.4) | 3.3 (1.04 to 5.47) |
| Systolic BP 91–119 | 86 (28.7) | 70 (23.3) | 1.31 (0.91 to 1.89) |
| Systolic BP ≥120 (ref) | 214 (71.3) | 230 (76.7) | [Reference] |
| Pulse rate >90 beats/min‡ | 56 (18.7) | 32 (10.7) | 1.86 (1.17 to 2.94) |
| Pulse rate 38–90 (ref) | 244 (81.3) | 268 (89.3) | [Reference] |
| Matched measure | |||
| Median age, IQR, y | 76, 11 | 77, 11 | N/A |
| Sex, (% female) | 132 (44) | 132 (44) | N/A |
| Emergency Severity Index | |||
| 2 (emergency) | 14 (4.7) | 14 (4.7) | N/A |
| 3 (urgent) | 240 (80) | 240 (80) | N/A |
| 4 (nonurgent) | 45 (15) | 45 (15) | N/A |
| 5 (minor) | 1 (0.3) | 1 (0.3) | N/A |
| Charlson comorbidity index | |||
| 0 | 18 (6) | 18 (6) | N/A |
| 1–2 | 42 (14) | 42 (14) | N/A |
| 3–4 | 70 (23.3) | 70 (23.3) | N/A |
| 5–6 | 61 (36.3) | 61 (36.3) | N/A |
| ≥7 | 109 (36.3) | 109 (36.3) | N/A |
| Discharge diagnosis (35) | — | — | |
IQR, Interquartile range; SD, standard deviation.
Group difference was calculated according to conditional logistic regression for discrete variables and paired t test for continuous variables.
Two patients with unknown race or ethnicity were included in the referent category of white.
P<.05. The P value was calculated according to McNemar’s test for discrete variables with 2 categories: conditional logistic regression for race or ethnicity, and paired t test for continuous variables.
Main Results
In Table 2, we present the abstraction instrument measures. In unadjusted analyses, the following were associated with a combined poor outcome of death or ICU admission: presence of cognitive impairment or acute or chronic mental status changes, a fall in the 30 days before the ED visit, change in disposition plan by either the patient or the provider (from a disposition of “admit” to “discharge”), and the use of a specialty consultant either with or without a consultant note in the chart. For change in disposition plan, the breakdown of disposition plan change by the physician or patient (also known as against medical advice) was the following: change in disposition by physician, 19 of 48 controls and 29 of 48 case patients; and change in disposition by patient, 6 of 48 controls and 18 of 48 case patients.
Table 2.
Candidate abstraction instrument measures.
| Question* | Case Patients, No. (%) | Controls, No. (%) | Group Difference† |
|---|---|---|---|
| Mental status change‡ | |||
| No | 253 (84.3) | 273 (91.0) | [Reference] |
| Yes | 47 (15.7) | 27 (9.0) | 1.91 (1.14–3.20) |
| Fall‡ | |||
| No | 250 (83.3) | 263 (87.7) | [Reference] |
| Yes | 50 (16.7) | 37 (12.3) | 2.08 (1.05–4.15) |
| Note addressing vital signs | |||
| No | 32 (10.7) | 22 (7.3) | [Reference] |
| Discussed | 10 (3.3) | 9 (3.0) | 0.65 (0.36–1.16) |
| Specific vital signs documented | 258 (86.0) | 269 (89.7) | 0.77 (0.26–2.27) |
| Different emergency physician reading of radiograph compared with radiology | 196 (65.3) | 212 (70.7) | [Reference] |
| Radiograph was not obtained | |||
| Different radiograph readings | 14 (4.7) | 14 (4.7) | 1.11 (0.51–2.41) |
| Same or similar radiograph readings | 90 (30.0) | 74 (24.7) | 1.46 (0.95–2.24) |
| Abdominal pain at discharge | |||
| No | 281 (93.7) | 273 (91.0) | [Reference] |
| Yes | 19 (6.3) | 27 (9.0) | 0.62 (0.31–1.24) |
| Chest pain at discharge | |||
