Abstract
Objectives
1) Describe thyroid-related diagnoses and procedures in CHEER across academic and community sites. 2) Compare management of malignant thyroid disease across these sites, and 3) Provide practice based data related to flexible laryngoscopy vocal fold assessment before and after thyroid surgery based on AAO-HNSF Clinical Practice Guidelines.
Study Design
Review of retrospective data collection (RDC) database of the CHEER network using ICD-9 and CPT codes related to thyroid conditions.
Setting
Multisite practice based network.
Subjects and Methods
There were 3,807 thyroid patients (1,392 malignant; 2,415 benign) with 10,160 unique visits identified from 1 year of patient data in the RDC. Analysis was performed for identified cohort of patients using demographics, site characteristics and diagnostic and procedural distribution.
Results
Mean number of patients with thyroid disease per site was 238 (range 23–715). In community practices, 19% of patients with thyroid disease had cancer versus 45% in the academic setting (p<0.001). While academic sites manage more cancer patients, community sites are also surgically treating thyroid cancer, and performed more procedures per cancer patient (4.2 vs. 3.5, p<0.001). Vocal fold function was assessed by flexible laryngoscopy in 34.0% of pre-operative patients and in 3.7% post-operatively.
Conclusion
This is the first overview of malignant and benign thyroid disease through CHEER. It shows how the RDC can be used alone and with national guidelines to inform of clinical practice patterns in academic and community sites. This demonstrates the potential for future thyroid related studies utilizing the Otolaryngology-H&N Surgery’s practice-based research network.
Keywords: CHEER, practice based research network, thyroid disease, cancer, clinical practice guidelines, academic, community, flexible laryngoscopy, vocal cord function, thyroidectomy, thyroid surgery
Introduction
Creation of research networks that integrate both academic and community practices offer the advantage of yielding research that is both widely generalizable and primed for implementation.1 Patient demographics, presenting diagnoses, and treatment patterns can vary substantially among practices, especially between community and academic sites. Extending the use of practice-based research networks that integrate a variety of practice settings can be a powerful resource for improving quality and cost-effectiveness of care nationally.2 This research is particularly pertinent to the field of otolaryngology–head and neck surgery, which covers a broad scope of disorders that may be managed across a variety of practice and resource settings.
The Creating Healthcare Excellence through Education and Research (CHEER) is a practice-based research network that was established to facilitate advancements in otolaryngology–head and neck surgery. Its infrastructure has been designed to facilitate collaborative studies with broadly applicable results, and is funded through the National Institute on Deafness and other Communication Disorders (NIDCD).3, 4 It currently encompasses 30 sites in 19 states and over 200 otolaryngologists, 100 audiologists, and 50 speech and language pathologists.
As its vital component, the retrospective data collection (RDC) project serves as capacity descriptor and currently encompasses 277,519 unique patients with demographic, ICD-9, and CPT codes. It is a robust indicator of the network’s research potential to enroll a wide spectrum of patients with a variety of disorders. More recently, the CHEER Otology Data Collection project further demonstrated the network’s capacity to move from retrospective RDC data to effectively recruit and quickly gather patient-related data for future prospective studies.5
While the capacity of CHEER has been explored in otology, no work utilizing the network has been undertaken for patients with thyroid diseases, which are commonly managed by otolaryngologists. Thyroid cancer remains the most common endocrine malignancy, with 44,670 estimated new cases in 2010 in the US alone.6 Benign disease is also common.7 For example, the incidence of hyperthyroidism is 1.3% in the US population and 5% to 15% of the adult population harbors clinically significant nodules.8 There is significant variability according to sex and ethnic groups, as well as healthcare access and utilization patterns among different patient populations.9 As such, research grounded in broad-based practice settings will likely continue to play an increasing role going forward.
National databases such Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute represent an essential infrastructure for thyroid cancer research.10 The Nationwide Inpatient Sample (NIS) database has also been successfully utilized to study benign thyroid disorders, but is also limited by pre-defined data elements and a retrospective design.11 CHEER offers a unique advantage of flexibility in either retrospective or prospective study designs, and study of both benign and malignant thyroid disorders. In addition, it allows for otolaryngology field-specific research across academic and community practices.
