Summary
Background
In literature, there are lack of studies proposing clear and rationally designed test battery to be performed after an ACL reconstruction.
Methods
From 2006 to 2015, 80 football players were subjected, after ACL reconstruction, to a newly conceived test battery analyzing:
Isometric and isokinetic force production
The different phases during the jump
The correct control of the landing phase after jump
The control of valgus during landing after jump and cutting movements.
Results
The isokinetic and isometric test do not show any significant relationship with the another test. The laboratory test as well the field test showed them a significant correlation.
Conclusions
The results showed that a normal force production during the laboratory does not guarantee an equally satisfactory production of force during the field test.
Study design
Case series (Level III).
Keywords: ACL, arthroscopic reconstruction, football, functional evaluation, rehabilitation
Introduction
The anterior cruciate ligament (ACL) injury represents the most frequent ligament damage of the knee joint in athletes representing about 50% of all knee lesions1,2. The most part of the ACL injuries is caused by non-contact trauma, i.e during movements in which the ACL is submitted to an excessive mechanical stress3. In football, the incidence of ACL injuries in football is equal to 0.063 events per 1.000 hours of exposure time4. About 90% of patients with an ACL lesion undergo a reconstructive surgery and for many of them, the aspiration is to return at the same pre-injury sport sports level. Unfortunately, some studies show that the positive outcome is lower if compared to the expectations. Ardern et al.5 show that the return to sports (RTS) or return to play (RTP) 12 months after ACL reconstruction (ACLR) is within a fairly wide range, between 33% and 92%. This breadth range leaves many questions and doubts about the safety of reaching a positive outcome. In addition, other Authors report a relatively high risk, between 4 and 13%, concerning recurrence or secondary injury6–12.
The higher incidence of re-injuries has been recorded in the first two years after surgery8.
This data should make us reflect on three main factors that are listed below:
The adequacy of rehabilitation programs;
The need of longer recovery period before RTS and RTP for high-level athletes;
The inadequacy of the functional tests used in the decision-making for RTS and RTP.
The aim of this article is to propose a new functional test battery that is particularly able to provide elements for RTS and RTP decision making. As required our research was ethically conducted according to international standards13.
Material and methods
Subjects
During the period between 2006–2015, the functional tests battery described in this paper was administered to 80 men football players (whose age, height, and weight were respectively 24.43±6.05 years, 178.06±4.20 cm and 78.18±4.1 kg) after ACLR. All the subjects underwent arthroscopic reconstruction following ACL injury. The type of reconstruction and the sports activity level of the considered subjects are shown in Table I. All the subjects were informed about the aims of the research and the connected risks and all of them gave a written consensus.
Table I.
Type of reconstruction and sports activity performed by the considered subjects.
| Graft type | N° cases | Professional football players (%) | Amateur football players (%) |
|---|---|---|---|
| Patellar tendon | 45 | 15.6 | 84.4 |
| Hamstring | 35 | 91.4 | 8.6 |
|
| |||
| Total | 80 | ||
Protocol
During the rehabilitation period (165.93±16.73 days) all the subjects performed a battery of test consisting of 8 different trials i.e.:
Isometric yo-yo test (IYYT)
Isokinetic test (IT)
Synchro plates test (SPT)
Modified triple leg jumping test (MTLJT)
Modified side-step cutting test (MSSCT)
Sprint braking test (SBT)
Illinois agility test (IAT)
Modified Illinois Agility Test (IATm).
Isometric yo-yo test (IYYT)
During IYYT (Fig. 1), the subject performs an isometric push contemporary with both legs over a double synchronized force platform (Thesis System, Globus Italy. Reliability of the measure: 0.5 Kg; error device: <1%; sample rate 1000 Hz; sample depth 140 bit). During the push, the subject was bound to the Yo-Yo machine that offered a supramaximal resistance thereby making isometric push. The duration of the isometric push was 5′ and the knee angle during the push was standardized at 110°. During the push, the above mentioned synchronized force platforms simultaneously detected the strength signal for each leg. Three trials were performed and it was used in calculating the average. The data were normalized in relationship to the percentage of subject’s body weight (BW).
Figure 1.
During the IYYT the subject is bound to the equipment via the yo-yo cable which offers a supramaximal resistance making isometric the push movement. Two synchronized force platforms (Thesis System, Globus Italy. Reliability of the measure: 0.5 Kg; error of device: <1%; sample rate 1000 Hz; sample depth 140 bit) record the isometric strength value during the push performed by the subject.
Isokinetic test (IT)
The isokinetic protocol test adopted was structured as follows:
Quadriceps contraction performed at 60°/sec (QC 60°)
Hamstring positive contraction performed at 60° (HC 60°).
The data were normalized in relationship to the subject BW. The recorded data were compared with reference data coming from our database and are shown in Table II.
Table II.
