Abstract
Background
Inhaled therapies are the cornerstone of pharmacologic management for COPD. Each device requires a unique series of steps to be most effective, making appropriate instruction in inhaler technique a key part of the management of COPD.
Objectives
Examine characteristics of patients and devices associated with poor technique among patients with COPD.
Methods
Cross-sectional study of subjects with COPD using at least one of: metered dose inhaler, Advair Diskus, Spiriva Handihaler, identified from the COPD Outcomes-based Network for Clinical Effectiveness and Research Translation (CONCERT) registry. Technique was assessed face-to-face using manufacturer-provided dummy inhalers, with standardized checklists for each device. We used logistic regression to model associations with poor inhaler technique, defined as an error in ≥20% of the steps, as a function of patient characteristics, with educational attainment the primary predictor.
Results
688 individuals meet eligibility criteria, 65.5% had poor technique for at least one device. In adjusted analyses, Black race was associated with poor technique (OR 3.25, 95%CI 1.86-5.67) while greater than high school education was associated with decreased odds of poor technique (OR 0.35, 95%CI 0.17-0.70 for trade school/some college, OR 0.25, 95%CI 0.11-0.61 for college or more, p≤0.001 for test of linear trend). The percentage of errors varied between devices, with subjects making proportionally the most errors for MDIs.
Conclusions
Poor inhaler technique is common among individuals with COPD, varies between devices, and is associated with race and educational attainment. Tailored educational interventions to teach inhaler should be part of the process of initiating and monitoring inhaled therapies.
Keywords: chronic obstructive pulmonary disease (COPD), inhaled therapy, technique, adherence
Background
Pharmacologic therapy is centrally important to the management of chronic obstructive pulmonary disease (COPD), and is one of the most important interventions after smoking cessation. Inhaled therapies represent the cornerstone of management, and the correct use of inhaled therapies has been linked to improved outcomes for respiratory diseases.[1, 2] Unlike oral medications, inhalers can be difficult for a patient to use correctly.[3] Each type of inhaler requires a unique series of steps to be effective,[4, 5] with significant variation between inhaler subtypes.[6] This can be a barrier for patients using multiple inhalers, as there can be contradictory techniques needed to obtain maximum medication between devices.[7] For example, metered dose inhalers (MDIs) require a long slow inhalation for maximum efficacy, whereas dry powder inhalers such as the Advair Diskus require a rapid inhalation, and the Spiriva Handihaler requires a breath just rapid enough to “vibrate” the capsule.[8, 9] MDIs need to be shaken before use, but shaking or tipping the Advair Diskus may result in loss of the medication. Unfortunately, many patients are not optimally adherent to inhaled therapies, missing doses or not using medications as directed,[10] with some studies finding rates of misuse as high as 80%.[11-13] Assuring correct inhaler technique is therefore an important aspect of the management of these patients.
Patients with COPD may face unique barriers to the use of inhaled medications.[14] Most are diagnosed later in life[15] and are disproportionately of lower socioeconomic status,[16] which may have important implications for health literacy and learning new techniques. Therefore, patients with COPD should be assessed for their individualized risks related to disease management, which includes assessment of appropriate inhaler technique. Individuals with low health literacy have worse COPD outcomes,[17] and poor inhaler technique may be a contributing factor. Though the use of inhaled therapies is a key area of management for patients with COPD, most previous studies have been small,[18-20] primarily focused on patients with asthma, or hospital-based,[1, 12, 21-23] with small numbers of outpatients with COPD. Many of these studies have taken place outside the United States,[1, 21, 23, 24] limiting the generalizability to a US population which has a different distribution of race, educational attainment, and level of literacy.
The goal of this study was to assess patient factors associated with poor inhaler technique for several common devices used by subjects with COPD, and to examine differences in errors made between devices. Based on prior evidence in asthma patients, we hypothesized that patients with lower educational attainment and health literacy would have worse inhaler technique, while patients with higher disease severity and more healthcare contact would have better inhaler technique.
Materials and Methods
Design, setting, participants, data source
We conducted a cross-sectional study of patients identified as having probable COPD. The complete methods for the identification of the study population have previously been published.[25] Briefly, subjects were selected from the COPD Outcomes-based Network for Clinical Effectiveness and Research Translation (CONCERT) DataHub,[26] which comprises over 220,000 patients aged ≥40 identified administratively from 2006-2010, drawn from 7 sites representing academic, private, and integrated healthcare organizations. We invited a subset of participants complete an in-person study visit and provide written informed consent (VA Puget Sound IRB #00207).[25] Subjects performed post-bronchodilator spirometry and standardized questionnaires to collect demographics, health history, symptoms, and measures of dyspnea. 1,206 patients completed the testing.
