Abstract
Background
Small-cell lung cancer (SCLC) is responsive to initial chemotherapy but becomes resistant to cytotoxic drugs. The aim of this study was to evaluate what proportion of patients with SCLC had received the first- and further-line chemotherapy and which patients had benefited from chemotherapy.
Methods
We retrospectively reviewed medical records of patients with SCLC who had been treated with the best supportive care alone and the first-, second-, or third-line chemotherapy at the Osaka Police Hospital from June 2007 until March 2015.
Results
Among 145 patients diagnosed with SCLC and eligible for analysis, 118 patients received chemotherapy. We added five patients who initiated the second-line chemotherapy during the study period at our institution. Sixty-five and 31 patients received the second- and third-line chemotherapies, respectively. Multivariate logistic regression analysis detected age ≥75 years (odds ratio, 2.80; 95% confidence interval, 1.01–7.75; P=0.047) and European Clinical Oncology Group Performance Status (ECOG PS) 3–4 (14.3; 4.86–41.9; P<0.01) as factors disturbing the introduction of chemotherapy. Multivariate Cox hazard analyses also detected ECOG PS 2–4 (3.34; 2.00–5.58; P<0.01) as a factor decreasing overall survival after the first-line chemotherapy, and C-reactive protein level ≥1.0 mg/dL (2.67; 1.30–5.47; P<0.01) and progression-free survival after the first-line chemotherapy ≥6 months (2.85; 1.50–5.43; P<0.01) as factors influencing overall survival after the second-line chemotherapy.
Conclusion
Approximately two-thirds and one-third of the patients who receive chemotherapy proceed to the second- and third-line chemotherapies, respectively. Several factors, such as age, ECOG PS, C-reactive protein level, and progression-free survival after previous treatment may be useful when considering the introduction of further-line chemotherapy.
Keywords: small-cell lung cancer, first-line chemotherapy, second-line chemotherapy, third-line chemotherapy, retrospective study, overall survival
Introduction
Small-cell lung cancer (SCLC) accounts for 15% of all lung cancers and is a highly aggressive tumor marked by early metastases and poor prognosis. Approximately 60%–75% of all patients with SCLC are found to have extensive disease at the time of diagnosis.1–3 SCLC is responsive to initial chemotherapy, but most patients progress within months. Thus, salvage chemotherapy is required. Although topotecan4 or amrubicin5 monotherapy may be the most optimal regimen in the second-line setting, their efficacy is unsatisfactory compared with that of the first-line regimen. Despite a good response to front-line chemotherapy, SCLC gradually becomes resistant to cytotoxic drugs in the further-line settings. Regarding the third- or further-line chemotherapy, there is no evidence-based recommended regimen.
The aim of our retrospective study was to evaluate what proportion of the patients with SCLC had actually received first- to third-line chemotherapies and which patients had benefited from chemotherapy.
Methods
Patient selection and experimental design
The study was carried out at the Osaka Police Hospital, Japan. We retrospectively reviewed electronic medical records and collected data on patients who had been diagnosed with SCLC histologically or cytologically, and who had been treated with the best supportive care alone and the first-, second-, or third-line chemotherapy at our hospital from June 2007 to March 2015. We excluded patients with combined SCLC, defined as SCLC combined with non-SCLC components.6 First, for the evaluation of factors that had influenced the introduction of chemotherapy, we analyzed a cohort of patients who had been diagnosed with SCLC at our hospital from June 2007 to March 2015 and compared the following two groups within the cohort: patients who received chemotherapy and patients who did not receive it after the diagnosis of SCLC. We excluded patients who had moved to other hospitals for further aggressive treatment after confirmed diagnosis. Second, for the investigation of factors associated with prognosis of the first- to third-line chemotherapies, we analyzed three retrospective cohorts of patients who had initiated chemotherapy from June 2007 to March 2015 at our hospital. The data collected from the patients’ medical records included the following: sex, age, European Clinical Oncology Group (ECOG) performance status (PS),7 clinical stage based on the seventh edition of TNM Classification of Malignant Tumours by the International Union Against Cancer and the American Joint Committee on Cancer,8 distant metastases, Charlson comorbidity index,9 chemotherapeutic regimens, body mass index (BMI), laboratory data, progression-free survival (PFS), overall survival (OS), response according to Response Evaluation Criteria In Solid Tumors Version 1.1,10 delivered cycles, and the reason for discontinuation of each regimen. In this study, we did not practically use the staging system proposed by Veterans Administration Lung Study Group,11 but we routinely adopted the TNM staging system.8 The Osaka Police Hospital Ethics Committee approved this study (number 501) and waived the requirement for informed consent.
Assessments
The evaluable population for overall response included all patients who had received at least one cycle of chemotherapy, and at least two response assessments over 6 weeks after the start of chemotherapy were necessary unless the documentation of objective progressive disease (PD). For patients who did not receive chemotherapy, OS was measured from diagnosis. For patients who received chemotherapy, OS was measured from the first day of chemotherapy, and PFS was defined as a period from the first day of chemotherapy until documented PD or death. The date of data cut-off was July 31, 2015.
