Abstract
Objective
The purpose of this study was to assess the self-reported knowledge of concussion recognition and treatment with first-contact family medical and chiropractic practitioners by means of a pilot study of the need, construct validity, and feasibility for further investigation of mild traumatic brain injury (MTBI) knowledge base.
Methods
Two hundred forty-eight practicing chiropractic and 120 medical physicians in the south and northeastern sections of the United States were contacted by e-mail, telephone, and postal mail to answer an 18-item survey on knowledge, diagnosis, and common practice with respect to traumatic brain injury patients. Descriptive analysis was used to assess common trends.
Results
Twenty-three chiropractic and 11 medical primary care practitioners returned completed surveys, making this a low-power pilot study. The majority claimed confidence in diagnosis of MTBI, but a lack of knowledge of many of the assessment tools and the international guidelines. Chiropractic and medical clinicians revealed similar competencies and differing deficiencies. Both groups admitted infrequent diagnosis of MTBI in practice. There was recognition of major TBI signs, but lack of recognition or inquiry for subtle MTBI signs.
Conclusions
There is a need and feasibility for further study of the knowledge transfer to the chiropractic physician with a larger population. These findings correlate with similar medical practitioner studies, and may also support previous findings of underreporting of the prevalence of MTBI. The survey instrument appears to provide valid data on knowledge of MTBIs, with some modifications.
Key Indexing Terms: Brain Concussion; Knowledge; Diagnosis; Guideline; Primary Health Care; Chiropractic, Surveys and Questionnaires
Introduction
Concussion prevalence has been reported as being at the epidemic level by the U.S. Centers for Disease Control and Prevention.1 The leading causes of traumatic brain injuries (TBIs) are falls and motor vehicle accidents (MVAs).2, 3 The prevalence of concussion or mild traumatic brain injuries (MTBIs) has been reported to be 70% to 90% of all treated brain injuries,4 with it being present in 38% of MVA hospital admissions and 46% of trauma center admissions.5 In the age group of 15 to 44 years, MVAs are the leading cause of TBI hospital admissions.1 The frequency of MTBIs in sports is also significant. The sport prevalence has been reported as ranging from 2.5% to 18.9% of all participants, dependent on the sport and the level of activity.6, 7, 8, 9 The prevalence of MTBI in both MVA and sport injury patients may actually be higher than what has been reported.10, 11 Moreau et al11 propose that a low recognition rate by primary care chiropractic or family practitioners (PCPs) may be one of many reasons that result in underreporting. The frequency of these primary modes of injury with which people present to the PCP necessitates that the PCP have the requisite knowledge to question, evaluate, and treat MTBIs.
The type of TBI often determines the actions of the patient. A TBI is defined by the American Academy of Neurology as a trauma-induced alteration in mental status that may or may not involve a loss of consciousness.12 The type is graded (Table 1) as mild, moderate, or severe, contingent on the Glasgow Coma Scale, period of posttraumatic amnesia, and absence of or duration of loss of consciousness.13, 14, 15 Patients with severe brain injuries are commonly transferred to emergency rooms, where they can be evaluated by trauma specialists. Moderate brain injuries involve loss of consciousness longer than 5 minutes13, 16 (or 30 minutes by some classifications17), posttraumatic amnesia lasting from 1 to 24 hours, symptoms greater than 15 minutes in duration, and an initial decrease in verbal, motor, and/or eye response.13, 15, 18 These may be more likely to be recognized by the layperson who commonly seeks emergency or specialist care. However, even 63% of American Academy of Neurology member specialists have not received formal or informal training in sports neurology, including objective diagnostic criteria for concussion, and therefore may be missing some patients with delayed-onset symptoms.19 Mild brain injuries may not always be immediately recognizable by the layperson. They may not involve any loss of consciousness; any initial change in motor, verbal, or eye response; posttraumatic amnesia of less than an hour; and only transient or no confusion.20 Yet, these mild injuries can have other subtle signs such as selective loss of (anterograde and retrograde) memory, difficulty with continuous train of thought, cloudy thought process, decreased concentration, cognitive difficulties, transient losses of balance, disruption of sleep, fatigue, tinnitus, sensitivity to sound or light, headaches, diminished reaction time, changes in personality, and change in emotions.15, 20, 21
Table 1.
Modified Cantu Traumatic Brain Injury Classification System
| Mild/Grade 1 | Moderate/Grade 2 | Severe/Grade 3 | |
|---|---|---|---|
| Loss of consciousness | None | <5 min | >5 min |
| Posttraumatic amnesia | 1 hr | 1-24 h | >24h |
| Glasgow Coma Scale | 13-12 | 9-12 | 3-8 |
| Symptoms | Transient | >15 min | Prolonged symptoms |
Some MTBIs may commonly self-resolve in 7 to 10 days. However, risks exist if there is a lack of appropriate action for some of these cases. The patient may progress to postconcussive syndrome or may unknowingly be prone to second-impact syndrome. This can have more severe consequences, including permanent neurologic injury or death.22, 23 If care is sought, the MTBI type of patient may consult his or her PCP for the initial consult for concurrent neuromusculoskeletal injuries or the mild subtle indescribable signs noticed by significant others. In fact, one study reported that 20% to 56% of MVA patients consult a chiropractor (96% consult a medical doctor) in the respective 6-week to 12-month postaccident period.24 Early recognition of MTBI is therefore imperative.
