Abstract
Isolated traumatic oculomotor nerve palsy without internal ophthalmoplegia is a rare condition after closed head trauma. The nerve strain leads to intraneural edema with nerve swelling on T2-weighted magnetic resonance (MR) images and traumatic disruption of the blood peripheral nerve barrier with contrast enhancement on T1-weighted MR images. In this patient, susceptibility-weighted MR imaging allowed the direct visualization of the intraneural hemorrhage after suspected traumatic diffuse neuronal axonal injury.
Keywords: Susceptibility weighted MR imaging, Traumatic oculomotor nerve palsy, Intraneural hemorrhage, Diffuse axonal injury
Introduction
After major head trauma, traumatic oculomotor nerve palsy may occur after direct or indirect injury to the nerve [1]. Oculomotor nerve injuries can be divided into different groups [2], [3]: nerve transection or nerve avulsion, nerve straining/stretching, or intraneural hemorrhage. Nerve damage to the oculomotor nerve may happen in its intramedullary part, at the tentorial gap or at the posterior petroclinoid ligament or in the intracavernous and intraorbital part [3], [4]. The nerve is especially prone to damage at the posterior petroclinoid ligament [5].
In major head trauma, basilar skull fractures, orbital injuries, traumatic epidural/subdural hematomas, cortical contusions, diffuse axonal injuries DAIs, and traumatic subarachnoid hemorrhage often accompany traumatic oculomotor nerve transection or nerve compression by adjacent hematoma [2]. Clinically, a complete oculomotor nerve palsy leads to a characteristic down and out position in the affected eye because of the lateral rectus innervated by the abducens nerve and the superior oblique muscle innervated by the trochlear nerve. It also results in a ptosis and mydriasis [6].
In rare cases, isolated complete oculomotor nerve palsy is caused by minor head trauma due to nerve straining at the posterior petroclinoid ligament [5] followed by diffuse axonal injury (DAI) to the nerve itself or to the nuclear area in the brainstem [2]. In very rare cases, isolated traumatic oculomotor nerve palsy without internal ophthalmoplegia is reported [5]. Brain computed tomography (CT) scans are not useful in such cases for CT is insufficient to detect midbrain damage and oculomotor nerve root avulsion or oculomotor nerve straining [7], [8]. However, magnetic resonance image (MRI) scans are highly recommended in order to demonstrate the nerve damage with nerve swelling, T2w hyperintensity, and contrast enhancement of the cisternal nerve segment of the oculomotor nerve resulting from DAI of the nerve.