Data analysis
The data for normally distributed continuous variables and categorical variables were expressed as the mean ± standard deviation and frequency. Comparisons between the two groups were performed using the chi-square test for relative frequencies, the Mann–Whitney U test for discrete variables, the unpaired t-test for normally distributed continuous variables, and log-rank test for survival time. Pearson’s correlation coefficient was used to evaluate the relationship between laboratory variables. Univariate and multivariate logistic regression analyses were used to examine which variables at diagnosis or before treatment influenced the decision whether or not to introduce chemotherapy. Independent variables in the univariate analyses were as follows: age, sex, ECOG PS, stage, extrathoracic metastases, BMI, and Charlson comorbidity index, at diagnosis of malignancy for patients who did not receive chemotherapy (nonchemotherapy group) and before the first-line chemotherapy for patients who received chemotherapy (chemotherapy group). On the other hand, univariate and multivariate Cox proportional hazards’ models were used to examine which pretreatment backgrounds influenced OS after the first- to third-line chemotherapies. Independent variables in the univariate analyses were as follows: age, sex, ECOG PS, stage, BMI, neutrophil-to- lymphocyte ratio,12 platelet-to-lymphocyte ratio (PLR),12 lymphocyte-to- monocyte ratio (LMR),13 hemoglobin,14,15 serum sodium,16,17 lactate dehydrogenase (LDH),15 alkaline phosphatase,18,19 C-reactive protein (CRP),20 and PFS after the first- or second-line15 chemotherapy. We defined the cut-off points of these laboratory data according to previous studies that had evaluated the association between the prognosis of patients with lung cancer and their pretreatment laboratory data. Instead of the type of sensitive or refractory relapse, which has been recognized as an important prognostic factor, we arbitrarily divided our patients by 6 months of PFS from the start of the first-line chemotherapy: first, because we could not decide the type of relapse precisely for the lack of sufficient clinical information during the first-line chemotherapy in five patients; second, because median time to the second-line therapy had been reported to be 6.9 months in a multi- institutional retrospective analysis of the second-line chemotherapy for SCLC21; and third, because, considering mean-delivered courses (3.9 courses) of the first-line chemotherapy in our study, approximately 6 months from the start of the first-line chemotherapy was reasonable as a borderline of two types of relapse. All variables with a P-value of <0.05 in univariate analysis were included in the multivariate analysis. The results were evaluated in terms of odds ratio (OR), hazard ratio (HR), and 95% confidence interval (CI). A P-value of <0.05 was considered statistically significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander, which is designed to add statistical functions frequently used in biostatistics.22
Results
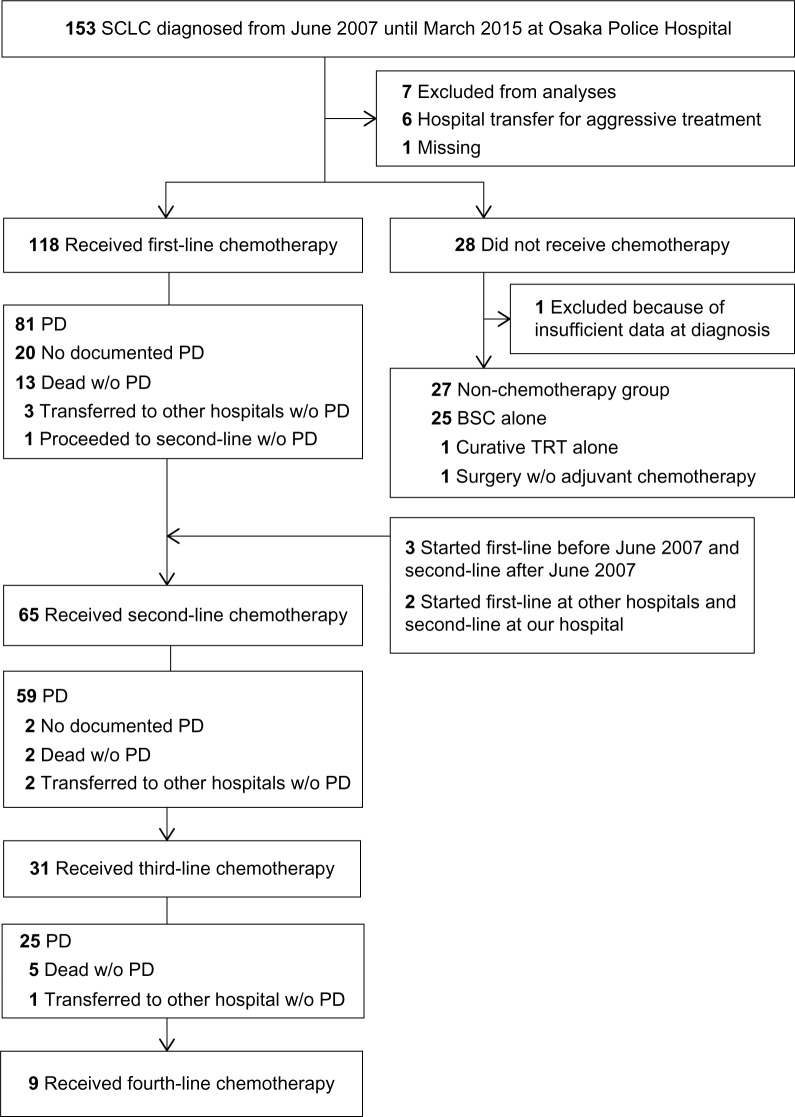
From June 2007 to March 2015, among 153 patients diagnosed with SCLC and 93 patients diagnosed with stage IV, 118 and 72 patients received the first-line chemotherapy, respectively. Eight patients were excluded from analysis because of transfer to other hospitals for aggressive treatment (n=6), missing (n=1), and insufficient data at diagnosis (n=1). Among 94 patients, which included those who progressed or died after or during the first-line chemotherapy until March 2015, 60 patients (64%) received the second-line chemotherapy until March 2015. We added three patients who had started the first-line chemotherapy before June 2007 and then the second-line chemotherapy after June 2007, and two patients who had started the first-line chemotherapy at other hospitals and the second-line chemotherapy at our hospital. Sixty-five patients received the second-line chemotherapy at our hospital. Among 55 patients, which included those who progressed after or during the second-line chemotherapy until March 2015, 31 patients (56%) received the third-line chemotherapy until March 2015 (Figure 1).
Figure 1.
Flow diagram of patients with small-cell lung cancer.
Abbreviations: BSC, best supportive care; PD, progressive disease; SCLC, small-cell lung cancer; TRT, thoracic radiotherapy; w/o, without.
Compared with the chemotherapy group (n=118), the nonchemotherapy group (n=27) was significantly older (75.4±8.6 vs 70.2±8.9 years; P<0.01), had poorer ECOG PS (P<0.01), and had higher Charlson comorbidity index (2.4±1.6 vs 1.5±1.4; P<0.01) and shorter survival time (median 114 vs 356 days; P<0.01) (Table 1). The univariate analyses detected age ≥75 years (OR 3.44; 95% CI 1.44–8.22; P<0.01), ECOG PS 3–4 (OR 15.1; 95% CI 5.46–41.9; P<0.01), and Charlson comorbidity index ≥2 (OR 2.82; 95% CI 1.17–6.79; P=0.02) as factors influencing the introduction of chemotherapy, while multivariate analysis detected age (OR 2.82; 95% CI 1.01–7.75; P=0.047) and ECOG PS (OR 14.3; 95% CI 4.86–41.9; P<0.01) (Table 2).
Table 1.