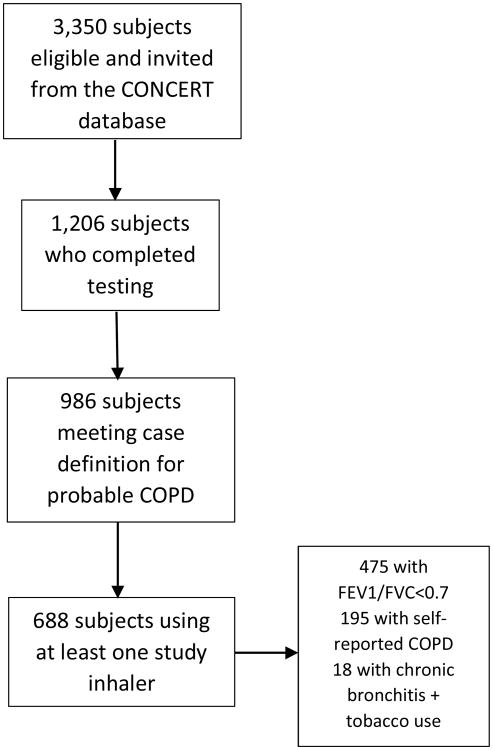
We limited our analysis to those patients who were taking at least one of the evaluated inhalers and who met one of the following criteria: 1) patient report of a diagnosis of COPD, chronic bronchitis and/or emphysema 2) post-bronchodilator FEV1/FVC ratio less than <0.70 on pulmonary function testing 3) symptoms of chronic bronchitis + a history of smoking. Symptomatic smokers (n=18) were included due to recent studies indicating that these individuals often use inhalers and suffer respiratory exacerbations at rates similar to those with mild to moderate COPD.[27] (Figure 1)
Figure 1. Results of cohort selection.
Predictors
Our primary predictor was education, assessed by both educational attainment and health literacy. Health literacy was evaluated using the Rapid Assessment of Adult Literacy in Medicine-Short Form (REALM-SF), a validated tool for quantifying health literacy, normalized to grade level.[28] We also examined additional demographic and behavioral factors, count of inhaler devices used, and markers of COPD severity and healthcare contact. These included: GOLD stage, COPD exacerbation in the past 3 months, hospitalization in the past 3 months, and dyspnea as measured by the modified Medical Research Council (mMRC) dyspnea scale.[29] Count of different inhaler types used was determined as follows: metered dose inhaler (MDI) used (includes Alvesco, Albuterol, Symbicort, Atrovent, Combivent, and Dulera) plus number of additional unique inhalers used (Asmanex, Foradil, Pulmicort, Spiriva Handihaler, Advair Diskus, and “other” inhaler not listed individually).
Outcome
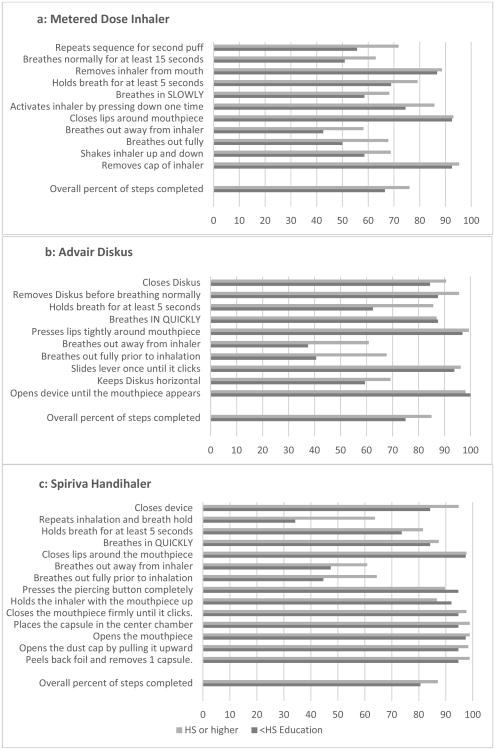
Inhaler technique was assessed using dummy inhalers provided by each manufacturer, with direct observation by trained study personnel using standardized checklists (steps outlined in figure 2). Standardized checklists were based on recommendations from the manufacturer. Previous studies have found excellent inter-rater reliability when using similar checklists.[30] Inhalers with few (<50) users were excluded, leaving MDIs, Spiriva Handihaler, and Advair Diskus in the analysis. The step “ejection of the capsule” was excluded from the analysis for Spiriva as it does not directly affect the dose received of the medication. Our primary outcome was poor inhaler technique, defined as the odds of making an error in 20% or more of the steps (≥2/11 steps for MDIs, ≥2/10 steps for Diskus, ≥3/14 steps for Spiriva) for 1) any inhaler used by an individual patient and 2) each individual inhaler. The 20% error cutoff was selected both as being similar to other studies of inhaler technique [24, 31] and more likely to be clinically relevant. Given the variability in steps between devices, as well as the fact that some steps are critical to receiving medication (ex: removing the cap), we were interested in whether individual steps or devices were particularly prone to error.
Figure 2. Percentage of patients with COPD correctly completing each step and overall proportion of steps for individual inhalers, by educational attainment. HS=High School.
Therefore, we performed additional analyses examining the association of educational attainment with each step performed.