However, to date, no reports are available demonstrating the hemorrhagic diffuse axonal nerve injury itself on high-resolution MRI [7], [8].
Case report
In June 2016, a 54 years old previously healthy female patient without previous medical record presented with complete right-sided ptosis, deviation of the right bulbus down to the right and out and diplopia of the right eye following a motorcycle accident. Pupillary dilatation was not present. Isolated right-sided posttraumatic oculomotor palsy without internal ophthalmoplegia was clinically diagnosed.
A nondislocated orbital floor fracture on the right side without any posttraumatic damage to the osseous skull or the brain itself was present on the emergency CT examination.
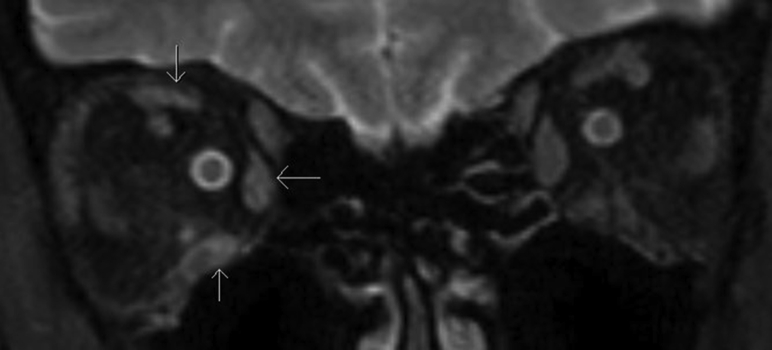
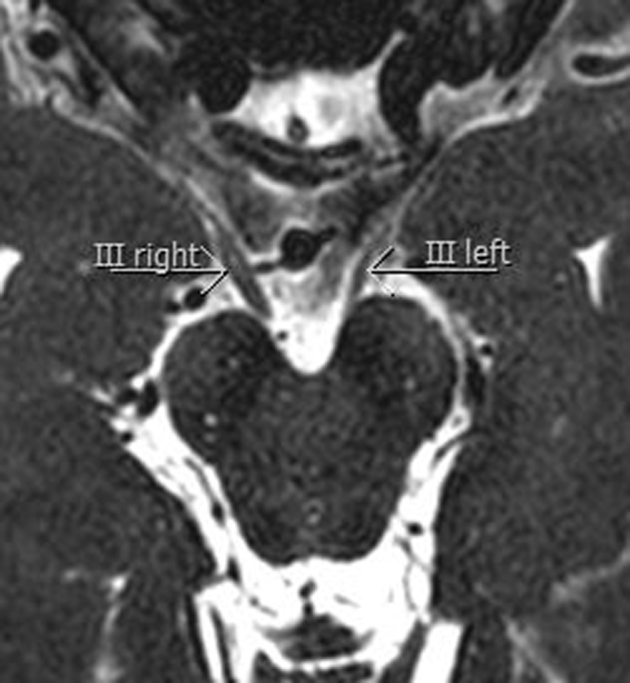
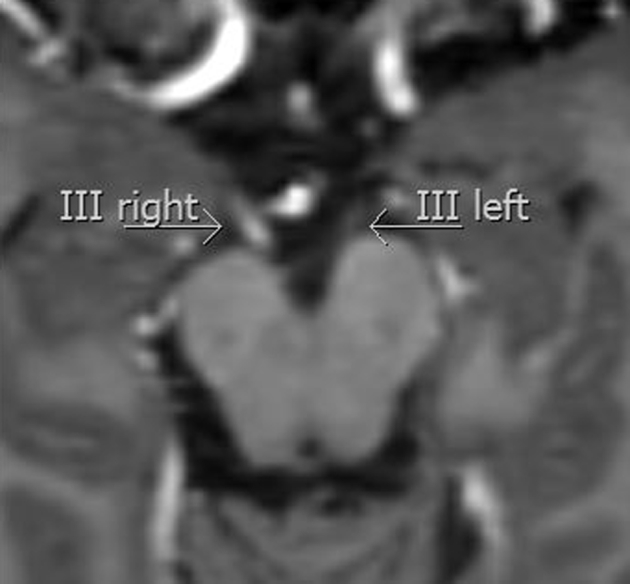
Initial MRI scans obtained on a Philips Achieva 3Tesla MR unit revealed swelling (Fig. 1) and contrast enhancement of the oculomotor nerve along the right cisternal segment (Fig. 2) on 3D T2 spin echo–weighted MRI and on T1-weighted contrast-enhanced MR images. On 3D double inversion recovery sequence, a slight hyperintensity of the cisternal nerve segment on the right side was visible (Fig. 3). On transverse susceptibility-weighted images (SWIs), a focal intraneural hypointense microbleed within the right cisternal oculomotor nerve could be demonstrated (Fig. 4A). Multifocal diffuse axonal hemorrhagic injuries were bilaterally present as hypointense spots on SWI in the amygdala, uncus and parahippocampus, posterior hippocampus, superior cerebellar peduncle, and thalamus (Fig. 4A and 4B). Cortical contusions and epidural or subdural hematomas were absent.
Fig. 1.
Transverse 3D T2w MR image with thickened cisternal segment of right oculomotor nerve (III right) compared to normally sized left oculomotor nerve (III left). 3D, three dimensional; MR, magnetic resonance.
Fig. 2.
Transverse 3D T1-weighted TFE MR image with contrast enhancing cisternal segment of oculomotor nerve (III right) in comparison with nonenhancing cisternal segment of left oculomotor nerve (III left). TFE, turbo field echo; 3D, three dimensional; MR, magnetic resonance.
Fig. 3.
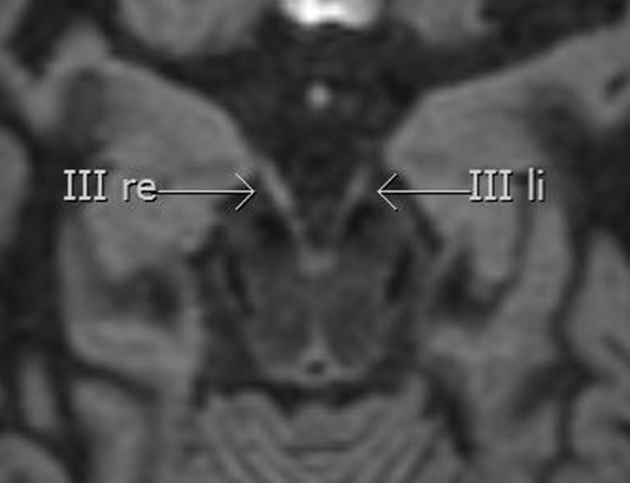
Transverse 3D DIR MR image with thickened and slightly hyperintense right oculomotor nerve (III right) compared to the left side (III left). DIR, double inversion recovery; 3D, three dimensional; MR, magnetic resonance.
Fig. 4.