| No | 286 (95.3) | 275 (91.7) | [Reference] |
| Yes | 14 (4.7) | 25 (8.3) | 0.52 (0.26–1.05) |
| Change in disposition plan‡ | |||
| No | 253 (84.3) | 275 (91.7) | [Reference] |
| Yes | 47 (15.7) | 25 (8.3) | 2.22 (1.27–3.88) |
| Patient not well appearing | |||
| No | 281 (93.7) | 287 (95.7) | [Reference] |
| Yes | 19 (6.3) | 13 (4.3) | 1.46 (0.72–2.96) |
| Sign out of care | |||
| No | 278 (92.7) | 280 (93.3) | [Reference] |
| Yes | 22 (7.3) | 20 (6.7) | 1.11 (0.59–2.10) |
| Consultation obtained‡ | |||
| No | 206 (68.7) | 229 (76.3) | [Reference] |
| Yes | 94 (31.3) | 71 (23.7) | 1.52 (1.04–2.23) |
| Symptomatic at discharge | |||
| No | 117 (39.0) | 105 (35.0) | [Reference] |
| Yes | 183 (61.0) | 195 (65.0) | 0.81 (0.56–1.17) |
The full question is included in the abstraction instrument in Appendix E1, available online at http://www.annemergmed.com.
Group difference was calculated according to conditional logistic regression.
P<.05. The P value was calculated according to McNemar’s test for discrete variables with 2 categories and conditional logistic regression for vital signs and radiograph.
Table 3 presents adjusted odds ratios (AORs) of the selective model variables and the combined poor outcome of death or ICU admission, death only, and ICU admission only in the following variables that were significant: race or ethnicity, vital sings of systolic blood pressure and pulse rate, and the abstraction instrument measures of cognitive impairment or change in mental status and change in disposition plan. Table E1 (available online at http://www.annemergmed.com) presents the AORs of all the full model variables and their association with the combined poor outcome of death or ICU admission, death only, and ICU admission only within 7 days of discharge from the ED.
Table 3.
Selective model of conditional logistic regression results.*
| Characteristics† | AOR (95% CI) for Death or ICU Admission | AOR (95% CI) for Death | AOR (95% CI) for ICU Admission |
|---|---|---|---|
| Race/ethnicity‡ | |||
| Asian/Pacific Islander | 2.13 (1.05–4.33) | 1.08 (0.19–5.95) | 2.74 (1.17–6.40) |
| Black | 0.68 (0.42–1.08) | 1.14 (0.33–4.04) | 0.61 (0.36–1.04) |
| Hispanic | 1.02 (0.64–1.62) | 0.65 (0.26–1.64) | 1.25 (0.70–2.24) |
| Vital signs | |||
| Systolic BP, mm Hg | |||
| <120§ | 1.48 (0.99–2.20) | 5.51 (1.98 –15.3) | 1.09 (0.68–1.73) |
| Pulse rate, beats/min | |||
| >90|| | 1.66 (1.02–2.71) | 2.97 (1.07–8.23) | 1.49 (0.82–2.69) |
| Abstraction instrument measures¶ | |||
| Mental status change | 2.10 (1.19–3.56) | 12.74 (3.14–51.63) | 0.99 (0.50–1.94) |
| Change in disposition plan | 2.71 (1.50–4.89) | 10.42 (2.28–47.67) | 2.0 (1.001–4.00) |
CI, Confidence interval.
Results are shown for the combined outcome of death or ICU admission, death only, and ICU admission only. Patient visits that resulted in both death and ICU admission were included in the death category to avoid their being counted 2 times.
All characteristics presented in this table were variables in the model.
Referent group: white race/ethnicity.
Referent group: systolic blood pressure greater than 120 mm Hg.
Reference group: pulse rate of 38 to 90 beats/min.
Reference group: no cognitive impairment or change in mental status and no change in disposition plan.