Increased predoctoral and postdoctoral MTBI training could improve the provider’s abilities in early recognition, diagnosis, and care of the MTBI patient. Previous studies reported inconsistent provider actions and insufficient training of pediatricians and emergency room physicians to adequately recognize, diagnose, and treat TBI.25 There is a reported lack of awareness of concussion guidelines among pediatricians.26 Other studies have reported the deficient TBI knowledge of coaches,27, 28 medical students,29 emergency physicians, and family medical physicians.30 Knowledge of chiropractors has not been well researched, and there is a lack of any cohort medical doctor (MD)/doctor of chiropractic (DC) studies. Specific predoctoral training in diagnosis and management of TBI is not outlined by the Council on Chiropractic Accreditation Standards31 and may vary between different training programs. This article describes a pilot study investigating the use of a survey instrument in evaluating the degree of the primary-contact clinician’s knowledge base and ability to recognize the subtle presentation of MTBI. Resulting information may indicate the need for further study that could help guide future educational programs.
Purpose
The purpose of this study was to assess a survey instrument used to assess self-reported knowledge of concussion recognition and treatment with first-contact family medical and chiropractic practitioners. The intent was to assess1 the informative need for and feasibility of further investigation into the TBI knowledge base, and2 the construct validity of the questionnaire as a potential measurement tool for the concept of sufficient PCP knowledge base.
Methods
To survey the professions involved, a standardized set of questions needed to be developed that would allow independent investigation of the clinician’s TBI knowledge and common procedures performed with a TBI patient. The survey was designed with the objective of obtaining information on the knowledge and procedures of PCPs, when presented with a potential MTBI patient. The response rates would determine the feasibility of the targeted population. The specific question responses would help determine the content validity. The primary outcome objective was to obtain a 25% response rate for feasibility of the utilization of the recruitment population and clear consistent delineation of knowledge and correlation of responses to determine question content validity and the need for further investigation.
Instrument Development
Previous validated and published survey questions on methods of diagnosis, guideline utilization, and prognosis and treatment of concussions were used and some were further customized.26, 32, 33, 34, 35, 36 Specific questions were devised to provide insight into the baseline MTBI knowledge and clinical process of first-contact chiropractic and medical physicians in their evaluation and care of TBI patients. The questions were devised to reflect current concepts, guidelines, and clinical practice. These questions were critiqued and edited by all authors. An initial pilot test was performed with 3 doctors: a chiropractic neurologist (DC, DACNB), a chiropractor with degreed experience in public health and education (DC, MPH, EdD), and a dual-degree chiropractor pharmacologist (DC, DPh). None of these was included in the final results. Feedback was provided by those doctors. Subsequent edits were made to increase the clarity of the questions and the potential information. One question was added. Surveys were again reviewed by all authors, and edits were made. The institutional review board at Texas Chiropractic College approved this study. The survey was limited to 18 questions and 2 pages to keep it comprehensive but concise in order to increase the response rate.
The demographic analysis consisted of delineating general or family practitioners from specialists, and chiropractic physicians from medical physicians. Questions were geared mainly toward recognition and knowledge of types of patients that commonly present with MTBI, the frequency of known concussions in practice, and the diagnosis of MTBIs. Common knowledge and usage of different patient symptom questionnaires for the evaluation was investigated, along with the doctor’s typical consults and physical exam inquiries. Knowledge of current guidelines was also assessed (Table 2). Multiple-choice and 5-point Likert scale questions were used to assess the doctor’s self-reported degree of knowledge and comfort with diagnosing MTBIs, and the perceived frequency of seeing MTBIs in practice (Table 3).
Table 2.
PCP Knowledge of Assessment Tools and Guidelines
| Assessment | How Would You Describe Your Familiarity With the Clinical Tools Below? |
|||
|---|---|---|---|---|
| Very Familiar | Somewhat Familiar | Not Very Familiar | Not at All Familiar | |
| SCAT 2 |
||||
| SCAT 3 |
||||
| BESS |
||||
| IMPACT |
||||
| SAC |
||||
| ACE |
||||
| Zurich Guidelines | ||||
ACE, Acute Concussion Evaluation; BESS, Balance Error Scoring System; IMPACT, Immediate Post-Concussion Assessment and Cognitive Test; PCP, primary care chiropractic or family practitioner; SAC, Standardized Assessment of Concussion; SCAT, Sport Concussion Assessment Tool.
Table 3.
