Abstract
Background
Diastolic dysfunction of the left ventricle is common but frequently under-diagnosed. Particularly in advanced stages affected patients may present with significant functional tricuspid regurgitation (TR) as the most prominent sign on echocardiography. The underlying left ventricular pathology may eventually be missed and symptoms of heart failure are attributed to TR, with respective therapeutic consequences.
The aim of the present study was to determine prevalence and mechanisms underlying TR evolution in heart failure with preserved ejection fraction (HFpEF).
Methods and results
Consecutive HFpEF patients were enrolled in this prospective, observational study. Confirmatory diagnostic tests including echocardiography and invasive hemodynamic assessments were performed.
Of the 175 patients registered between 2010 and 2014, 51% had significant (moderate or severe) TR without structural abnormalities of the tricuspid valve. Significant hemodynamic differences between patients with and without relevant TR were encountered. These included elevated pulmonary vascular resistance (p = 0.038), reduced pulmonary arterial compliance (PAC, p = 0.005), and elevated left ventricular filling pressures (p = 0.039) in the TR group. Multivariable binary logistic regression analysis revealed diastolic pulmonary artery pressure (p = 0.029) and PAC (p = 0.048) as independent determinants of TR.
Patients were followed for 18.1±14.1 months, during which 32% had a cardiac event. While TR was associated with outcome in the univariable analysis, it failed to predict event-free survival in the multivariable model.
Conclusions
The presence of ´isolated´ functional TR should prompt the suspicion of HFpEF. Our data show that significant TR is a marker of advanced HFpEF but neither an isolated entity nor independently associated with event-free survival.
1. Introduction
Diastolic dysfunction of the left ventricle that may convert into the clinical picture of heart failure with preserved ejection fraction (HFpEF) is a growing health care problem [1, 2]. We have observed that in advanced disease stages affected patients frequently present with significant functional tricuspid regurgitation (TR) as the most prominent sign on echocardiographic examination. The underlying left ventricular pathology may eventually be missed and symptoms of heart failure are attributed to TR. Although current guidelines on the management of valvular heart disease lack any recommendation for the treatment of ´isolated´ functional TR [3, 4] affected patients may be referred to surgical repair [5]. In the present work we hypothesized that hemodynamic alterations characteristic of HFpEF [6–8] cause functional TR.
2. Methods
2.1 Study design
The present study was undertaken in order to determine the prevalence of significant TR in HFpEF patients, the underlying mechanisms, and its impact on event-free survival. This was a prospective observational study performed at the Medical University of Vienna, approved by the local ethics committee (Ethics Committee of the Medical University of Vienna, EK #796/2010). All participants gave written informed consent.
After thorough baseline evaluation, patients were followed by ambulatory visits and phone calls at 6-month intervals. A combined endpoint consisting of hospitalization for heart failure or death from cardiac causes was defined as the main outcome measure. Endpoints were adjudicated by our adjudication committee consisting of CZT and AAK, who were blinded to hemodynamics and other patient characteristics. An age-matched control group was also assessed with respect to clinical characteristics and imaging parameters.
2.2 Diagnosis of heart failure with preserved ejection fraction
Consecutive patients with HFpEF were enrolled. HFpEF was diagnosed in the presence of: (1) symptoms or signs of heart failure; (2) normal or mildly reduced LV systolic function (LV ejection fraction (EF) >50%); and (3) evidence of abnormal LV relaxation or diastolic stiffness [1, 2].
Reasons for exclusion were: significant coronary artery disease as diagnosed by coronary angiography, significant aortic or mitral valve disease, congenital heart disease, and cardiac amyloidosis as diagnosed by cardiac magnetic resonance imaging (CMR) and / or endomyocardial biopsy. Furthermore, patients with chronic lung disease such as bronchial asthma or chronic obstructive pulmonary disease (COPD) with FEV1 <60% of predicted, restrictive lung disease with TLC <60% of predicted and / or current O2 therapy were excluded from the study.
The hemodynamic diagnosis of HFpEF was confirmed, if the pulmonary artery wedge pressure (PAWP) exceeded 12 mm Hg [1].
2.3 Assessment of tricuspid regurgitation
All echo studies were performed by board certified physicians, using high-end scanners such as GE Vivid 5 and Vivid 7 (GE Healthcare, Wauwatosa, WI, USA). The evaluation included M-mode and 2-dimensional echocardiography, as well as conventional and color Doppler ultrasonography according to current recommendations [9–11].
TR was quantified by an integrated approach (Table 1) [9, 11, 12]. Moderate and severe TR were considered significant and were compared with trace and mild TR. The graduation into non-significant and significant TR was chosen to account for inaccuracies due to the semiquantitative assessment of TR by echocardiography and has previously been deemed reasonable [5, 13, 14].
Table 1. Echocardiographic parameters used for grading of tricuspid regurgitation severity [9].
| Parameter | Mild | Moderate | Severe |
|---|---|---|---|
| Tricuspid valve | Normal | Normal or abnormal | Abnormal / flail leaflet / poor coaptation |
| RV/RA/IVC size | Normal | Normal or dilated | Dilated |
| VC width [mm] | Not defined | Not defined, but <7 | >7 |
| PISA radius [mm] | ≤5 | 6–9 | >9 |
| Hepatic vein flow | Systolic dominance | Systolic blunting | Systolic reversal |
RV indicates right ventricle; RA, right atrium; IVC, inferior vena cava; VC, vena contracta; PISA, proximal isovelocity surface area.
LVEF was assessed with the biplane Simpson´s method. Right ventricular (RV) function was assessed by the percentage RV fractional area change (FAC), defined as (end-diastolic area—end-systolic area) / end-diastolic area x 100, according to recent recommendations [15]. In addition, tricuspid annular plane systolic excursion (TAPSE) was measured [15]. RV dysfunction was defined as FAC < 35% and TAPSE <16 mm [15].
2.4 Influence of TR on imaging and hemodynamic parameters
Imaging and hemodynamic variables were split into two groups: 1. influenced by TR (i.e. TR- dependent) and 2. not influenced by TR (TR- independent). Changes in right heart segments and pressures were considered as TR- dependent, while pulmonary vasculature and left heart segments were defined as TR- independent.
2.5 Right and left heart catheterization
For right heart catheterization a 7F Swan-Ganz catheter (Baxter, Irvine, CA) was inserted via a jugular or femoral access. Filling pressures were averaged after recording of eight heart cycles using CathCorLX (Siemens AG, Berlin and Munich, Germany). PAWP, pulmonary arterial pressure (PAP), and cardiac output (CO), were determined. CO was measured by both thermodilution and Fick method. Simultaneously, all patients underwent direct assessment of LV filling pressures, followed by coronary angiography. Standard formulae were used for the calculation of hemodynamic parameters[16, 17].