Statistical Analysis
We used Stata 14 (College Station, TX) software for all analyses. We used chi-squared tests and t-tests to assess unadjusted associations, and logistic regression modelling to build our final models. Each predictor was assessed individually for an association with poor inhaler technique. Those variables attaining p≤0.1 in preliminary models for any individual inhaler were included in the final models. In the case of significant colinearity (Pearson's correlation coefficient ≥0.4), only one variable was retained in the final model. REALM-SF and education were highly collinear (coefficient 0.41), and therefore REALM-SF was excluded. Educational attainment was modeled as a dummy variable and with a test of linear trend. Age, sex, and income were included as confounders based on prior studies.[13, 18, 21, 30] Odds ratios were calculated using clustered estimates of variance by site. An α≤0.05 was considered significant. Examining the association between education and each individual step performed, we used a linear regression model adjusted for a priori determined predictors: age, sex, race, income, and count of inhalers, with clustered standard errors by site.
Results
688 subjects met the entry criteria and were taking at least 1 inhaler. (Figure 1). Subjects were predominantly white (70.0%), between 40 and 75 years old, and were equally split by gender, with 32% active smokers. The majority (69%) demonstrated fixed airflow obstruction. The majority of subjects had poor inhaler technique for at least one device used (65.5%). Subjects with poor technique for one or more device were more likely to be female, Black, current smokers, and have lower education and health literacy. (Table 1)
Table 1.
Characteristics of study subjects overall, and among subjects with and without poor inhaler technique for at least one tested device.
| Poor Technique | ||||
|---|---|---|---|---|
| Overall (N=688) | No (n=237) | Yes (n=451) | ||
| Variable | n(%) | n(%) | n(%) | p (chi2) |
| Female | 331 (48.1) | 93 (39.2) | 238 (52.8) | 0.001 |
| Race | ||||
| White | 482 (70.1) | 199 (84.0) | 283 (62.8) | <0.001 |
| Black | 173 (25.2) | 29 (12.5) | 144 (31.9) | |
| Other | 33 (4.8) | 9 (3.8) | 24 (5.3) | |
| ≥75 years old | 160 (23.3) | 52 (21.9) | 108 (24) | 0.554 |
| Current Smoker | 222 (32.3) | 64 (27.2) | 158 (35) | 0.032 |
| Education | ||||
| < High School | 112 (16.3) | 19 (8.6) | 93 (2 0.6) | <0.001 |
| High school | 164 (23.8) | 47 (19.8) | 117 (25.9) | |
| Trade school/some college | 265 (38.5) | 101 (42.6) | 164 (36.4) | |
| College degree or more | 147 (21.4) | 70 (29.5) | 77 (17.1) | |
| Annual Income | 0.171 | |||
| <$30,000 | 305 (44.3) | 95 (40.1) | 210 (46.6) | |
| $30-50,000 | 160 (23.3) | 55 (23.2) | 105 (23.3) | |
| $50,000+ | 223 (32.4) | 87 (36.7) | 136 (30.2) | |
| REALM-SF (reading level) | ||||
| ≤6th grade | 44 (6.4) | 6 (2.5) | 38 (8.5) | <0.001 |
| 7-8th grade | 132 (19.3) | 29 (12.2) | 103 (22.9) | |
| High school | 509 (74.3) | 201 (85.2) | 308 (68.6) | |
| GOLD stage | ||||
| No fixed airflow obstruction | 213 (36.0) | 71 (30.4) | 141 (3 1.3) | 0.816 |
| 1 and 2 | 285 (41.4) | 102 (43.1) | 183 (40.6) | |
| 3 and 4 | 190 (27.6) | 63 (26.6) | 127 (28.2) | |
| Hospitalized past 3 months | 90 (13.1) | 22 (9.3) | 68 (15.1) | 0.032 |
| Saw a physician in past 3 months | 562 (84.6) | 197 (83.1) | 385 (85.4) | 0.439 |
| Exacerbation past 3 months | 98 (14.2) | 26 (11.4) | 72 (16) | 0.075 |
| Count of inhaler devices used: | ||||
| 1 device | 317 (44.6) | 116 (49.4) | 191 (42.4) | 0.251 |
| 2 devices | 262 (38.1) | 84 (35.4) | 178 (39.5) | |
| 3 or more devices | 119 (17.3) | 37 (15.6) | 82 (18.2) | |
values presented are n (%). <2% missingness for all variables. P-values from chi-squared testing.
Abbreviations: REALM-SF: Assessment of Adult Literacy in Medicine-Short Form
GOLD: Global Initiative for Chronic Obstructive Lung Disease
Associations with poor inhaler technique (adjusted)
Several predictors were associated with poor inhaler technique across all drug delivery devices (ntot=688), with Black race (OR 3.25, 95%CI 1.86-5.67) and other race (OR 1.96, 95%CI 1.14-3.35) associated with increased odds of poor inhaler technique, and higher educational attainment associated with decreased odds of poor inhaler technique (OR 0.35, 95%CI 0.17-0.70 for trade school/some college, OR 0.25, 95%CI 0.11-0.61 for college+, p≤0.001 on test of linear trend). Subjects using multiple different device types were more likely to have poor technique for at least one device (OR 1.21 per device, 95% CI1.05-1.41).