Reference value considered during IT.
| Type of test | Reference value | Maximum % difference between injured and non-injured leg |
|---|---|---|
| QC 60° | 3.26 ± 0.47 (N.m−1 .kg−1) | 8.64 ± 9.1 |
| HC 60° | 1.75 ± 0.28 (N.m−1 .kg−1) | 5.12 ± 0.25 |
Synchro Plates Test (SPT)
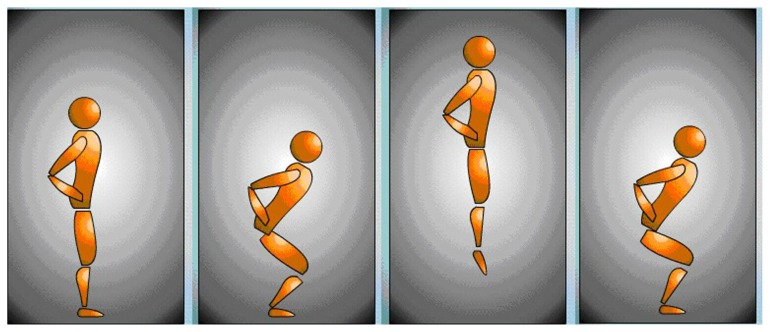
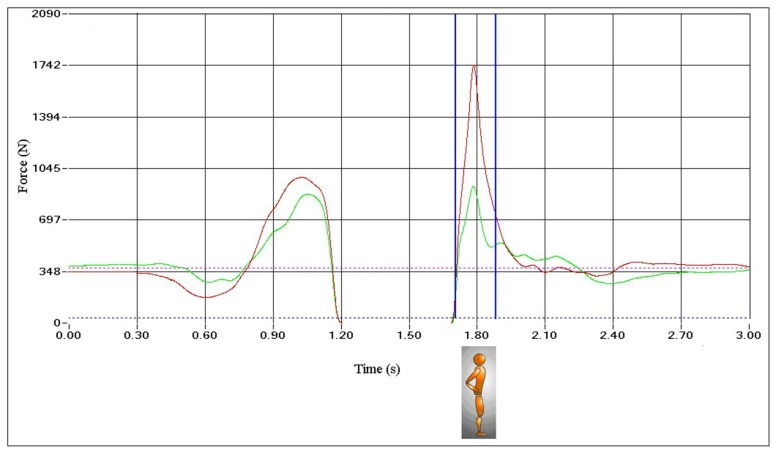
During SPT14 the subject is on a double synchronized force platform (Thesis System, Globus Italy. Reliability of the measure: 0.5 Kg; error of device: <1%; sample rate 1000 Hz; sample depth 140 bit) and performed a countermovement jump (CMJ) with 90° flexion knee angle. During the landing phase, the subject stopped the movement another time at 90° flexion knee angle (Fig. 2). The force platforms, after recording simultaneously the strength signal, automatically calculated and compared the two force signals recorded in four different phases, specifically:
Figure 2.
The SPT protocol provides that the subject performs a CMJ (90° knee flexion angle) and stops the landing phase with a knee angle another time equal to 90°. Two synchronized force platforms (Thesis System, Globus Italy. Reliability of the measure: 0.5 Kg; error of device: <1%; sample rate 1000 Hz; sample depth 140 bit) record the force signal during the jump movement.
- 1st phase or negative over-stretching phase
- 2nd phase or maximal negative strength phase
- 3rd phase or maximal positive strength phase
- 4th phase or landing phase.
During the above-listed four phases, corresponding to different muscular activation patterns, the following parameters were calculated:
The maximal negative acceleration value calculated during the stretching phase (MAneg recorded during the 1st phase)
The maximal negative force value (MFecc recorded during the 2nd phase)
The maximal positive force value (MFcon recorded during the 3rd phase)
The maximal landing force (or impact force) value (MFimp recorded during the 4th phase).
