Abstract
We examined religious/spiritual (RS) coping from the Survey of Experiences of Returning Veterans (SERV) Study, 630 participants who reported on their demographics, combat exposure, use of positive and negative RS coping, posttraumatic stress disorder (PTSD) symptoms and perceived posttraumatic growth (PPTG). PTSD symptoms and PPTG were inversely correlated. As hypothesized, negative RS coping was inversely associated with PPTG and positively with PTSD, while positive RS coping was related only to PPTG. Although we expected that RS coping would buffer relations between combat exposure and both PTSD and PPTG, we found only one moderator effect and it was opposite our hypothesized direction: Those with high combat exposure and high positive RS coping had the highest PTSD symptomatology. These results suggest, among veterans with combat exposure, negative RS coping is associated with higher PTSD symptomatology, while positive RS coping is generally associated with higher PPTG as well as higher PTSD for those with high combat exposure.
Religiousness and spirituality have been shown to be important and commonly used resources for people coping with a variety of stressful and traumatic experiences, including major illnesses (e.g., Schreiber & Brockopp, 2012), bereavement (e.g., Wortmann & Park, 2008), and natural disasters (e.g., Henslee, Coffey, Schumacher, Tracy, Norris, & Galea, 2014). Although religiousness and spirituality are distinct constructs, with religiousness often characterized as a system of beliefs residing in a larger context and spirituality as the subjective experiences of a higher power or transcendence, these terms are often used conjointly (Aldwin, Park, Jeong, & Nath, 2014) Importantly, religiousness and spirituality comprise many dimensions, including affiliation, religious group identification, personal practices such as prayer, public practices such as service attendance, personal identification, and coping (NIA/Fetzer, 1999; Ysseldyk, Matheson, & Anisman, 2010).
A burgeoning body of research has examined religious/spiritual (RS) coping, which is typically separated into two dimensions. Positive RS coping includes strategies such as seeking spiritual support and making benevolent religious reappraisals, while negative RS coping (also known as spiritual struggle) includes spiritual discontent and making punitive religious reappraisals. Positive RS coping efforts are sometimes related to higher levels of well-being (e.g., Pargament et al., 1998), but null or even inverse effects of positive RS coping are often reported (e.g., Gerber, Boals, & Schuettler, 2011). More consistent findings have been reported for negative RS coping, in that it tends to be infrequently used but strongly related to myriad dimensions of poorer mental and physical health (see Exline & Rose, 2013, for a review).
RS coping may be especially salient in the context of military service (Pargament & Sweeney, 2011). Religiousness and spirituality are often emphasized in the military implicitly as well as explicitly. For example, chaplains play a prominent role in providing RS support to military families, many military creeds and rituals invoke God or Heaven, and dog tags indicate service members’ religious affiliations (Besterman-Dahan et al., 2012). According to a Department of Defense (DoD) survey, the majority of military personnel self-identify as belonging to a religious group/organization (cited in Hourani, Williams, Forman-Hoffman, Lane, Weimer, & Bray, 2012). This 2011 DoD Survey, Religiosity/Spirituality and Health Behaviors, found fairly high levels of religiousness and spirituality among active duty personnel, with 28.3% classified as high, 35.3% as medium, 14.0% as low, and only 22.4% indicated religiousness and spirituality was “not applicable” to them (cited in Hourani et al., 2012). These numbers indicate that religiousness and spirituality are indeed a common potential resource for most members serving in the military.
Religiousness and spirituality may be particularly important as a resource for coping with experiences encountered in military service, because such service often involves threats of danger and death as well as participation in acts that may violate moral beliefs (Litz et al., 2009). Curiously, however, relatively little research has investigated the role of religiousness and spirituality in this context. Studies of predominantly Vietnam-era veterans have reported some weak and indirect evidence of protective effects of religiousness and spirituality. For example, in one study, stronger religious faith was associated with less extensive use of VA services (Fontana & Rosenheck, 2004). In another study of veterans with a history of sexual assault, two aspects of religiousness and spirituality (organizational and subjective) attenuated negative mental health symptoms for men (Chang, Skinner, Zhou & Kazis, 2003) while only organizational religiousness and spirituality buffered the effects for women (Chang, Skinner, & Boehmer, 2001). However, a study of VA outpatients found that positive RS coping was associated with more PTSD symptom severity and unrelated to anxiety or depression (Witvliet et al., 2004). More consistently, research suggests that Vietnam veterans who struggle with RS issues and use negative RS coping have more deficits in psychological, social, and physical functioning than do those who do not struggle (Berg, 2011; Fontana & Rosenheck, 2005). Most of this earlier work, with the exception of Chang et al. (2001), was conducted only with men.
A more recent study of returning combat veterans from Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) by Ogden and colleagues (Ogden et al., 2011) extended earlier findings with Vietnam veterans by not only examining psychiatric adjustment indices such as PTSD or depression, but also focusing on perceived posttraumatic growth (PPTG). PPTG, perceptions of positive changes one has experienced as the result of a traumatic event (Cho & Park, 2014), is a phenomenon of increasing interest in recent years. There is some evidence that PPTG may be a form of positive adaptation to highly stressful or traumatic experiences (Park & Helgeson, 2006). In Ogden and colleagues’ (2011) study, PTSD symptoms were associated with spiritual struggle (alienation from God, religious rifts, and religious fear and guilt). However, similar to other studies (e.g., Witvliet et al., 2004), Ogden and colleagues (2011) found that positive religious coping (religious comfort, prayers for acceptance, prayers for assistance, and prayers for calm and focus) was unrelated to PTSD symptoms. On the other hand, positive religious coping was associated with PPTG while negative religious coping was unrelated.