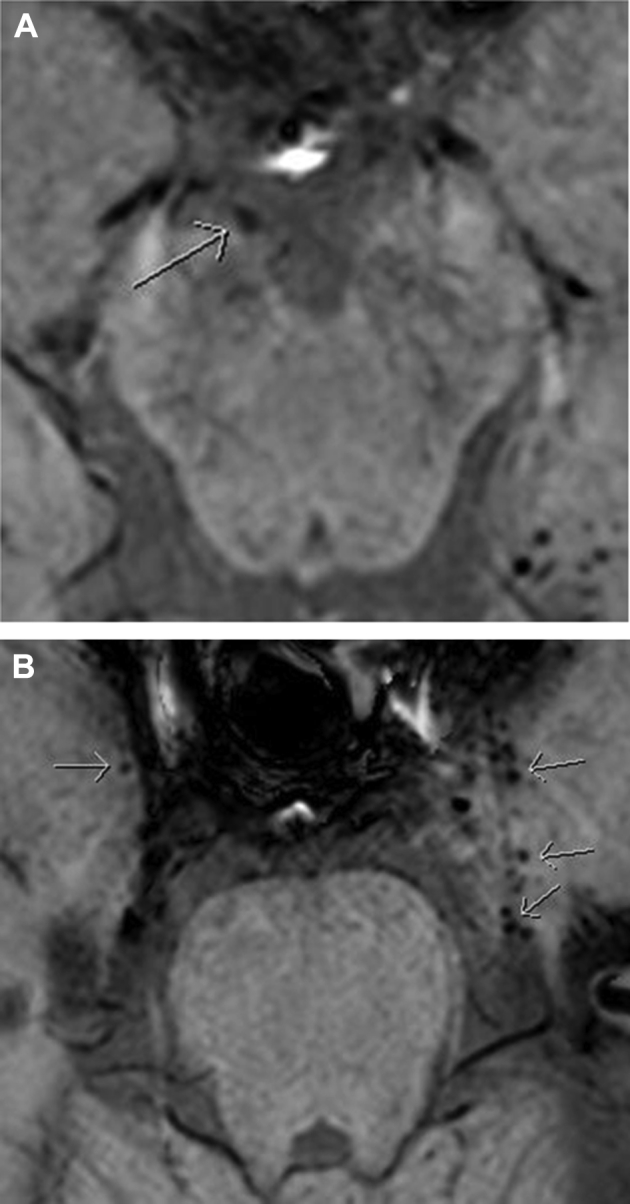
Transverse SW images with focal hypointense spot within the right oculomotor nerve (white arrow in A). Multiple hemorrhagic DAIs (white arrows) in the mediobasal temporal lobe bilaterally (white arrows in B). DAI, diffuse axonal injury; SE, susceptibility weighted.
On T2-weighted fat suppressed m-Dixon MR images, a slight hyperintensity of all the ocular muscles supplied by the oculomotor nerve, that is, inferior/medial and superior rectus muscle as well as of the inferior oblique muscle was visible on the right side (Fig. 5). The orbital floor fracture did not require any treatment.
Fig. 5.
T2-weighted m-Dixon spin echo sequence with hyperintensity of superior, medial, and inferior rectus muscles on the right side (white arrows).
After a 2-months clinical follow-up, no clinical recovery of the oculomotor nerve palsy was present.
Discussion
The oculomotor nerve originates in the midbrain. It runs rostrally through the interpeduncular cistern in close proximity to the posterior petroclinoid ligament in order to pierce the dura mater into the cavernous sinus. The nerve passes through the superior orbital fissure into the orbit and innervates certain extraocular muscles, that is, the inferior, medial, and superior rectus muscles and the inferior oblique muscle and the levator palpebrae superioris muscle as well as the ciliary muscle and iris sphincter [2].
In our patient’s case, isolated posttraumatic oculomotor nerve palsy without internal ophthalmoplegia was clinically diagnosed on the right side after closed head trauma associated with nondislocated orbital floor fracture on the right side.
Straining of axons after rapid deformation due to extreme acceleration and deceleration in head trauma damages, the axons and intraneural edema and hemorrhage may develop [5], [9]. This is the well-known mechanism leading to disruption of axons resulting in DAIs.
In our patient, multiple hemorrhagic DAIs could be demonstrated bilaterally on SWI MR images both infratentorially and supratentorially; however, no DAI was present in the brainstem in the nuclear area of the oculomotor nerve in the midbrain. The punctate hypointense focus on SWI within the right cisternal segment of the oculomotor nerve on the right side, however, was a suggestive morphological sign of a hemorrhagic DAI within the cisternal nerve segment after a severe nerve strain. The nerve damage led to intraneural edema and nerve swelling visible on 3D T2-weighted images. The blood-nerve barrier was damaged leading to contrast enhancement of the oculomotor nerve on T1-weighted contrast-enhanced T1-w-images. A disruption of the blood-nerve barrier in posttraumatic nerve palsy is already known [10].