2.6 Cardiac magnetic resonance imaging
CMR was primarily used as a complimentary method for the assessment of RV function. All patients without pacemaker or other precluding conditions underwent CMR at baseline, using a 1.5-T scanner (Avanto, Siemens Medical Solutions, Erlangen, Germany). Functional and late gadolinium enhancement imaging studies were performed according to standard protocols [18]. RV dysfunction was defined as RVEF <45%. Two independent observers (SA, AB) blinded to clinical data read all CMR studies.
2.7 Statistical analysis
Categorical variables were reported in percent and/or total numbers. Continuous data are presented as mean ± standard deviation. Baseline characteristics were compared using chi square or Fisher´s exact test for categorical variables and Wilcoxon two sample test for continuous variables. Variables were stratified into TR-dependent (right atrial (RA) and RV size, RV function, RA pressure, and PAP) and TR-independent (all others; see Tables 2–4). Binary logistic regression analysis was used to identify TR-independent parameters associated with the presence of significant TR. A multivariable regression model using a stepwise approach was run for clinical, hemodynamic and imaging parameters, respectively. To identify variables associated with cardiac events, a univariable Cox regression model was performed for each influence factor, followed by a multiple Cox regression model with stepwise backward selection. This was done for clinical, hemodynamic and imaging parameters.
Table 2. Baseline clinical characteristics of HFpEF patients and controls.
| HFpEF patients (n = 175) | Controls (n = 45) | p-value | |
|---|---|---|---|
| Baseline Characteristics | |||
| Age (years) | 71.0±8.7 | 69.9±7.2 | 0.263 |
| Female (%) | 69.1 | 53.3 | 0.046 |
| BMI (kg/m2) | 30.9±7.0 | 28.4±4.7 | 0.018 |
| Atrial Fibrillation (%) | 60.6 | 8.0 | 0.001 |
| Diabetes (%) | 38.6 | 18.3 | 0.008 |
| Arterial Hypertension (%) | 97.7 | 91.0 | 0.070 |
| CAD (%) | 20.5 | N/A | N/A |
| COPD, mild (%) | 37.8 | 24.6 | 0.096 |
| History of smoking (%) | 34.3 | 35.6 | 0.895 |
| Pacemaker (%) | 10.5 | 0.0 | 0.024 |
| NYHA (%) | <0.001 | ||
| NYHA II | 30.7 | 0.0 | |
| NYHA III-IV | 69.3 | 0.0 | |
| SBP (mmHg) | 137.4±21.0 | 150.9±11.4 | <0.001 |
| DBP (mmHg) | 78.2±12.9 | 69.4±11.3 | <0.001 |
| Heart rate (bpm) | 72.3±14.8 | 65.7±11.5 | 0.008 |
| NT-proBNP (pg/ml) | 1876.6±2916.5 | 288.9±227±3 | <0.001 |
| GFR (ml/1.73m2) | 59.1±20.0 | 68.4±11.8 | 0.001 |
BMI indicates body mass index; CAD, coronary artery disease as assessed by coronary angiography; COPD, chronic obstructive pulmonary disease; NYHA, New York Heart Association functional class; SBP, systolic blood pressure; DBP, diastolic blood pressure; GFR, glomerular filtration rate.
Table 4. Baseline clinical characteristics of HFpEF patients, stratified by tricuspid regurgitation severity.
| All patients (n = 175) | Non-significant TR (48.8%) | Significant TR (51.2%) | p-value | |
|---|---|---|---|---|
| Baseline Characteristics | ||||
| Age (years) | 71.0±8.7 | 69.5±9.2 | 72.5±7.8 | 0.026 |
| Female (%) | 69.2 | 70.2 | 68.2 | 0.770 |
| BMI (kg/m2) | 30.9±7.0 | 31.4±6.6 | 29.8±6.3 | 0.172 |
| Atrial Fibrillation (%) | 60.6 | 41.5 | 78.4 | <0.001 |
| Diabetes (%) | 38.6 | 38.6 | 38.6 | 0.991 |
| Arterial Hypertension (%) | 97.7 | 97.6 | 97.7 | 0.953 |
| CAD (%) | 20.5 | 24.1 | 17.0 | 0.253 |
| COPD, mild (%) | 37.8 | 41.2 | 34.7 | 0.423 |
| History of smoking* (%) | 34.3 | 36.1 | 32.6 | 0.623 |
| Pacemaker (%) | 10.5 | 9.6 | 11.4 | 0.713 |
| NYHA (%) | 0.028 | |||
| NYHA II | 30.7 | 38.8 | 22.9 | |
| NYHA III-IV | 69.3 | 61.3 | 77.2 | |
| 6-MWD (m) | 319.9±123.0 | 341.6±114.1 | 300.0±128.4 | 0.036 |
| SBP (mmHg) | 137.4±21.0 | 141.9±20.5 | 133.7±20.7 | 0.012 |
| DBP (mmHg) | 78.2±12.9 | 79.5±12.0 | 77.4±13.6 | 0.249 |
| Heart rate (bpm) | 72.3±14.8 | 71.1±14.7 | 73.0±14.5 | 0.348 |
| NT-proBNP (pg/ml) | 1876.6±2916.5 | 1290.8±1901.1 | 2405.3±3545.1 | <0.001 |
| GFR (ml/1.73m2) | 59.1±20.0 | 64.0±21.1 | 54.7±18.1 | 0.008 |
| Beta-blocker (%) | 73.3 | 71.0 | 75.0 | 0.586 |
| Calcium channel blocker (%) | 27.4 | 37.1 | 20.2 | 0.024 |
| ARB (%) | 35.6 | 43.5 | 29.8 | 0.086 |
| ACE-I (%) | 32.9 | 27.4 | 36.9 | 0.228 |
| Diuretics (%) | 76.0 | 67.7 | 82.1 | 0.044 |
TR indicates tricuspid regurgitation; BMI, body mass index; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; NYHA, New York Heart Association functional class; 6-MWD, six-minute walk distance; SBP, systolic blood pressure; DBP, diastolic blood pressure; GFR, glomerular filtration rate; ARB, angiotensin II receptor blocker; ACE-I, angiotensin-converting-enzyme inhibitor.
* Only two patients were current smokers.
Statistical analyses were performed using SPSS Statistics Version 18 (IBM, Armonk, NY) and STATA version 12 (Stata Corp, College Station, TX). Statistical significance was set at p<0.05 for all tests. P-values were considered exploratory.