The biomechanical interpretation of the above parameters recorded during the different phases can be briefly summarized as follows:
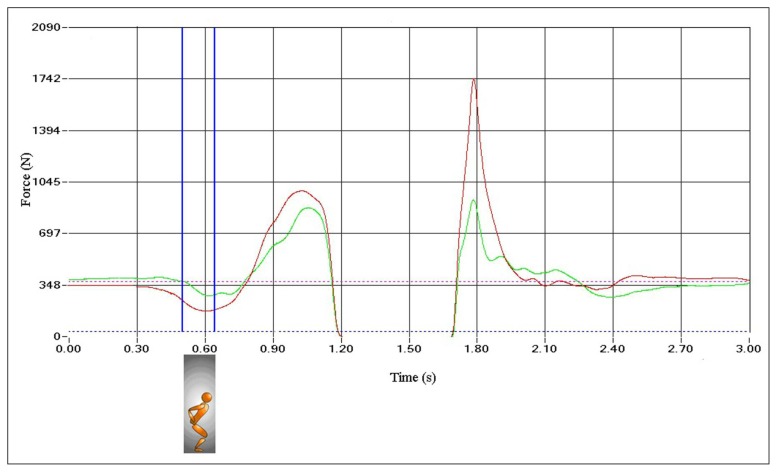
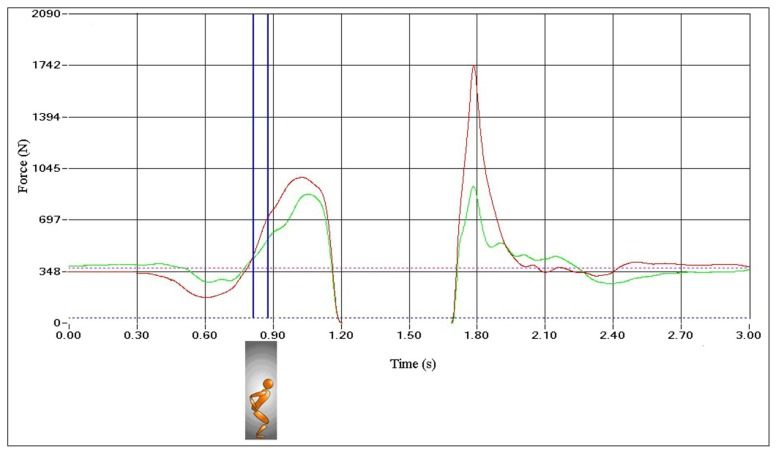
MAneg (Fig. 3) and MFecc (Fig. 4): those are specific parameters regarding the muscle extensor apparatus negative phase. The reference values must be less than (injured limb versus healthy limb) 15%14.
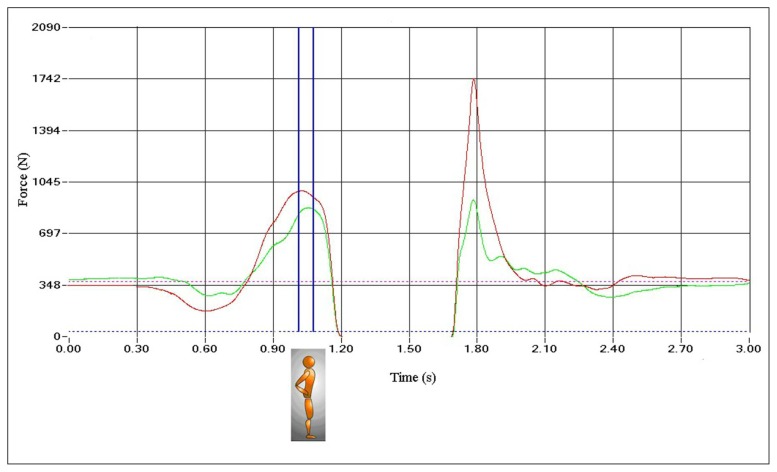
MFcon: during this phase, the elastic energy stored during the negative phase is transformed into mechanical work. The mechanical work generated from the stored elastic energy, enhance the force produced by the muscle contractile component during the positive phase. Therefore, the value recorded during this phase represents the extensor muscles elastic behavior. The reference values must be less than (injured limb versus healthy limb) 15%14 (Fig. 5).
MFimp: this value is recorded during the impact phase (i.e. the phase during which the subject lands over the force platform at the end of the fly phase) (Fig. 6). During this phase, it is evident the protective behavior for the safeguard of the injured limb. If the injured limb has not yet fully reached its functional and proprioceptive capacities, in this phase is present an important difference, in comparison to the uninjured limb, into the force signal recorded by the force platform15. The reference values must be less than (injured limb versus healthy limb) 10% 14.
Figure 3.
The negative acceleration peak (MAneg) represents the overstretching capabilities of the extensor muscles. (_ uninjured limb _ injured limb).
Figure 4.
The maximum force applied during the negative phase (MFecc) represents the maximum negative strength expressed by the extensor muscles immediately before the inversion of the movement (i.e immediately before the positive phase) (_ uninjured limb _ injured limb).
Figure 5.
The MFcon value represents the capacity of storage and reuse of elastic energy by the extensors muscle-tendon unit (_ uninjured limb _ injured limb).
Figure 6.
The maximum impact force value during the landing phase (MFimp) highlights the protective mechanisms used by the subject (_ uninjured limb _ injured limb).
For more details concerning the SPT protocol and the data interpretation, we refer the reader to consult the specific article14,15.