In the selective model, evaluating the association of characteristics with the combined poor outcome, having systolic blood pressure less than 120 mm Hg (AOR 1.48; 95% confidence interval [CI] 1.00 to 2.20) and pulse rate greater than 90 beats/min (AOR 1.66; 95% CI 1.02 to 2.71) were associated with death or ICU admission. Both vital signs were also associated with death only (systolic blood pressure <120 mm Hg, AOR 5.51, 95% CI 1.98 to 15.3; pulse rate >90 beats/min, AOR 2.97, 95% CI 1.07 to 8.23), whereas no vital signs were associated with ICU admission only. Cognitive impairment or change in mental status (AOR 2.10; 95% CI 1.19 to 3.56) and change in disposition plan (AOR 2.71; 95% CI 1.50 to 4.89) were associated with a combined poor outcome. There was also an association for death only (mental status change AOR 12.74, 95% CI 3.14 to 51.63; change in disposition plan AOR 10.42, 95% CI 2.28 to 47.67). For the outcome of ICU admission, only change in disposition plan was associated with the outcome. For the combined poor outcome, race or ethnicity was associated with the outcome; specifically, Asian/Pacific Islanders were more likely to sustain the outcome compared with whites (AOR 2.13; 95% CI 1.05 to 4.33). Asian/Pacific Islanders were also more likely to have an ICU admission only (AOR 2.74; 95% CI 1.17 to 6.40).
In the selective model of the combined poor outcome of death or ICU admission, specialty consultation was also associated with the outcome; however, including specialty consultation in the model caused “change in disposition plan” to be nonsignificant. Inspection showed that obtaining a consultant and change in disposition were in agreement in 88% of cases; thus, we omitted consultation from the final models because obtaining a consultation had a lower odds ratio associated with the combined poor outcome.
Comparison of the selective and full models showed that they were similar, except that when all the variables were included in the model (full model), the association of Asian/Pacific Islander and change in disposition plan with ICU admission only no longer remained significant.
LIMITATIONS
Our study has limitations. First, our results may not generalize to other settings. Although demographic characteristics of this managed care population are similar to those of the surrounding population in Southern California,22 our patient population may not match those of other regions. Furthermore, health plan members may have access to rapid outpatient evaluation that may not be available to the general population, and as a consequence, the practice patterns of emergency physicians in our study EDs may differ from those of other health systems. Second, vital signs are continuous measures that were dichotomized for this analysis. Third, the ability to abstract charts was limited by the thoroughness and content of the chart. In addition, lack of signs or symptoms, such as cognition, may not be accurately documented in an ED chart. Fourth, although we excluded patients receiving hospice care, this study did not distinguish between expected outcomes and unexpected ones. It also did not identify outcomes related to the initial ED visit.
DISCUSSION
We found that patients with a change in disposition plan (from admit to discharge), acute or chronic cognitive impairment or mental status changes, and systolic blood pressure less than 120 mm Hg and pulse rate greater than 90 beats/min had a greater likelihood of experiencing death or an ICU admission within 7 days of ED discharge. Our study identifies clinical characteristics and management decisions that are associated with poor outcomes after ED discharge. Our study also reaffirms the importance of vital signs and, to our knowledge, serves as the first case-control analysis to evaluate records of ED visits of patients older than 65 years who experience poor outcomes after discharge.
In our sample of discharged older adults, the change in disposition plan from admit to discharge could be directed by the ED provider or by the patient’s leaving the ED against medical advice. We found the change in disposition plan to be associated with the combined poor outcomes of death or ICU admission, death only, and ICU admission only. We also found that when all the variables were included in the model, change in disposition plan was no longer associated with ICU admission. Previous studies have found that patients who leave the ED against medical advice are more likely to experience poor outcomes after discharge, such as worsening of their medical condition or admission.23–26 Our findings, coupled with that of other studies, suggest that regardless of the initiating event causing the change in disposition status, the emergency providers’ clinical judgment about the disposition (admit versus discharge) of the patient should be given special attention by both the care team and the patient.27,28 The change in disposition could be a joint decision made by both the patient and provider. Understanding the factors leading to a change in disposition could improve care.