Among the subgroup using MDIs (n=616), the majority of subjects (65.7%) had poor technique. Higher odds of poor technique were associated with Black race (OR 3.82, 95%CI 2.47-5.92), while lower odds were associated with higher educational attainment (OR 0.31, 95%CI 0.14-0.67 for some college/trade school, OR 0.24, 95%CI 0.10-0.55 for college+, p<0.001 on test of linear trend). (Table 2)
Table 2. Results Of Model Building, Adjusted Ors Of Poor Inhaler Technique, Defined As Making An Error In 20% Of Steps For Any Inhaler, And For Each Device (2/11 Steps Mdi, 2/10 Advair Diskus, 3/14 Spiriva Handihaler).
| Error for any inhaler used (n=688) | MDI (n=616) | Diskus (n=190) | Spiriva (n=212) | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| Education | ||||||||
| < High School | referent | referent | referent | referent | ||||
| High school | 0.64 (0.21-1.92) | 0.42 | 0.61 (0.22-1.72) | 0.350 | 0.82 (0.36-1.85) | 0.628 | 0.65 (0.40-2.95) | 0.574 |
| Trade school/some college | 0.35 (0.17-0.70) | 0.003 | 0.31 (0.14-0.67) | 0.003 | 0.48 (0.21-1.10) | 0.085 | 0.62 (0.24-1.52) | 0.311 |
| College or higher | 0.25 (0.11-0.61) | 0.002 | 0.24 (0.10-0.55) | 0.001 | 0.36 (0.14-0.91) | 0.031 | 0.59 (0.25-1.40) | 0.230 |
| Trend | 0.62 (0.54-0.72) | <0.001 | 0.60 (0.52-0.69) | <0.001 | 0.68 (0.53-0.89) | 0.004 | 0.84 (0.72-1.00) | 0.057 |
| Race | ||||||||
| White | referent | referent | referent | referent | ||||
| Black | 3.25 (1.86-5.61) | <0.001 | 3.82 (2.47-5.92) | <0.001 | 2.24 (1.00-5.04) | 0.051 | 2.60 (1.46-4.52) | 0.001 |
| Other | 1.96 (1.14-3.35) | 0.014 | 1.81 (0.91-3.62) | 0.093 | 3.70 (0.33-41.1) | 0.289 | 2.78 (0.39-19.61) | 0.305 |
| Smoker | 1.46 (0.88-2.43) | 0.145 | 1.33 (0.84-2.09) | 0.225 | 2.05 (0.82-5.12) | 0.124 | 1.10 (0.36-3.33) | 0.864 |
| Gold stage | ||||||||
| No AFO | referent | referent | referent | referent | ||||
| 1 to 2 | 1.22 (0.82-1.32) | 0.323 | 1.39 (0.98-1.96) | 0.062 | 0.64 (0.21-2.01) | 0.447 | 1.00 (0.41-2.42) | 1.00 |
| 3 to 4 | 1.14 (0.68-1.92) | 0.628 | 1.17 (0.66-2.10) | 0.570 | 0.49 (0.13-1.88) | 0.301 | 0.74 (0.38-1.46) | 0.392 |
| Count of Devices | 1.20 (1.02-1.41) | 0.029 | 0.97 (0.66-2.10) | 0.795 | 1.40 (1.01-1.93) | 0.043 | 1.05 (0.44-1.50) | 0.773 |
Models adjusted for age in decades, income, and gender. Included variables are the primary predictor and any variable that attained p<0.1 in bivariate analyses for any inhaler, excluding variables that were highly collinear (Pearson's correlation coefficient>0.4). Bold typeface indicates statistical significance. Abbreviations: AFO=airflow obstruction
For subjects using the Advair Diskus (n=193), 49.5% had poor technique. Lower odds of poor technique were associated with higher educational attainment (OR 0.48, 95%CI 0.21-1.10 for some college/trade school, OR 0.36, 95%CI 0.14-0.91 for college+, p=0.004 on test of linear trend). Subjects using multiple device types were more likely to have poor technique (OR 1.40, 95%CI 1.01-1.93). (Table 2)
Finally, a similar pattern was observed for the Spiriva Handihaler (n=212), though fewer subjects had poor technique (33.9%). Black race was associated with increased odds of poor technique (OR 2.60, 95%CI 1.46-4.52). Subjects with higher educational attainment did demonstrate lower odds of poor technique, but this was not statistically significant.