Modified triple leg jumping test (MTLJT) and modified sidestep cutting test (MSSCT)
The protocol for both tests provide first, a knee Q-angle static measurement, classically carried out by measuring the angle formed by a line joining the antero superior iliac spine (ASIS) and the patella center (i.e. the quadriceps vector force) and with a line joining the center of the patella with the anterior tibial tuberosity (i.e. the patella anatomical axis). After the Q-angle measurement, the operator places 3 markers over the subject’s lower limb, the first is placed on the line connecting the ASIS to the center of the patella, about 20 cm above the patella, the second at the center of the patella and the third at anterior tibial tuberosity level.
During the MTLJT test, the subject is asked to perform three monopodalic jumps on frontal plane (Fig. 7), first with his uninjured leg and then with the injured leg. During the test, a camera is placed perpendicularly to the subject, in order to avoid parallax errors, it records the entire sequence. A dedicated software measures the maximum value of the dynamic Q-angle during the contact with the ground.
Figure 7.
Dynamic Q-angle measurement during MTLJT.
During the MSSCT test (Fig. 8) the subject is asked, after a run of 5 meters, to touch a skittle 50 cm tall and then make a change of direction at 90° and run at maximum speed to a second skittle, situated 5 meters away. As in the previous test a camera is again placed perpendicularly to the first skittle that records the test. The same software used for the MTLJ measures the dynamic Q-angle maximum value during the change of direction carried out in correspondence of the first skittle. The dynamic Q-angle reference value for the injured limb during both the MTLJT and MSSCT must not exceed the 20% of the value of the static Q-angle previously measured.
Figure 8.
Dynamic Q-angle measurement during MSSCT.
Sprint Braking Test
The Sprint Braking Test (SBT)15 protocol provides a preliminary test consisting a maximal sprint for 30 meters. Once the sprint test is performed the subject is asked to make a sprint over the same distance at 90% of the maximum speed recorded during the preliminary test and to stop at the level of a skittle placed at a determined distance from the end of the sprint. The protocol provides for three tests, the first of which the stop-skittle is placed at 8 meters, and the second and the third respectively at 6 and 4 meters from the end of the sprint. The purpose of the SBT is to quantify in an objective manner the effectiveness of the contraction of the flexor muscles during the braking phase. In fact, during the arrest time, the subject must dissipate the kinetic energy (C) taken during the sprint by a certain value (dependent on his mass and the speed reached) to zero. Knowing the C value and the stopping distance (s) is possible to calculate the value of the negative power1 expressed by the subject during the braking phase.
It is, therefore, possible to calculate in indirect manner the effectiveness of the flexor muscles co-contraction through the following formula:
| (1) |
in which P is the negative power expressed in W, M is the subject’s mass, V is the average speed reached during the sprint and Tf is the braking time, the time taken to reach V0 (zero speed, the full stop).
| (2) |
in which s is the braking and a the acceleration, and knowing that the a value is equal to: V2 /2.s (3) in which V2 is the square of the speed reached by the athlete during the sprint.
Replacing the a value derived from (3) to (2) and replacing to (1) the Tf value derived from (2), it is possible to calculate the P value, i.e. the negative power expressed during the contraction of the flexor muscles into the braked phase. An electronic spreadsheet specifically conceived, allowed the calculation. The reference minimum value to reach into the test was fixed in 20 W/kg−1.
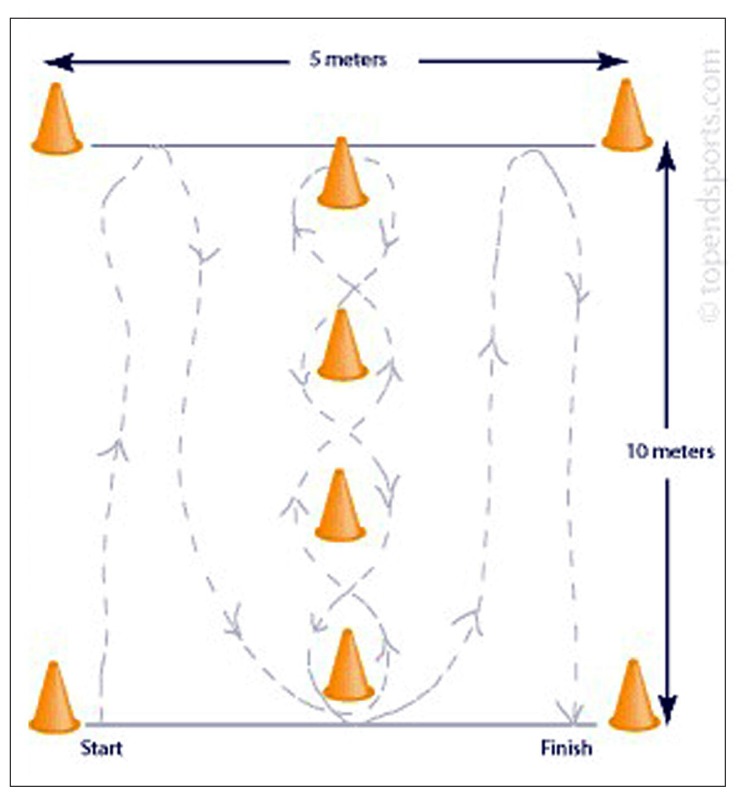
Illinois Agility test (IAT) and modified Illinois Agility Test (IATm)
In the Illinois Agility Test (IAT)16, 17 the subject must perform at maximum speed the entire path according to the scheme shown in Figure 9. The start is freely determined by the athlete. The chronometric result represents the final score of the test (Tab. III). The modified Illinois Agility Test (IATm)18 provides the same protocol of IAT but performed with the ball. Also, in this case, the start is freely determined by the athlete and the chronometric result represents the final score of the test (Tab. IV).