One essential question regarding religiousness and spirituality is whether, in addition to its general associations with adjustment and well-being, it becomes particularly important when people experience stressful events. This type of influence is termed stress-buffering or moderation. Research has demonstrated stress-buffering effects of religiousness and spirituality on a range of psychological, social, and physical outcomes (e.g., Park et al., 1990; Shannon, Oakes, Scheers, Richardson, & Stills, 2013). However, we were able to locate only one study that directly tested stress-buffering effects of religiousness/spirituality in the military context, which was a recent study of over 24,000 active duty men and women drawn from the 2008 Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel (Hourani et al., 2012). This study examined the extent to which religiousness and spirituality was associated with mental health problems among active duty military personnel and whether it moderated the relationship between combat exposure during deployment and psychiatric adjustment (depression, posttraumatic stress symptoms, and suicidality). Participants were categorized as high, medium or low in religiousness and spirituality. Results indicated that high religiousness and spirituality had a protective effect only for depression symptoms. Medium, as opposed to high or low, levels buffered all three mental health outcomes. Medium and low levels predicted depression symptoms but only among those with moderate combat exposure. Medium levels also predicted PTSD symptoms among those with moderate levels of combat exposure and predicted self-reported suicidal ideation/attempt among those who never deployed. These results indicate that the relationship between religiousness and spirituality, and mental health is complex.
Our goal was to extend previous research on religiousness and spirituality in the context of military service. In particular, building on Hourani et al.’s (2012) demonstration of stress-buffering effects of religiousness and spirituality on combat exposure in predicting adjustment among active duty military personnel, we expand this work in four ways: (1) We focused on veterans after their return from combat theater to examine how religiousness and spirituality may aid in adjustment after leaving a warzone environment and separating from the military; (2) we measured specifically RS coping rather than global RS; (3) we included a negative aspect of religiousness and spirituality (negative RS coping) as well as a positive aspect (positive RS coping), and (4) we included a positive outcome (PPTG) along with the negative adjustment variable (posttraumatic stress symptoms). Given previous evidence for gender differences in mean levels of religiousness and spirituality (women typically higher; e.g., Park, Lee, Sun, Klemmack, Roff, & Koenig, 2013) and associations between religiousness and spirituality, and mental health (Park & Slattery, 2013), all analyses tested for gender differences.
Based on previous research, we hypothesized: (1) Combat would be positively related to PTSD and PPTG; (2) RS coping would be related to PTSD symptoms and PPTG (i.e., positive to less PTSD and more PPTG, negative to more PTSD and less PPTG), and (3) RS coping would moderate combat-PTSD/PPTG relationships. Across these hypothesized relationships, we expected that men and women would differ, in that that women would score higher on religiousness and spirituality than would men and that religiousness and spirituality might also differentially buffer the effects of combat on adjustment by gender.
Method
Procedure and participants
We analyzed data from wave 1 of the Survey of the Experiences of Returning Veterans (SERV) study. The purpose of SERV is to study post-deployment experiences of returning OEF/OIF/OND veterans. Veterans who served in Iraq, Afghanistan, or surrounding areas or waters were eligible for SERV. Recruitment took place through multiple outlets, including the Internet (e.g., Facebook, YouTube), media outlets, Veterans Affairs (VA) resources such as listservs, and closed circuit televisions in VA facilities, and word of mouth. Respondents were interviewed by trained staff using structured telephone interviews lasting 60–80 minutes. At the time of the currently reported investigation, 770 veterans had completed the wave 1 survey. The current investigation was limited to those who did not report “I don’t believe in God” in response to the religious coping items (n = 630; see “Religious/Spiritual Coping” in the “Measures” subsection below). All study procedures were approved by the Institutional Review Board of the Department of Veterans Affairs.
Measures
Religious/spiritual coping
Positive coping was assessed with the three-item positive RS coping scale from the Brief Multidimensional Measure of Religiousness/Spirituality (BMMRS) (Fetzer/NIA, 1999) (sample item: “I work together with God as partners”). Each item is rated on a scale from 1 (not at all) to 4 (a great deal). Cronbach’s alpha was 0.89. Negative RS coping was assessed with the two items of negative RS coping on the BMMRS (sample item: “I feel God is punishing me for my sins or lack of spirituality”), rated on the same scale as positive coping. The correlation for these two items was 0.70. Due to a programming error, the last item for negative RS coping was left out of the questionnaire and, therefore, not included in the analysis. Due to IRB concerns, the religious coping items were modified to include an alternative response option, “I don’t believe in God at all.” Therefore, those who selected this response option did not have a value for RS coping and consequently were eliminated from our analyses. We considered coding this response as a value of 1 (equivalent to “not at all”); however, we determined that this would be inaccurate as these individuals may indeed use RS coping in spite of their report of a lack of belief in God (Exline & Rose, 2013).
Mental health outcomes
PTSD symptom severity was measured using the 17-item PTSD Checklist (PCL - Civilian) (Wilkins, Lang, & Norman, 2011), a widely used self-report measure that corresponds with diagnostic criteria for PTSD. The PCL contains 17 items rated on a five-point Likert scale from 1 (not at all) to 5 (extremely). Representative items include, “Trouble falling or staying asleep,” “Feeling very upset when something reminded you of a stressful experience from the past,” and “Avoiding thinking about or talking about a stressful experience from the past or avoiding having feelings related to it.” In the present study, Cronbach’s alpha was .94.
Perceived posttraumatic growth was measured using the 21-item Posttraumatic Growth Inventory (Tedeschi & Calhoun, 1996). For this measure, respondents rated how much each item described change that occurred as a result of their military experience on a scale of 0 (to a very small degree as a result of my military experience) to 5 (to a very great degree as a result of my military experience). Responses were averaged. Cronbach’s alpha was .90.
Combat exposure
Combat exposure during deployment was measured using the Combat Experiences subscale of the Deployment Risk and Resilience Inventory (King, King, Vogt, Knight, & Samper, 2006). Frequencies of occurrence for each of 17 experiences were measured on a scale of 0 (never) to 5 (daily or almost daily). Sample items included, “I went on combat patrols or missions” and “I took part in an assault on entrenched or fortified positions that involved naval and/or land forces.” Responses were summed for a total possible score between 0 and 85. This variable was highly skewed, and was not able to be normalized using transformation; therefore we divided combat exposure into three groups (low, moderate, high) based on 33rd and 66th percentile cut points.