Survey of PCP Knowledge of MTBI
| Survey Question | Choices | |
|---|---|---|
| I feel knowledgeable enough to recognize and diagnose a mild, moderate, or severe traumatic brain injury case. | a. Never b. Rarely c. Often d. Always confident |
|
| Postconcussive patients may present with (circle any that apply): | a. Fatigue b. Insomnia c. Change in balance d. Blurred vision e. Weakness f. Paresthesias |
|
| Subconcussions are: | a. Associated with whiplash b. Occur under water and involve cerebrospinal fluid pressure c. Classified as less severe than a mild traumatic brain injury d. Affect cellular glucose metabolism and can be chronic |
|
| The leading causes of traumatic brain injuries are: | a. Sports b. Football c. Falls, motor vehicle accidents, blows to the head d. Assaults e. Domestic violence |
|
| On evaluation of sports impact injuries and/or motor vehicle accident victims, I inquire about cognitive symptoms. | a. Never b. 10% of the time c. 50% of the time d. Always |
|
| During history taking of post sport impact or motor vehicle accident injuries, I inquire to family members or friends (or inquire about family/friend comments) about cognitive changes, memory loss, or personality and emotional changes. | a. Never b. 10% of the time c. 50% of the time d. Always |
|
| I diagnose a traumatic brain injury, concussion, or postconcussive syndrome in practice. | a. Never b. Infrequently c. Frequently d. Often |
|
| Which of the following signs or symptoms are recognized as results of mild brain trauma? (circle all that apply) | a. Irritability b. Tachycardia c. Sleep disturbance d. Light sensitivity e. Sound sensitivity |
f. Convulsions g. Weakness h. Depression i. Memory problems j. Headache |
| Survey Question | Strongly Agree | Agree | Neither Agree nor Disagree | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| Traumatic brain injuries and/or concussions can result from impact or nonimpact injuries to the head. | 1 | 2 | 3 | 4 | 5 |
| To be diagnosed, a “traumatic brain injury” must always be accompanied by a loss of consciousness. | 1 | 2 | 3 | 4 | 5 |
| Patients always have a self-awareness of whether they incurred a concussion or traumatic brain injury. | 1 | 2 | 3 | 4 | 5 |
| Postconcussive syndrome and second-impact syndrome symptoms are always of short duration. | 1 | 2 | 3 | 4 | 5 |
| Mild traumatic brain injury cannot result in long-term sequelae. | 1 | 2 | 3 | 4 | 5 |
| Upper cervical spine injuries can mimic symptoms of concussion and postconcussive syndrome. | 1 | 2 | 3 | 4 | 5 |
MTBI, mild traumatic brain injury; PCP, primary care chiropractic or family practitioner.
Study Design
The targeted database of subjects was generated through the following populations1: Texas Chiropractic College Alumni database,2 personal contacts of the authors, and3 solicitation of local medical groups.
All surveys were blinded as to the participant. No incentives were given to complete the survey, but the participants were promised to be informed of the results. All doctors were given information on the study with an invitation to participate. Those doctors who were initially contacted by e-mail were asked to respond directly via e-mail with either a yes or no to indicate their desire to participate. Those who did not respond were followed up by telephone. There were 248 chiropractic physicians contacted by e-mail with an invitation to participate in the study. Subsequent follow-up of 115 chiropractors via telephone was conducted; 46 subsequently expressed a willingness to participate, and 23 responded with completed survey. Medical physician e-mails were not available. Therefore, 120 medical physicians were contacted by telephone, and 60 were followed up by postal mail. Medical physicians who were known by the authors were contacted first by introductory postal mail and followed up by telephone. Thirteen expressed a willingness to participate, and 11 responded with completed surveys. Additional local Houston medical physicians were also initially contacted by telephone. Once consent to participate was indicated, a survey and cover letter were sent in a 15 × 12-in manila envelope with 10 smaller 8½ × 11-in surveys and self-addressed, stamped envelopes inside, by U.S. postal mail to all chiropractic and medical practitioners who expressed interest in participating (Fig 1).
Fig 1.
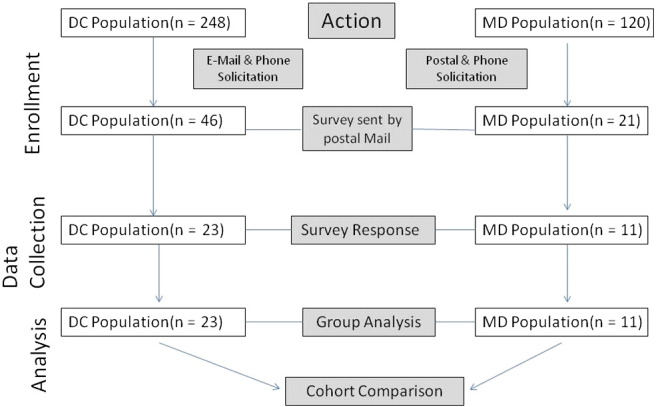
Method diagram.
Participant Recruitment
There was a targeted population of a geographic distribution between the South, Southwest, and Northeast and first-contact family and general medical and chiropractic practitioners versus specialists. The target population was intended to represent the family DCs and MDs most likely to see MTBIs vs moderate or severe cases and to recruit doctors with different regional educations. Medical physician responses were mainly from Texas and Massachusetts. Chiropractic physician responses were distributed throughout the areas mentioned, with a large percentage coming from Massachusetts and Texas. The study looked at such variables as type of practitioner, knowledge of the patient survey instruments, guidelines for care, recognition of typical subtle symptoms of MTBIs, and typical clinical procedures.
