Abstract
The postpartum period offers multiple opportunities for healthcare providers to assist with family planning decision making. However, there are also many changing factors during the first year after delivery that can affect family planning choices. Given that several different documents have addressed WHO guidance on postpartum family planning, the electronic WHO Postpartum Family Planning Compendium (http://srhr.org/postpartumfp) has been introduced. This resource integrates essential guidance on postpartum family planning for clinicians, program managers, and policy makers. The development of the Compendium included consultations with family planning experts, key international stakeholders, and web developers. Once the website had been created, user testing by family planning experts allowed for improvements to be made before the official launch. Future directions are adaptation of the website into a mobile application that can be more easily integrated to low‐resource settings, and translation of the content into French and Spanish.
Keywords: Contraception, Postpartum family planning, Provider counseling tools
Short abstract
The WHO Postpartum Family Planning Compendium is an electronic tool that integrates WHO guidance on postpartum family planning.
1. Introduction
Up to two‐thirds of women would like to avoid pregnancy in the first year after a delivery but are not using contraception.1, 2 This unmet need is an important public health concern, because approximately 20% of obstetric deaths are attributable to non‐use of modern contraception.3 Additionally, family planning has the potential to avert maternal and child morbidity by allowing couples to space their pregnancies more than 2 years apart.4, 5
Providers have traditionally given women postpartum family planning recommendations approximately 6 weeks after delivery. However, the immediate postpartum period (within 48 hours of delivery) is an ideal time to address family planning needs, given that women are often in contact with the medical system and can be assured that they are not pregnant. Furthermore, the extension of family planning services through the first year after delivery is appropriate in view of the changing needs and preferences of women during this period. For example, a change in a woman's breastfeeding status could trigger a need for initiation of a family planning method. The postpartum period provides women important opportunities of contact with the health system, during times of care for themselves and their newborns, and women can be highly motivated to initiate contraceptive methods at these times. These opportunities—whether part of routine or emergency care—should be taken to provide life‐saving family planning services.
However, the postpartum period is a complex time for family planning decision making. Recommendations on the timing and safety of hormonal and non‐hormonal contraceptive initiation are influenced by many changing factors: breastfeeding status, uterine involution, venous thromboembolism risk, and—in the case of intrauterine devices—expulsion risk. For program managers and policy makers, decisions about which methods will be available at the point of care (either at delivery or at outpatient visits) are influenced by women's interest in particular methods, clinician recommendations, and their own knowledge regarding safety and efficacy of each method.
To date, guidance on family planning in the postpartum period has been included in various WHO documents,6, 7, 8, 9, 10, 11 each of which focuses on a different aspect of family planning care. Providers have substantial time constraints at the point of patient care, and need quickly accessible and comprehensive references. Therefore, the WHO Postpartum Family Planning Compendium was developed with the aim of creating a user‐friendly platform for WHO guidance regarding postpartum family planning in one web‐based location for use by clinicians, program managers, and policy makers.
2. Development of the Compendium
Creation of the WHO Postpartum Family Planning Compendium started with a proposal by the WHO Department of Reproductive Health and Research at a meeting for stakeholders in postpartum family planning in Chiang Mai, Thailand, in June 2015. At this meeting, two potential web‐based formats for the Compendium were presented to stakeholders from 16 countries: one format presented all contraceptive methods in pictorial form as a homepage, whereas the second presented the methods in a Gantt chart format, organized by timepoint in the first year after delivery. Stakeholders provided feedback on the formats, and were asked to prioritize medical conditions for inclusion, indicate their preferred platforms (internet, mobile application, non‐internet computer program, paper pamphlet), identify the potential target audience, and suggest source guidance documents.
On the basis of stakeholder feedback, the Gantt chart format for presentation of information was used, and medical and other conditions for inclusion were determined. The stakeholder feedback, as well as input from medical and media consultants, allowed creation of a sitemap and webpage mock‐ups.
In September 2015, a second meeting was held in Geneva, Switzerland, with a working group of content and production experts, who reviewed webpage mock‐ups and finalized content for the site. A medical consultant then integrated all postpartum family planning content from six resources into the Compendium:
WHO. Medical eligibility criteria for contraceptive use, fifth edition. 2015.9
WHO. Selected practice recommendations for contraceptive use, second edition. 2004.6
WHO. Family planning/contraception: fact sheet. 2015.11
WHO. Ensuring human rights in the provision of contraceptive information and services: guidance and recommendations. 2014.8
WHO. Hormonal contraceptive methods for women at high risk of HIV and living with HIV: 2014 Guidance Statement. 2014.12
WHO. WHO recommendations on postnatal care for the mother and newborn. 2013.7
Once the website was created, user testing was conducted at the Implementing Best Practices Conference in Washington, D.C., USA, on December 10, 2015. Content experts in family planning were approached to provide feedback regarding initial impressions, understanding of the website's audience, ability to navigate and find information of interest, and ability to complete specific relevant tasks. Tasks tested included finding recommended contraceptive methods for particular clinical scenarios.