Association of education with individual steps
In unadjusted analyses for MDIs, subjects with less than high school education performed 10% fewer steps correctly (p<0.001). There was significant variation in the percentage of patients performing each step correctly, from 94.8% correctly removing the cap, a critical step to 55.5% for exhaling away from the inhaler. (Figure 2a) In adjusted analyses, subjects with less than high school education were less likely to breathe out fully prior to inhaling the medication (-13.6% of subjects, 95%CI -3.1-24.2%), less likely to breathe out away from the inhaler (-13.7% of subjects, 95%CI -7.0-21.0%), and less likely to breathe normally between puffs (-9.6% of subjects, 95%CI -3.1-16.3%).
In unadjusted analyses, for the Advair Diskus (n=193) subjects with less than high school education performed 10% fewer steps correctly (p<0.001). (Figure 2b) In adjusted analyses, subjects reporting less than high school education were significantly less likely to breathe out fully prior to inhaling the medication (-23.0% of subjects, 95%CI -8.6-37.3%), to exhale away from the device (-20.8% of subjects, 95%CI -2.9-38.7%), a potentially critical error, and to hold their breath correctly (-19.4% of subjects, 95%CI -3.6-35.4%).
In unadjusted analyses, for the Spiriva Handihaler (n=212) subjects with less than high school education performed 6.5% fewer steps correctly (p=0.006). (Figure 2c) In adjusted analyses, subjects reporting less than high school education were slightly more likely to depress the button correctly (8.6% of subjects, 95%CI 0.45-16.7).
Discussion
We found that a significant proportion of stable, ambulatory subjects with COPD made significant errors when using their inhaled therapies, with MDIs being associated with the largest number of errors when compared to the Advair Diskus and Spiriva Handihaler. Black race and lower educational attainment were both associated with increased odds of poor inhaler technique for nearly all devices. Contrary to some previous studies, we found a relatively weak association between multiple devices and poor technique,[21, 24] primarily driven by errors made in the use of the Advair Diskus. This is not surprising given the significant differences between optimum use of the Advair Diskus and the MDI system.
Overall, the largest number of errors were made with MDIs, with the majority of subjects (65.7%) having poor technique. Poor performance with MDIs has been found in multiple other studies, with error rates similar to those found in our study.[20, 31] In our analysis of individual steps, the most errors for both MDIs and Advair were errors of breathing—breath holding, appropriate rate of inhalation, full exhalation, etc. Careful coordination of breathing and breath holding may be difficult for subjects with cough or dyspnea, and is a much more subjective maneuver for a patient to perform in comparison to steps such as twisting the device or pressing to actuate. Many patients demonstrate significant difficulties in hand-breath coordination.[32] In addition, the instructions on breathing technique necessary to obtain the maximum benefit from each device (ex: rapid inhalation vs slow inhalation) vary significantly between devices,[33] further adding to confusion both for patients and instructors. The design of MDIs has remained fairly standard for decades, while newer devices such as breath-actuated inhalers and dry powder inhalers have come on the market more recently. These devices have been shown to give equivalent delivery of drug compared to MDIs with less coordination needed.[4, 34] Consideration of a patient's ability to correctly use a device should be a key part in selecting a given medication.
Our findings of an association between lower educational attainment and poor inhaler technique were expected, and echo the results from several studies of inhaler technique performed abroad.[35, 36] The persistence of a strong association between race and poor inhaler technique, despite adjustment for other markers of SES, is worrisome. There are several possible explanations for these findings. Individuals with less education may be less able to correctly interpret printed material describing the appropriate use of these devices, and may have less applicable knowledge of disease self-management. Unfortunately, up to 15% of adults in the United States have a less than basic level of literacy,[37] which significantly limits their ability to interpret the written materials that accompany inhalers. Formal inhaler teaching beyond written materials is an absolute necessity for these patients. Prior studies have noted worse technique among patients who had not received previous instruction in the use of their inhalers.[24] It is possible that in addition to literacy barriers, subjects with lower educational attainment or subjects who are Black have less access to training in correct device use. Although physicians should be able to provide inhaler teaching, due to time constraints and lack of knowledge, this service is often offered by non-physician medical providers such as pharmacists, respiratory therapists, and nurses. These staff members may not be present in all clinics, particularly free-standing clinics serving low-income or rural populations. Therefore, if a physician lacks the time for teaching and ancillary staff members are not present on site, the only choice for formal teaching would be a referral to an outpatient pharmacy. These types of transitions in the location of care provide a significant barrier to obtaining care. Patients may never undergo inhaler teaching, instead relying on written materials which may have limited effectiveness among individuals with poor healthcare literacy.
The observed variation in technique could be addressed by making inhaler teaching and disease education part of routine medical care for patients at all clinics, and by using novel methods for teaching. Inhaler teaching has been found to be effective among patients with low health literacy at baseline,[38] and routine use may help eliminate the observed disparity. A recent study examining methods of inhaler instruction for hospitalized patients with asthma and COPD found that subjects with low health literacy responded well to the intervention.[31] This suggests that while low educational attainment and health literacy may predict worse technique, they are not a barrier to improvement. Lack of knowledge about inhalers on the part of providers is a significant issue [32] that must be separately addressed. Standardized training videos, such as those offered by the COPD Foundation,[39] offer a time-efficient way for clinics to stay up to date on new devices. Boehringer-Ingelheim, the makers of the new Respimat devices, provided hand-held devices that show with a brief training video on the use of the new device to facilitate teaching of patients, pharmacists, and prescribers. Further study on the effectiveness of these technological interventions is needed.