We aim to evaluate the CHEER network’s capacity to study benign and malignant thyroid disease, describe the diagnostic and procedural variability across all sites, as well as draw comparisons between academic and community-based practices. Similarly, we wish to present our findings reflecting the rate of pre and post-operative flexible laryngoscopy for vocal cord assessment in thyroidectomy patients, as suggested by the American Academy of Otolaryngology-Head and Neck Surgery Foundation (AAO-HNSF) Clinical Practice Guidelines, and suggest how the network can be used in assessing statistics related to other national guidelines adherence in the future. 12
Methods
This study was evaluated by the Duke University School of Medicine IRB and deemed to be exempt research. The CHEER RDC project was developed as a site capacity descriptor database to facilitate feasibility analyses of proposed projects for the network. The administrative data capture occurs electronically at each respective site, where it is compiled, de-identified, and then transmitted to the coordinating center. All sites provided 1 year of patient data either from 2011–2012 or 2012–2013. An interim summary of the RDC project is posted at www.cheerresearch.org. At time of this analysis, the RDC project was complete in 22 of 30 sites and held 277,519 unique patients with associated ICD9, CPT codes and demographic data.
To identify a cohort of patients with benign and malignant thyroid disorders, ICD-9 and codes listed below were used to query for patients within the entire CHEER RDC database from 1 billing year. CPT codes related to thyroid surgical procedures were pulled from the RDC and are provided here as well.
Diagnostic ICD-9 codes for both non-cancer and cancer patient groups: Non-cancer - 240, 240.9, 241, 241.0, 241.9, 242, 242.0, 242.9, 243, 244, 244.0, 244.1, 244.9, 245, 245.0, 245.1, 245.2, 246, 246.2, 246.3, 246.8, 246.9, 226; Cancer (Malignant Neoplasm of Thyroid Gland) – 193.
Thyroid surgical procedures obtained using the following CPT codes: Partial thyroid lobectomy (60210, 60212); total thyroid lobectomy (60220, 60225); thyroidectomy (60240, 60252, 60254, 60260, 60270, 60271).
Flexible laryngoscopy (CPT 31575) and laryngoscopy with stroboscopy (CPT 31579) were utilized in assessing the number of patients that had pre-operative (up to 2 months) and post-operative laryngoscopy (2 months following) a thyroid surgical procedure. This is of particular interest since AAO-HNSF Clinical Practice Guideline Statements 2A and 10 recommend pre-operative and post-operative laryngeal assessment of the impaired voice.12 The statements are provided below:
Statement 2A: “Preoperative Laryngeal assessment of the impaired voice”: The surgeon should examine vocal fold mobility, or refer the patient to a clinician who can examine vocal fold mobility, if the patient’s voice is impaired and a decision has been made to proceed with thyroid surgery.
Statement 10: “Postoperative Laryngeal Examination”: Clinicians should examine vocal fold mobility or refer the patient for examination of vocal fold mobility in patients with a change in voice following thyroid surgery.
Descriptive statistics were used to summarize demographic parameters, as well as diagnostic and procedural variability within specified patient cohorts of interest. For association between categorical variables such as frequency of patients with cancer at each site type, chi-square tests for equal proportions was utilized. Associations between continuous variables such as number of visits, and procedures per patient, were assessed with the unpaired t-tests and summarized by 95% confidence intervals and a p-value. Significance of the tests was assessed at alpha = 0.05. The data in the RDC was analyzed using SAS v9.3 and JMP Pro 11.2.1 software based on the criteria specified by CHEER Task Force expertise, including breakdowns by site, and setting (community/academic).
Results
At the time of the RDC project data collection, 21 of the 22 sites of the RDC project had thyroid related data; the one site that was an exception was an otology specialty practice. This data were collected from 9 community-based and 12 academic practices. There were 3,807 thyroid patients (1,392 malignant; 2,415 benign) with 10,160 unique visits identified within 1 year of patient data, either from 2011–2012 or 2012–2013, depending on the site. The number of patients with thyroid disease per site ranged from 23 to 715 with a mean of 237.5 (SD 233.2) patients. This indicates that over a third (36.6%) of the thyroid patients in otolaryngology practices had a cancer-related diagnosis. As shown in Table 1, the average age, sex, and race distribution are similar to nationally reported averages and trends.13
Table 1.