Sociodemographic characteristics
We considered age, education, household income, marital status, gender, and race/ethnicity as sociodemographic covariates in our models (see Table 1). Education was coded as a binary variable, representing either “less than or equal to high-school” or “greater than high-school” (75.1% ≥ high-school). Income was examined as a continuous ordinal variable, with categories ranging from “under $20,000” to “$100,000 or more.” Mean income for this sample fell between $35,000 and $75,000, with a range of <$20,000 to ≥$100,000. Marital status was coded into three groups: 1) married or living with someone (54.9%), 2) divorced/widowed/separated (21.1%), and 3) never married (24.0%). Race/ethnicity was grouped into White/Caucasian, non-Hispanic (62.7%), Black/African American, non-Hispanic (14.6%), other non-Hispanic (7.7%), and Hispanic (15.1%). Respondents could endorse more than one race/ethnicity category.
Table 1.
Sample characteristics (n = 730)
| Range | Mean (SD) or n (%) |
|
|---|---|---|
| Age | 21.97 to 65.73 | 35.72 (8.86) |
| Gender | --- | |
| Male | 392 (62.22) | |
| Female | 238 (37.78) | |
| Education a | 1 to 8 | 5.18 (1.27) |
| Household income b | 1 to 6 | 3.31 (1.57) |
| Marital status | --- | |
| Married or living with someone | 346 (54.92) | |
| Never married | 151 (23.97) | |
| Divorced/widowed/separated | 133 (21.11) | |
| Race/ethnicity | --- | |
| White/Caucasian, non-Hispanic | 391 (62.66) | |
| Black/African American, non-Hispanic | 91 (14.58) | |
| Other, non-Hispanic | 48 (7.69) | |
| Hispanic | 94 (15.06) | |
| RS coping: Positive | 1 to 4 | 2.51 (0.97) |
| RS coping: Negative | 1 to 4 | 1.36 (0.63) |
| Combat exposure | --- | |
| Low | 192 (30.52) | |
| Moderate | 221 (35.14) | |
| High | 216 (34.34) | |
| PCL score (PTSD symptoms) | 17 to 85 | 47.07 (18.59) |
| Perceived posttraumatic growth | 0 to 5 | 2.78 (1.00) |
Note: RS = Religious/spiritual, PCL = PTSD Checklist
A mean education score of 5.17 is between the categories ‘Some college’ and ‘College graduate’
A mean household income score of 3.31 is between the categories ‘$35,000 to $50,000’ and ‘$50,000 to $75,000.’
Statistical Analyses
We first computed sample descriptive statistics, and compared primary study variables between men and women (RS coping, PTSD severity, PPTG). Statistical comparisons were conducted using chi-square tests for categorical variables and t-tests for continuous variables. We then computed a correlation matrix of our primary variables of interest. Next, we tested our study hypotheses using a series of regression analyses. We modeled PTSD symptom severity on combat exposure and RS coping, controlling for sociodemographic variables (Hypotheses 1 and 2). We then repeated this procedure, with PPTG as our outcome variable (Hypotheses 1 and 2). Finally, we regressed PTSD symptom severity (and then PPTG) on the interaction between combat exposure and RS coping, controlling for sociodemographic variables (Hypothesis 3). We tested gender interactions for all analyses, which were universally non-significant. As a result, we only present findings for the combined sample. All analyses were carried out using Stata version 13.1 (StataCorp, 2013).
Results
Descriptive statistics for sociodemographic variables and variables of interest are presented in Table 1. Bivariate associations among study variables are presented in Tables 2 and 3. The correlation between positive and negative RS coping was non-significant (r(624) = −.07, p = .07), confirming our operationalization of two distinct constructs. PPTG and PTSD symptoms were significantly negatively correlated (r(620) = −.15, p < .001). Combat exposure was significantly positively associated with positive RS coping (F(2,523) = 9.81, p < .001) and PTSD symptoms (F(2,624) = 40.78, p < .001). Positive RS coping was associated with PPTG (r(619) = .29, p < .001), but not with PTSD symptoms (r(624) = .004, p = .92). Negative RS coping was negatively associated with PPTG (r(618) = −.15, p < .001), and positively associated with PTSD symptoms (r(623) = .40, p < .001).
Table 2.
Correlation matrix for RS Coping, PTSD symptoms and perceived post-traumatic growth
| 1. | 2. | 3. | 4. | |
|---|---|---|---|---|
| 1. RS coping: Positive |
--- | .29*** | .004 | |
| 2. RS coping: Negative |
--- | --- | −.15*** | .40*** |
| 3. Perceived posttraumatic growth |
--- | --- | --- | −.15*** |
| 4. PCL score | --- | --- | --- | --- |
Note: RS = Religious/spiritual, PCL = PTSD checklist. Pairwise correlations for continuous variables (1–4) were calculated using Pearson correlations.
p < .05,
p < .01,
p < .001.
Table 3.
Means for key study variables by combat exposure level
| RS coping: Positive*** |
RS coping: Negative* |
Perceived posttraumatic growth |
PCL score*** | |
|---|---|---|---|---|
| Low | 2.66 (0.93) | 1.30 (0.55) | 2.74 (1.10) | 38.71 (17.40) |
| Moderate | 2.61 (0.98) | 1.32 (0.57) | 2.78 (0.95) | 47.36 (17.47) |
| High | 2.28 (0.97) | 1.46 (0.74) | 2.81 (0.97) | 54.41 (17.59) |
Note: RS = Religious/spiritual, PCL = PTSD checklist. Significance of mean differences in variables 1–4 between combat exposure categories were calculated using ANOVA.
p < .05,
p < .01,
p < .001.
