Abstract
The significance of maternal cholesterol transporting to the fetus under normal as well as pathological circumstances is less understood. The objective of this study was to observe the effects of maternal hypercholesterolemia on placental cholesterol transportation. Human full-time placenta, maternal and venous cord blood were sampled at delivery from the pregnant women with serum total cholesterol (TC) concentrations at third trimester higher than 7.25 mM (n = 19) and the pregnant women with normal TC concentrations (n = 19). Serum lipids and expression of genes related to cholesterol transportation were measured by western blot or real-time PCR. The results indicated that serum TC, high density lipoprotein cholesterol (HDL-C), and low density lipoprotein cholesterol (LDL-C) levels were significantly increased, in pregnancies, but decreased in cord blood in hypercholesterolemic group compared to the matched control group. All the subjects were no-drinking, non-smoker, and gestational disease free. The mRNA expression of lipoprotein receptors, including LDLR and VLDLR were significantly increased, while the protein expression of PCSK9 was significantly increased in hypercholesterolemic placenta. In conclusion, maternal hypercholesterolemia might decrease the transportation of cholesterol from mother to fetus because of the high levels of PCSK9 protein expression.
Introduction
During the normal gestation, pregnant women show an increase in serum total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), and triglycerides (TG) levels from first to third trimester [1,2]. Cholesterol, the key composition of cell membranes, metabolic regulators (oxysterols) and precursor of steroid hormones in human bodies, is important for fetal development as a modulator of hedgehog signaling [3]. During the gestation [3], cholesterol in maternal-fetal transport across the placental barrier to sustain the normal fetal development though the fetus can synthesize cholesterol endogenously [4].
Maternal cholesterol was firstly taken up by lipoprotein receptors localized on the human placenta including the low-density lipoprotein receptor (LDLR), the very low density lipoprotein receptor (VLDLR), and the scavenger receptor class B type I (SRBI) [5–7]. Among them, the LDLR is responsible for binding and the internalization of LDL particles and regulating the plasma LDL level [8]. The internalized cholesterol is then either used by the placenta for synthesizing hormones or transferred to the fetus through liver X receptor (LXR) -induced up-regulation of ATP-Binding Cassette Transporter A1 (ABCA1) and G1 (ABCG1) [9].
The increase of serum cholesterol levels has been considered as a normal pregnancy physiologic change with little clinical relevance [10]. And the significance of maternal cholesterol transporting to the fetus under normal as well as pathological circumstances is also less understood. Recently, studies suggest that maternal hyperlipidemia were associated with large for gestational age (LGA) baby [11,12], preeclampsia [13], preterm birth (PTB) [14] and pregnancy-induced hypertension (PIH) [15]. Even, the gestational hypercholesterolemia also resulted in the residence of lipid on the aortas of fetuses of 6-month-old [16].
Few studies suggest that maternal contribution can vary with the maternal metabolic environment during pregnancy [9,17]. Therefore, the objectives of the present study were to (1) analyze the impact of maternal hypercholesterolemia on the expression of cholesterol metabolism genes in human term placenta and (2) to evaluate if there is any correlation between maternal/cord serum cholesterol with the expression of theses transporters.
Materials and methods
Subjects & recruitment
The pregnant women were recruited at the first time of prenatal visit, before their 12th week of pregnancy at Bei Jing Xuanwu hospital, from Jan to Dec 2014. The length of the follow up period is about 28weeks from the first prenatal visit (before their 12th week of pregnancy) to the delivery. This study received ethics approval from the ethical committee of Capital Medical University and Xuanwu Hospital. Written informed consent was obtained from all participants before their enrollment in the study. Pregnant women with endocrine, metabolic disorder (such as diabetes, hypertension, and hypercholesterolemia), severe infectious diseases, and those with multiple pregnancies as well as premature birth, asphyxia in offspring were excluded. Pregnant women who conceived the fetus using artificial methods including in-vitro fertilization were also excluded. There were no data was available about family hypercholesterolemia diagnosis in the recruited pregnant women. After signing a consent form, each woman was interviewed and the information containing general sociodemographic data, medical history, drinking, and smoking habit was obtained by a questionnaire.
There is no definition of gestational hyperlipidemia or hypercholesterolemia and no cutoff value for normal serum cholesterol level for pregnant women. According to the reference [18], the women with serum TC concentration at third trimester (36th week of pregnancy) lower than 7.25 mM were grouped to the control group (n = 19) while women with TC level higher than 7.25 mM were grouped to the hypercholesterolemia group (n = 19). All the subjects were no-drinking, non-smoker, and gestational disease free. The pregnant women in control group were matched with hypercholesterolemia group at age, pre-gestational BMI, and the fetal gender. A follow-up was made to assess body weight and height of the neonates.
