Abstract
A 78-year-old male presented to the Emergency Department complaining of a 1-week onset of increasing fatigue and anorexia. The patient was previously well but had a history of depression, chronic diarrhea, and hypertension. His examination was remarkable for mild fever (100.1°F). He had no acute neurologic deficits. The patient felt better after intravenous fluids and was discharged to follow-up with the primary care provider. With no resolution of symptoms and new memory loss, the patient's primary care doctor ordered an MRI which revealed abnormal signal/patchy enhancement of the left temporal lobe indicative (pathognomonic) of herpes simplex encephalitis. This case emphasizes the importance of early consideration of herpes simplex encephalitis in the differential of patient's with these symptoms.
Keywords: Herpes Simplex, Encephalitis, MRI
Case report
A 78-year-old male presented to the Emergency Department complaining of a 1-week onset of increasing fatigue and anorexia. The patient had a history of depression, chronic diarrhea, and hypertension. His examination was remarkable for mild fever (100.1°F). He had no acute neurologic deficits. Laboratory workup showed modest neutrophilia, and urinalysis revealed moderate microscopic blood. The patient felt better after intravenous fluids and was discharged to follow-up with the primary care provider.
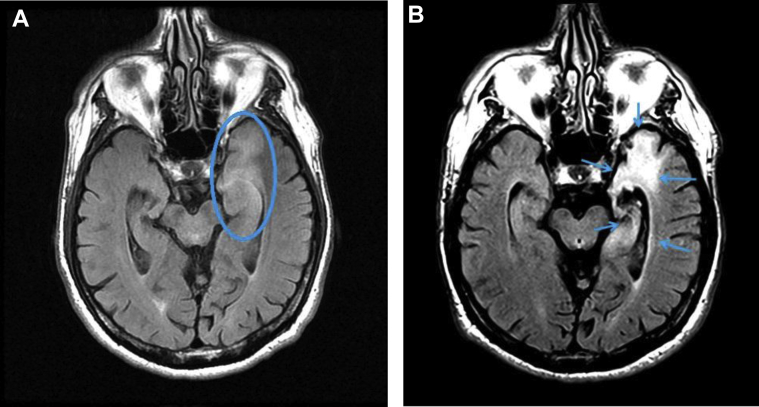
With no resolution of symptoms and new memory loss, the patient's primary care provider ordered an MRI (Fig. 1A) which revealed abnormal signal/patchy enhancement of the left temporal lobe indicative of herpes simplex encephalitis (HSE). The patient was admitted, and diagnosis confirmed with viral polymerase chain reaction of the cerebrospinal fluid (CSF). The patient responded to treatment and was discharged with some residual symptoms.
Fig. 1.
Axial T2 FLAIR MRI of this 78-year-old man who was taken at time of diagnosis (A) and 4 months after diagnosis (B). Hyperintensity of the anterior and medial temporal lobe indicative of inflammation due to encephalitis (depicted in the circled area). Glial scarring extending into limbic structures including the left hippocampus (highlighted by arrows). Cerebral atrophy can also be appreciated in the temporal lobe.
Discussion
HSE has an annual prevalence of 1 in 500,000 cases in the United States and is the most common cause of fatal sporadic encephalitis. Early diagnosis and treatment of HSE is imperative, as demonstrated by its untreated mortality rate of 70%, with only 3% of untreated survivors retaining normal neurologic function [1], [2]. HSE is characterized by symptoms of neurologic infection including focal deficits of the lesioned site (most commonly in the temporal lobe), fever, and seizures [3]. Delay in treatment with acyclovir increases mortality from 19% to more than 70% and may result in permanent neuropsychological impairment [4]. HSE's high inherent morbidity [5] was demonstrated in this patient's lasting cerebral changes (Fig. 1B).
The clinical presentation does not distinguish herpes simplex virus (HSV) from encephalitis caused by other viruses such as St. Louis (flavivirus), Eastern equine (togavirus), and Epstein-Barr virus (EBV) so testing to confirm the etiology of HSV is recommended. Culture of HSV from the CSF of adults with HSE has a sensitivity of less than 10 percent, and better results are obtained with polymerase chain reaction testing for antibodies in the CSF; these tests are associated with sensitivity and specificity rates of 75%-85% and 60%-90%, respectively [6]. The clinical presentation of our case is nonspecific in contrast to the more commonly presenting fever and neurologic (seizures or neurologic deficit) symptoms; although about 50% of the cases of HSE occur in patient's over 50 years old [4], our patient was unusually elderly. It is difficult to know exactly when the clinician should proceed to MRI. Patients may undergo CT and have abnormal findings that lead to further evaluation by MRI, authors recommend this particularly in the elderly. This case reinforces the importance of consideration of HSE in the differential of patient's with these symptoms.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Sabah M., Mulcahy J., Zeman A. Herpes simplex encephalitis. BMJ. 2012;344:e3166. doi: 10.1136/bmj.e3166. [DOI] [PubMed] [Google Scholar]
- 2.Steiner I., Benninger F. Update on herpes virus infections of the nervous system. Curr Neurol Neurosci Rep. 2013;13:414. doi: 10.1007/s11910-013-0414-8. [DOI] [PubMed] [Google Scholar]
- 3.Rice C.M., Yadav S., Boyanton B., Subedi P., Band J. A creeping suspicion. N Engl J Med. 2014;371:68–73. doi: 10.1056/NEJMcps1212310. [DOI] [PubMed] [Google Scholar]
- 4.Whitley R.J., Gnann J.W. Viral encephalitis: familiar infections and emerging pathogens. Lancet. 2002;359:507–514. doi: 10.1016/S0140-6736(02)07681-X. [DOI] [PubMed] [Google Scholar]
- 5.Hjalmarsson A., Blomqvist P., Sköldenberg B. Herpes simplex encephalitis in Sweden, 1990-2001: incidence, morbidity, and mortality. Clin Infect Dis. 2007;45:875–880. doi: 10.1086/521262. [DOI] [PubMed] [Google Scholar]
- 6.Caliendo A. PCR testing for the diagnosis of herpes simplex virus in patients with encephalitis or meningitis. http://www.uptodate.com/contents/pcr-testing-for-the-diagnosis-of-herpes-simplex-virus-in-patients-with-encephalitis-or-meningitis [accessed 11.09.16]