We also compared study variables of interest (RS coping, combat exposure, PTSD symptoms, and PPTG) by gender. Women scored significantly higher on positive RS coping than did men (women: M(SD) = 2.72(.96); men: M(SD) = 2.38(.96); t(625) = −4.32, p < .001). Negative RS coping did not vary by gender (women: M(SD) = 1.32(.60); men: M(SD) = 1.39(0.65); t(624) = 1.16; p = .67). Combat exposure group frequencies varied by sex (χ2(2) = 89.59, p < .001). Post-hoc comparisons demonstrated women were more likely than men to be in the low-exposure group (47.26% vs. 20.41%) and less likely to be in the high-exposure group (12.66% vs. 47.45%). There was no gender difference in likelihood of inclusion in the moderate-exposure group (women: 40.08%; men: 32.14%). Women had a significantly lower mean for PTSD symptoms than did men (women: M(SD) = 44.82(18.90); men: M(SD) = 48.45(18.28); t(626) = 2.38; p = .007). There was no gender difference in PPTG (women: M(SD) = 2.85(.99); men: M(SD) = 2.74(1.01); t(621) = −1.27; p = .26).
Hypothesis 1: Main Effects of Combat Exposure
We first hypothesized that combat exposure would be positively associated with both PTSD symptoms and PPTG. Regression results are displayed in Table 4. In the fully-adjusted main-effects only model, combat exposure was significantly and positively associated with PTSD symptoms. Those with moderate combat exposure had higher PCL scores than did those with low combat exposure (β = 8.23, 95% CI = 5.15, 11.31; p < .001), as did those with high combat exposure (β = 14.68, 95% CI = 11.34, 18.03; p < .001). Only high combat exposure was significantly positively associated with PPTG, relative to low exposure (β = 0.30, 95% CI = .09, .51; p = .004). Hypothesis 1 was therefore confirmed, with the qualification that only high, and not moderate, combat exposure was associated with elevated PPTG scores relative to low exposure. All gender interactions were non-significant.
Table 4.
Linear regression estimates
| PCL score (PTSD symptoms) | Perceived posttraumatic growth | |||
|---|---|---|---|---|
| Main effects only B (95% CI) |
Model with RS coping X Combat interactions B (95% CI) |
Main effects only B (95% CI) |
Model with RS coping X Combat interactions B (95% CI) |
|
| Intercept | 22.65 (14.15, 31.14)** | 21.49 (9.75, 33.23)** | 2.00 (1.48, 2.52)*** | 2.03 (1.32, 2.75)*** |
| Combat exposure | ||||
| Low | Ref. | Ref. | Ref. | Ref. |
| Moderate | 8.23 (5.15, 11.31)*** | 10.73 (−1.20, 22.67) | 0.08 (−0.11, 0.27) | 0.33 (−0.40, 1.06) |
| High | 14.68 (11.34, 18.03)*** | 11.45 (−0.15, 23.04) | 0.30 (0.09, 0.51)** | −0.07 (−0.78, 0.64) |
| RS coping: Positive | 0.62 (−0.75, 1.99) | −0.93 (−3.37, 1.51) | 0.29 (0.21, 0.38)*** | 0.29 (0.14, 0.44)*** |
| RS coping: Negative | 9.59 (7.54, 11.63)*** | 12.83 (8.47, 17.19)*** | −0.23 (−0.36, −0.11)*** | −0.26 (−0.52, 0.01) |
| RS coping: Positive X … | --- | --- | ||
| Low combat exposure | Ref. | Ref. | ||
| Moderate combat exposure | 1.26 (−1.99, 4.51) | −0.16 (0.36, 0.04) | ||
| High combat exposure | 3.27 (0.003, 6.54)* | 0.17 (−0.03, 0.37) | ||
| RS coping: Negative X … | --- | --- | ||
| Low combat exposure | Ref. | Ref. | ||
| Moderate combat exposure | −4.52 (−10.16, 1.12) | 0.13 (−0.22, 0.47) | ||
| High combat exposure | −3.70 (−8.88, 1.48) | −0.01 (−0.32, 0.31) | ||
| Age | 0.32 (0.16, 0.49)*** | 0.31 (0.14, 0.48)*** | 0.003 (−0.008, 0.013) | 0.002 (−0.01, 0.01) |
| Gender | ||||
| Male | Ref. | Ref. | Ref. | Ref. |
| Female | 1.51 (−1.32, 4.33) | 1.47 (−1.35, 4.29) | 0.06 (−0.11, 0.23) | 0.06 (−0.11, 0.24) |
| Education a | −1.45 (−2.56, −0.34)* | −1.40 (−2.51, −0.29)* | 0.01 (−0.06, 0.07) | 0.01 (−0.06, 0.07) |
| Household income b | −1.36 (−2.38, −0.35)** | −1.33 (−2.35, −0.31)* | 0.002 (−0.06, 0.06) | −0.01 (−0.07, 0.06) |
| Marital status | ||||
| Married or living with | ||||
| someone | Ref. | Ref. | Ref. | Ref. |
| Never married | −1.52 (−4.86, 1.82) | −1.87 (−5.21, 1.48) | 0.16 (−0.05, 0.36) | 0.14 (−0.06, 0.35) |
| Divorced/widowed/separated | 2.42 (−0.97, 5.81) | 2.49 (−0.91, 5.89) | −0.14 (−0.35, 0.07) | −0.15 (−0.39, 0.06) |
| Race/ethnicity | ||||
| White/Caucasian, non- | ||||
| Hispanic | Ref. | Ref. | Ref. | Ref. |
| Black/African American, | ||||
| non-Hispanic | 5.18 (1.34, 9.01)** | 5.39 (1.55, 9.23)** | 0.10 (−0.13, 0.34) | 0.12 (−0.12, 0.35) |
| Other, non-Hispanic | 1.51 (−3.29, 6.31) | 1.42 (−3.39, 6.23) | 0.32 (0.02, 0.61)* | 0.32 (0.03, 0.61)* |
| Hispanic | 4.99 (1.40, 8.58)** | 4.64 (1.04, 8.24)* | 0.18 (−0.04, 0.39) | 0.14 (−0.08, 0.36) |
Note: RS = Religious/spiritual, PCL = PTSD Checklist, Ref. = reference group
A mean education score of 5.17 is between the categories ‘Some college’ and ‘College graduate’
A mean household income score of 3.31 is between the categories ‘$35,000 to $50,000’ and ‘$50,000 to $75,000.’