Blood and tissue samples
Fasting venous blood samples were collected at first and third trimester from the subjects. At delivery, the venous cord blood and arterial cord blood were collected in gel Vacutainer tube (BD, Oakville, ON, Canada). A portion of placentas were obtained and the amnion, the chorion and the decidual layer were removed Villous tissue was cut into approximately 5 cm2 pieces and kept at -80°C for further use.
The serum levels of TC, LDL-C, HDL-C, and TG were measured individually using the Unicel 36 DX600 Synchron Clinical System (Beckman-Coulter, Mississauga, ON, Canada).
Total RNA extraction and real-time RT-PCR
Total RNA was extracted from placenta tissue using the Trizol reagent (Invitrogen) and reverse transcribed using the Revert Aid First Strand cDNA Synthesis Kit (Thermo Scientific) and Oligo-dT primers (Thermo Scientific) according to the manufacturer’s instructions.
Real-time RT-PCR was performed on the CFX Connect Real-Time Systerm (BIO-RAD) with 480 ng of cDNA template and specific primers using a Thermo Scientific Maxima SYBR Green qPCR Master Mix (Thermo Scientific) according to the manufacturer's protocols. Primers for each gene are listed in Table 1 [9,19–21] were synthesized by Sangon Biotech (Shanghai). PCR conditions were 95°C for 10 min; 59°C for 30 s, and 72°C for 30 s, 40 cycles. The 2-ΔΔCT was used to calculate the relative mRNA expression levels.
Table 1. Primers used for real-time PCR.
| Gene | Forward primer set (5’-3’) | Reverse primer set (5’-3’) |
|---|---|---|
| LDLR | GACGTGGCGTGAACATCTG | CTGGCAGGCAATGCTTTGG |
| VLDLR | TACGCTGTTGTGGAAATGTGAT | ATTCAGCACACGTCTTCTTTACA |
| SRBI | CGGCTCGGAGAGCGACTAC | GGGCTTATTCTCCATGATCACC |
| ABCA1 | ACCCACCCTATGAACAACATGA | GAGTCGGGTAACGGAAACAGG |
| ABCG1 | CAGGAAGATTAGACACTGTGG | GAAAGGGGAATGGAGAGAAGA |
| PPARα | AGCTTTGGCTTTACGGAATACCA | CCACAGGATAAGTCACCGAGGA |
| PPARγ | TCAGGGCTGCCAGTTTCG | CCCTCGGATATGAGAACCC |
| LXRα | AGGGCTGCAAGGGATTCTTCC | TCTGACAGCACACACTCCTCCC |
| LXRβ | GGAGCTGGCCATCATCTCA | GTCTCTAGCAGCATGATCTCGATAGT |
| PCSK9 | ATGGGGCTCTGGTGGCGTGA | TCGACGTCGCTGCGGAAACC |
| GAPDH | GAAGGTGAAGGTCGGAGTCAA | GGAAGATGGTGATGGGATTTC |
Proteins extraction and western blot analysis
The placenta samples (200 mg) were homogenized in 2 ml of lysing buffer using a Fluka homogenizer for 10s for three times on ice. After incubation on ice for 20 min, homogenates were centrifuged at 13,000 g for 20 min at 4°C. Supernatants were collected and protein concentration was measured using a BCA protein detection kit (Biosinoble, China). We separated the proteins on 12% SDS polyacrylamide gels under reducing conditions and transferred them onto PVDF membranes (Bio-Rad, USA). Subsequently, membranes were blocked in 10% bovine serum albumin in Tris buffered saline with 0.1% Tween 20 for 30 minutes. Membranes were incubated with primary antibody (PCSK9 antibody, 1:500 and β-actin antibody, 1:5000) at 4°C for overnight. After five washings with Tris buffered saline containing 0.1% Tween 20 for 3 minutes, membranes were incubated with second antibody at a 1:10000 dilution for 40 minutes. After washing, the membranes were developed with ECL western blotting reagents according to the manufacturer’s instructions. Films were scanned and quantified by using Image-Quant software (Molecular Dynamics).
Statistical analyses
Data were expressed as the means ± SD or SEM, and analyzed with the paired Student’s t-test at p < 0.05 level of significance, to evaluated difference between groups. For the relationship between two variables of the same population, results are expressed as Pearson’s correlation and the curve represent Pearson’s linear correlation. All statistical analyses were performed using the SPSS software 13.0.