In our chart review analysis, we found that a specialty consultation and change in disposition plan were related. When one was in the model, the other no longer remained significant. This suggests that the presence of a specialty consultation likely results in a change in the disposition plan or that a change in disposition plan caused the introduction of a specialty consultation. Specialty consultants are an integral part of the emergency care delivery system. They provide care, services, and follow-up that are outside of an emergency provider’s training and scope of practice. Although previous studies on consultation services for the ED are sparse,29 they have found that close to 1 of 3 ED patients requires consultation services.30 In our sample, 28% of patients required consultation services. Although the services of consultants are important, our findings suggest that ED provider decisions should not be based solely on consultant recommendations and should include the ED providers’ intuition as well.
We also found that older adults with an acute change in mental status or chronic cognitive impairment were more likely to experience a combined poor outcome. Change in mental status was also associated with the outcome of death only. This is possibly due to patients having a difficult time understanding discharge instructions or changes in medications or due to ED providers not being well trained in the care of these patients. It could also signal that a change in mental status is indicative of significant changes in the life course. Previous studies have found that a small number of ED providers detect and document cognitive impairment in older adults in the ED setting15,31 and that, for patients in whom cognitive deficits were recognized, the management plan was not altered.15 This could be attributed to numerous factors such as the time it takes to conduct a cognitive assessment, as well as an uncertainty about how to manage such patients. The Mini-Mental State Examination has high sensitivity and specificity for detecting cognitive impairment, yet even with only a dozen items it is considered to be cumbersome. The Six-Item Screener has been reported to have sensitivity comparable to that of the Mini-Mental State Examination while taking less time to administer.32,33 Because ED providers or the ancillary staff may not have a predetermined plan about how to manage these patients, EDs, ED managers, and follow-up services should consider creating preset disposition plans for them.
We found that abnormal vital signs in older adults were associated with the combined poor outcome. Systolic blood pressure less than 120 mm Hg was associated with either death or an ICU admission and had a high association with death only shortly after discharge. This is consistent with previous literature that has found low blood pressure to be associated with poor outcomes.34–36 This finding suggests that in an ED setting, patients with reduced systolic blood pressure warrant further scrutiny before discharge. We also found that an elevated pulse rate greater than 90 beats/min was associated with the outcome. This is consistent with previous literature that has found lower pulse rate to be cardioprotective and associated with a lower likelihood of experiencing poor outcomes.37,38
Compared with non-Hispanic whites, Asian/Pacific Islanders were more likely to have a combined poor outcome. This racial group was also more likely to experience an ICU admission alone in the selective model, although in the full model with all the variables, the association with ICU admission alone was no longer significant. In 2 studies conducted by the primary author (G.Z.G.) evaluating short-term outcomes after ED discharge, compared with white race or ethnicity, race or ethnicity was not associated with being admitted to the hospital5 or with mortality.3 Although not validated by literature, the findings in this study suggest that older adults of different ethnicities may have differing social support services, have a higher threshold for visiting the ED, or be subject to racial bias when evaluated in the ED.
We found that older adults who present to the ED with acute or chronic cognitive impairment, change in ED disposition plan, and systolic blood pressure less than 120 mm Hg and pulse rate greater than 90 beats/min were at increased risk for death or an ICU admission within 7 days of ED discharge. Our findings suggest that EDs use higher scrutiny when managing patients with cognitive impairment and emergency providers address abnormal vital signs before discharge while being especially cautious when a change in disposition plan is initiated by the patient or care team.
Supplementary Material
Acknowledgments
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist and provided the following details: This research and Dr. Gabayan were supported by the National Institutes of Health (NIH), National Center for Research Resources, National Center for Advancing Translational Science, and the University of California at Los Angeles Clinical and Translational Science Institute (grant KL2TR000122). Dr. Gabayan is currently supported by the National Institute on Aging (NIA) Grant for Early Medical/Surgical Specialists Transition to Aging Research (GEMSSTAR R03AG047862-01). Dr. Sarkisian is supported by the NIA (1K24AG047899-01).