Our study has several limitations. Each individual was observed using their inhaler by a single trained observer, which did not allow for assessment by multiple observers as would be available with a video recording. While we had reasonable representation of Black and white patients, we had few members of other racial and ethnic groups. The individuals assessed had agreed to participate in a study assessment, and therefore may not be fully representative of patients with COPD in general. However, we suspect that subjects who participate in research are likely to be more engaged in their health and with fewer cognitive issues than the general population, suggesting that our results may in fact underestimate the prevalence of poor inhaler technique. We did not have an assessment of previous formal inhaler teaching, which may be a mediating factor between race, education, and inhaler technique. Finally, it should be noted that a subset of our patients did not meet the threshold for fixed airflow obstruction on pulmonary function testing, but rather were more representative of a real-world, mixed phenotype population of COPD patients. This may actually increase generalizability to patients seen in clinical practice. We also found no association between GOLD stage and correct use of inhalers, suggesting that the presence of airflow obstruction is not an important confounder of inhaler technique. Our study had several strengths, including a multicenter design and detailed information on demographics and disease severity, including pulmonary function tests. Subjects were selected to be representative of multiple geographic regions with variation in demographic characteristics, selection was based on clinically relevant criteria, and the assessment of inhaler technique was performed in an unbiased fashion.
In conclusion, this study confirms that many individuals with COPD have poor technique when using their inhalers, particularly when using MDIs, with associations with lower educational attainment and race. This has important implications, as poor technique has been linked to poor disease control,[1, 2, 35] and when combined with poor adherence, results in high medical costs and missed opportunities for disease management.[10] The odds of making these errors vary by race and educational background—a finding which opens the door to implementing evidence-based, tailored educational interventions to improve technique. Poor inhaler technique may therefore be a significant contributor to worse outcomes among patients with poor health literacy, but may not be a sole barrier to improving technique. One potential approach to improve COPD outcomes and reduce health disparities may include teaching appropriate inhaler technique to all individuals provided with these medications, with methods validated among individuals with poor literacy.
The majority of individuals with COPD (65.6%) demonstrate poor technique for at least one inhaler.
Subjects who are Black or have lower educational attainment are more likely to have poor technique.
The largest number of errors are made with metered dose inhalers compared to other devices.
The most errors made are related to breathing (breath holding, exhalation, rate of inhalation).
Acknowledgments
This material is based upon work supported by the Department of Veterans Affairs, Health Services Research and Development (HSR&D), who provided access to data, office space, and programming and data management. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. We would like to acknowledge the other member sites of the CONCERT Consortium, without whom this project could not have been completed. Dr. Au has personally reviewed the data, understands the statistical methods employed for efficacy analysis, and confirms an understanding of this analysis, that the methods are clearly described and that they are a fair way to report the results. Dr. Melzer was supported by an institutional F-32 (HL007287) through the University of Washington Department of Pulmonary and Critical Care. Additional support was received through the VA Health Services Research and Development (HSR&D). Support for this project was also provided by the National Heart, Lung, and Blood Institute (HL101618) for the CONCERT group. The views presented are that of the researchers and do not necessary reflect those of the Department of Veterans Affairs.
This material is based upon work supported in part by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the United States government, or the NIH. Dr. Au is an unpaid research consultant for Analysis Group.