In order to diagnose DAIs, susceptibility-weighted MR imaging is highly recommendable preferably obtained on a 3T MR unit. To date, SWI is the best available MRI sequence in the detection of small hemorrhages within the brain; SWI is superior to conventional MRI in detecting microbleeds of different origin in the brain [11]. SWI is designed to detect small changes in the local magnetic susceptibility in the brain tissue. Therefore, a variety of pathologic changes can be visualized with SWI compared to conventional MRI, including hemorrhage, calcification, neurovascular abnormalities (ie, developmental venous anomalies, teleangiectasies, cavernomas), iron deposits, and change in oxygenation levels that result from altered blood flow or pathologic processes.
SWI is especially able to detect traumatic microhemorrhagic DAI lesions that are invisible or inconspicuous on other conventional MRI sequences, giving SWI a huge potential in documenting the presence of brain injury even without any additional pathologic traumatic findings like cortical contusions, epidural, and subdural hematoma [11].
Several years ago, patients were not diagnosed these severe posttraumatic injuries due to the fact that previous MR sequences (especially T2-weighted spin echo images as well as T2* images) were much less able to diagnose hemorrhagic or nonhemorrhagic DAIs because of a lack of advanced MRI technology [11]. Susceptibility-weighted MR imaging due to its high spatial resolution and high susceptibility capacity has brought tremendous advantage in demonstrating small pathologic hemorrhagic foci [11].
Therefore, the authors show for the first time that SWI obtained on a 3T MR unit is also able to directly demonstrate microbleeds in a very small structure as the oculomotor nerve with its nerve diameter in the submillimeter range.
Conclusion
Posttraumatic oculomotor nerve palsy usually is the result of severe head trauma. However, isolated posttraumatic oculomotor nerve palsy resulting from DAI either to the nuclear area of the oculomotor nerve or to the cisternal segment of the nerve itself is also known in patients with minor closed head trauma.
This case report shows that posttraumatic oculomotor nerve palsy can be caused by DAI as a result of straining of the oculomotor nerve itself at the posterior petroclinoid ligament leading to focal intraneural hemorrhage and to disruption of the blood-nerve barrier with nerve swelling and contrast enhancement of the nerve. The authors recommend MRI scans and especially high-resolution SWIs to diagnose this condition.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Chen C.C., Pai Y.M., Wang R.F., Wang T.L., Chong C.F. Isolated oculomotor nerve palsy from minor head trauma. Br J Sports Med. 2005;39:e34. doi: 10.1136/bjsm.2004.016311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erenler A.K., Yalcin A., Baydin A. Isolated unilateral oculomotor nerve palsy due to head trauma. Asian J Neurosurg. 2015;10(3):265–267. doi: 10.4103/1793-5482.161169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heinz J. Cranial nerve avulsion and other neural injuries. Med J Aust. 1969;2:1246–1249. doi: 10.5694/j.1326-5377.1969.tb103371.x. [DOI] [PubMed] [Google Scholar]
- 4.Otsuka S.I., Yamazoe N., Kikuta K., Kunieda T. Study on cases with primary traumatic oculomotor nerve palsy. Nippon Geka Hokan. 1994;63:87–90. in Japanese. [PubMed] [Google Scholar]
- 5.Kaido T., Tanaka Y., Kanemoto Y., Katsuragi Y., Okura H. Traumatic oculomotor nerve palsy. J Clin Neurosci. 2006;13:852–855. doi: 10.1016/j.jocn.2005.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Chugh J.P., Prachi J., Chouhan R.S., Rathi A. Third nerve palsy: an overview. Indian J Clin Prac. 2012;22(12):17–20. [Google Scholar]
- 7.Liu Y.T., Lee Y.I.C., Liu H.C. Isolated oculomotor nerve palsy due to head injury. J Chin Med Assoc. 2004;67:149–151. [PubMed] [Google Scholar]
- 8.Ealmaan K., Hyukwon C. Isolated oculomotor nerve palsy following minor head trauma: case illustration and literature review. J Korean Neurosurg Soc. 2013;54:434–436. doi: 10.3340/jkns.2013.54.5.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith E.D., Meaney D.F., Shull W.H. Diffuse axonal injury in head trauma. J Head Trauma Rehabil. 2003;18:307–316. doi: 10.1097/00001199-200307000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Sartoretti-Schefer S., Scherler M., Wichmann W., Valavanis A. Contrast-enhanced MR of the facial nerve in patients with posttraumatic peripheral facial nerve palsy. Am J Neuroradiol AJNR. 1997;18:1115–1125. [PMC free article] [PubMed] [Google Scholar]
- 11.Liu J., Kou Z., Tian Y. Diffuse axonl injury after treumatic cerebral microbleeds: an evaluation of imaging techniques. Neural Regen Res. 2014;9(12):1222–1230. doi: 10.4103/1673-5374.135330. [DOI] [PMC free article] [PubMed] [Google Scholar]