3. Results
3.1 Baseline characteristics
Between January 2010 and November 2014, 175 consecutive patients with a confirmed diagnosis of HFpEF and 45 age-matched control subjects were registered. Clinical and imaging characteristics of patients and controls are summarized in Tables 2 and 3. While 51% of HFpEF patients presented with significant TR, none of the control subjects had significant TR.
Table 3. Baseline imaging characteristics of HFpEF patients and controls.
| HFpEF patients (n = 175) | Controls (n = 45) | p-value | |
|---|---|---|---|
| Echocardiography | |||
| TR- dependent | |||
| RA diameter (mm) | 63.0±9.6 | 51.5±5.1 | <0.001 |
| RA area (cm2) | 26.8±9.3 | 18.5±4.2 | <0.001 |
| RVEDD (mm) | 37.4±7.6 | 31.8±3.6 | <0.001 |
| TAPSE (mm) | 19.6±5.8 | 24.6±3.1 | <0.001 |
| sPAP (mmHg) | 60.0±17.8 | 38.4±8.4 | <0.001 |
| Significant TR (%) | 51.2 | 0.0 | <0.001 |
| TR- independent | |||
| LA diameter (mm) | 64.2±8.3 | 52.5±5.8 | <0.001 |
| LA area (cm2) | 29.3±7.1 | 22.7±4.1 | <0.001 |
| LVEDD (mm) | 45.1±5.8 | 44.0±3.5 | 0.326 |
| LVEF (%) | 60.4±9.4 | 59.6±8.9 | 0.164 |
| IVS (mm) | 12.6±2.0 | 12.6±1.5 | 0.586 |
| E/E’ | 16.2±7.4 | 9.5±3.7 | <0.001 |
| E/A | 2.4±2.6 | 0.9±1.6 | <0.001 |
| Cardiac magnetic resonance imaging | |||
| TR- dependent | |||
| RA diameter (mm) | 65.1±9.2 | 56.0±6.6 | <0.001 |
| RA area (cm2) | 29.1±10.2 | 22.2±3.7 | <0.001 |
| RVEDD (mm) | 39.6±7.5 | 36.5±3.9 | 0.008 |
| RVEDV (ml) | 157.7±111.6 | 126.8±29.8 | 0.048 |
| RVEF (%) | 52.7±11.0 | 57.6±7.4 | 0.007 |
| TR- independent | |||
| LA diameter (mm) | 65.2±9.2 | 56.3±6.4 | <0.001 |
| LA area (cm2) | 31.2±9.4 | 25.0±5.1 | <0.001 |
| LVEDD (mm) | 47.6±5.9 | 47.1±6.7 | 0.533 |
| IVS (mm) | 11.4±2.2 | 11.1±1.5 | 0.580 |
| LVEDV (ml) | 127.5±46.2 | 127.2±24.9 | 0.422 |
| LVEF (%) | 63.3±11.2 | 68.5±6.6 | 0.004 |
| CO (l/min) | 5.3±1.8 | 5.7±1.4 | 0.105 |
Parameters are listed according to right heart segments (TR-dependent) versus right heart afterload (TR-independent). Changes in right heart segments are considered consequences of both right heart afterload as well as TR, while parameters of right ventricular afterload are not thought to be influenced by TR.
TR indicates tricuspid regurgitation; RA, right atrium; RVEDD, right ventricular end-diastolic diameter; RV FAC, right ventricular fractional area change; TAPSE, tricuspid annular plane systolic excursion; sPAP, systolic pulmonary artery pressure; LA, left atrium; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; IVS, interventricular septal thickness; E/A, ratio of early to late ventricular filling velocities; E/E’, ratio of transmitral early peak velocity to septal mitral annulus velocity; RVEDV, right ventricular end-diastolic volume; RVEF, right ventricular ejection fraction; LVEDV, left ventricular end-diastolic volume; CO, cardiac output.
Baseline characteristics of HFpEF patients, stratified by tricuspid regurgitation severity, are displayed in Table 4.
In brief, patients with relevant TR were older (p = 0.026), more frequently presented with atrial fibrillation (p<0.001), and renal dysfunction (p = 0.008). Furthermore, TR patients were more symptomatic as measured by NYHA functional class (p = 0.028), had lower systolic blood pressures (p = 0.012), and shorter 6-minute walk distances (p = 0.036).
Table 5 lists imaging parameters with respect to the presence or absence of significant TR. Right heart dimensions were enlarged in TR patients (mean RA area, p<0.001; mean RV end-diastolic diameter, p<0.001), and RV systolic function by FAC was worse (p = 0.001) than in the comparator.
Table 5. Baseline imaging characteristics in HFpEF patients, stratified by tricuspid regurgitation severity.
| All (n = 175) | Non-significant TR (48.8%) | Significant TR (51.2%) | p-value | |
|---|---|---|---|---|
| Echocardiography | ||||
| TR- dependent | ||||
| RA diameter (mm) | 63.0±9.6 | 59.4±7.9 | 66.7±10.0 | <0.001 |
| RA area (cm2) | 26.8±9.3 | 23.2±6.8 | 30.5±10.1 | <0.001 |
| RVEDD (mm) | 37.4±7.6 | 34.5±6.3 | 40.4±7.6 | <0.001 |
| RV FAC (%) | 41.0±12.8 | 44.4±12.5 | 37.6±12.3 | 0.001 |
| TAPSE (mm) | 19.6±5.8 | 20.9±5.2 | 18.2±6.1 | 0.001 |
| sPAP (mmHg) | 60.0±17.8 | 52.4±15.7 | 65.8±17.2 | <0.001 |
| TR- independent | ||||
| LA diameter (mm) | 64.2±8.3 | 62.3±8.2 | 66.1±9.1 | 0.003 |
| LA area (cm2) | 29.3±7.1 | 28.0±6.9 | 30.7±7.0 | 0.020 |
| LVEDD (mm) | 45.1±5.8 | 45.2±6.0 | 45.0±5.6 | 0.790 |
| LVEF (%) | 60.4±9.4 | 61.4±10.5 | 59.2±8.2 | 0.263 |
| IVS (mm) | 12.6±2.0 | 12.9±2.0 | 12.4±1.9 | 0.027 |
| E/E’ | 16.2±7.4 | 16.4±7.3 | 15.9±7.5 | 0.636 |
| E/A | 2.4±2.6 | 2.0±3.0 | 3.0±2.0 | <0.001 |
| Cardiac magnetic resonance imaging (n = 122, 70% of all patients) | ||||
| TR- dependent | ||||
| RA diameter (mm) | 65.1±9.2 | 61.4±7.9 | 69.1±9.0 | <0.001 |
| RA area (cm2) | 29.1±10.2 | 24.9±6.9 | 33.9±11.2 | <0.001 |
| RVEDD (mm) | 39.6±7.5 | 36.9±6.2 | 42.8±7.7 | <0.001 |
| RVEDV (ml) | 157.7±111.6 | 131.9±39.2 | 187.6±153.6 | 0.001 |
| RVEF (%) | 52.7±11.0 | 55.2±11.5 | 49.5±9.6 | 0.006 |
| TR-independent | ||||
| LA diameter (mm) | 65.2±9.2 | 62.6±8.3 | 68.0±9.6 | 0.002 |
| LA area (cm2) | 31.2±9.4 | 28.3±7.9 | 34.5±10.1 | <0.001 |
| LVEDD (mm) | 47.6±5.9 | 47.3±6.2 | 47.4±5.4 | 0.238 |
| IVS (mm) | 11.4±2.2 | 11.9±2.3 | 10.9±2.0 | 0.024 |
| LVEDV (ml) | 127.5±46.2 | 130.1±54.4 | 124.4±35.7 | 0.923 |
| LVEF (%) | 63.3±11.2 | 64.3±11.8 | 62.3±10.7 | 0.223 |
| CO (l/min) | 5.3±1.8 | 5.4±2.1 | 5.2±1.6 | 0.985 |
Parameters are listed according to right heart segments versus right heart afterload. Changes in right heart segments are considered consequences of both right heart afterload as well as TR, while parameters of right ventricular afterload are not thought to be influenced by TR.