Hypothesis 2: Main Effects of RS Coping
We hypothesized that higher positive RS coping would be associated with lower PTSD symptoms and higher PPTG; conversely, we hypothesized that negative RS coping would be associated with higher PTSD symptoms scores and lower PPTG. As shown in Table 4, positive RS coping was significantly and positively associated with PPTG (β = .29, 95% CI = 0.21, 0.38; p < .001), but was not related to PTSD symptoms (p = .37). Negative RS coping was positively associated with PTSD symptoms (β = 9.59, 95% CI = 7.54, 11.63; p < .001) and negatively associated with PPTG (β = −.23, 95% CI = −0.36, −0.11; p < .001). Therefore hypothesis 2 was supported, with the exception that positive RS coping was not associated with PTSD symptoms. No gender interaction was statistically significant.
Hypothesis 3: Moderation of RS Coping
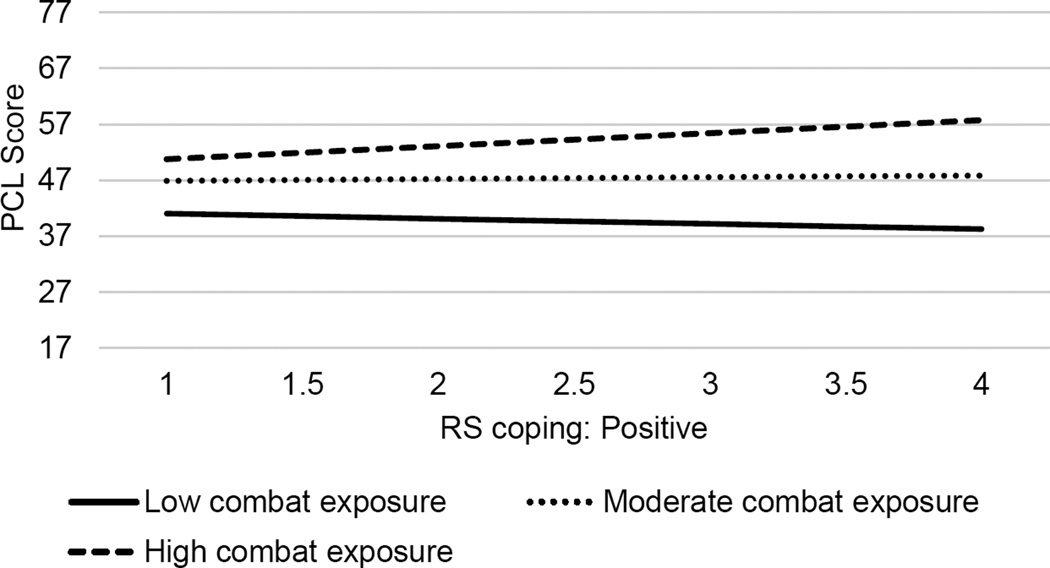
We hypothesized significant interactions between combat exposure and RS coping, with the following directions for associations: 1) positive coping would weaken the association between combat exposure and PTSD symptoms, 2) positive coping would strengthen the association between combat exposure and PPTG, 3) negative coping would strengthen the association between combat exposure and PTSD symptoms, and 4) negative coping would weaken the association between combat exposure and PPTG. As shown in Table 4, we found only one significant interaction: positive coping x high combat exposure (relative to low) in association with PTSD symptoms (Figure 1). The direction of the association was opposite from our hypothesis: Those with high combat and high positive coping had the highest levels of PTSD symptoms. No gender interaction was statistically significant.
Figure 1.
Interaction between combat exposure and religious/spiritual positive coping, in association with PCL score (PTSD symptom severity). PCL = PTSD Checklist, RS = Religious/spiritual. The slope for positive coping was significant and positive among those with high combat exposure scores (β = 2.34, 95% CI = 0.08, 4.59; p < .05). The slope for positive coping was non-significant for those with low and moderate combat exposure.
Discussion
This study advances our understanding of how religiousness and spirituality may function for veterans returning from the recent conflicts in Iraq, Afghanistan, and nearby regions. Although religiousness and spirituality have been shown to be important to the majority of military personnel, very little research has examined them in the context of their mental health. We built upon and expanded previous work demonstrating stress-buffering effects of religiousness and spirituality on combat exposure- adjustment links (Hourani et al., 2012). Focusing on veterans after their return from combat theater, we examined how RS coping relates to adjustment once they leave a warzone environment and separate from the military.
Before testing the stress-buffering effects, we first examined relations of both combat exposure and RS coping with adjustment. As expected, we found that combat exposure was indeed related to PTSD symptoms and PPTG. The more combat exposure a veteran had, the more symptoms he or she reported currently experiencing. These results are consistent with a great deal of work demonstrating a fairly linear relationship between combat exposure and symptomatology (e.g., Britt, Adler, Bliese, & Moore, 2013). Regarding combat exposure and PPTG, relationships were more complex than we had hypothesized: Only high levels of combat exposure were related to more PPTG, relative to low levels of combat. Previous research has also demonstrated fairly linear effects of combat exposure on PPTG (e.g., Gallaway, Millikan, & Bell, 2011). Consistent with a linear trend, our results showed a difference between moderate and low combat exposure in the hypothesized direction, although the difference did not reach statistical significance (p = .13). This lack of findings for low levels of combat may be due a significant amount of trauma being necessary in order to perceive one has grown from that experience (Cho & Park, 2014).