Characteristics of patients according to chemotherapy history
| Variables | Chemotherapy | Nonchemotherapya | P-value |
|---|---|---|---|
| N | 118 | 27 | |
| Age (years) | |||
| Mean ± SD | 70.2±8.9 | 75.4±8.6 | <0.01b |
| Median (range) | 70 (43–88) | 79 (58–87) | |
| Sex | |||
| Male/female | 94/24 | 20/7 | 0.69c |
| Staging | |||
| I–II/III/IV/not assessed | 11/35/72/0 | 2/3/21/1 | |
| IV vs others | 0.17c | ||
| Extrathoracic distant metastases | |||
| Brain/liver/bone/others | 14/25/15/14 | 6/10/7/6 | |
| Yes/no | 51/67 | 14/13 | 0.42c |
| ECOG PS | |||
| 0–1/2/3/4 | 85/24/9/0 | 5/7/11/4 | <0.01d |
| BMI (kg/m2) | |||
| Mean ± SD | 22.6±3.9 | 21.5±3.5 | 0.22b |
| Charlson comorbidity index | |||
| Mean ± SD | 1.5±1.4 | 2.4±1.6 | <0.01d |
| Overall survival (days)e | |||
| Median (95% CI) | 356 (280–417) | 114 (21–NA) | <0.01f |
Notes:
One patient received only curative thoracic radiotherapy without systemic chemotherapy, another patient received only curative surgical resection without adjuvant chemotherapy, and the others received best supportive care alone.
Unpaired t-test.
Chi-square test.
Mann–Whitney U test.
From initiation of first-line chemotherapy for the chemotherapy group and from diagnosis for the nonchemotherapy group.
Log-rank test.
Abbreviations: BMI, body mass index; CI, confidence interval; ECOG, European Clinical Oncology Group; NA, not available; PS, performance status; SD, standard deviation.
Table 2.
Univariate and multivariate logistic regression analyses of factors influencing the introduction of chemotherapy
| Variables | Univariate
|
Multivariate
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Age (years) | ||||||
| <75 vs ≥75 | 3.44 | 1.44–8.22 | <0.01 | 2.80 | 1.01–7.75 | 0.047 |
| Sex | ||||||
| Male vs female | 1.37 | 0.52–3.62 | 0.52 | |||
| ECOG PS | ||||||
| 0–2 vs 3–4 | 15.1 | 5.46–41.9 | <0.01 | 14.3 | 4.86–41.9 | <0.01 |
| Staging | ||||||
| I–III vs IV | 2.32 | 0.87–6.17 | 0.09 | |||
| Extrathoracic metastases | ||||||
| No vs yes | 1.46 | 0.64–3.35 | 0.37 | |||
| BMI (kg/m2) | ||||||
| ≥18.5 vs <18.5 | 1.40 | 0.50–3.91 | 0.52 | |||
| Charlson comorbidity index | ||||||
| 0–1 vs ≥2 | 2.82 | 1.17–6.79 | 0.02 | 2.33 | 0.83–6.54 | 0.11 |
Note: Coded as 1 (age ≥75 years, female, ECOG PS 3–4, stage IV, positive extrathoracic distant metastases, BMI <18.5 kg/m2, and Charlson comorbidity index ≥2) and as 0 (age <75 years, male, ECOG PS 0–2, stages I–III, no extrathoracic distant metastasis, BMI ≥18.5 kg/m2, and Charlson comorbidity index 0–1).
Abbreviations: BMI, body mass index; CI, confidence interval; ECOG, European Clinical Oncology Group; OR, odds ratio; PS, performance status.
Table 3 shows the backgrounds of patients who received the second- and third-line chemotherapies. Table S1 presents the pretreatment laboratory data of patients who received the first-, second-, and third-line chemotherapies. The most frequent regimen was carboplatin plus etoposide in the first-line setting and amrubicine monotherapy in the second- and third-line settings. All but one patient received the platinum-based doublet regimen as the first-line regimen. In the second-line regimen, 33 and four patients were rechallenged with platinum and a regimen used in the first-line chemotherapy, respectively. In the third-line regimen, five patients were rechallenged with platinum, and one patient received platinum-based regimen in all three lines (Table S2). The most frequent reasons of discontinuation were the completion of defined courses in the first-line setting (46%), and PD in the second- (63%) and third-line settings (58%). The overall response and disease control rates, PFS, and OS gradually decreased from the first- to third-line settings (Table S3).
Table 3.
Characteristics of patients who received second- or third-line chemotherapy
| Variables | Second-line chemotherapy | Third-line chemotherapy |
|---|---|---|
| N | 65 | 31 |
| Age (years)a | ||
| Mean ± SD | 69.3±8.7 | 67.5±8.5 |
| Sex | ||
| Male/female | 55/10 | 26/5 |
| Staginga | ||
| III/IV | 7/58 | 2/29 |
| Extrathoracic distant metastasesa | ||
| Brain/liver/bone/others | 20/14/10/18 | 13/10/8/9 |
| ECOG PSa | ||
| 0–1/2/3/4 | 43/19/3/0 | 18/11/2/0 |
| BMI (kg/m2)a | ||
| Mean ± SD | 23.1±4.1 | 22.5±4.0 |
| Overall survival (days)b | ||
| Median (95% CI) | 218 (150–243) | 123 (94–177) |
Notes:
At the start of each line chemotherapy.
From the initiation of the second-or third-line chemotherapy.
Abbreviations: BMI, body mass index; CI, confidence interval; ECOG, European Clinical Oncology Group; PS, performance status; SD, standard deviation.
The univariate analyses detected the following eight variables as factors decreasing the OS after the first-line chemotherapy: ECOG PS 2–4 (HR 2.72; 95% CI 1.73–4.29; P<0.01), stage IV (HR 1.96; 95% CI 1.25–3.08; P<0.01), PLR ≥150 (HR 2.03; 95% CI 1.31–3.13; P<0.01), LMR <4(HR 1.67; 95% CI 1.07–2.59; P=0.02), hemoglobin <11 g/dL (HR 2.03; 95% CI 1.12–3.69; P=0.02), serum sodium <135 mEq/L (HR 1.92; 95% CI 1.11–3.32; P=0.02), LDH ≥225 IU/L (HR 1.73; 95% CI 1.10–2.73; P=0.02), and CRP ≥1 mg/dL (HR 1.67; 95% CI 1.09–2.55; P=0.02) (Table 4). Because of a significant correlation between PMR and LMR (r=0.41; 95% CI 0.25−0.55; P<0.01), and same laboratory data (lymphocyte) included in these two variables, we selected PMR in the multivariate model. Multivariate analysis detected only ECOG PS (HR 3.34; 95% CI 2.00–5.58; P<0.01) (Table 5). On the other hand, univariate analysis detected the following five variables as factors decreasing the OS after the second line chemotherapy: PLR ≥150 (HR 1.76; 95% CI 1.02–3.04; P=0.04), serum sodium <135 mEq/L (HR 2.30; 95% CI 1.09–4.85; P=0.03), LDH ≥225 IU/L (HR 1.97; 95% CI 1.15–3.41; P=0.01), CRP ≥1 mg/dL (HR 3.23; 95% CI 1.77–5.92; P<0.01), and PFS after the first-line chemotherapy <6 months (HR 2.85; 95% CI 1.58–5.12; P<0.01) (Table 4); while multivariate analysis detected only CRP (HR 2.67; 95% CI 1.30–5.47; P<0.01) and PFS after the first-line chemotherapy (HR 2.85; 95% CI 1.50–5.43; P<0.01) (Table 5). We did not detect any significant prognostic factor for the third-line chemotherapy (Table 4).