Footnotes
Author contributions: GZG conceived the study and obtained funding. MKG, JPJ, JRH, and CAS aided in the design of the study and supervised its conduct. SCY managed the data. REW and VYC provided statistical advice and analyzed the data. NP and KAD conducted the chart reviews. GZG drafted the article and all authors contributed substantially to its revision. GZG takes responsibility for the paper as a whole.
References
- 1.Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Rep. 2010;26:1–31. [PubMed] [Google Scholar]
- 2.Gabayan GZ, Sun BC, Asch SM, et al. Qualitative factors in patients who die shortly after emergency department discharge. Acad Emerg Med. 2013;20:778–785. doi: 10.1111/acem.12181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gabayan GZ, Derose SF, Asch SM, et al. Patterns and predictors of short-term death after emergency department discharge. Ann Emerg Med. 2011;58:551–558. e552. doi: 10.1016/j.annemergmed.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gabayan GZ, Sarkisian CA, Liang LJ, et al. Predictors of admission after emergency department discharge in older adults. J Am Geriatr Soc. 2015;63:39–45. doi: 10.1111/jgs.13185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gabayan GZ, Asch SM, Hsia RY, et al. Factors associated with short-term bounce-back admissions after emergency department discharge. Ann Emerg Med. 2013;62:136–144. doi: 10.1016/j.annemergmed.2013.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kefer MP, Hargarten SW, Jentzen J. Death after discharge from the emergency department. Ann Emerg Med. 1994;24:1102–1107. doi: 10.1016/s0196-0644(94)70239-x. [DOI] [PubMed] [Google Scholar]
- 7.Sklar DP, Crandall CS, Loeliger E, et al. Unanticipated death after discharge home from the emergency department. Ann Emerg Med. 2007;49:735–745. doi: 10.1016/j.annemergmed.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 8.Gunnarsdottir OS, Rafnsson V. Death within 8 days after discharge to home from the emergency department. Eur J Public Health. 2008;18:522–526. doi: 10.1093/eurpub/ckn045. [DOI] [PubMed] [Google Scholar]
- 9.Guttmann A, Schull MJ, Vermeulen MJ, et al. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983. doi: 10.1136/bmj.d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gower JC. A comparison of some methods of cluster analysis. Biometrics. 1967;23:623–637. [PubMed] [Google Scholar]
- 11.Wuerz RC, Milne LW, Eitel DR, et al. Reliability and validity of a new five-level triage instrument. Acad Emerg Med. 2000;7:236–242. doi: 10.1111/j.1553-2712.2000.tb01066.x. [DOI] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Mehta KM, Yaffe K, Covinsky KE. Cognitive impairment, depressive symptoms, and functional decline in older people. J Am Geriatr Soc. 2002;50:1045–1050. doi: 10.1046/j.1532-5415.2002.50259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tilvis RS, Kahonen-Vare MH, Jolkkonen J, et al. Predictors of cognitive decline and mortality of aged people over a 10-year period. J Gerontol A Biol Sci Med Sci. 2004;59:268–274. doi: 10.1093/gerona/59.3.m268. [DOI] [PubMed] [Google Scholar]
- 15.Hustey FM, Meldon SW, Smith MD, et al. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med. 2003;41:678–684. doi: 10.1067/mem.2003.152. [DOI] [PubMed] [Google Scholar]
- 16.Beach C, Croskerry P, Shapiro M. Profiles in patient safety: emergency care transitions. Acad Emerg Med. 2003;10:364–367. doi: 10.1111/j.1553-2712.2003.tb01350.x. [DOI] [PubMed] [Google Scholar]
- 17.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Measurement. 1960;20:37–46. [Google Scholar]
- 18.Maclure M, Willett WC. Misinterpretation and misuse of the kappa statistic. Am J Epidemiol. 1987;126:161–169. doi: 10.1093/aje/126.2.161. [DOI] [PubMed] [Google Scholar]