On the basis of the results of user testing, the web content, navigation features, and web presentation were revised. The official launch of the Compendium coincided with the International Conference on Family Planning in Bali, Indonesia, on January 26, 2016. The launch of the WHO Postpartum Family Planning Compendium included a press conference and a hands‐on workshop session for users to practice with clinical scenarios.
3. Using the Compendium
The Compendium's homepage (http://srhr.org/postpartumfp) consists of two sections: (1) dropdown menus that allow the user to select characteristics of a woman in the postpartum period needing family planning services, and (2) a chart of family planning methods arranged by timing eligibility in the postpartum period (Fig. 1). The user selects comorbid conditions, breastfeeding status, and personal characteristics (e.g. smoking or adolescence) that could affect a woman's eligibility for a specific method, and selects the timing in the year after delivery. The user can then click on each family planning method to see whether the woman in question is eligible for that method on the basis of the characteristics selected. Both general information on the contraceptive method and relevant information from WHO family planning guidelines are then displayed (Box 1). The user‐friendly interface allows for easy toggling between conditions and among contraceptive methods .
Figure 1.
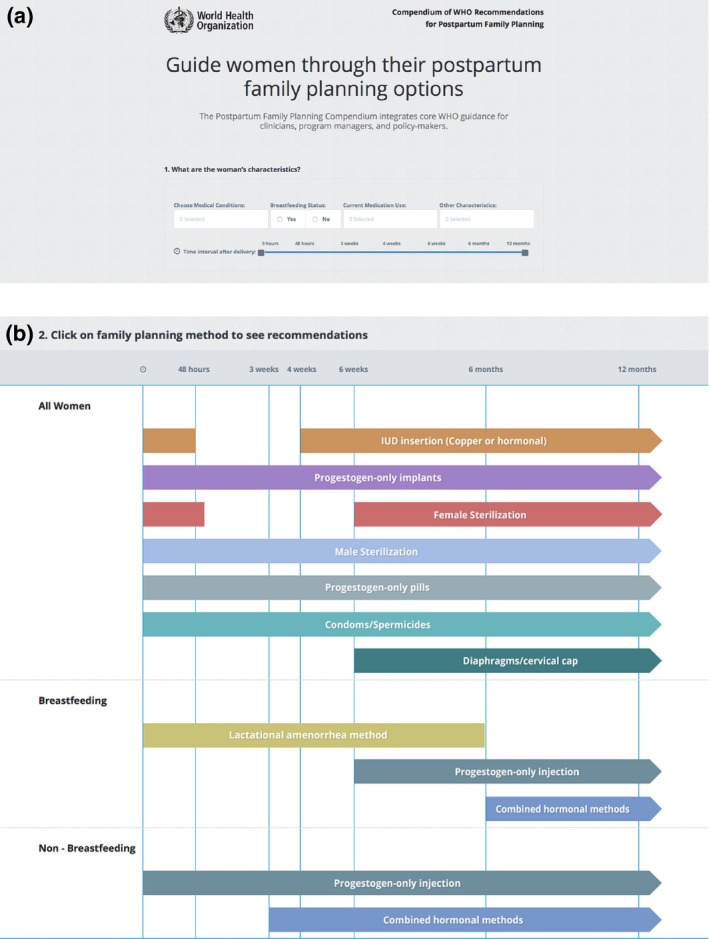
Screenshots of the Compendium's homepage. (a) Dropdown menus allowing selection of a woman's relevant characteristics. (b) Chart of family planning methods arranged by postpartum timing eligibility.
Box 1. An example of using the WHO Postpartum Family Planning Compendium.
1.
A 16‐year‐old girl taking medication for a seizure disorder who delivered 3 months ago has been brought to the family planning clinic by her mother. She has been breastfeeding her baby exclusively until now and is amenorrheic, but is returning to school and is not sure she will continue breastfeeding exclusively. She is asking if she can have an intrauterine device placed.
Is an intrauterine device (IUD) appropriate for this patient?
-
1
Navigate to http://srhr.org/postpartumfp.
-
2Set conditions from dropdown boxes:
- Choose medical condition: No condition from dropdown menu is applicable.
- Breastfeeding Status: “No.”
- Current Medications “Anticonvulsants.”