Table 4.
Univariate Cox hazard analyses of factors associated with overall survival after the first-, second-, and third-line chemotherapies
| Factors | First-line chemotherapy
|
Second-line chemotherapy
|
Third-line chemotherapy
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Age (years) | |||||||||
| <75 vs ≥75 | 1.20 | 0.76–1.89 | 0.43 | 0.74 | 0.41–1.34 | 0.32 | 1.38 | 0.53–3.59 | 0.51 |
| Sex | |||||||||
| Male vs female | 0.81 | 0.46–1.42 | 0.46 | 1.01 | 0.48–2.16 | 0.97 | 1.19 | 0.45–3.17 | 0.73 |
| ECOG PS | |||||||||
| 0–1 vs 2–4 | 2.72 | 1.73–4.29 | <0.01 | 1.26 | 0.73–2.16 | 0.41 | 2.09 | 0.94–4.67 | 0.07 |
| Stage | |||||||||
| I–III vs IV | 1.96 | 1.25–3.08 | <0.01 | 1.24 | 0.53–2.89 | 0.62 | 5.08 | 0.67–38.4 | 0.12 |
| BMI (kg/m2) | |||||||||
| ≥18.5 vs <18.5 | 1.30 | 0.77–2.22 | 0.33 | 0.90 | 0.42–1.92 | 0.78 | 2.71 | 0.77–9.53 | 0.12 |
| NLR | |||||||||
| <5 vs ≥5 | 1.54 | 0.90–2.67 | 0.12 | 1.60 | 0.84–3.04 | 0.15 | 0.72 | 0.21–2.40 | 0.59 |
| PLR | |||||||||
| <150 vs ≥150 | 2.03 | 1.31–3.13 | <0.01 | 1.76 | 1.02–3.04 | 0.04 | 1.49 | 0.68–3.26 | 0.32 |
| LMR | |||||||||
| ≥4 vs <4 | 1.67 | 1.07–2.59 | 0.02 | 1.30 | 0.72–2.31 | 0.38 | 1.56 | 0.53–4.56 | 0.42 |
| Hemoglobin (g/dL) | |||||||||
| ≥11 vs <11 | 2.03 | 1.12–3.69 | 0.02 | 1.54 | 0.90–2.64 | 0.12 | 1.69 | 0.76–3.76 | 0.20 |
| Serum sodium (mEq/L) | |||||||||
| ≥135 vs <135 | 1.92 | 1.11–3.32 | 0.02 | 2.30 | 1.09–4.85 | 0.03 | 2.86 | 0.64–12.7 | 0.17 |
| LDH (IU/L) | |||||||||
| <225 vs ≥225 | 1.73 | 1.10–2.73 | 0.02 | 1.97 | 1.15–3.41 | 0.01 | 1.73 | 0.79–3.79 | 0.17 |
| ALP (IU/L) | |||||||||
| ≤340 vs >340 | 1.48 | 0.89–2.47 | 0.13 | 1.37 | 0.64–2.89 | 0.42 | 1.06 | 0.42–2.65 | 0.91 |
| CRP (mg/dL) | |||||||||
| <1 vs ≥1 | 1.67 | 1.09–2.55 | 0.02 | 3.23 | 1.77–5.92 | <0.01 | 1.40 | 0.65–3.01 | 0.39 |
| PFS after first-line chemotherapy (months) | |||||||||
| ≥6 vs <6 | – | – | – | 2.85 | 1.58–5.12 | <0.01 | 1.54 | 0.71–3.34 | 0.28 |
| PFS after second-line chemotherapy (months) | |||||||||
| ≥3 vs <3 | – | – | – | – | – | – | 1.72 | 0.79–3.78 | 0.18 |
Note: Coded as 1 (age ≥75 years, female, ECOG PS 2–4, stage IV, BMI <18.5 kg/m2, NLR ≥5, PLR ≥150, LMR <4, hemoglobin <11 g/dL, serum sodium <135 mEq/L, LDH ≥225 IU/L, ALP >340 IU/L, CRP ≥1 mg/dL, PFS after the first-line chemotherapy <6 months, and PFS after the second-line chemotherapy <3 months) and as 0 (age <75 years, male, ECOG PS 0–1, stages I–III, BMI ≥18.5 kg/m2; NLR <5, PLR <150, LMR ≥4, hemoglobin ≥11 g/dL, serum sodium ≥135 mEq/L, LDH <225 IU/L, ALP ≤340 IU/L, CRP <1 mg/dL, PFS after the first-line chemotherapy ≥6 months, and PFS after the second-line chemotherapy ≥3 months).
Abbreviations: ALP, alkaline phosphatase; BMI, body mass index; CI, confidence interval; CRP, C-reactive protein; ECOG, European Clinical Oncology Group; HR, hazard ratio; LDH, lactate dehydrogenase; LMR, lymphocyte-to-monocyte ratio; NLR, neutrophil-to-lymphocyte ratio; PFS, progression-free survival; PLR, platelet-to-lymphocyte ratio; PS, performance status.
Table 5.