Thyroid disease patient characteristics by diagnosis compared to all RDC patients.
| RDC Patients with Thyroid Disease | All RDC Patients | |||
|---|---|---|---|---|
| Parameter | Non-Cancer Diagnosis | Cancer Diagnosis | Combined | |
| Unique Patients | 2,415 | 1,392 | 3,807 | 277,519 |
| Unique Visits | 6,309 | 3,851 | 10,160 | 685,913 |
| Visits per Patient – Mean (SD) | 2.6 (0.98) | 2.8 (0.91) | 2.7 (0.95) | 2.5 (0.89) |
| Procedures per Patient – Mean (SD) | 3.0 (1.11) | 3.6 (1.42) | 3.2 (1.27) | 3.0 (1.24) |
| Age – Mean (SD) | 53.2 (4.6) | 52.9 (4.47) | 53.1 (4.62) | 41.4 (8.04) |
| % Male | 20.7% | 31.6% | 24.7% | 46.8% |
| % Caucasian1 | 75.1% | 84.3% | 78.5% | 80.9 % |
Race data was not available from all sites
The majority of the patients within the network (57%, n=2,179) had benign thyroid disease and did not undergo partial thyroid lobectomy, total thyroid lobectomy, or thyroidectomy. Some of the most frequent benign disorders were nontoxic nodular goiter (n=1,569), hypothyroidism (n=462), thyroiditis (n=124) and cyst of the thyroid gland (n=92). Interestingly, of the 12% of patients that received a thyroid surgical procedure, they were approximately evenly split between 230 patients with thyroid cancer and 222 with benign disease. It must be noted that many of the patients in the group that had a cancer diagnosis and received no surgical procedure (30%) likely represent follow-up care for those that were treated surgically for cancer at a different practice. These numbers demonstrate the heterogeneity of diagnosis and management of CHEER thyroid patients.
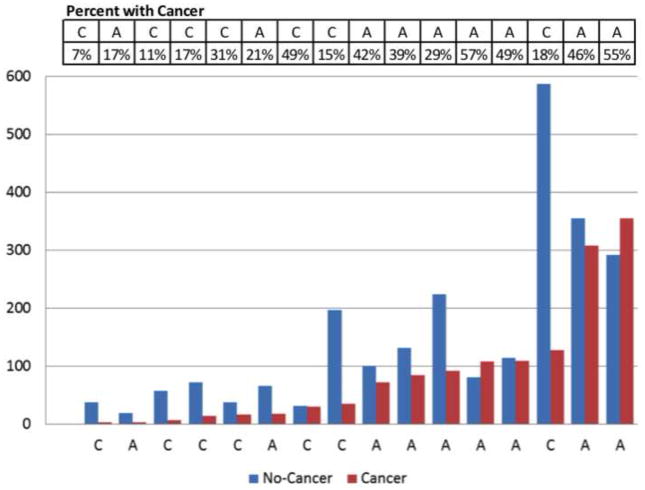
We also analyzed our results by practice setting – community or academic, with results shown in Table 2. Sites with fewer than 20 thyroid patients in the year of RDC data were excluded from analysis due to setting a minimum for site inclusion in analysis, since they likely represent outliers. Notably, in the community setting, 19% of the patients with thyroid disease had cancer, versus 45% in the academic setting, and this difference was statistically significant (p<0.001). Despite seeing less cancer patients, community sites actually had more visits per patient for cancer patients with mean of 3.8 visits (95%CI: 3.4–4.2) per patient vs. 2.6 visits (95%CI: 2.4–2.7) at academic sites (p<0.001). This was also true for patients with benign thyroid disease, although mean number of visits was smaller than for cancer patients: 3.2 (2.8–3.4) for community and 2.2 (2.1–2.3) for academic sites. Furthermore, community sites had more procedures per patient for cancer patients than academic sites (4.2 vs. 3.5; p<0.001), but no such difference was observed for patients with benign thyroid disease (3.2 vs. 3.1; p=0.373) as shown in Table 2. “Procedures per patient” variable includes the average number of all CPT codes per patient. Out of thyroid surgical procedures most frequent were: total lobectomy/hemi-thyroidectomy (60220) n=195, total thyroidectomy (60240) n=136, total or subtotal thyroidectomy with limited neck dissection (60252) n=51. Some of these procedural codes were evaluation and management, representing a limitation of our analysis. Other frequently performed procedures besides thyroid surgeries in our cohort included laryngoscopy and ultrasound of the head and neck. Figure 1 further demonstrates the burden of thyroid cancer patients across individual academic and community practices. This provides information at a site-specific level and allows for identification of outliers. Rates of patients with thyroid cancer diagnosis ranged from 7% to 57% with an average of 37%.
Table 2.