Figure 9.
IAT and IATm scheme. The test length – i.e the distance between the start point and the stop point – is, in both cases, 10 meters, while the width of the test area is 5 meters.
Table III.
IAT reference values.
| Rating | Lap result (sec) |
|---|---|
| Excellent | < 15.2 |
| Good | 16.1-15.2 |
| Medium | 18.1-16.2 |
| Insufficient | 18.3-18.2 |
| Very insufficient | > 18.3 |
Table IV.
IATm reference values.
| Rating | Lap result (sec) |
|---|---|
| Excellent | < 16.2 |
| Good | 17.1-16.2 |
| Medium | 19.1-17.2 |
| Insufficient | 19.3-19.2 |
| Very insufficient | > 19.3 |
The timing of administration of the battery of functional evaluation
The progression of the battery is supported by a rational application mainly based on a proper balance between the need to monitor the progress of the patient and the need to safeguard the biological integrity of the neo-ligament.
The results of functional tests performed will define the entire rehabilitation process towards a “goal- target protocol”. In Table V the various tests mentioned above are presented in their temporal sequence of administration depending upon the rehabilitation period.
Table V.
The various tests above placed in a logical temporal sequence of execution depending on the rehabilitation period. The sig (+) indicates the period in which the execution of the test is advisable. In the last column it is indicated the period during which the test was performed in the considered series.
| Type of test | 60 days | 90 days | 120 days | 150 days | 180 days | Period in which the test was performed |
|---|---|---|---|---|---|---|
| IYYT | + | + | + | 90.7±17.1 days post-surgery | ||
| IT | + | + | + | 168.6±12.2 days post-sugery | ||
| SPT | + | + | 163.6±8.2 days post-surgery | |||
| MSSCT | + | + | 168.6±6.3 days post-surgery | |||
| MTLJT | + | 181.5±7.2 days post-surgery | ||||
| SBT | + | + | 165.3±11.8 days post-surgery | |||
| IAT | + | + | 170.6±9.8 days post-surgery | |||
| IATm | + | + | 169.6±8.5 days post-surgery |
Statistics
The homogeneity of the sample regarding age and anthropometric values was tested by a non-parametric Kolmogorov-Smirnov test. The force value recorded during IT and SPT as well as the power recorded during SPT was standardized on the basis of subjects BW. The relationship between all recorded value was calculated by a Spearman’s rank correlation coefficient. Statistical significance was set at p<0.05.
Results
IYYT recorded value in the injured limb was 46.32 ±7.09 of the BW.
IT recorded value in the injured limb were 2.36 ± 0.51 and 1.15± 0.31 N.m−1 .kg−1 respectively, for QC 60° and HC 60° test.
SPT recorded values in the injured limb were 3.52 ± 2.12 m.s−2 for MAneg test; 97.81 ± 15.13% BW for MFecc test; 124.10 ± 13.20% BW for MFcon test and 213.12 ± 42.3 % BW for MFimp.
The dynamic Q-angle value measured during MTLJT was 16.21 ± 2.31% greater than the static Q-angle value previously measured.
The dynamic Q-angle value measured during MSSCT was 17.11 ± 1.98% greater than the static Q-angle value previously measured.
SBT recorded values was 22.51±2.31 W.kg−1.
The IAT recorded value was 17.11 ± 1.62 sec.
The IATm recorded value was 18.91 ± 2.03 sec.
The statistic significance of the relationship of the considered values are shown in Table VI.
Table VI.