Study Participant Implied Consent
All doctors participating in the study provided their implied consent by voluntarily completing the survey, as per the instructions listed on the survey, and mailing it back to the research office.
Statistical Analysis
Survey results were entered into a table in Excel (Microsoft, Redmond, WA). Data were then exported and analyzed in SPSS Version 20.0 (IBM, Armonk, NY). Descriptive statistics were used to illustrate the number of responses and overall percentage of responses for each survey question option. In most of the Results section, the percentage values were followed by a colon and the actual number of positive respondents to the given question divided by the entire sample size for that given question.
Results
The survey response rate was 9.3% for DCs and 9.2% for MDs from the initial database. Among those who were mailed the survey, the response rates were 50% for DCs and 52% for MDs. Geographic distribution of the initial solicited population of DCs included the states of Massachusetts (50%), Texas (25%), and an even distribution of Florida, Louisiana, New Mexico, California, New York, Arizona, Ohio, Maryland, North Carolina, Oklahoma, Minnesota, Alabama, Montana, Nevada, South Dakota, North Carolina, Idaho, New Jersey, New Hampshire Pennsylvania, Illinois, and Nebraska. The response was similar in the distribution. Geographic distribution of the MD solicitation was unable to be as broad and consisted of the states of Texas, Florida, and Massachusetts. Although the surveys were blinded, the geographic response was observed through the postmarks. The overall response appeared to reflect the distribution, with the majority of responses coming from Texas, Massachusetts, and Florida.
Twenty-three DCs and 11 MDs completed the survey. The most commonly reported chiropractic specialty was sports chiropractic (18.2%: 4/23), but 68% had no specialty. The most commonly reported medical specialty was family practice (54.5%: 6/11). When combining “often” and “always confident” response options, MDs self-reported being more knowledgeable about diagnosing mild, moderate, or severe TBIs (90.9%: 10/11) compared with DCs (82.6%: 19/23), but the majority in both groups did feel confident on diagnosis.
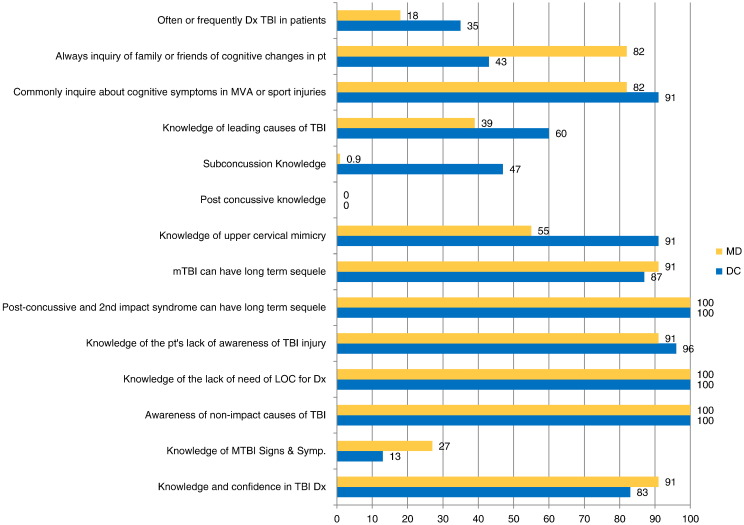
The survey supported that the majority were aware of the primary symptoms, but not the assessment tools. Only 13% of the DCs and 27% of the MDs were able to correctly identify all common symptoms of MTBIs. Medical physicians were not as aware of the cervical injury mimicry of TBI. Despite their confidence, both groups admitted that they infrequently diagnose a concussive disorder in practice (81% MDs, 65% DCs). The most common symptom both groups of doctors reported after MTBI was headache. Both groups of doctors stated they strongly agree that TBI or concussion, or both, can result from impact or nonimpact injuries (no direct external blow to skull) to the head. Chiropractic and medical doctors both stated they strongly disagreed that TBI must always be accompanied by a loss of consciousness for diagnosis. Most responses of chiropractic and medical physicians were similar throughout the survey. Postconcussive knowledge was lacking in both groups. No respondent correctly identified all common symptoms. Subconcussive symptoms were known by 48% of the DCs (11/23), but only 1 MD (of 11) (Fig 2).
Fig 2.
Comparison of knowledge of medical doctors (MD) and doctors of chiropractic (DC).