Differences between patients with thyroid disease by practice type (academic vs. community) and cancer status.
| Cancer Diagnosis | Non-Cancer Diagnosis | |||||
|---|---|---|---|---|---|---|
| Site Type | Academic (n=9) | Community (n=7) | P-Stat | Academic (n=9) | Community (n=7) | P-Stat |
| % Patients with Cancer | 45% | 19% | <0.001 | - | - | |
| % Visits for Cancer Patients | 49% | 22% | <0.001 | - | - | |
| Unique Patients | 1,154 | 237 | 1,386 | 1,023 | ||
| Unique Visits | 2,944 | 904 | 3,057 | 3,232 | ||
| Visits per Patient Mean (95% CI) | 2.6 (2.4–2.7) | 3.8 (3.4–4.2) | <0.001 | 2.2 (2.1–2.3) | 3.2 (2.8–3.4) | <0.001 |
| Procedures per Patient Mean (95% CI) | 3.5 (3.3–3.6) | 4.2 (3.8–4.6) | <0.001 | 3.1 (2.9–3.2) | 3.2 (3.0–3.3) | 0.373 |
Only includes practices with >= 20 thyroid patients (n = 16 sites). The p values represent comparison of measures between academic and community cohorts within each diagnostic group.
Figure 1.
Depicts volume of thyroid disease at each individual site, including site-specific proportion of malignant disease and practice setting (A-academic and C-community). Only practices with >= 20 thyroid patients.
Laryngeal examination through flexible laryngoscopy either with or without stroboscopy was documented via CPT code in 34.0% of pre-operative patients and in 3.7% of patients post-operatively across all sites for patients undergoing thyroid surgery. These were obtained by assessing the number of patients with laryngoscopy within 2 months leading up to, and within 2 months following a thyroid procedure.
Discussion
In describing the occurrence of thyroid disease and management across academic and community sites, we have exhibited the potential of CHEER to serve as a practice-based research network. As mentioned, advantages of using the CHEER network for thyroid disease include flexibility of prospective and retrospective study designs, incorporation of a variety of otolaryngology practice settings (academic, community), and inclusion of neoplastic and benign disease.
Our findings suggest that patients are being evaluated and managed in both the community and academic settings, with both demonstrating the capacity to contribute to management of surgical and non-surgical thyroid disease. We provided a general overview of thyroid disorders in the RDC (Table 1), and show that this population encompasses both malignant and benign disease, with many patients receiving intervention (eg, lobectomy or thyroidectomy) at the site. Figure 1 depicts the burden of thyroid disease at each individual site by illustrating per site patient volumes, as well as proportion of practice patients that are treated for malignant disease. For thyroid disorders, site type does not seem to carry a specific profile, but does show notable variability according to the individual population served and practice goals. This site-by-site variability is important to take into account in future prospective studies.
It is intriguing that thyroid cancer patients are more commonly seen at academic centers, but community sites have higher number of visits and procedures per patient, as presented in Table 2. One would surmise that patients with a cancer diagnosis require more management and treatment than those who do not. However, this may be an indication of collaboration between community and academic sites and patient preferences. For example, a patient diagnosed with a malignancy in a community setting may choose to receive further care in an academic setting depending on the stage, need for radioactive iodine, and nature of the malignancy. Similarly, a patient that has been treated in an academic setting may choose to receive follow-up care and treatment in a community setting with caregivers or a location that is more familiar to them.
In this work, we present data on pre-operative and post-operative flexible laryngoscopy use prior to and following thyroid procedure. In 2013, the AAO-HNSF released guidelines with the purpose of optimizing voice outcomes for adult patients following thyroid surgery. The guidelines indicate criteria for evaluation of laryngeal function, through pre-operative and post-operative laryngeal assessment of the impaired voice (Grade C evidence).12 However, the guideline statement also references appeals by some organizations such as National Comprehensive Cancer Network (NCCN) to include preoperative laryngoscopy for all patients with thyroid malignancy due to frequent diagnosis of asymptomatic vocal fold paresis and minimal risk of the procedure.14 We report that within CHEER, 34.0% of patients received pre-operative flexible laryngoscopy with or without stroboscopy within 2 months of thyroid surgery, and only 3.7% of patients 2 months following surgery. This includes all patients undergoing thyroid surgery, and does not account for patient symptoms. Our findings fall within the previously reported range of 6.1–54% of preoperative flexible laryngoscopy rates in UK and USA for thyroidectomy patients.15, 16 Since it is recommended that post-surgery voice complaints are evaluated by flexible laryngoscopy, the low frequency of post-operative evaluation in our population may indicate preserved vocal quality following surgery performed by otolaryngologists. It may also simply be a coding phenomenon, with providers less likely to enter procedure codes during a global period after surgery.