Results
Population characteristics
Characteristics of pregnancies and neonates were presented in Table 2. Both in control and hypercholesterolemia group, the age of women was 29 years old. The gestational age was significant longer in hypercholesterolemia women. No significant difference was observed in the pre-gestational BMI, bodyweight gain, newborn birth weight and height, blood pressure, and blood glucose.
Table 2. Population characteristics.
| Control (n = 19) | Hypercholesterolemia (n = 19) | P value | |
|---|---|---|---|
| age (year) | 29.53±3.08 | 29.05±2.86 | 0.626 |
| Gestational age (week) | 39.03±0.92 | 39.73±1.12 | 0.040 |
| Pre-gestational BMI (kg/m2) | 22.28±3.04 | 21.82±3.03 | 0.644 |
| Body weight (kg) | |||
| Pre-gestation | 58.22±9.05 | 57.57±8.83 | 0.825 |
| Second trimester | 68.16±9.73 | 68.37±9.62 | 0.947 |
| Third trimester | 72.90±9.08 | 73.25±10.07 | 0.909 |
| Body weight gain (kg) | 13.68±3.54 | 15.05±6.40 | 0.410 |
| Newborn birth weight (g) | 3466±466 | 3468±392 | 0.985 |
| Newborn height (cm) | 50.18±1.47 | 50.22±1.72 | 0.955 |
| Diastolic blood pressure (mm Hg) | |||
| First trimester | 75.22±9.93 | 71.94±9.24 | 0.155 |
| Second trimester | 68.89±8.14 | 66.18±7.40 | 0.311 |
| Third trimester | 71.50±8.43 | 74.21±6.72 | 0.286 |
| Systolic Blood Pressure(mm Hg) | |||
| First trimester | 111.39±12.98 | 105.65±10.08 | 0.319 |
| Second trimester | 110.56±9.38 | 107.65±10.77 | 0.400 |
| Third trimester | 112.50±10.88 | 114.74±11.36 | 0.545 |
| Fasting blood glucose (g/L) | 4.27±0.34 | 4.25±0.35 | 0.850 |
| OGT1h | 7.27±1.33 | 7.23±1.52 | 0.931 |
| OGT2h | 5.93±1.03 | 6.08±1.23 | 0.682 |
Results are expressed as means ± SD where compared to control group.
Influence of maternal hypercholesterolemia on maternal and cord blood lipids profile
In control and hypercholesterolemia women, the concentrations of serum TC, HDL-C, LDL-C, and TG were given in Table 3. At first trimester, the maternal serum TC and LDL-C concentrations were significantly higher than that in hypercholesterolemia women. At third trimester, TC, HDL-C, and LDL-C levels were significantly increased in hypercholesterolemia group compared to the control group. In all pregnant women, the serum lipids in third trimester were significantly higher than that in first trimester.
Table 3. Serum lipids profile in dams at fist and third trimester.
| First trimester | Third trimester | |||
|---|---|---|---|---|
| Control group (n = 19) | Hypercholesterlemia (n = 19) | Control group (n = 19) | Hypercholesterlemia (n = 19) | |
| TC (mM) | 4.25±0.79 | 4.80±0.49* | 5.25±0.90# | 7.62±0.54*# |
| TG (mM) | 1.41±0.62 | 1.24±0.31 | 3.36±1.42# | 3.38±0.98# |
| HDL-C (mM) | 1.82±0.38 | 2.22±0.31* | 1.97±0.37# | 2.53±0.42*# |
| LDL-C (mM) | 2.19±0.55 | 2.38±0.33 | 2.73±0.81# | 4.55±0.76*# |
| HDL/LDL | 0.88±0.25 | 0.92±0.18 | 0.78±0.24 | 0.57±0.15*# |
* comparing to the control group, P<0.05;
# comparing to the first trimester, P<0.05.
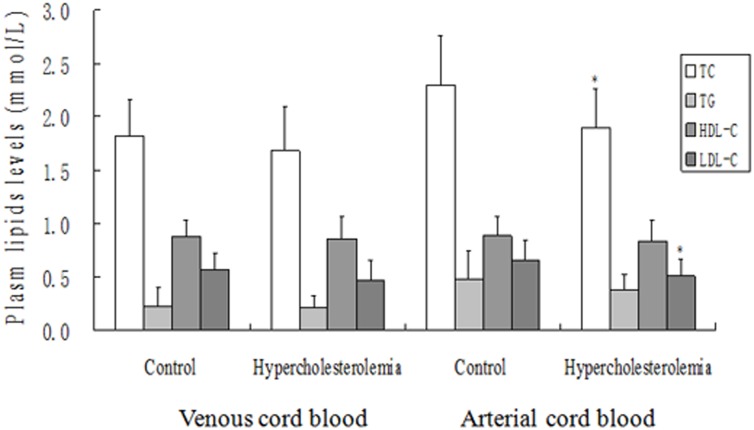
The plasma TC, HDL-C, LDL-C, and TG concentrations in venous cord blood were not significantly different between the two groups, while the TC and LDL-C levels in arterial cord blood were significantly lowed in hypercholesterolemia women (Fig 1).
