Abstract
Renal lymphangiomatosis is a rare, benign malformation, characterized by developmental malformation of the perirenal, peripelvic, and intrarenal lymphatics. Radiologist knowledge of the unique radiological features of this entity helps patient's safety in terms of management. We study the case of a 27-month-old boy presented to the emergency department with upper respiratory tract infection. He had a high blood pressure and had been diagnosed earlier with autosomal recessive polycystic kidney disease based on renal ultrasound findings. Because the clinical presentation and laboratory work of the patient did not support the diagnosis of autosomal recessive polycystic kidney disease, further, extensive work-up was performed, which confirmed the diagnosis of renal lymphangiomatosis. This case report emphasizes the imaging features of this rare entity to promote early diagnosis and better patient care.
Keywords: Ultrasound, Magnetic resonance imaging, Lymphangiomatosis, Kidney
Introduction
Renal lymphangiomatosis is a rare, benign entity, characterized by developmental malformation of the perirenal, peripelvic, and intrarenal lymphatics. In children, it can be confused with autosomal recessive polycystic kidney disease (ARPCKD); however, imaging findings are quite characteristic and allow easy diagnosis.
Case report
A 27-month-old boy presented to the emergency department with cough, fever, and decreased oral intake. In a different hospital, he was diagnosed with ARPCKD based on renal ultrasound.
On clinical examination, he had a wheezy chest and distended abdomen with palpable kidneys. The patient was febrile, 38°C; and his blood pressure was high, 130/83.
The liver function test, urine analysis, and renal function test were normal.
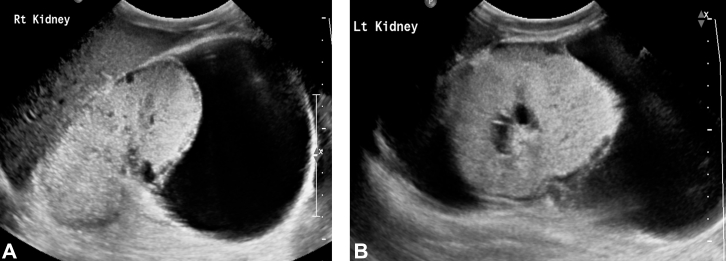
Abdominal ultrasound revealed enlarged kidneys (right, 8.9 cm; left, 8.4 cm) with increased renal cortical echogenicity and loss of corticomedullary differentiation. There were multiple bilateral subcapsular cysts of varying sizes. There were large bilateral perirenal multiseptated fluid collections (Fig. 1). The liver was normal.
Fig. 1.
(A) Oblique sagittal sonogram of the right kidney, (B) oblique sagittal sonogram of the left kidney revealing increased echogenicity with loss of the corticomedullary differentiation of both kidneys. There are numerous anechoic cortical and peripelvic cysts. Large bilateral perinephric fluid collection is noted.
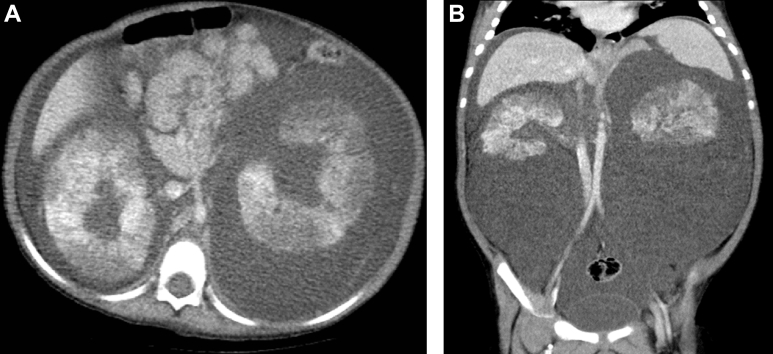
Computed tomography (CT) scan showed enlarged kidneys with heterogeneous cortical enhancement. Bilateral perinephric fluid collection with multiple septations surrounding the kidneys was noted. There were multiple small subcortical cysts with subtle bilateral renal sinus cysts splaying the adjacent collecting system (Fig. 2). No hydronephrosis was noted. A small amount of ascites was seen.
Fig. 2.
(A) Axial and (B) coronal contrast-enhanced computed tomography (CT) demonstrate bilateral perirenal fluid collections, and peripelvic fluid collections with heterogeneous enhancement of the renal parenchyma.
Magnetic resonance imaging of the kidneys demonstrated increased cortical intensity and decreased medullary intensity on T2-weighted images, resulting in poor corticomedullary differentiation. Perinephric fluid was hypointense on T1WI and hyperintense on T2WI with septal enhancement, and there were multiple small subcortical cysts with bilateral renal sinus cysts splaying the adjacent collecting system (Fig. 3). These findings were consistent with the diagnosis of renal lymphangiomatosis.
Fig. 3.
(A) Coronal T1-weighted image and (B) axial T2-weighted image demonstrating bilateral perirenal and parapelvic cysts. Both kidneys are enlarged with reversal of corticomedullary signal intensity (more clearly appreciated in the right kidney).