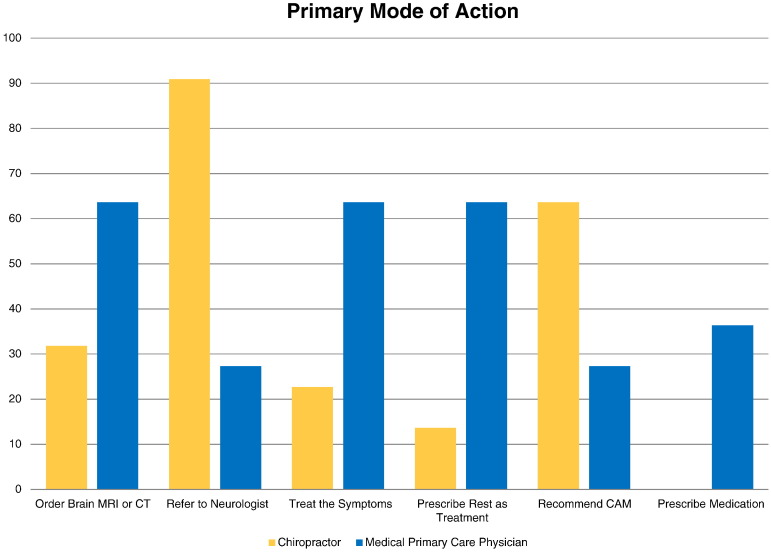
If a TBI was suspected, the DC would most commonly refer to a neurologist, whereas the MD would be more likely to order imaging such as magnetic resonance imaging (MRI) and computed tomography, prescribe rest, and treat the symptoms (Fig 3).
Fig 3.
Primary mode of action. CT, computed tomography; MRI, magnetic resonance imaging; CAM, complementary and alternative medicine.
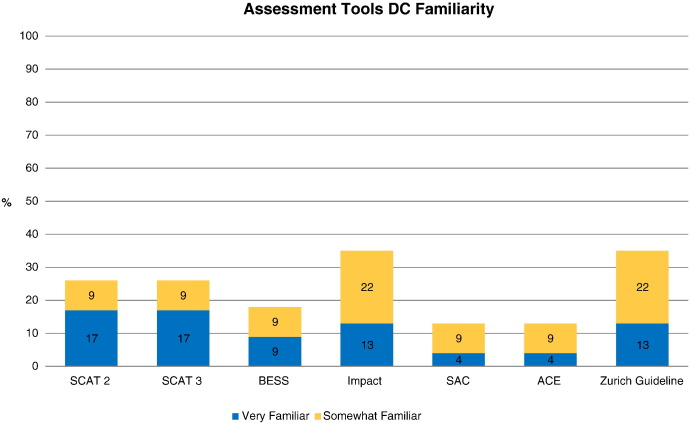
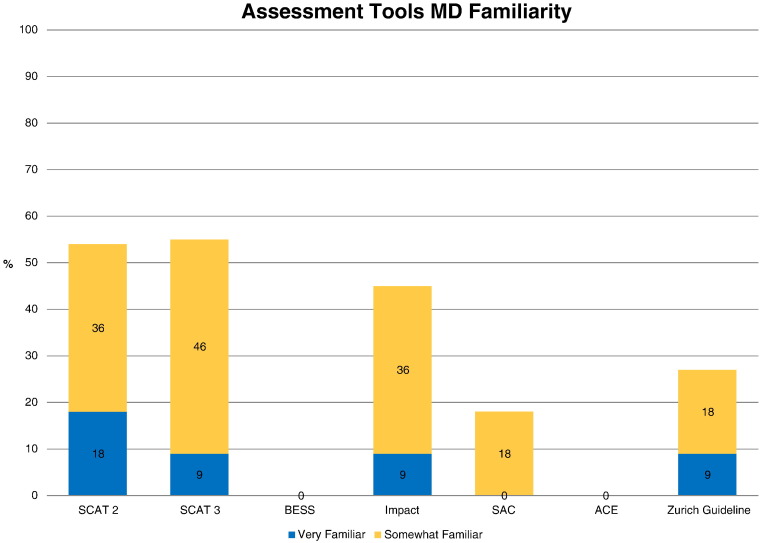
One item worth mentioning is that DCs more rarely reported asking family members or friends of the patient about cognitive changes they may have observed. Only 42.9% (9/23) of DCs reported that they always asked this compared with 81.8% (9/11) of MDs. Additionally, there appeared to be a difference in the surveys with which DCs and MDs were familiar (Fig 4, Fig 5). Chiropractic doctors were more familiar with the Balance Error Scoring System (BESS), Acute Concussion Evaluation (ACE), and Zurich guidelines than MDs. On the other hand, MDs were more familiar with Sport Concussion Assessment Tool 2 (SCAT2), SCAT3, Immediate Post-Concussion Assessment and Cognitive Testing (IMPACT), and Standardized Assessment of Concussion (SAC) guidelines than DCs. Overall, neither group had much familiarity with the common assessment tools.
Fig 4.
Familiarity of doctors of chiropractic (DCs) with patient assessment tools. ACE, Acute Concussion Evaluation; BESS, Balance Error Scoring System; SCAT2,3 Sport Concussion Assessment Tool 2(3).
Fig 5.
Familiarity of medical doctors (MDs) with patient assessment tools. ACE, Acute Concussion Evaluation; BESS, Balance Error Scoring System; SCAT2,3 Sport Concussion Assessment Tool 2(3).