Fig 1. Influence of maternal hypercholesterolemia on cord blood lipid levels.
* means comparing with control group P<0.05.
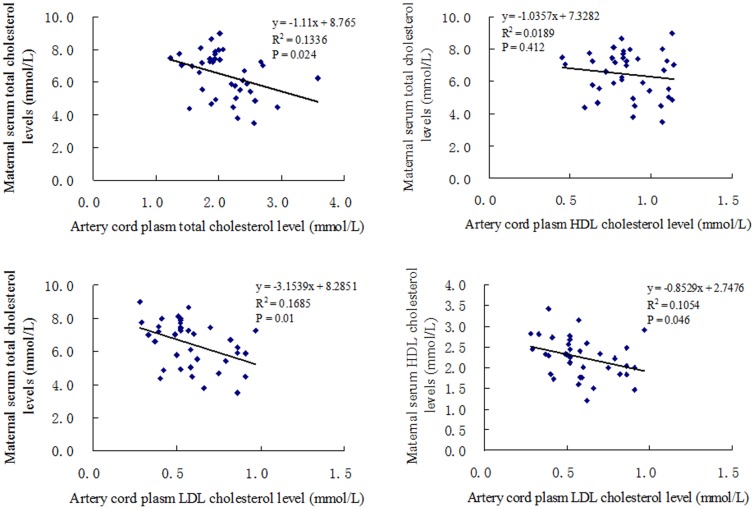
When the correlations between maternal serum cholesterol concentration and cord blood serum lipids were analyzed, no significant correlation were found between maternal serum TC, HDL-C, LDL-C, and TG levels at first trimester and venous cord blood lipids levels. Maternal serum TC and HDL-C concentrations at third trimester were negatively correlated with artery cord plasma LDL-C level significantly (Fig 2). Artery cord plasma TC level was found negatively to correlate with maternal serum TC levels at third trimester significantly (Fig 2).
Fig 2. Correlation analysis between maternal serum cholesterol (third trimester) concentration and artery cord blood cholesterol concentration.
Results are expressed as Pearson’s correlation and the curve represent Pearson’s linear correlation.
Influence of maternal hypercholesterolemia on mRNA expression of lipoprotein receptors, nuclear receptors, and transporters in human term placentas
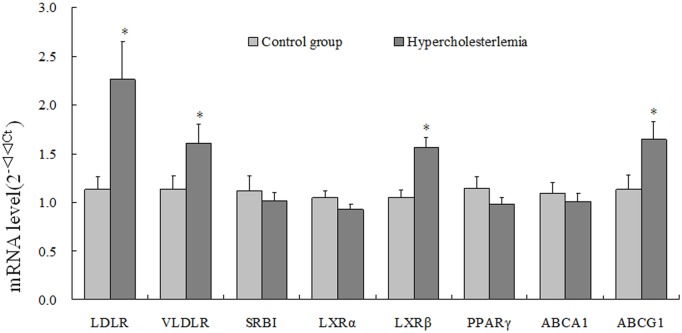
The mRNA expression of lipoprotein receptors, including LDLR and VLDLR were significantly increased in placenta from hypercholesterolemic women comparing to control group, while the expression of SRBI was not affected significantly. Among the three nuclear receptors regulating cholesterol metabolism in cells, only the LXRβ’s expression was significantly increased. The mRNA expression of ABCG1, the membrane transporter that mediates cellular efflux of cholesterol, was significantly induced by maternal hypercholesterolemia. The mRNA expressions of other genes measured in the present study were not significant difference between in two groups (Fig 3).
Fig 3. Expressions of genes related to cholesterol transporting in placenta.
Real-time PCR analysis of ABCG1, LXRβ, LXRα, SRBI, PPARγ, VLDLR, ABCA1 and LDLR genes expression from placenta of control and hypercholesterolemia groups. Results are the means ± SE (n = 19).