Multivariate Cox hazard analysis of factors associated with overall survival after the first- and second-line chemotherapies
| Factors | First-line chemotherapy
|
Second-line chemotherapy
|
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| ECOG PS | ||||||
| 0–1 vs 2–4 | 3.34 | 2.00–5.58 | <0.01 | – | – | – |
| Stage | ||||||
| I–III vs IV | 1.40 | 0.86–2.28 | 0.18 | – | – | – |
| Platelet-to-lymphocyte ratio | ||||||
| <150 vs ≥150 | 1.44 | 0.87–2.39 | 0.16 | 0.96 | 0.52–1.78 | 0.90 |
| Hemoglobin (g/dL) | ||||||
| ≥11 vs <11 | 1.43 | 0.72–2.82 | 0.31 | – | – | – |
| Serum sodium (mE q/L) | ||||||
| ≥135 vs <135 | 1.40 | 0.79–2.48 | 0.24 | 0.86 | 0.37–2.01 | 0.73 |
| LDH (IU/L) | ||||||
| <225 vs ≥225 | 1.63 | 0.99–2.68 | 0.052 | 1.62 | 0.89–2.94 | 0.12 |
| CRP (mg/dL) | ||||||
| <1 vs ≥1 | 1.47 | 0.85–2.55 | 0.17 | 2.67 | 1.30–5.47 | <0.01 |
| PFS after the first-line chemotherapy (months) | ||||||
| ≥6 vs <6 | – | – | – | 2.85 | 1.50–5.43 | <0.01 |
Notes: Coded as 1 (ECOG PS 2–4, stage IV, platelet-to-lymphocyte ratio ≥150, hemoglobin <11 g/dL, serum sodium <135 mEq/L, LDH ≥225 IU/L, CRP ≥1 mg/dL, and PFS after the first-line chemotherapy <6 months) and as 0 (ECOG PS 0–1, stages I–III, platelet-to-lymphocyte ratio <150, hemoglobin ≥11 g/dL, serum sodium ≥135 mEq/L, LDH <225 IU/L, CRP <1 mg/dL, and PFS after the first-line chemotherapy ≥6 months).
Abbreviations: CI, confidence interval; CRP, C-reactive protein; ECOG, European Clinical Oncology Group; HR, hazard ratio; LDH, lactate dehydrogenase; PFS, progression-free survival; PS, performance status.
Discussion
This longitudinal and observational study revealed the proportions of patients with SCLC who received the first-, second-, and third-line chemotherapies, the predictive factors influencing the introduction of chemotherapy, and survival rates from the first- and second-line chemotherapies.
The most important finding was that our study revealed a trajectory of chemotherapy for patients with SCLC. First, in our study, 81% of patients with all stages of SCLC and 77% of patients with metastatic SCLC received chemotherapy. These proportions were similar to those of some previous studies based on national databases. Regarding the extensive stage SCLC, 71% of patients from Taiwan (N=1,215),2 65% of patients from UK (N=9,874),23 and 67% of patients from the USA (N=643)24 received chemotherapy. Second, among the 81 patients who progressed and 13 patients who died after the first-line chemotherapy, 60 (64%) proceeded to the second-line chemotherapy. The rates of receipt of the second-line chemotherapy were different. Our proportion of patients who had received the second-line chemotherapy, 64%, was >30%, >32%, and >48% of patients in the single institutional studies from Greek university hospital,3 Canadian regional cancer center,25 and Japanese university hospital,15 respectively, but <88% of 49 patients with extensive stage SCLC who had received cisplatin plus irinotecan as the first-line chemotherapy at a Japanese regional cancer center.26 Third, among 59 patients who progressed and two patients who died after the second-line chemotherapy, 31 (51%) proceeded to the third-line chemotherapy. Based on our results, 25% (77%×64%×51%) of all patients with metastatic SCLC and 33% (64%×51%) of patients who underwent chemotherapy received the third-line chemotherapy. There were a few studies that had followed patients with SCLC until the third-line chemotherapy. Regarding the patients treated with chemotherapy, our proportion, 33%, was similar to 26% of 73 patients in a Japanese university hospital15 but slightly less than 18% of 191 patients in a Dutch university medical center27 and 22% of 120 patients in an international and multicenter study.28
The second important finding was that our study detected some prognostic factors at each treatment point. First, age and PS were independent factors predicting the receipt of chemotherapy. Our multivariate analysis revealed that patients with poorer ECOG PS and older age were unlikely to receive chemotherapy. A US study based on the national database showed that patients with older age, African American race, extensive stage disease, higher comorbidity score, and lower income were less likely to receive chemotherapy,29 while a recent US study detected only age ≥80 years and the presence of a residency program where patients were treated as factors associated with receiving any chemotherapy.24 A study from the UK also showed that older age, poorer PS, higher comorbidity index, and lower socioeconomic status potentially hinder receiving the chemotherapy.23 Age and PS may be the universally common factors for receiving chemotherapy, while other additional factors differ between studies and countries. Second, poorer PS and shorter PFS after the first-line chemotherapy and higher CRP level were independent prognostic factors for shorter OS after the first- and second-line chemotherapies, respectively. These factors detected in our study were similar to those in the previous studies. PS before the first-line chemotherapy,30,31 PS at the time of disease recurrence,3,32 and sensitivity to the first-line chemotherapy (sensitive/refractory)32,33 were well-known prognostic factors that influenced survival after the first- and second-line chemotherapies. Higher level of CRP was reported as an independent serum marker for the poorer prognosis of patients with newly diagnosed SCLC,34 while our study also detected higher CRP level as a poorer prognostic marker for the second-line chemotherapy. On the other hand, LDH,35 hyponatremia,16,17 and systemic inflammation-based scores, such as neutrophil-to-lymphocyte ratio36 and LMR,13 were reported to be prognostic markers of survival for chemonaive patients with extensive disease SCLC. Our univariate analysis detected PLR, LMR, hyponatremia, and LDH as prognostic factors of OS after the first- or second-line chemotherapy, but multivariate analysis did not detect them. Prognostic markers are desirable as they are easily measurable and available. Such markers would be useful when deciding further treatment for patients with SCLC.
Of note, the response rate and median PFS decreased from 73.7% and 161 days in the first-line chemotherapy and 32.3% and 103 days in the second-line chemotherapy to 12.9% and 63 days in the third-line chemotherapy. Our response rate and median OS of the third-line chemotherapy were lower and shorter than 44% and 5.1 months by amrubicine monotherapy in a Japanese regional medical support center,37 26% and 5 months in a Dutch university medical center,27 20% and 8.5 months in a Japanese university hospital,15 and 18% and 4.7 months in an international and multicenter study.28 Based on these retrospective and real-world analyses, we request at least a response rate of 20%–30% and survival of 5–6 months for the third-line regimen. There is neither any randomized trial comparing the third-line chemotherapy with the best supportive care alone nor evidence to guide the third-line chemotherapy. Thus, the benefits of treatment remain unknown. Our results were inferior in efficacy to those in the previous studies and also failed to support the third-line chemotherapy.