TR indicates tricuspid regurgitation; RA, right atrium; RVEDD, right ventricular end-diastolic diameter; RV FAC, right ventricular fractional area change; TAPSE, tricuspid annular plane systolic excursion; sPAP, systolic pulmonary artery pressure; LA, left atrium; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; IVS, interventricular septal thickness; E/A, ratio of early to late ventricular filling velocities; E/E’, ratio of transmitral early peak velocity to septal mitral annulus velocity; RVEDV, right ventricular end-diastolic volume; RVEF, right ventricular ejection fraction; LVEDV, left ventricular end-diastolic volume; CO, cardiac output.
Left atrial (LA) chamber dimensions were also enlarged in TR patients (p = 0.003) reflecting elevated LV filling pressures. Further significant differences were found with respect to interventricular septum thickness (p = 0.027) and E/A ratio (p<0.001).
Table 6 shows hemodynamic parameters with respect to the presence or absence of significant TR. Importantly, subtle but significant between-group differences were found with respect to invasively measured hemodynamic parameters of RV afterload, i.e. PVR (p = 0.038), pulmonary arterial compliance (PAC; p = 0.005), and LV filling pressures (PAWP, p = 0.039).
Table 6. Baseline hemodynamic characteristics of HFpEF patients, stratified by tricuspid regurgitation severity.
| All (n = 175) | Non-significant TR (48.8%) | Significant TR (51.2%) | p-value | |
|---|---|---|---|---|
| Hemodynamic parameters | ||||
| TR independent | ||||
| sPAP (mmHg) | 52.7±17.0 | 48.6±14.4 | 55.7±17.9 | 0.021 |
| dPAP (mmHg) | 22.1±7.4 | 20.3±6.8 | 23.5±7.3 | 0.007 |
| mPAP (mmHg) | 33.8±9.9 | 31.4±8.9 | 35.7±9.9 | 0.009 |
| DPG (mmHg) | 2.3±5.4 | 1.3±4.6 | 3.0±5.8 | 0.132 |
| TPG (mmHg) | 14.1±7.0 | 12.5±6.0 | 15.3±7.3 | 0.036 |
| PPP (mmHg) | 30.5±12.4 | 28.2±10.9 | 32.2±13.3 | 0.057 |
| PAWP (mmHg) | 19.9±5.2 | 19.0±5.6 | 20.6±4.6 | 0.039 |
| PVR (dyn·s·cm−5) | 226.3±141.9 | 188.6±93.9 | 257.4±168.8 | 0.038 |
| PAC (ml/mmHg) | 2.8±1.5 | 3.2±1.8 | 2.5±1.2 | 0.005 |
| Cardiac Output (l/min) | 5.3±1.3 | 5.5±1.4 | 5.1±1.2 | 0.085 |
| TR dependent | ||||
| RAP (mmHg) | 12.8±5.8 | 11.1±5.7 | 14.2±5.4 | <0.001 |
TR indicates tricuspid regurgitation; sPAP, systolic pulmonary artery pressure; dPAP, diastolic pulmonary artery pressure; mPAP, mean pulmonary artery pressure; DPG, diastolic pulmonary vascular pressure gradient; TPG, transpulmonary pressure gradient; PPP, pulmonary pulse pressure; PAWP, pulmonary artery wedge pressure; PVR, pulmonary vascular resistance; PAC, pulmonary arterial compliance; RAP, right atrial pressure.
3.2 Factors determining the occurrence of tricuspid regurgitation
Table 7 summarizes the results of the uni- and multivariable binary logistic regression analyses. With respect to clinical parameters, atrial fibrillation was found to be independently associated with TR (p<0.001, Table 5). We also tested the association of TR- independent parameters (RV afterload) and the occurrence of TR. Multivariable analysis of hemodynamic parameters revealed diastolic PAP (p = 0.029) and PAC (p = 0.048) as independently associated with TR occurrence. Among imaging variables LA size (p = 0.001) was independently associated with the presence of significant TR.
Table 7. Uni- and multivariable binary logistic regression analysis for the presence of significant tricuspid regurgitation.