Discussion
The reporting of concussions is dependent on the ability of the practitioner to diagnose them. The symptoms of MTBIs with which people present to the practitioner's office can vary and often are not overt. The patient may not be aware of the signs and symptoms or might be hiding them because of either embarrassment or a fear of restrictions in athletics, work, or play. Even those MTBI patients brought to the emergency room may be discharged without a TBI diagnosis because of the temporal delay of onset of some symptoms37 or the lack of recognition of the changes in cognitive function by the patient. As a result of the decreased frequency of such patients presenting with TBI as the primary complaint, a PCP in a private office may be less likely to have sufficient experience in recognizing the subtle signs or inquiring appropriately in the consult, as compared with the emergency room physician or specialist. The PCP patients often may present to the PCP with primary trauma-related complaints other than those directly related to the concussion. The primary complaint may necessitate that the provider's attention be drawn away from some of the subtle TBI symptoms. It is therefore hypothesized that concussions may be an underreported and underdiagnosed injury.
There has been extensive outreach of education to laypersons involved in sports to improve the recognition of TBIs.21 According to the Concussion in Sport Group (Federation Internationale de Football Association, International Ice Hockey Federation, and International Olympic Committee), “as the ability to treat or reduce the effects of concussive injury after the event is minimal, education of athletes/colleagues and the general public is a mainstay of progress in the field of concussion.”5 Early recognition and enhanced education and awareness of the appropriate care and the risks of lack of care affect the outcome of the patient.
A similar educational outreach to PCPs has not been as extensive as the implementation of education programs to laypersons, such as parents and coaches involved in sports. In the United States, it was found that only 12.7% of MDs obtained their information through medical school training. The majority found it necessary to take continuing education credits to obtain the knowledge.36 Lebrun et al reported in 2012 that one-third of Canadian family physicians received their concussion knowledge primarily from colleagues, websites, and medical school training. Their survey concluded that family physicians may be managing concussions in an inconsistent manner with current information.36 Studies of medical students and neurology/neurosurgery residents revealed that 32% were either sure they never learned about concussions or could not remember if they had ever learned about concussions in their undergraduate medical education,29 whereas other studies indicated that 63% of neurologists did not receive the MTBI education.19 The Zurich guidelines acknowledge the need for more knowledge transfer,21, 38 and others report that it is critical for evidence-informed practices to implement new information and make the best clinical decisions.39 Concussion history, examination, and recognition may be taught in an abbreviated fashion in Emergency Medicine or Clinical Neurology classes at some accredited chiropractic colleges, but is not specifically required by the accrediting body.31, 40 Given the different state scope of practice laws, there may be a void of availability of TBI continuing education for the chiropractor. The aforementioned findings raise concern over the carry forward of sufficient information and the clinical implementation of the knowledge of brain injuries in relation to both diagnosis and treatment for MTBIs for first-contact MDs32 and DCs. A literature search reveals a lack of studies on the knowledge transfer of concussion information in practicing DCs, making this a unique population for investigation.
The purpose of this study was to identify the need for further evaluation of the concussion knowledge transfer, to assess the feasibility of the study, to evaluate the survey construct validity of the instrument in assessing the level of knowledge transfer, and to gain insight into the utilization of current principles and tools in the recognition and diagnosis of MTBI (concussion) between disciplines. The results of this study imply a possible lack of sufficient knowledge transfer of many of the most up-to-date evaluation tools used to assess patients, but there was a demonstrated overconfidence of both types of PCP in the diagnosis of MTBI (combined 82% of DCs and 91% of MDs). The lack of knowledge surprisingly correlated with Covassin et al’s survey of athletic trainers (ATs) and AT program directors, 72% of whom did not use BESS in the assessment.33 However, the ATs and AT program directors in the study by Covassin et al used mainly the symptom checklist as a tool, and this study revealed that both DCs (87%) and MDs (82%) were either not very familiar or not at all familiar with the Standard Assessment of Concussion symptom tool.33 The ability to recognize MTBI is dependent on the knowledge to inquire and examine the patient and use the appropriate assessment tools. Moreau et al refer to a number of additional reporting, training, and cultural complicating variables that result in underreporting of the diagnosis of TBI.11 The prevalence of TBI may therefore be higher than commonly reported, for numerous reasons.11 In this case it is suggested that 1 reason may be the lack of inquiry about or recognition of the subtle signs of MTBI or the lack of sufficient utilization of common assessment tools by the PCP. Further study is therefore warranted for external validation. This lack of knowledge can result in insufficient care of the concussed patient and place the patient at increased risk of second-impact syndrome during the acute phase of the concussion.23 The patient may also progress to postconcussive syndrome with more prolonged symptoms.12, 41
Recently, the public has become more aware of TBI because of its occurrence and subsequent sequelae in professional athletes. The sports in which TBIs are most frequent include men’s football, women’s soccer, pedal cycling,34 and hockey. It was found that 5% to 9% of all sport-related injuries are brain injuries.33 The importance of concussion knowledge transfer is further appreciated when we realize that the majority of causes of TBI are not sport-related concussions. Traumatic brain injuries are more commonly caused by the MVAs and fall-induced concussion.1, 5 There has been little public education with respect to these causes. This places greater responsibility to detect TBIs on the PCP. This study illustrates that there may be a need to study dissemination of the latest common guidelines and means of evaluation in a larger PCP population, especially the chiropractic physician population. This is inferred from1 the low level of knowledge of common signs and symptoms of MTBIs and2 the unfamiliarity or low familiarity of MDs (72%) and DCs (65%) with the latest consensus Zurich guidelines for evaluation and management of concussion.21, 38
These figures parallel Carl and Kinsella’s26 and Gordon et al’s35 findings of only 14% and 18% utilization of the Zurich guidelines by pediatricians. The Zurich guidelines also recommend improved methods of knowledge transfer, but addressed mainly the public’s need.21, 38 No attention was given to the needs of the PCP for knowledge transfer. This study implies that there may be a similar knowledge transfer problem with chiropractic PCPs and parallels other studies performed on medical practitioners,19, 30 indicating the need for further study. This study is unique in that it is the first study performed on primary-contact chiropractic physicians.