- Other characteristics: “Adolescents.”
-
3
Set time since delivery: Set interval to 6 weeks to 6 months.
-
4
Click on “IUD insertion (Copper or Hormonal)” in the method chart.
Search Results
General information regarding the IUD is shown, including a description, mechanism, effectiveness, and comments. Medical Eligibility Criteria Categories are presented on the basis of the selected conditions. For non‐breastfeeding women, IUDs are Category 1 when placed greater than or equal to 4 weeks after delivery, Category 1 for women concurrently using anticonvulsants, and Category 2 for adolescents. Definitions of the categories can be obtained by clicking an icon next to the category heading, and Clarifications/Special Considerations, if applicable, are presented. Based on the Medical Eligibility Criteria Categories, the user may conclude that the girl is eligible for an IUD.
4. Expected Outcomes and Future Directions
It is hoped that the WHO Postpartum Family Planning Compendium will see swift and widespread uptake among clinicians, program managers, and policy makers. It is recognized that the Compendium's need for internet connection and its limitation to the English language could be barriers to use in low‐resource settings. As a result, an adaptation of the tool is being developed for a mobile application, and French and Spanish translations of the content will be prepared. This will allow use on smartphones without dependence on connectivity, and allow the potential for geolocation which takes into account language, cultural, and access differences in populations. There are many other barriers to contraceptive use such as cost, access, confidentiality, and tolerance of adverse effect that are not currently addressed in this tool. With further user testing and planned research on the efficacy and influence of the tool, continued updates and incorporation of additional elements (such as other languages) are planned.
This resource could have the potential to change women's lives by improving their access to evidence‐based family planning methods in the postpartum period. Please visit the website (http://srhr.org/postpartumfp) to start using this resource today.
Conflict of Interest
The authors have no conflicts of interest.
Acknowledgments
The present work was funded through a grant from the Bill & Melinda Gates Foundation.
References
- 1. Ross J, Winfrey W. Contraceptive use, intention to use and unmet need during the extended postpartum period. Int Fam Plan Perspect. 2001;27:20–27. [Google Scholar]
- 2. Rossier C, Bradley SE, Ross J, Winfrey W. Reassessing unmet need for family planning in the postpartum period. Stud Fam Plann. 2015;46:355–367. [DOI] [PubMed] [Google Scholar]
- 3. Collumbien M, Gerressu M, Cleland J. Non‐use and use of ineffective methods of contraception In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, eds. Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attibutable to Selected Major Risk Factors. Geneva: World Health Organization; 2004. [Google Scholar]
- 4. DaVanzo J, Hale L, Razzaque A, Rahman M. Effects of interpregnancy interval and outcome of the preceding pregnancy on pregnancy outcomes in Matlab, Bangladesh. BJOG. 2007;114:1079–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DaVanzo J, Hale L, Razzaque A, Rahman M. The effects of pregnancy spacing on infant and child mortality in Matlab, Bangladesh: how they vary by the type of pregnancy outcome that began the interval. Popul Stud (Camb). 2008;62:131–154. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization . Selected practice recommendations for contraceptive use, second edition. [WHO website]. 2004. http://www.who.int/reproductivehealth/publications/family_planning/9241562846index/en/. Accessed April 25, 2016.
- 7. World Health Organization . WHO recommendations on postnatal care for the mother and newborn. [WHO website]. 2013. http://www.who.int/maternal_child_adolescent/documents/postnatal-care-recommendations/en/. Accessed April 25, 2016. [PubMed]
- 8. World Health Organization . Ensuring human rights in the provision of contraceptive information and services: guidance and recommendations. [WHO website]. 2014. http://who.int/reproductivehealth/publications/family_planning/human-rights-contraception/en/. Accessed April 25, 2016. [PubMed]
- 9. World Health Organization . Medical eligibility criteria for contraceptive use, fifth edition. [WHO website]. August 2015. http://who.int/reproductivehealth/publications/family_planning/MEC-5/en/. Accessed April 25, 2016.
- 10. World Health Organization . Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice, 3rd edn Geneva, Switzerland: World Health Organization; 2015. [PubMed] [Google Scholar]
- 11. World Health Organization . Family planning/contraception: fact sheet. [WHO website]. May 2015. http://www.who.int/mediacentre/factsheets/fs351/en. Accessed July 1, 2016.
- 12. World Health Organization . Hormonal contraceptive methods for women at high risk of HIV and living with HIV: 2014 Guidance Statement. [WHO website]. July 2014. http://www.who.int/reproductivehealth/publications/family_planning/HC_and_HIV_2014/en/. Accessed April 25, 2016. [PubMed]