| B | p-value | HR (95% CI) | p-value | HR (95% CI) | ||
|---|---|---|---|---|---|---|
| UNIVARIABLE | MULITVARIABLE | |||||
| Clinical parameters | ||||||
| Male sex | 0.097 | 0.770 | 1.101 | (0.576–2.106) | ||
| Age | 0.041 | 0.027 | 1.042 | (1.005–1.081) | ||
| BMI | -0.035 | 0.174 | 0.965 | (0.917–1.016) | ||
| BSA | -0.185 | 0.795 | 0.831 | (0.207–3.341) | ||
| Obesity | -0.258 | 0.482 | 0.773 | (0.376–1.586) | ||
| AF | 1.635 | <0.001 | 5.127 | (2.620–10.034) | <0.001 | 4.864 (2.470–9.580) |
| Diabetes | 0.003 | 0.991 | 1.003 | (0.542–1.858) | ||
| Hypertension | 0.060 | 0.953 | 1.062 | (0.146–7.715) | ||
| COPD | -0.277 | 0.423 | 0.758 | (0.385–1.493) | ||
| CAD | -0.435 | 0.255 | 0.647 | (0.306–1.370) | ||
| Imaging parameters | ||||||
| LA diameter | 0.075 | 0.001 | 1.067 | (1.0326–1.109) | 0.001 | 1.067 (1.026–1.109) |
| LVEDD | -0.007 | 0.781 | 0.993 | (0.942–1.046) | ||
| IVS | -0.107 | 0.128 | 0.898 | (0.782–1.031) | ||
| LVEF | -0.003 | 0.681 | 0.997 | (0.980–1.013) | ||
| Hemodynamic parameters | ||||||
| sPAP | 0.028 | 0.010 | 1.028 | (1.007–1.050) | ||
| dPAP | 0.069 | 0.008 | 1.071 | (1.018–1.127) | 0.029 | 1.061 (1.006–1.119) |
| mPAP | 0.049 | 0.008 | 1.050 | (1.013–1.089) | ||
| PAWP | 0.062 | 0.058 | 1.064 | (0.998–1.134) | ||
| CO | -0.245 | 0.054 | 0.783 | (0.610–1.005) | ||
| DPG | 0.067 | 0.052 | 1.070 | (0.999–1.145) | ||
| TPG | 0.066 | 0.014 | 1.068 | (1.013–1.125) | ||
| PVR | 0.005 | 0.004 | 1.005 | (1.002–1.008) | ||
| PPP | 0.028 | 0.046 | 1.028 | (1.001–1.057) | ||
| PAC | -0.321 | 0.011 | 0.725 | (0.565–0.930) | 0.048 | 0.776 (0.603–0.997) |
All tested variables were determined at baseline.
TR-dependent variables were excluded from this analysis.B indicates regression correlation coefficient; HR, hazard ratio; CI, confidence interval; BMI, body mass index; BSA, body surface area; AF, atrial fibrillation; COPD, chronic obstructive pulmonary disease; CAD, coronary artery disease; LA, left atrium; LVEDD, left ventricular end-diastolic diameter; IVS, interventricular septum; LVEF, left ventricular ejection fraction; sPAP, systolic pulmonary artery pressure; dPAP, diastolic pulmonary artery pressure; mPAP, mean pulmonary artery pressure; PAWP, pulmonary artery wedge pressure; CO, cardiac output; DPG, diastolic pulmonary vascular pressure gradient; TPG, transpulmonary pressure gradient; PVR, pulmonary vascular resistance; PPP, pulmonary pulse pressure; PAC, pulmonary artery compliance.
3.3. Tricuspid regurgitation and event-free survival
Table 8 shows the results of the uni- and multivariable model with respect to event-free survival. Mean follow-up was 18.1±14.1 months (range: 0.1–48.0 months). Within the follow-up period, none of the patients with non-relevant TR developed relevant TR and vice-versa.
Table 8. Uni- and multivariable Cox regression analysis for event-free survival.
| p-value | HR (95% CI) | p- value | HR (95% CI) | |
|---|---|---|---|---|
| UNIVARIABLE | MULTIVARIABLE | |||
| Clinical parameters | ||||
| Age | 0.065 | 1.031 (0.998–1.065) | ||
| Male gender | 0.111 | 1.554 (0.904–2.672) | ||
| BMI | 0.064 | 1.034 (0.998–1.072) | ||
| 6-MWD | <0.001 | 0.995 (0.992–0.997) | <0.001 | 0.995 (0.992–0.998) |
| AF | 0.012 | 2.131 (1.178–3.853) | ||
| Diabetes | 0.003 | 2.234 (1.314–3.797) | ||
| Hyperlipidemia | 0.503 | 0.836 (0.495–1.412) | ||
| Hypertension | 0.506 | 1.957 (0.271–14.150) | ||
| CAD | 0.810 | 1.081 (0.571–2.047) | ||
| COPD | 0.030 | 1.901 (1.064–3.397) | 0.010 | 2.207 (1.209–4.030) |
| Pacemaker | 0.045 | 2.076 (1.016–4.245) | ||
| NT-proBNP * | <0.001 | 1.937 (1.478–2.539) | <0.001 | 1.744 (1.283–2.371) |
| GFR | 0.001 | 0.976 (0.963–0.989) | ||
| Hemodynamic parameters | ||||
| sPAP | <0.001 | 1.029 (1.016–1.042) | <0.001 | 1.029 (1.016–1.043) |
| dPAP | <0.001 | 1.065 (1.031–1.101) | ||
| mPAP | <0.001 | 1.049 (1.024–1.075) | ||
| RAP | <0.001 | 1.080 (1.032–1.130) | ||
| PAWP | 0.007 | 1.070 (1.018–1.124) | ||
| Cardiac output | 0.753 | 0.967 (0.783–1.194) | ||
| Stroke volume | 0.242 | 1.007 (0.995–1.019) | ||
| DPG | 0.008 | 1.077 (1.019–1.138) | ||
| TPG | <0.001 | 1.074 (1.035–1.114) | ||
| PVR | <0.001 | 1.003 (1.002–1.005) | ||
| PPP | <0.001 | 1.035 (1.017–1.053) | ||
| PAC | 0.016 | 0.720 (0.552–0.940) | ||
| Echocardiographic parameters | ||||
| LVEDD | 0.404 | 1.019 (0.974–1.067) | ||
| LVEF | 0.169 | 1.020 (0.992–1.049) | ||
| LA diameter | 0.008 | 1.043 (1.011–1.076) | ||
| IVS | 0.143 | 0.900 (0.781–1.036) | ||
| RVEDD | 0.001 | 1.058 (1.023–1.094) | ||
| RV FAC | 0.009 | 0.972 (0.952–0.993) | 0.011 | 0.9967 (0.942–0.992) |
| RA diameter | 0.061 | 1.025 (0.999–1.053) | ||
| E/A | 0.006 | 1.109 (1.030–1.194) | 0.003 | 1.147 (1.046–1.256) |
| E/E’ | 0.104 | 1.039 (0.992–1.089) | ||
| TAPSE | 0.060 | 0.941 (0.883–1.003) | ||
| Significant TR | 0.005 | 2.242 (1.279–3.929) | ||
| Cardiac magnetic resonance imaging parameter | ||||
| LVEDD | 0.688 | 0.988 (0.932–1.048) | ||
| RVEDD | 0.066 | 1.037 (0.998–1.078) | ||
| IVS | 0.987 | 1.001 (0.865–1.159) | ||
| LA | 0.024 | 1.042 (1.005–1.080) | ||
| RA | 0.166 | 1.026 (0.990–1.063) | ||
| LVEF | 0.406 | 1.013 (0.982–1.046) | ||
| LVEDV | 0.875 | 0.999 (0.992–1.007) | ||
| CO | 0.643 | 0.954 (0.780–1.166) | ||
| RVEF | 0.039 | 2.096 (1.036–4.241) | 0.043 | 2.071 (1.024–4.189) |
| RVEDV | 0.802 | 1.000 (0.998–1.003) | ||
All variables were determined at baseline. Patients were followed for a mean of 18.1±14.1 months.