Our study includes the following two limitations: first, our study was single institutional, retrospective, and small sized. We are also afraid that our institutional bias may make it difficult to generalize the results of our study and that our small-sized study failed to detect any significant difference between groups and influential factors. Especially, our study included a very small number of patients with limited disease SCLC to evaluate those patients and detect stage as a significant prognostic factor. Second, we did not evaluate other promising prognostic markers of various nutrition-based indexes, because we did not routinely measure nutrition markers, such as serum albumin level.
Conclusion
Approximately two-thirds and one-third of patients who receive chemotherapy proceed to the second- and third-line chemotherapies, respectively. Evaluating several factors, such as age, ECOG PS, CRP level, and PFS, after previous treatment may be useful when considering the introduction of further-line chemotherapy.
Supplementary materials
Table S1.
Laboratory data at the start of the first-, second-, and third-line chemotherapies
| Variables | Mean ± SD
|
||
|---|---|---|---|
| First-line chemotherapy (N=118) |
Second-line chemotherapy (N=65) |
Third-line chemotherapy (N=31) |
|
| Leukocyte (cells/μL) | 7,535±2,743 | 6,448±2,088 | 6,319±2,457 |
| Neutrophil (cells/μL) | 5,174±2,505 | 4,211±1,875 | 4,348±1,690 |
| Lymphocyte (cells/μL) | 1,663±675 | 1,545±610 | 1,321±516 |
| Monocyte (cells/μL) | 487±213 | 500±176 | 487±195 |
| Hemoglobin (g/dL) | 12.9±1.9 | 12.0±2.0 | 11.5±1.9 |
| Platelet (×103 cells/μL) | 243±93 | 217±75 | 222±91 |
| Serum sodium (mEq/L) | 138.6±4.5 | 138.8±3.9 | 138.9±3.6 |
| Lactate dehydrogenase (IU/L) | 316±177 | 320±241 | 403±418 |
| Alkaline phosphatase (IU/L) | 305±216 | 288±336 | 277±147 |
| C-reactive protein (mg/dL) | 2.48±4.46 | 1.42±3.33 | 2.35±3.80 |
| Neutrophil-to-lymphocyte ratio | 3.83±3.21 | 3.27±2.17 | 5.80±14.16 |
| Platelet-to-lymphocyte ratio | 177.4±128.1 | 168.2±108.1 | 240.3±342.6 |
| Lymphocyte-to-monocyte ratio | 3.86±2.03 | 3.50±1.89 | 3.19±1.80 |
Abbreviation: SD, standard deviation
Table S2.
Regimens
| Regimens | First-line chemotherapy | Second-line chemotherapy | Third-line chemotherapy |
|---|---|---|---|
| N | 118 | 65 | 31 |
| Platinum-based doublet | |||
| CDDP + CPT-11 | 14 | 24 | 1 |
| CDDP + VP-16 | 18 | 2 | 0 |
| CBDCA + VP-16 | 84 | 8 | 3 |
| CBDCA + CPT-11 | 1 | 0 | 1 |
| Nonplatinum doublet | |||
| AMR + CPT-11 | 1 | 0 | 0 |
| Nonplatinum monotherapy | |||
| AMR | 0 | 29 | 19 |
| CPT-11 | 0 | 2 | 4 |
| NGT | 0 | 0 | 3 |
| Concurrent thoracic radiotherapy | 25a | 0 | 0 |
Note:
Including one palliative thoracic radiotherapy.
Abbreviations: AMR, amrubicine; CBDCA, carboplatin; CDDP, cisplatin; CPT-11, irinotecan; NGT, topotecan; VP-16, etoposide.
Table S3.
Treatment outcomes and response
| First-line chemotherapy | Second-line chemotherapy | Third-line chemotherapy | |
|---|---|---|---|
| N | 118 | 65 | 31 |
| Outcomes | |||
| Delivered courses (courses) | |||
| Mean ± standard deviation | 3.9±1.6 | 3.4±1.9 | 2.5±1.6 |
| Reasons of discontinuation (N) | |||
| Progressive disease | 31 | 41 | 18 |
| Completion of 4–6 courses | 54 | 13 | 2 |
| Adverse effects | 6 | 0 | 1 |
| Refused by patients | 9 | 3 | 3 |
| Cancer-related deteriorated condition | 2 | 3 | 5 |
| Comorbidity-related deteriorated condition | 14 | 5 | 2 |
| Ongoing | 2 | 0 | 0 |
| Response | |||
| CR (N) | 17 | 1 | 0 |
| PR (N) | 70 | 20 | 4 |
| SD (N) | 13 | 10 | 4 |
| PD (N) | 8 | 31 | 23 |
| NE (N) | 10 | 3 | 4 |
| ORR (%) | 73.7 | 32.3 | 12.9 |
| DCR (%) | 84.7 | 47.7 | 25.8 |
| PFS (days) | |||
| Median (95% CI) | 161 (140–181) | 103 (71–112) | 63 (39–82) |
Abbreviations: CI, confidence interval; CR, complete response; DCR, disease control rate; NE, not evaluated; ORR, overall response rate; PD, progressive disease; PFS, progression-free survival; PR, partial response; SD, stable disease.
Acknowledgments
The authors thank Moto Yaga, Kentaro Masuhiro, Yumi Mitsuyama, Son-Ho Kim, Sou Takada, Yuuki Hosono, and Narumi Noda at the Department of Respiratory Medicine, Osaka Police Hospital, for their clinical practice and management in diagnosis, treatment and care, and medical records for their patients.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hann CL, Rudin CM. Management of small-cell lung cancer: incremental changes but hope for the future. Oncology (Williston Park) 2008;22(13):1486–1492. [PMC free article] [PubMed] [Google Scholar]
- 2.Kuo YH, Lin ZZ, Yang YY, et al. Survival of patients with small cell lung carcinoma in Taiwan. Oncology. 2012;82(1):19–24. doi: 10.1159/000335084. [DOI] [PubMed] [Google Scholar]
- 3.Zarogoulidis K, Boutsikou E, Zarogoulidis P, et al. The role of second-line chemotherapy in small cell lung cancer: a retrospective analysis. Onco Targets Ther. 2013;6:1493–1500. doi: 10.2147/OTT.S52330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Brien ME, Ciuleanu TE, Tsekov H, et al. Phase III trial comparing supportive care alone with supportive care with oral topotecan in patients with relapsed small-cell lung cancer. J Clin Oncol. 2006;24(34):5441–5447. doi: 10.1200/JCO.2006.06.5821. [DOI] [PubMed] [Google Scholar]
- 5.von Pawel J, Jotte R, Spigel DR, et al. Randomized phase III trial of amrubicin versus topotecan as second-line treatment for patients with small-cell lung cancer. J Clin Oncol. 2014;32(35):4012–4019. doi: 10.1200/JCO.2013.54.5392. [DOI] [PubMed] [Google Scholar]
- 6.Travis WD, Brambilla E, Müller-Hermelink HK, et al. World Health Organization . Classification of Tumors Pathology and Genetics of Tumors of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2004. pp. 31–34. [Google Scholar]
- 7.National Cancer Institute, Cancer Therapy Evaluation Program [homepage on the Internet] Common Toxicity Criteria, Version 2.0. [Accessed March 12, 2016]. [published 1999 April 30]. Available from: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcv20_4-30-992.pdf.