Footnotes
Conflicts of Interest: None of the other authors have any conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J. 2002;19(2):246–51. doi: 10.1183/09031936.02.00218402. [DOI] [PubMed] [Google Scholar]
- 2.Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M, Dekhuijzen R, Sanchis J, Viejo JL, Barnes P, Corrigan C, Levy M, Crompton GK. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med. 2008;102(4):593–604. doi: 10.1016/j.rmed.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Papi A, Haughney J, Virchow JC, Roche N, Palkonen S, Price D. Inhaler devices for asthma: a call for action in a neglected field. European Respiratory Journal. 2011;37(5):982–985. doi: 10.1183/09031936.00150910. [DOI] [PubMed] [Google Scholar]
- 4.Newman SP, Weisz AW, Talaee N, Clarke SW. Improvement of drug delivery with a breath actuated pressurised aerosol for patients with poor inhaler technique. Thorax. 1991;46(10):712–716. doi: 10.1136/thx.46.10.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dolovich MB, Dhand R. Aerosol drug delivery: developments in device design and clinical use. The Lancet. 377(9770):1032–1045. doi: 10.1016/S0140-6736(10)60926-9. [DOI] [PubMed] [Google Scholar]
- 6.Chrystyn H, Price D. Not all asthma inhalers are the same: factors to consider when prescribing an inhaler. Primary care respiratory journal: journal of the General Practice Airways Group. 2009;18(4):243–9. doi: 10.4104/pcrj.2009.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haughney J, Price D, Barnes NC, Virchow JC, Roche N, Chrystyn H. Choosing inhaler devices for people with asthma: current knowledge and outstanding research needs. Respir Med. 2010;104(9):1237–45. doi: 10.1016/j.rmed.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Usmani OS, Biddiscombe MF, Barnes PJ. Regional lung deposition and bronchodilator response as a function of beta2-agonist particle size. Am J Respir Crit Care Med. 2005;172(12):1497–504. doi: 10.1164/rccm.200410-1414OC. [DOI] [PubMed] [Google Scholar]
- 9.Pedersen S, Hansen OR, Fuglsang G. Influence of inspiratory flow rate upon the effect of a Turbuhaler. Archives of disease in childhood. 1990;65(3):308–10. doi: 10.1136/adc.65.3.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sulaiman I, Seheult J, MacHale E, D'Arcy S, Boland F, McCrory K, Casey J, Bury G, Al-Alawi M, O'Dwyer S, Ryder SA, Reilly RB, Costello RW. Irregular and Ineffective: A Quantitative Observational Study of the Time and Technique of Inhaler Use. The journal of allergy and clinical immunology. 2016;4(5):900–909.e2. doi: 10.1016/j.jaip.2016.07.009. In practice. [DOI] [PubMed] [Google Scholar]
- 11.Laforest L, Denis F, Van Ganse E, Ritleng C, Saussier C, Passante N, Devouassoux G, Chatte G, Freymond N, Pacheco Y. Correlates of adherence to respiratory drugs in COPD patients. Primary care respiratory journal: journal of the General Practice Airways Group. 2010;19(2):148–54. doi: 10.4104/pcrj.2010.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shrestha M, Parupia H, Andrews B, Kim SW, Martin MS, Park DI, Gee E. Metered-dose inhaler technique of patients in an urban ED: prevalence of incorrect technique and attempt at education. The American journal of emergency medicine. 1996;14(4):380–4. doi: 10.1016/s0735-6757(96)90054-6. [DOI] [PubMed] [Google Scholar]
- 13.Agh T, Inotai A, Meszaros A. Factors associated with medication adherence in patients with chronic obstructive pulmonary disease. Respiration. 2011;82(4):328–34. doi: 10.1159/000324453. [DOI] [PubMed] [Google Scholar]
- 14.Barnes PJ. Chronic obstructive pulmonary disease: a growing but neglected global epidemic. PLoS Med. 2007;4(5):e112. doi: 10.1371/journal.pmed.0040112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. CHEST Journal. 2002;121(5_suppl):121S–126S. doi: 10.1378/chest.121.5_suppl.121s. [DOI] [PubMed] [Google Scholar]
- 16.Prescott E, Vestbo J. Socioeconomic status and chronic obstructive pulmonary disease. Thorax. 1999;54(8):737–741. doi: 10.1136/thx.54.8.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Omachi TA, Sarkar U, Yelin EH, Blanc PD, Katz PP. Lower Health Literacy is Associated with Poorer Health Status and Outcomes in Chronic Obstructive Pulmonary Disease. Journal of General Internal Medicine. 2013;28(1):74–81. doi: 10.1007/s11606-012-2177-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodman DE, Israel E, Rosenberg M, Johnston R, Weiss ST, Drazen JM. The influence of age, diagnosis, and gender on proper use of metered-dose inhalers. Am J Respir Crit Care Med. 1994;150(5 Pt 1):1256–61. doi: 10.1164/ajrccm.150.5.7952549. [DOI] [PubMed] [Google Scholar]
- 19.Gray SL, Williams DM, Pulliam CC, Sirgo MA, Bishop AL, Donohue JF. CHaracteristics predicting incorrect metered-dose inhaler technique in older subjects. Archives of Internal Medicine. 1996;156(9):984–988. [PubMed] [Google Scholar]
- 20.Allen SC, Prior A. What determines whether an elderly patient can use a metered dose inhaler correctly? British Journal of Diseases of the Chest. 1986;80:45–49. doi: 10.1016/0007-0971(86)90008-2. [DOI] [PubMed] [Google Scholar]