HR, hazard ratio; CI, confidence interval; 6-MWD, six minute walking distance; AF, atrial fibrillation; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; GFR, glomerular filtration rate; sPAP, systolic pulmonary artery pressure; dPAP, diastolic pulmonary artery pressure; mPAP, mean pulmonary artery pressure; RAP, right atrial pressure; PAWP, pulmonary artery wedge pressure; DPG, diastolic pressure gradient; TPG, transpulmonary pressure gradient; PVR, pulmonary vascular resistance; PPP, pulmonary pulse pressure; PAC, pulmonary artery compliance; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; LA, left atrium; IVS, interventricular septal thickness; RVEDD, right ventricular end-diastolic diameter; RV FAC, right ventricular fraction area change; RA, right atrium; E/A, ratio of early to late ventricular filling velocities; E/E’, ratio of transmitral early peak velocity to septal mitral annulus velocity; TAPSE, tricuspid annular plane systolic excursion; TR, tricuspid regurgitation; LVEDV, left ventricular end-diastolic volume; CO, cardiac output; RVEF, right ventricular ejection fraction; RVEDV, right ventricular end-diastolic volume.
* NT-proBNP was analyzed by quartiles.
While TR was associated with outcome in the univariable analysis, it failed to predict event-free survival in the multivariable model. Independent predictors of cardiac events or death included 6-minute walk distance (p<0.001), chronic obstructive pulmonary disease (p = 0.010), NT-proBNP (p<0.001), E/A ratio (p = 0.003), RV dysfunction (p = 0.011) and systolic PAP (p<0.001).
4. Discussion
We suggest that “isolated” functional TR is a feature of HFpEF. In fact, we demonstrate here that the evolution of TR is associated with only subtle hemodynamic changes, such as reduced PAC and elevated PAP in the presence of elevated LV filling pressures. Furthermore, we show that the presence of significant TR indicates adverse outcome but is not independently associated with event-free survival.
Significant TR is a common finding [19], and has primarily been studied in patients with heart failure and reduced ejection fraction [13, 20–22] as well as those with mitral and aortic valve disease [23–25]. Thus, TR is mostly functional in nature and is thought to be the consequence of geometric alterations caused by RV dilatation, distortion of the subvalvular apparatus, tricuspid annular dilatation or a combination of these factors [26]. However, pathomechanisms underlying isolated functional TR in the absence of overt left heart pathology have not been studied.
4.1 Prevalence of tricuspid regurgitation in heart failure with preserved ejection fraction
We and others [27] have observed that a substantial number of consecutively enrolled HFpEF patients also suffer from relevant TR.
Despite well-established diagnostic criteria for HFpEF [2, 28] the awareness among physicians is still limited and the condition is by far under-diagnosed [29]. In a substantial number of patients presenting with shortness of breath and preserved LV systolic function, significant TR may be the only overt pathology detected by transthoracic echocardiography beneath subtle signs of diastolic dysfunction.
4.2 Etiology of tricuspid regurgitation in heart failure with preserved ejection fraction
In a recent publication [27], potential mechanisms underlying TR evolution in HFpEF have been discussed, attributing a role to annular dilatation due to atrial enlargement in atrial fibrillation, presence of pulmonary hypertension, or pacemaker lead impingement on the tricuspid valve leaflets. In the present study, there was no difference in TR severity between pacemaker carriers and the remainder of the group. While displacement of the right annulus in patients with atrial fibrillation is a possible mechanism of TR, the present study for the first time provides clear evidence for the pathomechanistic impact of the pulmonary circulation for TR development. In fact, pulmonary hypertension was present in both groups with and without relevant TR. However, the degree of pulmonary hypertension was more pronounced in patients with significant TR, reflected by slightly higher pulmonary pressures. In the multivariable regression model diastolic PAP was identified as a parameter independently associated with relevant TR. Moreover, PAC was lower in the TR group compared with the non-TR group and also remained independently associated with relevant TR.
PAC in post-capillary pulmonary hypertension is dependent on PAWP [30]. Indeed, PAWP was significantly higher in the TR versus non-TR group.
4.3 Significance of tricuspid regurgitation in heart failure with preserved ejection fraction
With respect to event-free survival, relevant TR failed to predict outcome in the Cox regression analysis (Table 8). This is in line with a recent report by Mohammed et al [27] where RV dysfunction but not TR was an independent predictor of adverse outcome. These findings suggest that the presence of functional relevant TR is a bystander or marker of disease, but not a stand-alone pathology in HFpEF.