Influence of maternal hypercholesterolemia on mRNA and protein expression of PCSK9 in human term placentas
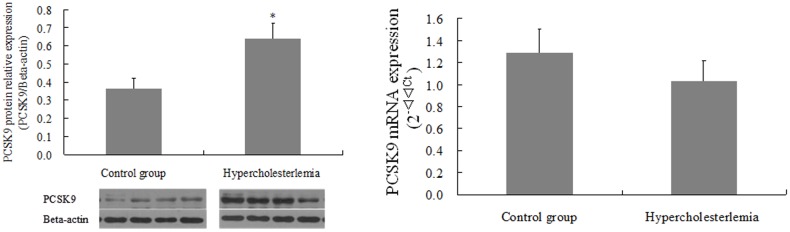
The protein expression of PCSK9 was significantly increased by maternal hypercholesterolemia compared to control group with no significantly change of mRNA expression in human term placenta (Fig 4).
Fig 4. Pcsk9 protein expression (western blot, A) and mRNA expression (real-time PCR, B) in placenta from control and hypercholesterolemic pregnancy.
Results are the means ± SEM (n = 17). *p < 0.01 compared to control group.
Discussion
In the present study, the lipids profile of pregnant women at first and third trimester were analyzed and the results showed that TC, TG, HDL-C, and LDL-C levels were significant higher in third trimester. The results indicated that the transportation of cholesterol to fetus was lower in hypercholesterolemic pregnancy evidenced by the significant lower artery plasma TC and LDL-C levels and significant higher expression of PCSK9 in placenta.
In fetal development, cholesterol plays an important role as it is a fundamental component of cell membranes and a precursor substance for steroid hormones [22]. The fetus can synthesize cholesterol endogenously [4], nevertheless the placenta also transports cholesterol from maternal circulation to the fetus by cholesterol-carrying lipoproteins, such as LDL, HDL and VLDL [23]. Maternal cholesterol has been shown to across the placenta and enter the fetal circulation, contributing substantially to the fetal cholesterol pool in animals [24] and humans [25]. Maternal hypercholesterolemia may pose a significant risk [26] to the fetus on account of the increase in maternal cholesterol transfer to fetus and then the formation of fatty streak in the artery [16]. So, it was supposed that cholesterol transportation increased as the maternal serum cholesterol concentration increased. Using 3H labeled cholesteryl oleate [27], Burke and the colleagues found that increasing maternal lipoprotein-cholesterol concentrations could enhance the cholesterol in maternal-fetal transport. It was even showed that there was a direct correlation between the concentration of maternal cholesterol and the presence of fatty streaks in fetus [16]. Vuorio[28] also showed a significant increase of cholesterol and LDL-C in the cord blood of familiar hypercholesterolemia(FH) newborns if compared with non-FH newborns. In our study, the cord blood cholesterol concentrations were lower in hypercholesterolemia group than that in control ones. And the negative correlations were found between the maternal serum cholesterol concentrations at third trimester and artery blood cholesterol levels, indicating the possibility that there were less cholesterol transportation from mothers to fetus in hypercholesterolemic pregnant women. We supposed the transfer of the cholesterol to the fetal circulation may be altered in hypercholesterolemic group. Some authors [29] have reported that there were no associations between maternal and newborn cholesterol levels. Marseille-Tremblay [30] and Ethier-Chiasson M [31] found a decrease serum TC and LDL-C concentrations in venous cord blood. So, the study design might be the major factors resulted in the discrepancy.
Placenta is a vital organ for cholesterol transfer from the maternal to the fetus. ABCG1, LXRβ, LXRα, SRBI, PPARγ, VLDLR, ABCA1 and LDLR are important factors responsible for cholesterol transportation localized on placenta [23]. In our study, we found that the mRNA expression of ABCA1 which priority expressed on the maternal side to induce a decreased cholesterol efflux [32] was unchanged, whereas the mRNA expression of ABCG1 which priority expressed on the fetal side of the placenta to provoke a decreased cholesterol efflux was significant increased in hypercholesterolemic pregnancies. Evemie Dube [9] and Anger [33] have shown that the expression of ABCA1 and ABCG1 mRNA and other ABC transporters are not changed in GDM pregnancies. The increased expression of ABCG1 could be part of a compensatory mechanism to satisfy the demand of cholesterol to the fetal circulation. A study [34] using mice found that the lacking of PCSK9 increased the protein expression of LDLR in the liver reducing the cholesterol in the circulation. The altered mRNA expression of LDLR and VLDLR could be attributed to the maternal inflammatory status [35]. There is a now growing evidence [36] that during the first weeks of life, the fetus largely depend on maternal cholesterol as its cholesterol source when most organs developed. Petar [37] found that PCSK9 mRNA is most ample in yolk sac and fetal liver. While the abundant PCSK9 degraded the cholesterol receptors to transfer the cholesterol from maternal to the fetal to support the organs develop during the early pregnancy. At the third trimester, fetus’s cholesterol is synthesized by itself, mainly by the fetal liver [38]. In this period, placental may plays a protection role in the cholesterol circulation from maternal to the fetal to prevent so much cholesterol transport to the fetal. So we found the increased level of PCSK9 protein expression may plays such a part in the circulation of cholesterol to the fetal. Leiva [39] suggested that newborn umbilical blood lipoprotein and triglyceride concentrations compared with those in maternal circulation were lower, without comparing the different between newborns.