Consistent with our expectations, positive RS coping was related to PPTG but, unexpectedly, was not associated with PTSD symptoms. Further, higher negative RS coping was related to more PTSD symptoms and lower PPTG, as we had expected. These results regarding relations between RS coping and adjustment were fairly consistent with previous research on RS coping, which often fails to find links between positive RS coping and adjustment (e.g., Hebert, Zdaniuk, Schulz, & Scheier, 2009). Specifically within veteran samples, studies have found that negative RS coping is associated with poorer posttraumatic adjustment (e.g., Berg, 2011) and that positive RS coping relates to PPTG but not PTSD symptomatology (e.g., Ogden et al., 2012).
Still, it is disappointing that we did not identify aspects of RS coping that might be related to lower PTSD symptomatology. Such lack of protective effects is consistent with other literature on more general coping that identifies coping that is not helpful but does not identify coping that is helpful (e.g., Tyler Boden et al., 2014; Rodrigues & Renshaw, 2010). That negative RS coping was negatively related to PPTG is consistent with our expectations and the previous study of veterans that examined this issue (Ogden et al., 2012).
PPTG and PTSD symptoms were inversely related, suggesting that PPTG may indeed reflect a positive aspect of adjustment in our sample. Much previous research has found positive relationships between PTSD symptoms and PPTG among veterans (e.g., Pietrzak et al., 2010), but other studies found results similar to those of the present study, in which PPTG was related to better levels of mental health indices (e.g., Gallaway, Millikan, & Bell, 2011). These inconsistent findings suggest that PPTG may sometimes reflect distress and efforts to cope, while at other times, may reflect better functioning (Park & Helgeson, 2006). That negative RS coping was associated with lower PPTG is also supportive of this interpretation, perhaps reflecting underlying processes of poorer adjustment.
Our third set of hypotheses expected RS coping to moderate combat-PTSD/PPTG relationships. Contrary to our expectations, three of the four analyses did not demonstrate stress-buffering, and the one that did was in the direction opposite our hypothesis: Positive RS coping was related to higher levels of PTSD symptoms among those who had more combat exposure. This finding is consistent with the notion that positive RS coping may have not only been ineffective in alleviating symptoms of PTSD but may actually have strengthened the influence of high combat exposure. However, given the cross-sectional nature of our study, this finding may also reflect those with greater psychiatric distress turning to religiousness and spirituality for relief. As noted earlier, findings regarding the effects of positive RS coping are spotty and inconsistent (e.g., Thune-Boyle et al., 2006; Pargament, Koenig, & Perez, 2000), although, similar to our study, Mota and colleagues (Mota et al., 2013) found positive associations between spirituality and psychiatric outcomes in a sample of veterans. However, very little research has examined RS coping as a moderator of levels of traumatic exposure; thus, our findings are provocative but will require much additional research to replicate and understand.
Our finding that women reported greater positive RS coping compared to men is consistent with other military samples (McLaughlin et al., 2010). There were no gender differences in negative RS coping or in associations between negative RS coping and PTSD symptoms, suggesting interventions targeted at negative RS coping may benefit both male and female veterans. Only one gender difference emerged in associations between RS coping and trauma outcomes. Among those with moderate combat exposure, positive RS coping was more strongly related to greater PPTG for women compared to men. Therefore, although women did not score higher than men on PPTG, spirituality may play a more salient role in perceptions of growth for women compared to men.
Limitations of our study must be noted. The cross-sectional nature of the study design does not allow for teasing out causality or even directionality among the variables. For example, while it is plausible that combat exposure is reported accurately, it is possible that current PTSD symptoms may influence those recollections. It is also possible that combat exposure or PTSD symptoms influenced subsequent levels of RS coping as well as RS coping influencing PTSD. Therefore, it is quite likely that the relationship of negative RS coping and PTSD is bidirectional as well—individuals experiencing high levels of distress may draw more heavily on negative RS coping as well as the use of more RS coping leading to more distress. Such questions always arise with cross-sectional designs; at best, these data can provide only suggestive possibilities rather than convincing causal chains of explanation. Further, we did not assess RS coping specifically with military or combat stressors, but rather as a general coping style. Thus, we do not know if participants were using RS coping specifically to deal with their military stressors or their PTSD symptoms. Given that PPTG was self-reported, we could only measure perceived, rather than actual, growth. Additionally, using the short form for measuring positive and negative RS coping limits the number of specific RS coping methods that were assessed; however, empirical support for the short form still demonstrates good internal consistency, construct validity, predictive validity, and incremental validity (Pargament, Feuille, & Burdzy, 2011).
Because our RS coping items included a response of not believing in God, we were unable to include individuals who answered the items in this way in analyses of RS coping. This exclusion is unfortunate because studies often find that individuals report not believing in God yet report a fair amount of religious coping (Exline & Rose, 2013). In fact, individuals who are engaging in a great deal of negative RS coping may be more likely to endorse a lack of belief in God (Exline & Rose, 2013). Future research is needed to understand the associations between RS coping and psychological adjustment in veterans who identify as not believing in God.
In spite of these limitations, our findings clearly illustrate the need to attend to veterans’ RS issues to better understand their post-deployment adjustment. Future research should be designed to be longitudinal and, ideally, prospective. It would be useful to know more about the specific coping efforts of the veterans, including the events to which they refer describing their coping, and to incorporate non-RS coping along with RS coping into studies to understand their interplay.
Our findings also support the notion that addressing spiritual issues could play an important role in mental health treatment for veteran populations (Fontana & Rosenheck, 2004). Several recent intervention efforts highlight these possibilities. For example, Harris and colleagues (Harris et al., 2011) have developed a trauma-focused, spiritually-integrated intervention and demonstrated promising initial findings for helping veterans alleviate negative religious coping and resolve spiritual struggles. Taking another approach, Bormann and colleagues (Bormann, Thorp, Wetherell, Golshan, & Lang, 2013) demonstrated that mantram meditation reduced PTSD symptoms among veterans, and that the improvements were mediated by increasing spiritual well-being (Bormann, Liu, Thorp, & Lang, 2012). Given the strong and urgent need for alternative effective treatments for returning veterans’ mental health issues (e.g., Kroesen, Baldwin, Brooks, & Bell, 2002; Smeeding, Bradshaw, Humpfer, Trevithick, & Stoddard, 2010), RS avenues are promising. Before such approaches can be wholeheartedly embraced, much future research on the roles of various RS aspects and mental health should be vigorously pursued.