4.4 Right ventricular dysfunction in heart failure with preserved ejection fraction
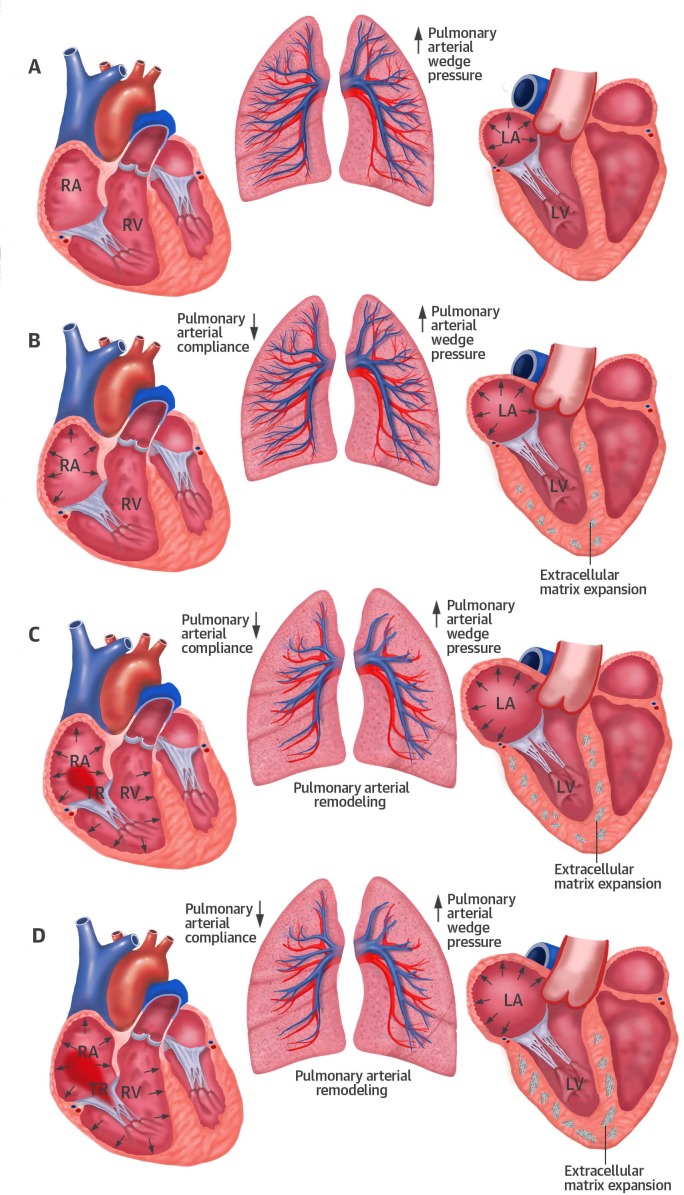
In contrast to non-TR patients, those with significant TR had larger right heart dimensions and worse RV function by echo as well as CMR studies. RV dysfunction was an independent predictor of event-free survival in the present study (Table 8), confirming previous publications [6, 8, 27]. As illustrated in Fig 1, RV dysfunction ensues elevation of LV filling pressures causing a passive and—occasionally–also active rise in PAP due to pulmonary vascular remodeling [31]. As soon as significant TR develops due to RV dilatation, volume overload adds to the pre-existing pressure overload, thereby promoting the vicious circle of RV failure. In the presence of significant TR, the degree of RV systolic dysfunction may frequently be underestimated in analogy to LV systolic function in the presence of mitral regurgitation. Because RV dysfunction is a key determinant of prognosis, more emphasis should be put on its evaluation, in particular in the presence of relevant TR.
Fig 1. Pathomechanistic processes underlying the development of tricuspid regurgitation in heart failure with preserved ejection fraction.
HFpEF is characterized by impaired left ventricular (LV) diastolic function due to abnormal relaxation and increased chamber stiffness. The consecutive rise in LV filling pressure results in a passive rise of pulmonary arterial pressure (PAP, Panel A). As a consequence, pulmonary vascular compliance declines and adds to the increasing resistance against the right ventricle (RV, Panel B). Remodeling of the pre-capillary pulmonary vascular bed may occur as an additional mechanism aggravating RV pressure overload (Panel C). The RV fails to compensate pressure overload and dilates. Tricuspid annular dilatation and distortion of the subvalvular apparatus lead to increasing tricuspid regurgitation and consecutive right heart failure (Panel D).
Reprinted with permission from John Wiley and Sons, from Aschauer et al. [8], license number 3858290307001.
5. Limitations
The present study has been undertaken in a single center with a relatively small sample size. A center-specific bias cannot be excluded. However, the major advantages of limiting data collection to a single center are 1. inclusion of a homogenous patient population, 2. constant clinical routine, 3. constant quality of assessment techniques and 4. constant follow-up.
CO derived by the thermodilution method may be confounded by the presence of relevant TR. However, there was a tight correlation between this method and additional CO measurements, including the Fick method (r = 0.631, p<0.001) and the CMR-derived CO (r = 0.515, p<0.001). Parameters of LA function have not been assessed in the present study.
6. Conclusions
The diagnosis of ´isolated´ functional TR should prompt further evaluation of the LV, in particular with respect to the presence of LV diastolic dysfunction. In addition to non-invasive assessment, right heart catheter to determine the relation between pulmonary pressures and flow should be considered, since only subtle changes may be associated with relevant TR. Although patients with significant TR face a dismal prognosis, TR itself is not independently associated with outcome. Our data suggest that isolated TR is a bystander of HFpEF and the necessity of therapeutic interventions, such as tricuspid valve surgery, should be questioned.
Data Availability
All relevant data are within the paper.
Funding Statement
This study received support from the Austrian Society of Cardiology (to JM; http://www.atcardio.at/en), the Österreichischer Herzfonds (to JM; http://www.herzfonds.at) and the Austrian Science Fund (FWF; https://www.fwf.ac.at) grant KLI 245 (to JM) and KLI 246 (to DB). There are no relationships with industry. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28(20):2539–50. Epub 2007/04/13. 10.1093/eurheartj/ehm037 [DOI] [PubMed] [Google Scholar]
- 2.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr., Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2013;62(16):e147–239. 10.1016/j.jacc.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 3.Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;63(22):e57–185. Epub 2014/03/08. 10.1016/j.jacc.2014.02.536 [DOI] [PubMed] [Google Scholar]
- 4.Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Baron-Esquivias G, Baumgartner H, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012;33(19):2451–96. Epub 2012/08/28. 10.1093/eurheartj/ehs109 [DOI] [PubMed] [Google Scholar]
- 5.Kammerlander AA, Marzluf BA, Graf A, Bachmann A, Kocher A, Bonderman D, et al. Right Ventricular Dysfunction, But Not Tricuspid Regurgitation, Is Associated With Outcome Late After Left Heart Valve Procedure. Journal of the American College of Cardiology. 2014;64(24):2633–42. 10.1016/j.jacc.2014.09.062 [DOI] [PubMed] [Google Scholar]
- 6.Goliasch G, Zotter-Tufaro C, Aschauer S, Duca F, Koell B, Kammerlander AA, et al. Outcome in Heart Failure with Preserved Ejection Fraction: The Role of Myocardial Structure and Right Ventricular Performance. PloS one. 2015;10(7):e0134479 10.1371/journal.pone.0134479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mascherbauer J, Marzluf BA, Tufaro C, Pfaffenberger S, Graf A, Wexberg P, et al. Cardiac magnetic resonance postcontrast T1 time is associated with outcome in patients with heart failure and preserved ejection fraction. Circ Cardiovasc Imaging. 2013;6(6):1056–65. Epub 2013/09/17. 10.1161/CIRCIMAGING.113.000633 [DOI] [PubMed] [Google Scholar]
- 8.Aschauer S, Kammerlander AA, Zotter-Tufaro C, Ristl R, Pfaffenberger S, Bachmann A, et al. The right heart in heart failure with preserved ejection fraction: insights from cardiac magnetic resonance imaging and invasive haemodynamics. European journal of heart failure. 2016;18(1):71–80. 10.1002/ejhf.418 [DOI] [PubMed] [Google Scholar]