- 8.Rami-Porta R, Crowley JJ, Goldstraw P. The revised TNM staging system for lung cancer. Ann Thorac Cardiovasc Surg. 2009;15(1):4–9. [PubMed] [Google Scholar]
- 9.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 10.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 11.Green RA, Humphrey E, Close H, Patno ME. Alkylating agents in bronchogenic carcinoma. Am J Med. 1969;46(4):516–525. doi: 10.1016/0002-9343(69)90071-0. [DOI] [PubMed] [Google Scholar]
- 12.Hong X, Cui B, Wang M, Yang Z, Wang L, Xu Q. Systemic Immune-inflammation Index, based on platelet counts and neutrophil-lymphocyte ratio, is useful for predicting prognosis in small cell lung cancer. Tohoku J Exp Med. 2015;236(4):297–304. doi: 10.1620/tjem.236.297. [DOI] [PubMed] [Google Scholar]
- 13.Go SI, Kim RB, Song HN, et al. Prognostic significance of the lymphocyte-to-monocyte ratio in patients with small cell lung cancer. Med Oncol. 2014;31(12):323. doi: 10.1007/s12032-014-0323-y. [DOI] [PubMed] [Google Scholar]
- 14.Holgersson G, Sandelin M, Hoye E, et al. Swedish lung cancer radiation study group: the prognostic value of anaemia, thrombocytosis and leukocytosis at time of diagnosis in patients with non-small cell lung cancer. Med Oncol. 2012;29(5):3176–3182. doi: 10.1007/s12032-012-0247-3. [DOI] [PubMed] [Google Scholar]
- 15.Inomata M, Hayashi R, Tokui K, et al. Outcome and prognostic factors in patients with small cell lung cancer who receive third-line chemotherapy. Tumori. 2014;100(5):507–511. doi: 10.1700/1660.18164. [DOI] [PubMed] [Google Scholar]
- 16.Tiseo M, Buti S, Boni L, Mattioni R, Ardizzoni A. Prognostic role of hyponatremia in 564 small cell lung cancer patients treated with topotecan. Lung Cancer. 2014;86(1):91–95. doi: 10.1016/j.lungcan.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 17.Hermes A, Waschki B, Reck M. Hyponatremia as prognostic factor in small cell lung cancer – a retrospective single institution analysis. Respir Med. 2012;106(6):900–904. doi: 10.1016/j.rmed.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 18.Christodolou C, Pavlidis N, Samantas E, et al. Prognostic factors in Greek patients with small cell lung cancer (SCLC). A Hellenic Cooperative Oncology Group study. Anticancer Res. 2002;22(6b):3749–3757. [PubMed] [Google Scholar]
- 19.Kawahara M, Fukuoka M, Saijo N, et al. Prognostic factors and prognostic staging system for small cell lung cancer. Jpn J Clin Oncol. 1997;27(3):158–165. doi: 10.1093/jjco/27.3.158. [DOI] [PubMed] [Google Scholar]
- 20.Jin Y, Sun Y, Shi X, Zhao J, Shi L, Yu X. Prognostic value of circulating C-reactive protein levels in patients with non-small cell lung cancer: a systematic review with meta-analysis. J Cancer Res Ther. 2014;10(suppl):C160–C166. doi: 10.4103/0973-1482.145854. [DOI] [PubMed] [Google Scholar]
- 21.Garassino MC, Torri V, Michetti G, et al. Outcomes of small-cell lung cancer patients treated with second-line chemotherapy: a multi-institutional retrospective analysis. Lung Cancer. 2011;72(3):378–383. doi: 10.1016/j.lungcan.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khakwani A, Rich AL, Tata LJ, et al. Small-cell lung cancer in England: trends in survival and chemotherapy using the National Lung Cancer Audit. PLoS One. 2014;9(2):e89426. doi: 10.1371/journal.pone.0089426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parsons HM, Harlan LC, Stevens JL, Ullmann CD. Treatment of small cell lung cancer in academic and community settings: factors associated with receiving standard therapy and survival. Cancer J. 2014;20(2):97–104. doi: 10.1097/PPO.0000000000000039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Froeschl S, Nicholas G, Gallant V, Laurie SA. Outcomes of second-line chemotherapy in patients with relapsed extensive small cell lung cancer. J Thorac Oncol. 2008;3(2):163–169. doi: 10.1097/JTO.0b013e318160c0cb. [DOI] [PubMed] [Google Scholar]
- 26.Imai H, Mori K, Wakuda K, et al. Progression-free survival, post-progression survival, and tumor response as surrogate markers for overall survival in patients with extensive small cell lung cancer. Ann Thorac Med. 2015;10(1):61–66. doi: 10.4103/1817-1737.146885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Jong WK, ten Hacken NH, Groen HJ. Third-line chemotherapy for small cell lung cancer. Lung Cancer. 2006;52(3):339–342. doi: 10.1016/j.lungcan.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Simos D, Sajjady G, Sergi M, et al. Third-line chemotherapy in small-cell lung cancer: an international analysis. Clin Lung Cancer. 2014;15(2):110–118. doi: 10.1016/j.cllc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Caprario LC, Kent DM, Strauss GM. Effects of chemotherapy on survival of elderly patients with small-cell lung cancer: analysis of the SEER-medicare database. J Thorac Oncol. 2013;8(10):1272–1281. doi: 10.1097/JTO.0b013e3182a007ba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arinc S, Gonlugur U, Devran O, et al. Prognostic factors in patients with small cell lung carcinoma. Med Oncol. 2010;27(2):237–241. doi: 10.1007/s12032-009-9198-8. [DOI] [PubMed] [Google Scholar]