Acknowledgments
This study was funded by Veteran’s Affairs CSR&D Grant ZDA1 and NIH P50DA033945 (SAM) and T32MH06299412
Contributor Information
Crystal L. Park, University of Connecticut, Department of Psychology
Philip H. Smith, Yale University School of Medicine, Department of Psychiatry; Women’s Health Research at Yale
Sharon Y. Lee, University of Connecticut, Department of Psychology
Carolyn M. Mazure, Yale University School of Medicine, Department of Psychiatry; Women’s Health Research at Yale
Sherry A. McKee, Yale University School of Medicine, Department of Psychiatry; Women’s Health Research at Yale
Rani Hoff, Yale University School of Medicine, Department of Psychiatry; Women’s Health Research at Yale; VISN1 MIRECC, VA Connecticut Healthcare System.
References
- Aldwin CM, Park CL, Jeong Y-J, Nath R. Differing pathways between religiousness, spirituality, and health: A self-regulation perspective. Psychology of Religion and Spirituality. 2014;6:9–21. [Google Scholar]
- Besterman-Dahan K, Gibbons SW, Barnett SD, Hickling EJ. The role of military chaplains in mental health care of the deployed service member. Military Medicine. 2012;177:1028–1033. doi: 10.7205/milmed-d-12-00071. [DOI] [PubMed] [Google Scholar]
- Bormann JE, Thorp SR, Wetherell JL, Golshan S, Lang AJ. Meditation based mantram intervention for veterans with posttraumatic stress disorder: A randomized trial. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:259–267. [Google Scholar]
- Bormann JE, Liu L, Thorp SR, Lang AJ. Spiritual wellbeing mediates PTSD change in veterans with military-related PTSD. International Journal of Behavioral Medicine. 2012;19:496–502. doi: 10.1007/s12529-011-9186-1. [DOI] [PubMed] [Google Scholar]
- Britt TW, Adler AB, Bliese PD, Moore D. Morale as a moderator of the combat exposure-PTSD symptom relationship. Journal of Traumatic Stress. 2013;26:94–101. doi: 10.1002/jts.21775. [DOI] [PubMed] [Google Scholar]
- Chang BH, Skinner KM, Boehmer U. Religion and mental health among women veterans with sexual assault experience. International Journal of Psychiatry in Medicine. 2001;31:77–95. doi: 10.2190/0NQA-YAJ9-W0AM-YB3P. [DOI] [PubMed] [Google Scholar]
- Chang BH, Skinner KM, Zhou C, Kazis LE. The relationship between sexual assault, religiosity, and mental health among male veterans. The International Journal of Psychiatry in Medicine. 2003;33:223–239. doi: 10.2190/NM3D-EWYR-4B59-DFM8. [DOI] [PubMed] [Google Scholar]
- Cho D, Park CL. Growth following trauma: Overview and current status. Terapia Psicologica. 2013;31:69–79. [Google Scholar]
- Exline JJ, Rose E. Religious and spiritual struggles. In: Paloutzian RF, Park CL, editors. Handbook of the Psychology of Religion and Spirituality. 2nd. New York: Guilford; 2013. pp. 380–398. [Google Scholar]
- Fetzer Institute & National Institute on Aging. Multidimensional measurement of religiousness/spirituality for use in health research. Kalamazoo, MI: Fetzer Institute; 1999. [Google Scholar]
- Fontana A, Rosenheck R. Trauma, change in strength of religious faith and mental health service use among veterans treated for PTSD. The Journal of Nervous and Mental Disease. 2004;192:579–584. doi: 10.1097/01.nmd.0000138224.17375.55. [DOI] [PubMed] [Google Scholar]
- Gallaway MS, Millikan AM, Bell MR. The association between deployment related posttraumatic growth among US Army soldiers and negative behavioral health conditions. Journal of Clinical Psychology. 2011;67:1151–1160. doi: 10.1002/jclp.20837. [DOI] [PubMed] [Google Scholar]
- Berg G. The relationship between spiritual distress, PTSD and depression in Vietnam combat veterans. The Journal of Pastoral Care & Counseling. 2011;65:1–11. doi: 10.1177/154230501106500106. No doi available. [DOI] [PubMed] [Google Scholar]
- Boden MT, Kimerling R, Kulkarni M, Bonn-Miller MO, Weaver C, Trafton J. Coping among military veterans with PTSD in substance use disorder treatment. Journal of Substance Abuse and Treatment. 2014;47:160–167. doi: 10.1016/j.jsat.2014.03.006. [DOI] [PubMed] [Google Scholar]
- Feder A, Ahmad S, Lee EJ, Morgan JE, Singh R, Smith BW, Charney DS. Coping and PTSD symptoms in Pakistani earthquake survivors: Purpose in life, religious coping and social support. Journal of Affective Disorders. 2013;147:156–163. doi: 10.1016/j.jad.2012.10.027. [DOI] [PubMed] [Google Scholar]
- Gerber MM, Boals A, Schuettler D. The unique contributions of positive and negative religious coping to posttraumatic growth and PTSD. Psychology of Religion and Spirituality. 2011;3:298–307. [Google Scholar]
- Harris JI, Erbes CR, Engdhal BE, Thuras P, Ogden H, Olson RHA, Winskowski AM, Bacon R, Malec C, Campoin K, Le T. The effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma. Journal of Clinical Psychology. 2011;67:425–438. doi: 10.1002/jclp.20777. [DOI] [PubMed] [Google Scholar]