- 9.Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, et al. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010;11(4):307–32. 10.1093/ejechocard/jeq031 [DOI] [PubMed] [Google Scholar]
- 10.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7(2):79–108. Epub 2006/02/07. 10.1016/j.euje.2005.12.014 [DOI] [PubMed] [Google Scholar]
- 11.Pierard LA, Moonen M, Lancellotti P. Valvular Regurgitation In: Zamorano JL, Bax JJ, Knuuti J, Rademakers FE, editors. The ESC Textbook of Cardiovascular Imaging. London: Springer; 2010. p. 150–76. [Google Scholar]
- 12.Rivera JM, Vandervoort PM, Mele D, Siu S, Morris E, Weyman AE, et al. Quantification of tricuspid regurgitation by means of the proximal flow convergence method: a clinical study. Am Heart J. 1994;127(5):1354–62. [DOI] [PubMed] [Google Scholar]
- 13.Neuhold S, Huelsmann M, Pernicka E, Graf A, Bonderman D, Adlbrecht C, et al. Impact of tricuspid regurgitation on survival in patients with chronic heart failure: unexpected findings of a long-term observational study. European heart journal. 2013;34(11):844–52. Epub 2013/01/22. 10.1093/eurheartj/ehs465 [DOI] [PubMed] [Google Scholar]
- 14.Taramasso M, Vanermen H, Maisano F, Guidotti A, La Canna G, Alfieri O. The growing clinical importance of secondary tricuspid regurgitation. Journal of the American College of Cardiology. 2012;59(8):703–10. Epub 2012/02/22. 10.1016/j.jacc.2011.09.069 [DOI] [PubMed] [Google Scholar]
- 15.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. Journal of the American Society of Echocardiography: official publication of the American Society of Echocardiography. 2010;23(7):685–713; quiz 86–8. [DOI] [PubMed] [Google Scholar]
- 16.Zotter-Tufaro C, Duca F, Kammerlander AA, Koell B, Aschauer S, Dalos D, et al. Diastolic Pressure Gradient Predicts Outcome in Patients With Heart Failure and Preserved Ejection Fraction. Journal of the American College of Cardiology. 2015;66(11):1308–10. 10.1016/j.jacc.2015.07.011 [DOI] [PubMed] [Google Scholar]
- 17.Karakus G, Kammerlander AA, Aschauer S, Marzluf BA, Zotter-Tufaro C, Bachmann A, et al. Pulmonary artery to aorta ratio for the detection of pulmonary hypertension: cardiovascular magnetic resonance and invasive hemodynamics in heart failure with preserved ejection fraction. Journal of cardiovascular magnetic resonance: official journal of the Society for Cardiovascular Magnetic Resonance. 2015;17(1):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. Journal of cardiovascular magnetic resonance: official journal of the Society for Cardiovascular Magnetic Resonance. 2013;15:91. Epub 2013/10/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh JP, Evans JC, Levy D, Larson MG, Freed LA, Fuller DL, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). The American journal of cardiology. 1999;83(6):897–902. Epub 1999/04/06. [DOI] [PubMed] [Google Scholar]
- 20.Hung J, Koelling T, Semigran MJ, Dec GW, Levine RA, Di Salvo TG. Usefulness of echocardiographic determined tricuspid regurgitation in predicting event-free survival in severe heart failure secondary to idiopathic-dilated cardiomyopathy or to ischemic cardiomyopathy. The American journal of cardiology. 1998;82(10):1301–3, A10. [DOI] [PubMed] [Google Scholar]
- 21.Koelling TM, Aaronson KD, Cody RJ, Bach DS, Armstrong WF. Prognostic significance of mitral regurgitation and tricuspid regurgitation in patients with left ventricular systolic dysfunction. Am Heart J. 2002;144(3):524–9. Epub 2002/09/14. [DOI] [PubMed] [Google Scholar]
- 22.Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. Journal of the American College of Cardiology. 2004;43(3):405–9. Epub 2004/03/12. 10.1016/j.jacc.2003.09.036 [DOI] [PubMed] [Google Scholar]
- 23.Sagie A, Freitas N, Chen MH, Marshall JE, Weyman AE, Levine RA. Echocardiographic assessment of mitral stenosis and its associated valvular lesions in 205 patients and lack of association with mitral valve prolapse. Journal of the American Society of Echocardiography: official publication of the American Society of Echocardiography. 1997;10(2):141–8. Epub 1997/03/01. [DOI] [PubMed] [Google Scholar]
- 24.Varadarajan P, Pai RG. Prognostic implications of tricuspid regurgitation in patients with severe aortic regurgitation: results from a cohort of 756 patients. Interact Cardiovasc Thorac Surg. 2012;14(5):580–4. Epub 2012/02/22. PubMed Central PMCID: PMC3329311. 10.1093/icvts/ivr047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mascherbauer J, Kammerlander AA, Marzluf BA, Graf A, Kocher A, Bonderman D. Prognostic Impact of Tricuspid Regurgitation in Patients Undergoing Aortic Valve Surgery for Aortic Stenosis. PloS one. 2015;10(8):e0136024 10.1371/journal.pone.0136024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mascherbauer J, Maurer G. The forgotten valve: lessons to be learned in tricuspid regurgitation. European heart journal. 2010;31(23):2841–3. Epub 2010/08/24. 10.1093/eurheartj/ehq303 [DOI] [PubMed] [Google Scholar]
- 27.Mohammed SF, Hussain I, AbouEzzeddine OF, Abou Ezzeddine OF, Takahama H, Kwon SH, et al. Right ventricular function in heart failure with preserved ejection fraction: a community-based study. Circulation. 2014;130(25):2310–20. PubMed Central PMCID: PMCPMC4276536. 10.1161/CIRCULATIONAHA.113.008461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European heart journal. 2016;37(27):2129–200. 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 29.Tschope C, Westermann D. Heart failure with normal ejection fraction. Pathophysiology, diagnosis, and treatment. Herz. 2009;34(2):89–96. 10.1007/s00059-009-3197-6 [DOI] [PubMed] [Google Scholar]
- 30.Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. European heart journal. 2011;32(6):670–9. 10.1093/eurheartj/ehq426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gerges C, Gerges M, Lang MB, Zhang Y, Jakowitsch J, Probst P, et al. Diastolic pulmonary vascular pressure gradient: a predictor of prognosis in "out-of-proportion" pulmonary hypertension. Chest. 2013;143(3):758–66. Epub 2013/04/13. 10.1378/chest.12-1653 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.