Both types of PCP clinicians were not familiar with many evaluation tools. Balance Error Scoring System was especially unfamiliar to both (combined “not very familiar” and “not at all familiar”; DCs = 82%; MDs = 100%). This is a simple test that can be performed in the office, but it is apparently not being integrated into examination. It is noted that 55% of MDs are familiar with the SCAT3 assessment tool, although the study did not inquire whether they used it. In contrast, only 26% of DCs were familiar with it. This implies that this tool, which is recommended primarily for use in the doctor’s office, may not be used very often in the chiropractic office. The SCAT3 integrates symptom assessment with cognitive testing, neurologic examination, and BESS testing. There appears to be a need to introduce this into education of the predoctoral student. The preliminary findings that both types of general practitioners infrequently diagnose concussive disorders (82% of MDs, 65% of DCs) suggest that they are missing the diagnosis of these patients as a result of their lack of use of the evaluation tools or their lack of knowledge of the subtle symptoms. This suggestion warrants further study.
The Concussion in Sport Group points out the fact that minimal treatment is available for concussion.21 This study therefore took the liberty to inquire what common treatments were rendered by PCPs. The results confirm that a variety of actions is rendered (Fig 3). Doctors of chiropractic primarily referred the patient to a neurologist. This correlates with Zonfrillo et al,25 who reported on pediatric providers’ self-reported knowledge of concussion. They reported that the majority of PCPs referred concussion patients to specialists because of their lack of comfort in managing concussions. One might therefore question whether the DC recognizes that treatment of spine, musculoskeletal, and head pain can facilitate recovery from MTBIs.22
Kerr et al report a distinct difference (40%) between athletes’ recall of concussion and clinically documented concussions. The reasons for the disparity included not informing the medical staff, not thinking it was serious, not knowing it was a concussion until they were later educated about the symptoms, and not wanting to leave current or future play.42 Some of these reasons may also apply to patients who suffer concussions in MVA or falls. All these types of patients who first consult with DCs, pediatricians, and family medical physicians may not be evaluated sufficiently by PCPs to catch these “patient unreported” concussions. This study exposes the need for increased opportunities for and methods of dissemination of material to PCPs for knowledge transfer of concussion, inquiry, recognition, and diagnosis. Finch et al suggest that there is a need to improve dissemination of the current guidelines.43 For the chiropractic profession, education begins at the predoctoral level and continues through the continuing education requirements for licensed doctors. The brief predoctoral coverage of this topic may need to become more comprehensive. It is suggested that educational programs introduce students to the following information:
-
1
CDC Heads Up Facts for Physicians about MTBI44
-
2
Sport Concussion Assessment Tool 345
-
3
2013 Zurich Guidelines for diagnosis and management of TBIs38
-
4
Balance Error Scoring System46
Postgraduate courses are also available at various institutions. These may need to be further developed through the process of dissemination to the established practitioners. Johnson et al’s study concludes with the need for DCs to become more aware of current guidelines and assessment tools.37 This study concurs with Lebrun et al36 regarding the need for better dissemination and knowledge transfer of assessment tools and current guidelines to first-contact medical physicians.
This pilot study found prospective professional differences in particular aspects of recognition of the TBI patient, but was statistically inconclusive, indicating a need for further study. The survey of MDs revealed unfamiliarity with cervical mimicry and the BESS screening tool, whereas DCs were less familiar with SCAT3. Both groups had minimal familiarity with the Zurich guidelines. The survey revealed common symptom recognition for diagnosis of grade 2 and 3 TBIs by both MDs and DCs and little difference in competencies. This study implies a need for further study of the lack of knowledge of common assessment tools and current guidelines for diagnosis and management of concussion patients in both groups.
This study revealed an insufficient database of MDs, and therefore the results from the MD PCP population are inconclusive. The low MD response may have resulted from the lack of an initial relationship with or knowledge of the authors and the lack of reimbursement for time taken from their reimbursable services. Further study involving the medical profession may not be feasible unless there is either increased funding or other incentives for the participants or access to a captive population (such as at a conference). The access to an increased database and the 50% response rate of DCs do appear to indicate the feasibility of pursuing knowledge transfer to chiropractic physicians. To increase the diversity of predoctoral educational and geographic distribution, it would be appropriate to pursue a larger multicenter study with data from other chiropractic doctoral institutions and their respective alumni. This would improve the generalizability and feasibility of a future study.