- 19.Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27:305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 20.Gabayan GZ, Derose SF, Asch SM, et al. Patterns and predictors of short-term death after emergency department discharge. Ann Emerg Med. 2011;58:551–558. doi: 10.1016/j.annemergmed.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nunez S, Hexdall A, Aguirre-Jaime A. Unscheduled returns to the emergency department: an outcome of medical errors? Qual Saf Health Care. 2006;15:102–108. doi: 10.1136/qshc.2005.016618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koebnick C, Langer-Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16:37–41. doi: 10.7812/tpp/12-031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gabayan GZ, Hsia RY, Zingmond D, et al. Factors associated with short-term bounce-back admissions following emergency department discharge. Ann Emerg Med. 2013;62:136–144. doi: 10.1016/j.annemergmed.2013.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ding R, Jung JJ, Kirsch TD, et al. Uncompleted emergency department care: patients who leave against medical advice. Acad Emerg Med. 2007;14:870–876. doi: 10.1197/j.aem.2007.06.027. [DOI] [PubMed] [Google Scholar]
- 25.Henson VL, Vickery DS. Patient self discharge from the emergency department: who is at risk? Emerg Med J. 2005;22:499–501. doi: 10.1136/emj.2003.005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pennycook AG, McNaughton G, Hogg F. Irregular discharge against medical advice from the accident and emergency department—a cause for concern. Arch Emerg Med. 1992;9:230–238. doi: 10.1136/emj.9.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White AL, Armstrong PA, Thakore S. Impact of senior clinical review on patient disposition from the emergency department. Emerg Med J. 2010;27:262–265. 296. doi: 10.1136/emj.2009.077842. [DOI] [PubMed] [Google Scholar]
- 28.Guly HR. Diagnostic errors in an accident and emergency department. Emerg Med J. 2001;18:263–269. doi: 10.1136/emj.18.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee RS, Woods R, Bullard M, et al. Consultations in the emergency department: a systematic review of the literature. Emerg Med J. 2008;25:4–9. doi: 10.1136/emj.2007.051631. [DOI] [PubMed] [Google Scholar]
- 30.Cortazzo JM, Guertler AT, Rice MM. Consultation and referral patterns from a teaching hospital emergency department. Am J Emerg Med. 1993;11:456–459. doi: 10.1016/0735-6757(93)90082-m. [DOI] [PubMed] [Google Scholar]
- 31.Hustey FM, Meldon SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002;39:248–253. doi: 10.1067/mem.2002.122057. [DOI] [PubMed] [Google Scholar]
- 32.Wilber ST, Lofgren SD, Mager TG, et al. An evaluation of two screening tools for cognitive impairment in older emergency department patients. Acad Emerg Med. 2005;12:612–616. doi: 10.1197/j.aem.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 33.Callahan CM, Unverzagt FW, Hui SL, et al. Six-Item Screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Duran L, Balci K, Kati C, et al. Has admission blood pressure any prognostic value in patients with subarachnoid hemorrhage? an emergency department experience. J Clin Hypertens (Greenwich) 2013;15:737–741. doi: 10.1111/jch.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lalezarzadeh F, Wisniewski P, Huynh K, et al. Evaluation of prehospital and emergency department systolic blood pressure as a predictor of in-hospital mortality. Am Surg. 2009;75:1009–1014. doi: 10.1177/000313480907501032. [DOI] [PubMed] [Google Scholar]
- 36.Lipsky AM, Gausche-Hill M, Henneman PL, et al. Prehospital hypotension is a predictor of the need for an emergent, therapeutic operation in trauma patients with normal systolic blood pressure in the emergency department. J Trauma. 2006;61:1228–1233. doi: 10.1097/01.ta.0000196694.52615.84. [DOI] [PubMed] [Google Scholar]
- 37.Hsia J, Larson JC, Ockene JK, et al. Resting heart rate as a low tech predictor of coronary events in women: prospective cohort study. BMJ. 2009;338:b219. doi: 10.1136/bmj.b219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ho JE, Bittner V, Demicco DA, et al. Usefulness of heart rate at rest as a predictor of mortality, hospitalization for heart failure, myocardial infarction, and stroke in patients with stable coronary heart disease (data from the Treating to New Targets [TNT] trial) Am J Cardiol. 2010;105:905–911. doi: 10.1016/j.amjcard.2009.11.035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.