- Hebert R, Zdaniuk B, Schulz R, Scheier M. Positive and negative religious coping and well-being in women with breast cancer. Journal of Palliative Medicine. 2009;12:537–545. doi: 10.1089/jpm.2008.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henslee AM, Coffey SF, Schumacher JA, Tracy MH, Norris F, Galea S. Religious coping and psychological and behavioral adjustment after Hurricane Katrina. The Journal of Psychology. 2014:1–13. doi: 10.1080/00223980.2014.953441. online first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hourani LL, Williams J, Forman-Hoffman V, Lane ME, Weimer B, Bray RM. Influence of spirituality on depression, posttraumatic stress disorder, and suicidality in active duty military personnel. Depression Research and Treatment. 2012 doi: 10.1155/2012/425463. Article 425463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroesen K, Baldwin CM, Brooks AJ, Bell IR. US military veterans’ perceptions of the conventional medical care system and their use of complementary and alternative medicine. Family Practice. 2002;19:57–64. doi: 10.1093/fampra/19.1.57. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, Samper RE. Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology. 2006;18:89–120. [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, Maguen S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review. 2009;29:695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- McLaughlin SS, McLaughlin AD, Van Slyke JA. Faith and religious beliefs in outpatient military population. Southern Medical Journal. 2010;103:527–531. doi: 10.1097/SMJ.0b013e3181de0304. [DOI] [PubMed] [Google Scholar]
- Mota NP, Medved M, Whitney D, Hiebert-Murphy D, Sareen J. Protective factors for mental disorders and psychological distress in female, compared with male, service members in a representative sample. Canadian Journal of Psychiatry. 2013;58:570–578. doi: 10.1177/070674371305801006. [DOI] [PubMed] [Google Scholar]
- Ogden H, Harris J, Erbes CR, Engdahl BE, Olson RA, Winskowski A, McMahill J. Religious functioning and trauma outcomes among combat veterans. Counselling and Spirituality/Counseling et Spiritualité. 2011;30:71–89. [Google Scholar]
- Pargament K, Feuille M, Burdzy D. The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions. 2011;2:51–76. [Google Scholar]
- Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: Development and initial validation of the RCOPE. Journal of Clinical Psychology. 2000;56:519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pargament KI, Smith BW, Koenig HG, Perez L. Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion. 1998;37:710–724. [Google Scholar]
- Pargament K, Sweeney P. Building spiritual fitness in the army: An innovative approach to a vital aspect of human development. American Psychologist. 2011;66:58–64. doi: 10.1037/a0021657. [DOI] [PubMed] [Google Scholar]
- Park CL, Helgeson VS. Growth following highly stressful life events: Current status and future directions. Journal of Consulting and Clinical Psychology. 2006;74:791–796. doi: 10.1037/0022-006X.74.5.791. [DOI] [PubMed] [Google Scholar]
- Park NS, Lee BS, Sun F, Klemmack DL, Roff LL, Koenig HG. Typologies of religiousness/spirituality: Implications for health and well-being. Journal of Religion and Health. 2013;52:828–839. doi: 10.1007/s10943-011-9520-6. [DOI] [PubMed] [Google Scholar]
- Park CL, Slattery JM. Religion and emotional health and well-being. In: Paloutzian RF, Park CL, editors. Handbook of the Psychology of Religion and Spirituality. 2nd. New York: Guilford; 2013. pp. 540–559. [Google Scholar]
- Pietrzak RH, Goldstein MB, Malley JC, Rivers AJ, Johnson DC, Morgan CA, III, Southwick SM. Posttraumatic growth in veterans of Operations Enduring Freedom and Iraqi Freedom. Journal of Affective Disorders. 2010;126:230–235. doi: 10.1016/j.jad.2010.03.021. [DOI] [PubMed] [Google Scholar]
- Rodrigues CS, Renshaw KD. Associations of coping processes with posttraumatic stress disorder symptoms in national guard/reserve service members deployed during the OEF-OIF era. Journal of Anxiety Disorders. 2010;24:694–699. doi: 10.1016/j.janxdis.2010.04.013. [DOI] [PubMed] [Google Scholar]
- Schreiber JA, Brockopp DY. Twenty-five years later - what do we know about religion/spirituality and psychological well-being among breast cancer survivors? A systematic review. Journal of Cancer Survivorship. 2012;6:82–94. doi: 10.1007/s11764-011-0193-7. [DOI] [PubMed] [Google Scholar]
- Shannon DK, Oakes KE, Scheers NJ, Richardson FJ, Stills AB. Religious beliefs as moderator of exposure to violence in African American adolescents. Psychology of Religion and Spirituality. 2013;5:172–181. [Google Scholar]
- Smeeding SJ, Bradshaw DH, Humpfer K, Trevithick S, Stoddard GJ. Outcome evaluation of the Veterans Affairs Salt Lake City Integrative Health Clinic for chronic pain and stress-related depression, anxiety, and post-traumatic stress disorder. Alternative and Complementary Medicine. 2010;16:823–835. doi: 10.1089/acm.2009.0510. [DOI] [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9:455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- Thune-Boyle IC, Stygall JA, Keshtgar MR, Newman SP. Do religious/spiritual coping strategies affect illness adjustment in patients with cancer? A systematic review of the literature. Social Science & Medicine. 2006;63:151–164. doi: 10.1016/j.socscimed.2005.11.055. [DOI] [PubMed] [Google Scholar]
- Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and Anxiety. 2011;28:596–606. doi: 10.1002/da.20837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witvliet CVO, Phipps KA, Feldman ME, Beckham JC. Posttraumatic mental and physical health correlates of forgiveness and religious coping in military veterans. Journal of Traumatic Stress. 2004;17:269–273. doi: 10.1023/B:JOTS.0000029270.47848.e5. [DOI] [PubMed] [Google Scholar]
- Wortmann J, Park CL. Religion and spirituality in adjustment following bereavement: An integrative review. Death Studies. 2008;32:703–736. doi: 10.1080/07481180802289507. [DOI] [PubMed] [Google Scholar]
- Ysseldyk R, Matheson K, Anisman H. Religiosity as identity: Toward an understanding of religion from a social identity perspective. Personality and Social Psychology Review. 2010;14:60–71. doi: 10.1177/1088868309349693. [DOI] [PubMed] [Google Scholar]