The patient was treated medically for hypertension. Ultrasound-guided percutaneous drainage was performed. A 6-French pigtail catheter was inserted bilaterally by our pediatric intervention radiologist. The aspirated fluid was chylous, which confirmed the diagnosis of renal lymphangiomatosis.
The perinephric fluid accumulated again after the aspiration. The patient had 2 sessions of sclerotherapy with doxycycline, and the last follow-up showed no fluid accumulation and normal renal function test.
Discussion
Renal lymphangiomatosis is a rare condition where there is abnormal communication between the renal lymphatics and the rest of the lymphatic system. The entity has been known by other names such as renal lymphangiomatosis, renal lymphangioma, peripelvic lymphangiectasia, renal sinus polycystic disease, and renal hygroma [1].
The origin of this disorder is unknown. Lymphatic developmental malformation, which leads to lymphatic drainage obstruction, as well as development of renal sinus and perinephric cysts formation, is the most acceptable theory [2], [3]. There is no sex predilection, and the age of presentation varies.
In pediatric patients, the usual presentation is palpable abdominal mass. The blood pressure might be normal or elevated, and renal function is essentially normal.
According to a review of a literature by Jorge Mejía Restrepo et al, there are 2 radiological manifestations of renal lymphangiomatosis. The first pattern involves a cystic lesion in the renal sinus that could be either small peripelvic cysts that originate in the renal sinus or a large single parapelvic cyst that originates in the medial renal parenchymal tissue. The second pattern is lobular perinephric fluid with multiple septations and less apparent renal sinus cysts, which resembles our case [2].
Sonography and CT scans have been previously described [1], [3] with typical imaging findings. The ultrasounds show increased cortical echogenicity and loss of corticomedullary differentiation mimicking ARPCKD, as in our case. Nevertheless, the presence of perirenal and renal sinus cysts are typical findings for renal lymphangiomatosis [1]. The CT scan confirms the fluid attenuation of the multilocular cystic masses with thin walls in the renal sinus or perinephric cysts. However, the patchy renal cortical enhancement also noted in our patient could be related to renal congestion, and this finding has not been described earlier, in our opinion.
Magnetic resonance imaging of lymphangiomatosis has been described before [1], [2], [4], and it confirms the presence of renal sinus cysts and perinephric cysts. Mani et al [4] reported reversal of normal corticomedullary signal intensity on T2W, which could be due to minimal renal edema and/or congestion secondary to obstructed lymphatics, and this finding is clearly present in our patient.
Although the radiological findings of this entity are quite specific and diagnostic, the diagnosis is usually confirmed by needle aspiration of chylous fluid from the perinephric fluid collections.
In the pediatric patient, the differential diagnosis includes ARPCKD, polycystic renal disease, nephroblastomatosis, lymphoma, and hydronephrosis with perinephric urinoma [3], [5]. The complications of this condition include ascites, renal vein thrombosis, obstructive uropathy, and renin-dependent arterial hypertension.
The treatment plan usually depends on the patient's symptoms and clinical presentation. Our case patient, received 2 sessions of sclerotherapy with doxycycline, and this treatment option was the cure in his case.
Conclusion
We emphasize the classic radiological findings of renal lymphangiectasia in a pediatric patient, that allow the diagnosis to be made with certainty and thus preventing misdiagnosis of other differential diagnoses, especially ARPCKD.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Bagheri M.H., Zare Z., Sefidbakht S., Nabavizadeh S., Meshksar A., Roozbeh J. Bilateral renal lymphangiomatosis: sonographic findings. J Clin Ultrasound. 2009;37(2):115–118. doi: 10.1002/jcu.20488. [DOI] [PubMed] [Google Scholar]
- 2.Restrepo J.M., López Amaya J.E., Sepúlveda N.A., Vélez M.U., Massaro M. Renal lymphangiectasia MDCT and MRI findings. Rev Colomb Radiol. 2011;22(3):1–8. [Google Scholar]
- 3.Gupta R., Sharma R., Gamanagatti S., Dogra P.N., Kumar A. Unilateral renal lymphangiectasia: imaging appearance on sonography, CT and MRI. Int Urol Nephrol. 2007;39:361–364. doi: 10.1007/s11255-006-9039-z. [DOI] [PubMed] [Google Scholar]
- 4.Mani N.B.S., Sodhi K.S., Singh P., Katariya S., Poddar U., Thapa B.R. Renal lymphangiomatosis: a rare cause of bilateral nephromegaly. Australas Radiol. 2003;47:184–187. doi: 10.1046/j.0004-8461.2003.01149.x. [DOI] [PubMed] [Google Scholar]
- 5.Ashraf K., Raza S.S., Ashraf O., Memon W., Memon A., Zubairi T.A. Renal lymphangiectasia. Br J Radiol. 2007;80:e117–e118. doi: 10.1259/bjr/16931054. [DOI] [PubMed] [Google Scholar]