This study has some advantages from other studies. First, the control pregnant women were matched with the hypercholesterolemic pregnant women in age, pre-gestational BMI, and fetal gender, and then, the confounders were adjusted. Second, the fasting samples were used during the first and third time of pregnancy. Some researchers measured the lipids in umbilical venous blood, but we measured both the venous and artery blood. But we also have limitations, such as the sample size is small and the DNA test for the pregnancies and the newborns is lack.
In conclusion, our study found that lipid profiles in maternal and cord blood are altered in the case of hypercholesterolemic pregnancies and the consequence of the modulation of placental LDLR and PCSK9 expression in the control of cholesterol concentrations in both term placenta and fetus. Our experiment using human placenta and thus cannot be observed the maternal cholesterol levels how inhibited the cholesterol transports from mother to fetus in full-term. Further studies would be assessed the exact influence of these changes on placental cholesterol transport with dynamic observation.
Supporting information
(PPT)
Acknowledgments
We thank all the pregnancies who contributied date from 2014 to 2015. We would like to thank the Editor and the reviewers for their suggestions and comments, which helped to improve the quality of this paper.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by the National Natural Science Foundation of China (81273070) HLY. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mazurkiewicz JC, Watts GF, Warburton FG, Slavin BM, Lowy C, Koukkou E. Serum lipids, lipoproteins and apolipoproteins in pregnant non-diabetic patients. J Clin Pathol. 1994; 47(8):728–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piechota W, Staszewski A. Reference ranges of lipids and apolipoproteins in pregnancy. Eur J Obstet Gynecol Reprod Biol. 1992; 16;45(1):27–35. [DOI] [PubMed] [Google Scholar]
- 3.Palinski W. Maternal-fetal cholesterol transport in the placenta: good, bad, and target for modulation. Circ Res. 2009; 104: 569–571. 10.1161/CIRCRESAHA.109.194191 [DOI] [PubMed] [Google Scholar]
- 4.Herrera E. Lipid metabolism in pregnancy and its consequences in the fetus and newborn. Endocrine. 2002; 19: 43–55. 10.1385/ENDO:19:1:43 [DOI] [PubMed] [Google Scholar]
- 5.Furuhashi M, Seo H, Mizutani S, Narita O, Tomoda Y, Matsui N. Expression of low density lipoprotein receptor gene in human placenta during pregnancy. Mol Endocrinol.1989; 3: 1252–1256. 10.1210/mend-3-8-1252 [DOI] [PubMed] [Google Scholar]
- 6.Wadsack C, Hammer A, Levak-Frank S, Desoye G, Kozarsky KF, Hirschmugl B, et al. Selective cholesteryl ester uptake from high density lipoprotein by human first trimester and term villous trophoblast cells. Placenta. 2003;24: 131–143. [DOI] [PubMed] [Google Scholar]
- 7.Wittmaack FM, Gafvels ME, Bronner M, Matsuo H, McCrae KR, Tomaszewski JE, et al. Localization and regulation of the human very low density lipoprotein/apolipoprotein-E receptor: trophoblast expression predicts a role for the receptor in placental lipid transport. Endocrinology.1995; 136: 340–348. 10.1210/endo.136.1.7828550 [DOI] [PubMed] [Google Scholar]
- 8.Hu L, van der Hoogt CC, Espirito Santo SM, Out R, Kypreos KE, van Vlijmen BJ, et al. The hepatic uptake of VLDL in lrp-ldlr-/-vldlr-/- mice is regulated by LPL activity and involves proteoglycans and SR-BI. J Lipid Res. 2008; 49: 1553–1561. 10.1194/jlr.M800130-JLR200 [DOI] [PubMed] [Google Scholar]
- 9.Dube E, Ethier-Chiasson M, Lafond J. Modulation of cholesterol transport by insulin-treated gestational diabetes mellitus in human full-term placenta. Biol Reprod. 2013; 88: 16 10.1095/biolreprod.112.105619 [DOI] [PubMed] [Google Scholar]