Correlation matrix of the considered value.
| IYYT | QC | HC | MAneg | MFecc | MFcon | MFimp | MSSCT | MTLJT | SBT | IAT | IATm | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IYYT | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | |
| QC | n.s | * | * | * | * | * | n.s | n.s | n.s | n.s | n.s | |
| HC | n.s | * | * | * | * | * | n.s | n.s | n.s | n.s | n.s | |
| MAneg | n.s | * | * | ** | * | * | n.s | n.s | n.s | n.s | n.s | |
| MFecc | n.s | * | * | ** | * | * | n.s | n.s | n.s | n.s | n.s | |
| MFcon | n.s | * | * | * | * | * | n.s | n.s | n.s | n.s | n.s | |
| MFimp | n.s | * | * | * | * | * | n.s | n.s | n.s | n.s | n.s | |
| MSSCT | n.s | n.s | n.s | n.s | n.s | n.s | n.s | * | n.s | n.s | n.s | |
| MTLJT | n.s | n.s | n.s | n.s | n.s | n.s | n.s | * | n.s | n.s | n.s | |
| SBT | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | * | * | |
| IAT | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | * | * | ||
| IATm | n.s | n.s | n.s | n.s | n.s | n.s | n.s | n.s | * | * |
Legend.
n.s: not significant;
p<0.005;
p<0.001.
Notes: MAneg, MFecc, MFcon, and MFimp are the parameters recorded during SPT.
QC and HC are the parameters recorded during IT.
Discussion
Many studies noted a change in the movements neuromuscular pattern at the injured limb level compared to the contralateral in male and female subjects underwent ACLR19–21.
The alteration of the pattern movement is particularly evident during the execution of movements such as the monopodalic jump (single leg jumping), jumping with both feet in the sagittal plane (sagittal double leg jumping), lateral jumps, changes of direction (sidestep cutting) and run19,22–24. This alteration would remain for a period of time between 6 and 24 months, even in the case where the athlete has fully resumed the sporting activity19. The most significant changes are an increase in the valgus dynamic especially in landing phase after jump, an asymmetry of the two lower limbs in the initial moment of contact with the ground, instability in monopodalic movements, and a rotation of the hips in the opposite direction of the injured limb25.
It is important to point out that the mechanical stress of the ACL increases dramatically in the condition of valgus, especially if this situation is associated with internal rotation, while the valgus associated with external rotation, even if presupposes less mechanical stress, creates the condition for impingement of the ACL26.
The force vector generated by the contraction of the quadriceps muscle, if not properly counterbalanced by the carrier generated in the opposite direction from the contraction of the flexor muscles of the thigh, can cause an anterior sliding of the tibia that can damage the anatomical integrity of the neo-ligament27. In other words, the action of co-contraction of the flexor muscles is essential for the protection of neo-ligament in order to counteract excessive forces tending to produce anterior tibial sliding by the extensor musculature28. For all these reasons, it is clear the need to dispose of a battery of tests able to detect the impairment and the progress of a rehabilitation program29.
For this reason, we propose a battery of tests analyzing:
A correct force production in isometric condition by the extensor muscles of the lower limbs and by the hip extensors muscles by of the injured and healthy limb during the early phase of rehabilitation plan (YYT)
A correct force production during isokinetic condition in a more advanced phase of rehabilitation plan (IT)
The correct activation of the extensor, flexor muscles and the correct control of the landing phase during bipodalic ballistic movement (SPT)
The correct control of dynamic valgus (MTLJT and MSSCT)
The effectiveness of the contraction of flexor muscle during a braking movement into the control of the anterior tibial shift (SBT)
The correct control of valgus and anterior tibial shift during cutting movement performed at high run speed without and with ball (IAT and IATm).
Each type of tests will be inserted within a time sequence of the administration taking into account the biological times of integration of the neo-ligament. Although it must be remembered that the studies in the literature about the so-called process of ligamentization are, to date, rather far from reaching a consensus about it30–32.
It is important to emphasize that this sequence of tests is based on the principle of “goal-target protocol”. In other words, the various steps of the rehabilitation plan are rather based on the achievement of a well-defined functional outcome rather than on the principle of “time-frame protocol”.
The loss of correlation between YYT and the other strength laboratory test (IT and SPT) may explain the difference of the activation pattern between isometric contraction and positive work contraction33. In any case, YYK allows the advantage to be able to test the subject into the early phase of the rehabilitation (starting from 60 days). Furthermore, this test is performed in the closed kinetic chain and therefore the mechanical stress at neo-ligament level is minimal. Indeed, in the literature, there is still present a controversy concerning the early introduction of exercises and test in open kinetic chain as part of rehabilitation after ACLR34–36.
The correlation that the different parameters recorded during SPT (i.e. MAecc, MFecc, MFconc and MFimp) shows that the jump movement patterns of activation are strongly interconnected. Therefore, a deficiency of one of these parameters may compromise the entire motion pattern15,37. Furthermore, the correlation between the parameters recorded during IT (i.e. QC and HC) and the different parameters recorded during SPT (i.e. MAecc, MFecc, MFconc and MFimp) show the influence of isokinetic force and the explosive force applied during a ballistic movement38.
The correlation between MSSCT and MTLJT shows how the movement control of dynamic valgus during the landing phase after a jump (MSSCT) and during a cutting movement (MTLJT) are strongly interrelated.