- 31.Hong S, Cho BC, Choi HJ, et al. Prognostic factors in small cell lung cancer: a new prognostic index in Korean patients. Oncology. 2010;79(3–4):293–300. doi: 10.1159/000323333. [DOI] [PubMed] [Google Scholar]
- 32.Kim YH, Goto K, Yoh K, et al. Performance status and sensitivity to first-line chemotherapy are significant prognostic factors in patients with recurrent small cell lung cancer receiving second-line chemotherapy. Cancer. 2008;113(9):2518–2523. doi: 10.1002/cncr.23871. [DOI] [PubMed] [Google Scholar]
- 33.Owonikoko TK, Behera M, Chen Z, et al. A systematic analysis of efficacy of second-line chemotherapy in sensitive and refractory small-cell lung cancer. J Thorac Oncol. 2012;7(5):866–872. doi: 10.1097/JTO.0b013e31824c7f4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hong S, Kang YA, Cho BC, Kim DJ. Elevated serum C-reactive protein as a prognostic marker in small cell lung cancer. Yonsei Med J. 2012;53(1):111–117. doi: 10.3349/ymj.2012.53.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hermes A, Gatzemeier U, Waschki B, Reck M. Lactate dehydrogenase as prognostic factor in limited and extensive disease stage small cell lung cancer – a retrospective single institution analysis. Respir Med. 2010;104(12):1937–1942. doi: 10.1016/j.rmed.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 36.Kang MH, Go SI, Song HN, et al. The prognostic impact of the neutrophil-to-lymphocyte ratio in patients with small-cell lung cancer. Br J Cancer. 2014;111(3):452–460. doi: 10.1038/bjc.2014.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Asai N, Ohkuni Y, Matsunuma R, Nakashima K, Iwasaki T, Kaneko N. Efficacy and safety of amurubicin for the elderly patients with refractory relapsed small cell lung cancer as third-line chemotherapy. J Cancer Res Ther. 2012;8(2):266–271. doi: 10.4103/0973-1482.98983. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Laboratory data at the start of the first-, second-, and third-line chemotherapies
| Variables | Mean ± SD
|
||
|---|---|---|---|
| First-line chemotherapy (N=118) |
Second-line chemotherapy (N=65) |
Third-line chemotherapy (N=31) |
|
| Leukocyte (cells/μL) | 7,535±2,743 | 6,448±2,088 | 6,319±2,457 |
| Neutrophil (cells/μL) | 5,174±2,505 | 4,211±1,875 | 4,348±1,690 |
| Lymphocyte (cells/μL) | 1,663±675 | 1,545±610 | 1,321±516 |
| Monocyte (cells/μL) | 487±213 | 500±176 | 487±195 |
| Hemoglobin (g/dL) | 12.9±1.9 | 12.0±2.0 | 11.5±1.9 |
| Platelet (×103 cells/μL) | 243±93 | 217±75 | 222±91 |
| Serum sodium (mEq/L) | 138.6±4.5 | 138.8±3.9 | 138.9±3.6 |
| Lactate dehydrogenase (IU/L) | 316±177 | 320±241 | 403±418 |
| Alkaline phosphatase (IU/L) | 305±216 | 288±336 | 277±147 |
| C-reactive protein (mg/dL) | 2.48±4.46 | 1.42±3.33 | 2.35±3.80 |
| Neutrophil-to-lymphocyte ratio | 3.83±3.21 | 3.27±2.17 | 5.80±14.16 |
| Platelet-to-lymphocyte ratio | 177.4±128.1 | 168.2±108.1 | 240.3±342.6 |
| Lymphocyte-to-monocyte ratio | 3.86±2.03 | 3.50±1.89 | 3.19±1.80 |
Abbreviation: SD, standard deviation
Table S2.
Regimens
| Regimens | First-line chemotherapy | Second-line chemotherapy | Third-line chemotherapy |
|---|---|---|---|
| N | 118 | 65 | 31 |
| Platinum-based doublet | |||
| CDDP + CPT-11 | 14 | 24 | 1 |
| CDDP + VP-16 | 18 | 2 | 0 |
| CBDCA + VP-16 | 84 | 8 | 3 |
| CBDCA + CPT-11 | 1 | 0 | 1 |
| Nonplatinum doublet | |||
| AMR + CPT-11 | 1 | 0 | 0 |
| Nonplatinum monotherapy | |||
| AMR | 0 | 29 | 19 |
| CPT-11 | 0 | 2 | 4 |
| NGT | 0 | 0 | 3 |
| Concurrent thoracic radiotherapy | 25a | 0 | 0 |
Note:
Including one palliative thoracic radiotherapy.
Abbreviations: AMR, amrubicine; CBDCA, carboplatin; CDDP, cisplatin; CPT-11, irinotecan; NGT, topotecan; VP-16, etoposide.
Table S3.
Treatment outcomes and response
| First-line chemotherapy | Second-line chemotherapy | Third-line chemotherapy | |
|---|---|---|---|
| N | 118 | 65 | 31 |
| Outcomes | |||
| Delivered courses (courses) | |||
| Mean ± standard deviation | 3.9±1.6 | 3.4±1.9 | 2.5±1.6 |
| Reasons of discontinuation (N) | |||
| Progressive disease | 31 | 41 | 18 |
| Completion of 4–6 courses | 54 | 13 | 2 |
| Adverse effects | 6 | 0 | 1 |
| Refused by patients | 9 | 3 | 3 |
| Cancer-related deteriorated condition | 2 | 3 | 5 |
| Comorbidity-related deteriorated condition | 14 | 5 | 2 |
| Ongoing | 2 | 0 | 0 |
| Response | |||
| CR (N) | 17 | 1 | 0 |
| PR (N) | 70 | 20 | 4 |
| SD (N) | 13 | 10 | 4 |
| PD (N) | 8 | 31 | 23 |
| NE (N) | 10 | 3 | 4 |
| ORR (%) | 73.7 | 32.3 | 12.9 |
| DCR (%) | 84.7 | 47.7 | 25.8 |
| PFS (days) | |||
| Median (95% CI) | 161 (140–181) | 103 (71–112) | 63 (39–82) |
Abbreviations: CI, confidence interval; CR, complete response; DCR, disease control rate; NE, not evaluated; ORR, overall response rate; PD, progressive disease; PFS, progression-free survival; PR, partial response; SD, stable disease.