- 21.van der Palen J, Klein JJ, van Herwaarden CL, Zielhuis GA, Seydel ER. Multiple inhalers confuse asthma patients. Eur Respir J. 1999;14(5):1034–7. doi: 10.1183/09031936.99.14510349. [DOI] [PubMed] [Google Scholar]
- 22.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. INadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114(4):1008–1015. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 23.Hesselink AE, Penninx BW, Wijnhoven HA, Kriegsman DM, van Eijk JT. Determinants of an incorrect inhalation technique in patients with asthma or COPD. Scand J Prim Health Care. 2001;19(4):255–60. doi: 10.1080/02813430152706792. [DOI] [PubMed] [Google Scholar]
- 24.Rootmensen GN, van Keimpema AR, Jansen HM, de Haan RJ. Predictors of incorrect inhalation technique in patients with asthma or COPD: a study using a validated videotaped scoring method. Journal of aerosol medicine and pulmonary drug delivery. 2010;23(5):323–8. doi: 10.1089/jamp.2009.0785. [DOI] [PubMed] [Google Scholar]
- 25.Prieto-Centurion V, Rolle AJ, Au DH, Carson SS, Henderson AG, Lee TA, Lindenauer PK, McBurnie MA, Mularski RA, Naureckas ET, Vollmer WM, Joese BJ, Krishnan JA. Multicenter Study Comparing Case Definitions Used to Identify Patients with Chronic Obstructive Pulmonary Disease. American Journal of Respiratory and Critical Care Medicine. 2014;190(9):989–995. doi: 10.1164/rccm.201406-1166OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishnan JA, Lindenauer PK, Au DH, Carson SS, Lee TA, McBurnie MA, Naureckas ET, Vollmer WM, Mularski RA. Stakeholder Priorities for Comparative Effectiveness Research in Chronic Obstructive Pulmonary Disease. American Journal of Respiratory and Critical Care Medicine. 2013;187(3):320–326. doi: 10.1164/rccm.201206-0994WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woodruff PG, Barr RG, Bleecker E, Christenson SA, Couper D, Curtis JL, Gouskova NA, Hansel NN, Hoffman EA, Kanner RE, Kleerup E, Lazarus SC, Martinez FJ, Paine RI, Rennard S, Tashkin DP, Han MK. Clinical Significance of Symptoms in Smokers with Preserved Pulmonary Function. New England Journal of Medicine. 2016;374(19):1811–1821. doi: 10.1056/NEJMoa1505971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arozullah AM, Yarnold PR, Bennett CL, Soltysik RC, Wolf MS, Ferreira RM, Lee SY, Costello S, Shakir A, Denwood C, Bryant FB, Davis T. Development and validation of a short-form, rapid estimate of adult literacy in medicine. Med Care. 2007;45(11):1026–33. doi: 10.1097/MLR.0b013e3180616c1b. [DOI] [PubMed] [Google Scholar]
- 29.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Press V, Arora V, Shah L, Lewis S, Ivy K, Charbeneau J, Badlani S, Naurekas E, Mazurek A, Krishnan J. Misuse of Respiratory Inhalers in Hospitalized Patients with Asthma or COPD. Journal of General Internal Medicine. 2011;26(6):635–642. doi: 10.1007/s11606-010-1624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Press VG, Arora VM, Trela KC, Adhikari R, Zadravecz FJ, Liao C, Naureckas E, White SR, Meltzer DO, Krishnan JA. Effectiveness of Interventions to Teach Metered-Dose and Diskus® Inhaler Technique: A Randomized Trial. Annals of the American Thoracic Society. 2016 doi: 10.1513/AnnalsATS.201509-603OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Respiratory care. 2005;50(10):1360–74. discussion 1374-5. [PubMed] [Google Scholar]
- 33.Haidl P, Heindl S, Siemon K, Bernacka M, Cloes RM. Inhalation device requirements for patients' inhalation maneuvers. Respiratory Medicine. 118:65–75. doi: 10.1016/j.rmed.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 34.Dhar R, Salvi S, Rajan S, Dalal S, Tikkiwal S, Bhagat R, Ahmed MM, Balki A, Jain M, Gogtay J. Salmeterol/fluticasone through breath-actuated inhaler versus pMDI: a randomized, double-blind, 12 weeks study. The Journal of asthma : official journal of the Association for the Care of Asthma. 2015;52(10):1065–72. doi: 10.3109/02770903.2015.1050499. [DOI] [PubMed] [Google Scholar]
- 35.Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, Serra M, Scichilone N, Sestini P, Aliani M. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respiratory medicine. 2011;105(6):930–938. doi: 10.1016/j.rmed.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Oliveira PDd, Menezes AMB, Bertoldi AD, Wehrmeister FC, Macedo SEC. Assessment of inhaler techniques employed by patients with respiratory diseases in southern Brazil: a population-based study. Jornal Brasileiro de Pneumologia. 2014;40:513–520. doi: 10.1590/S1806-37132014000500007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baer J, Kutner M, Sabatini J. Basic Reading Skills and the Literacy of America's Least Literate Adults: Results from the 2003 National Assessment of Adult Literacy (NAAL) Supplemental Studies (NCES 2009-481) National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education; Washington, DC: 2009. [Google Scholar]
- 38.Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, Brancati FL, Krishnan JA. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172(8):980–6. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cerreta S. Inhaler Training Videos: COPD Foundation. [accessed November 15.2016];2016 < http://www.copdfoundation.org/Learn-More/For-Patients-Caregivers/Educational-Video-Series/Inhaler-Training-Videos.aspx>.