The correlation between SBT, IAT and IATm show the specificity of this test for the assessment of the control of tibial anterior shift during a run in which is required an important deceleration phase. Indeed, during the deceleration phase, the hamstring contraction is essential into the control of tibial anterior shift and, therefore, for the neo-ligament protection18,28.
Finally, the loss of correlation between the so-called laboratory tests (IYYT, IT and SPT) and field tests (MSSCT, MTLJT, SBT, IAT and IATm) shows how the force production patterns are highly “velocity-dependent” 39,40. In other words, a satisfactory force production during the laboratory tests does not guarantee an equally satisfactory production of force during the field test.
Conclusions
It is important to underline that, concerning ACLR, the most important variable is represented by the validity of the surgical technique performed and by the accuracy with which the latter is made. In addition, we think that an essential part of the positive outcome after surgery is a proper rehabilitation process and an equally suitable strategy of functional assessment, based on a solid scientific rationale. The rehabilitation following ACLR should not be trivialized, and it is a milestone for a full recovery both from an anatomical and functional point of view.
It is noted that the rehabilitation process can be considered, in fact, finished with anatomical healing for sedentary patients, but this is not true for sports subjects. Indeed, in sports, subjects is essential to the resumption of full functionality, this aspect is as much important as higher is the performance level of the subject.
The battery of functional tests described in this study is certainly an ambitious and innovative proposal, an alternative to those normally used. This requires the use of highly specific structures, materials and technical skills which represent, in our opinion, the discriminating variables between the mainstream and excellence rehabilitation programs.
Footnotes
The definition of “negative” power is justified by the fact that represents a power used to decelerate a mass and not to accelerate as in case of “positive” power.
References
- 1.Risberg MA, Lewek M, Synder-Mackler L. A systematic review of evidence for anterior cruciate ligament rehabilitation: how much and what type? Phys Ther in Sport. 2004;5(3):125–145. [Google Scholar]
- 2.Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810–817. doi: 10.4085/1062-6050-48.6.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Velázquez-Rueda ML, Martínez-Ávila JP, Pérez-Serna AG, Gómez-García F. Risk factors and frequency in re-ruptures of the anterior cruciate ligament in adults. Acta Ortop Mex. 2016;30(2):61–66. [PubMed] [Google Scholar]
- 4.Bjordal JM1, Arnły F, Hannestad B, Strand T. Epidemiology of anterior cruciate ligament injuries in soccer. Am J Sports Med. 1997;25(3):341–345. doi: 10.1177/036354659702500312. [DOI] [PubMed] [Google Scholar]
- 5.Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549–1558. doi: 10.1177/0363546513489284. [DOI] [PubMed] [Google Scholar]
- 6.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 7.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–567. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 8.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 9.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 10.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41(1):203–215. doi: 10.1177/0363546512460637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42(7):1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal - Basic principles and recommendations in clinical and field Science Research: 2016 Update. MLTJ. 2016;6(1):1–5. doi: 10.11138/mltj/2016.6.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bisciotti GN. La validazione di una nuova batteria di test per la quantificazione dello squilibrio muscolare: il Tesys Globus Evaluation System. New Athletic Research in Science Sport. 2006;198:5–15. [Google Scholar]
- 15.Bisciotti GN, Sannicandro I, Manno R. Cambiamenti nel pattern di attivazione muscolare balistico a seguito di due diverse tecniche ricostruttive di legamento crociato anteriore del ginocchio. Med Sport. 2011;64(2):185–200. [Google Scholar]
- 16.Lockie RG, Schultz AB, Callaghan SJ, Jeffriess MD, Berry SP. Reliability and Validity of a New Test of Change-of-Direction Speed for Field-Based Sports: the Change-of-Direction and Acceleration Test (CODAT) J Sports Sci Med. 2013;12(1):88–96. [PMC free article] [PubMed] [Google Scholar]
- 17.Hachana Y, Chaabène H, Ben Rajeb G, et al. Validity and reliability of new agility test among elite and subelite under 14-soccer players. PLoS One. 2014;9(4):e95773. doi: 10.1371/journal.pone.0095773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bisciotti GN. Return to play after muscle lesion. In: Volpi, editor. Football Traumatology. New Springer International Publishing; Switzerland: 2015. [Google Scholar]