One limitation of this study is its use of the RDC database, which is an incomplete set, comprised of demographic, ICD-9 and CPT data, which inherently lacks diagnostic and procedural specificity, and thus should be cautiously used in drawing conclusions. Additionally, the analysis of this data is retrospective. However, this analysis is unique in describing a disease-specific otolaryngology population across practice settings and can be used to generate hypotheses for future research. This work further demonstrates the benefits of utilizing a practice-based network and will expectantly stimulate further thyroid related research through CHEER, the nation’s otolaryngology-head and neck surgery practice-based research network.
Acknowledgments
The authors wish to acknowledge statistical programmer Vidya Ramamurthy for her contribution to the data analysis. We acknowledge all of the CHEER Network sites that contribute data to the RDC.
References
- 1.Heintzman J, Gold R, Krist A, et al. Practice-based research networks (PBRNs) are promising laboratories for conducting dissemination and implementation research. J Am Board Fam Med. 2014;27:759–62. doi: 10.3122/jabfm.2014.06.140092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindbloom EJ, Ewigman BG, Hickner JM. Practice-based research networks: the laboratories of primary care research. Med Care. 2004;42(4 Suppl):III45–9. [PubMed] [Google Scholar]
- 3.Tucci DL, Schulz K, Witsell DL. Building a National Research Network for Clinical Investigations in Otology & Neurotology. Otol Neurotol. 2010;31:190–5. doi: 10.1097/MAO.0b013e3181c9940c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Witsell DL, Rauch SD, Tucci DL, et al. The Otology Data Collection project: report from the CHEER network. Otolaryngol Head Neck Surg. 2011;145:572–80. doi: 10.1177/0194599811416063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Witsell DL, Schulz KA, Moore K, Tucci DL CHEER Investigators. Implementation and testing of research infrastructure for practice-based research in hearing and communication disorders. Otolaryngol Head Neck Surg. 2011;145:565–71. doi: 10.1177/0194599811406369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown RL, de Souza JA, Cohen EE. Thyroid cancer: burden of illness and management of disease. J Cancer. 2011;2:193–9. doi: 10.7150/jca.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang C, Crapo LM. The epidemiology of thyroid disease and implications for screening. Endocrinol Metab Clin North Am. 1997;26:189–218. doi: 10.1016/s0889-8529(05)70240-1. [DOI] [PubMed] [Google Scholar]
- 8.Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III) J Clin Endocrinol Metab. 2002;87:489–99. doi: 10.1210/jcem.87.2.8182. [DOI] [PubMed] [Google Scholar]
- 9.Enewold L, Zhu K, Ron E, et al. Rising thyroid cancer incidence in the United States by demographic and tumor characteristics, 1980–2005. Cancer Epidemiol Biomarkers Prev. 2009;18:784–91. doi: 10.1158/1055-9965.EPI-08-0960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu JB, Gross CP, Wilson LD, et al. NCI SEER public-use data: applications and limitations in oncology research. Oncology. 2009;23:288–95. [PubMed] [Google Scholar]
- 11.Ho TW, Shaheen AA, Dixon E, Harvey A. Utilization of thyroidectomy for benign disease in the United States: a 15-year population-based study. Am J Surg. 2011;201:570–4. doi: 10.1016/j.amjsurg.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Chandrasekhar SS, Randolph GW, Seidman MD, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013;148(6 Suppl):S1–37. doi: 10.1177/0194599813487301. [DOI] [PubMed] [Google Scholar]
- 13.Ries LAG, Eisner MP, Kosary CL, et al. SEER Cancer Statistics Review, 1975–2000. National Cancer Institute; Bethesda, MD: 2003. http://seer.cancer.gov/csr/1975_2000/ [Google Scholar]
- 14.Tuttle RM, Ball DW, Byrd D, et al. Thyroid Carcinoma. J Natl Compr Canc Netw. 2010;8:1228–74. doi: 10.6004/jnccn.2010.0093. [DOI] [PubMed] [Google Scholar]
- 15.Scott-Coombes D. The British Association of Endocrine and Thyroid Surgeons—Third National Audit Report. Henley-on-Thames, UK: Dendrite Clinical Systems Ltd; 2009. [Google Scholar]
- 16.Hundahl SA, Cady B, Cunningham MP, et al. An American College of Surgeons Commission on Cancer Patient Care Evaluation study. Cancer. 2000;89:202–217. doi: 10.1002/1097-0142(20000701)89:1<202::aid-cncr27>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]