- 10.Tabatabaei M. Gestational weight gain, prepregnancy body mass index related to pregnancy outcomes in KAZERUN, FARS, IRAN. J Prenat Med. 2011; 5: 35–40. [PMC free article] [PubMed] [Google Scholar]
- 11.Di Cianni G, Miccoli R, Volpe L, Lencioni C, Ghio A, Giovannitti MG, et al. Maternal triglyceride levels and newborn weight in pregnant women with normal glucose tolerance. Diabet Med. 2005; 22: 21–25. [DOI] [PubMed] [Google Scholar]
- 12.Kushtagi P, Arvapally S. Maternal mid-pregnancy serum triglyceride levels and neonatal birth weight. Int J Gynaecol Obstet. 2009; 106: 258–259. 10.1016/j.ijgo.2009.03.004 [DOI] [PubMed] [Google Scholar]
- 13.Magnussen EB, Vatten LJ, Lund-Nilsen TI, Salvesen KA, Davey Smith G, Romundstad PR, et al. Prepregnancy cardiovascular risk factors as predictors of pre-eclampsia: population based cohort study. BMJ. 2007; 335: 978 10.1136/bmj.39366.416817.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Catov JM, Bodnar LM, Kip KE, Hubel C, Ness RB, Harger G, et al. Early pregnancy lipid concentrations and spontaneous preterm birth. Am J Obstet Gynecol. 2007; 197: 610 e611–617. [DOI] [PubMed] [Google Scholar]
- 15.Jan MR, Nazli R, Shah J, Akhtar T. A study of lipoproteins in normal and pregnancy induced hypertensive women in tertiary care hospitals of the north west frontier province-Pakistan. Hypertens Pregnancy. 2012; 31: 292–299. 10.3109/10641955.2010.507843 [DOI] [PubMed] [Google Scholar]
- 16.Napoli C, D'Armiento FP, Mancini FP, Postiglione A, Witztum JL, Palumbo G, et al. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J Clin Invest. 1997; 100: 2680–2690. 10.1172/JCI119813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Busso D, Mascareno L, Salas F, Berkowitz L, Santander N, Quiroz A, et al. Early onset intrauterine growth restriction in a mouse model of gestational hypercholesterolemia and atherosclerosis. Biomed Res Int. 2014; 2014: 280497 10.1155/2014/280497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liguori A, D'Armiento FP, Palagiano A, Balestrieri ML, Williams-Ignarro S, de Nigris F, et al. Effect of gestational hypercholesterolaemia on omental vasoreactivity, placental enzyme activity and transplacental passage of normal and oxidised fatty acids. BJOG. 2007; 114: 1547–1556. 10.1111/j.1471-0528.2007.01510.x [DOI] [PubMed] [Google Scholar]
- 19.Dong B, Singh AB, Fung C, Kan K, Liu J. CETP inhibitors downregulate hepatic LDL receptor and PCSK9 expression in vitro and in vivo through a SREBP2 dependent mechanism. Atherosclerosis. 2014; 235: 449–462. 10.1016/j.atherosclerosis.2014.05.931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daoud G, Simoneau L, Masse A, Rassart E, Lafond J. Expression of cFABP and PPAR in trophoblast cells: effect of PPAR ligands on linoleic acid uptake and differentiation. Biochim Biophys Acta. 2005; 1687: 181–194. 10.1016/j.bbalip.2004.11.017 [DOI] [PubMed] [Google Scholar]
- 21.Dube E, Chan PT, Hermo L, Cyr DG. Gene expression profiling and its relevance to the blood-epididymal barrier in the human epididymis. Biol Reprod. 2007; 76: 1034–1044. 10.1095/biolreprod.106.059246 [DOI] [PubMed] [Google Scholar]
- 22.Brett KE, Ferraro ZM, Yockell-Lelievre J, Gruslin A, Adamo KB. Maternal-fetal nutrient transport in pregnancy pathologies: the role of the placenta. Int J Mol Sci. 2014; 15: 16153–16185. 10.3390/ijms150916153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woollett LA. Review: Transport of maternal cholesterol to the fetal circulation. Placenta. 2011; 32 Suppl 2: S218–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woollett LA. Maternal cholesterol in fetal development: transport of cholesterol from the maternal to the fetal circulation. Am J Clin Nutr. 2005; 82: 1155–1161. [DOI] [PubMed] [Google Scholar]
- 25.Yoshida S, Wada Y. Transfer of maternal cholesterol to embryo and fetus in pregnant mice. J Lipid Res. 2005; 46: 2168–2174. 10.1194/jlr.M500096-JLR200 [DOI] [PubMed] [Google Scholar]