- 19.McLean SG, Myers PT, Neal RJ, Walters MR. A quantitative analysis of knee joint kinematics during the sidestep cutting maneuver. Implications for non-contact anterior cruciate ligament injury. Bull Hosp Jt Dis. 1998;57(1):30–38. [PubMed] [Google Scholar]
- 20.Powers CM, Fisher B. Mechanisms underlying ACL injury-prevention training: the brain-behavior relationship. J Athl Train. 2010;45(5):513–515. doi: 10.4085/1062-6050-45.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peterson JR, Peterson ED. Anterior cruciate ligament injury in the athlete-an update in prevention strategies. S D Med. 2012;65(11):421–425. [PubMed] [Google Scholar]
- 22.McLean SG. The ACL injury enigma: we can’t prevent what we don’t understand. J Athl Train. 2008;43(5):538–540. doi: 10.4085/1062-6050-43.5.538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chappell JD, Yu B, Kirkendall DT, Garrett WE. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30(2):261–267. doi: 10.1177/03635465020300021901. [DOI] [PubMed] [Google Scholar]
- 24.McLean SG, Neal RJ, Myers PT, Walters MR. Knee joint kinematics during the sidestep cutting maneuver: potential for injury in women. Med Sci Sports Exerc. 1999;31(7):959–968. doi: 10.1097/00005768-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Sigward SM, Powers CM. Loading characteristics of females exhibiting excessive valgus moments during cutting. Clin Biomech (Bristol, Avon) 2007;22(7):827–833. doi: 10.1016/j.clinbiomech.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Mariani PP, Cerullo G, Iannella G, Giacobbe M. Arthroscopic and sport injuries: Application in high-level atlete. Springer International Publishing; Switzerland: 2016. Anterior cruciate ligament; pp. 339–346. [Google Scholar]
- 27.Pollard CD, Sigward SM, Powers CM. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech (Bristol, Avon) 2010;25(2):142–146. doi: 10.1016/j.clinbiomech.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silvers HJ, Mandelbaum BR. Prevention of anterior cruciate ligament injury in the female athlete. Br J Sports Med. 2007;41(Suppl 1):152–159. doi: 10.1136/bjsm.2007.037200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foti C, Laurin A, Tiberti S, et al. Leg extension test, sEMG and vibratory stimuli to assess functional recovery following knee joint surgery. Muscles Ligaments Tendons J. 2012;2(2):127–132. [PMC free article] [PubMed] [Google Scholar]
- 30.Muller B, Bowman KF, Jr, Bedi A. ACL graft healing and biologics. Clin Sports Med. 2013;32(1):93–109. doi: 10.1016/j.csm.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 31.Pauzenberger L, Syré S, Schurz M. “Ligamentization“ in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29(10):1712–1721. doi: 10.1016/j.arthro.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 32.Dong S, Xie G, Zhang Y, Shen P, Huangfu X, Zhao J. Ligamentization of Autogenous Hamstring Grafts After Anterior Cruciate Ligament Reconstruction: Midterm Versus Long-term Results. Am J Sports Med. 2015;43(8):1908–1917. doi: 10.1177/0363546515584039. [DOI] [PubMed] [Google Scholar]
- 33.Bosco C, Komi PV, Tihanyi J, Fekete G, Apor P. Mechanical power test and fiber composition of human leg extensor muscles. Eur J Appl Physiol Occup Physiol. 1983;51(1):129–135. doi: 10.1007/BF00952545. [DOI] [PubMed] [Google Scholar]
- 34.Heijne A, Werner S. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):402–414. doi: 10.1007/s00167-006-0246-z. [DOI] [PubMed] [Google Scholar]
- 35.Fukuda TY, Fingerhut D, Moreira VC, et al. Open kinetic chain exercises in a restricted range of motion after anterior cruciate ligament reconstruction: a randomized controlled clinical trial. Am J Sports Med. 2013;41(4):788–794. doi: 10.1177/0363546513476482. [DOI] [PubMed] [Google Scholar]
- 36.Uçar M, Koca I, Eroglu M, et al. Evaluation of open and closed kinetic chain exercises in rehabilitation following anterior cruciate ligament reconstruction. J Phys Ther Sci. 2014;26(12):1875–1878. doi: 10.1589/jpts.26.1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bosco C, Komi PV, Ito A. Prestretch potentiation of human skeletal muscle during ballistic movement. Acta Physiol Scand. 1981;111(2):135–140. doi: 10.1111/j.1748-1716.1981.tb06716.x. [DOI] [PubMed] [Google Scholar]
- 38.Jacopetti M, Pasquini A, Costantino C. Evaluation of strength muscle recovery with isokinetic, squat jump and stiffness tests in athletes with ACL reconstruction: a case control study. Acta Biomed. 2016;87(1):76–80. [PubMed] [Google Scholar]
- 39.Bobbert MF. Why is the force-velocity relationship in leg press tasks quasi-linear rather than hyperbolic? J Appl Physiol. 2012;112(12):1975–1983. doi: 10.1152/japplphysiol.00787.2011. [DOI] [PubMed] [Google Scholar]
- 40.Cuk I, Markovic M, Nedeljkovic A, Ugarkovic D, Kukolj M, Jaric S. Force-velocity relationship of leg extensors obtained from loaded and unloaded vertical jumps. Eur J Appl Physiol. 2014;114(8):1703–1714. doi: 10.1007/s00421-014-2901-2. [DOI] [PMC free article] [PubMed] [Google Scholar]