- 26.Narverud I, Iversen PO, Aukrust P, Halvorsen B, Ueland T, Johansen SG, et al. Maternal familial hypercholesterolaemia (FH) confers altered haemostatic profile in offspring with and without FH. Thromb Res. 2013; 131: 178–182. 10.1016/j.thromres.2012.11.008 [DOI] [PubMed] [Google Scholar]
- 27.Burke KT, Colvin PL, Myatt L, Graf GA, Schroeder F, Woollett LA, et al. Transport of maternal cholesterol to the fetus is affected by maternal plasma cholesterol concentrations in the golden Syrian hamster. J Lipid Res. 2009; 50: 1146–1155. 10.1194/jlr.M800538-JLR200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vuorio AF, Miettinen TA, Turtola H, Oksanen H, Gylling H. Cholesterol metabolism in normal and heterozygous familial hypercholesterolemic nerborns. J Lab Clin Med. 2002;140(1):35–42. [DOI] [PubMed] [Google Scholar]
- 29.Bansal N, Cruickshank JK, McElduff P, Durrington PN. Cord blood lipoproteins and prenatal influences. Curr Opin Lipidol. 2005; 16: 400–408. [DOI] [PubMed] [Google Scholar]
- 30.Marseille-Tremblay C, Ethier-Chiasson M, Forest JC, Giguere Y, Masse A, Mounier C, et al. Impact of maternal circulating cholesterol and gestational diabetes mellitus on lipid metabolism in human term placenta. Mol Reprod Dev. 2008; 75: 1054–1062. 10.1002/mrd.20842 [DOI] [PubMed] [Google Scholar]
- 31.Ethier-Chiasson M, Duchesne A, Forest JC, Giguere Y, Masse A, Mounier C, et al. Influence of maternal lipid profile on placental protein expression of LDLr and SR-BI. Biochem Biophys Res Commun.2007; 359: 8–14. 10.1016/j.bbrc.2007.05.002 [DOI] [PubMed] [Google Scholar]
- 32.Aye IL, Waddell BJ, Mark PJ, Keelan JA. Placental ABCA1 and ABCG1 transporters efflux cholesterol and protect trophoblasts from oxysterol induced toxicity. Biochim Biophys Acta. 2010; 1801: 1013–1024. 10.1016/j.bbalip.2010.05.015 [DOI] [PubMed] [Google Scholar]
- 33.Anger GJ, Cressman AM, Piquette-Miller M. Expression of ABC Efflux transporters in placenta from women with insulin-managed diabetes. PLoS One. 2012; 7: e35027 10.1371/journal.pone.0035027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rashid S, Curtis DE, Garuti R, Anderson NN, Bashmakov Y, Ho YK, et al. Decreased plasma cholesterol and hypersensitivity to statins in mice lacking Pcsk9. Proc Natl Acad Sci U S A. 2005; 102: 5374–5379. 10.1073/pnas.0501652102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poirier S, Mayer G, Benjannet S, Bergeron E, Marcinkiewicz J, Nassoury N, et al. The proprotein convertase PCSK9 induces the degradation of low density lipoprotein receptor (LDLR) and its closest family members VLDLR and ApoER2. J Biol Chem. 2008; 283: 2363–2372. 10.1074/jbc.M708098200 [DOI] [PubMed] [Google Scholar]
- 36.Baardman ME, Kerstjens-Frederikse WS, Berger RM, Bakker MK, Hofstra RM, Plösch T. The role of maternal-fetal cholesterol transport in early fetal life: current insights. Biol Reprod. 2013; 88: 24 10.1095/biolreprod.112.102442 [DOI] [PubMed] [Google Scholar]
- 37.Grozdanov PN, Petkov PM, Karagyozov LK, Dabeva MD. Expression and localization of PCSK9 in rat hepatic cells. Biochem Cell Biol. 2013; 84: 80–92. [DOI] [PubMed] [Google Scholar]
- 38.Jurevics HA, Kidwai FZ, Morell P. Sources of cholesterol during development of the rat fetus and fetal organs. J Lipid Res. 1997; 38: 723–733. [PubMed] [Google Scholar]
- 39.Leiva A, Salsoso R, Saez T, Sanhueza C, Pardo F, Sobrevia L. Cross-sectional and longitudinal lipid determination studies in pregnant women reveal an association between increased maternal LDL cholesterol concentrations and reduced human umbilical vein relaxation. Placenta. 2015; 36: 895–902. 10.1016/j.placenta.2015.05.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PPT)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.