Construct validity can be improved by constructing the questions to better emphasize a grade 1 TBI, improving delineation of choices to obtain further insight and decreasing the number of questions to improve response rates.
Limitations and Future Studies
There was a limited population and limited responses. Therefore, conclusions cannot be extrapolated beyond this sample. The low numbers create a statistical weakness in external validity. Further study of a larger population would provide more conclusive data. In addition, there was an imbalance of 2:1 group sample responses and a limited geographic distribution of responses, which may have introduced a geographic bias.
It is concluded that the feasibility of the cohort study with medical practitioners would require more funding and better access to populations. The response rate indicated that further study of chiropractic practitioners is feasible. The data accumulated indicated the worthiness of a more robust study. This new study would need to involve a larger population or more than 1 center to capture sufficient data for generalizability or external validity. It may also allow increased survey expert review to improve validity. A future study might also include use of a revised survey with chiropractors and comparison of results with previous MD studies. Revision of some questions would be appropriate to emphasize grade 1 TBIs and improve internal construct validity.
Conclusions
This study indicated that assessment of the self-reported knowledge of concussion recognition and treatment of first-contact family medical and chiropractic practitioners is feasible. Further study of knowledge transfer to the chiropractic physician in a larger population is needed and feasible. These findings correlate with similar medical practitioner studies, and may also support previous findings of underreporting of the prevalence of MTBIs. The survey instrument appears to provide valid data on knowledge of MTBIs, with some modifications.
Acknowledgments
The authors thank Dr. John Ward for his guidance during this study.
Funding Sources and Potential Conflicts of Interest
No funding sources or conflicts of interest were reported for this study
Contributorship Information
Concept development (provided idea for the research): D.N.T.
Design (planned the methods to generate the results): D.N.T., S.J.D.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): D.N.T.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): D.N.T.
Literature search (performed the literature search): D.N.T.
Writing (responsible for writing a substantive part of the manuscript): D.N.T.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): D.N.T., S.J.D.
Participant recruitment: D.N.T., F.J.P.
Practical Applications
-
•
Increased clinical recognition of MTBI is warranted.
-
•
Improved education in the utilization and application of the standard assessment tools to a post-traumatic head injury patient may improve recognition and allow earlier treatment.
-
•
Training in practice integration of the assessment tools in the professional and continuing education programs may be beneficial.
Alt-text: Image 1
References
- 1.Centers for Disease Control and Prevention (CDC) Percent distributions of TBI-related hospitalizations by age group and injury mechanism—United States, 2006-2010. 2014. http://www.cdc.gov/traumaticbraininjury/data/dist_hosp.html [updated 2014; cited]. Available at. Accessed January 4, 2015.
- 2.Langlois JA, Sattin RW. Traumatic brain injury in the United States: research and programs of the Centers for Disease Control and Prevention (CDC) J Head Trauma Rehabil. 2005;20(3):187–188. doi: 10.1097/00001199-200505000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–548. doi: 10.1097/00001199-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Cassidy JD, Carroll LJ, Peloso PM. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;43:28–60. doi: 10.1080/16501960410023732. [suppl] [DOI] [PubMed] [Google Scholar]
- 5.Dischinger P, Read K, Kerns T. Causes and outcomes of mild traumatic brain injury: an analysis of CIREN data. Annu Proc Assoc Adv Automot Med. 2003;47:577–589. [PMC free article] [PubMed] [Google Scholar]
- 6.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Harmon KG, Drezner J, Gammons M. American Medical Society for Sports Medicine position statement: concussion in sport. Clin J Sport Med. 2012;23(1):1–18. doi: 10.1097/JSM.0b013e31827f5f93. [DOI] [PubMed] [Google Scholar]
- 8.Houck Z, Asken B, Bauer R, Pothast J, Michaudet C, Clugston J. Epidemiology of sport-related concussion in an NCAA Division I Football Bowl Subdivision Sample. Am J Sports Med. 2016;44(9):2269–2275. doi: 10.1177/0363546516645070. [DOI] [PubMed] [Google Scholar]
- 9.Daneshvar DH, Nowinski CJ, McKee AC, Cantu RC. The epidemiology of sport-related concussion. Clin Sports Med. 2011;30(1):1–17. doi: 10.1016/j.csm.2010.08.006. [vii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kohn L. Concussion in high school sports: overall estimate of occurrence is not available, but key state laws and nationwide guidelines address injury management. GAO-10-569T. 2010. http://www.gao.gov/products/GAO-10-569Thttp://www.gao.gov/assets/130/124717.pdf [updated 2010; cited]. Available at. Accessed March 28, 2015.
- 11.Moreau WJ, Nabhan DC, Walden T. Sport concussion knowledge and clinical practices: a survey of doctors of chiropractic with sports certification. J Chiropr Med. 2015;14(3):169–175. doi: 10.1016/j.jcm.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giza CC, Kutcher JS, Ashwal S. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80(24):2250–2257. doi: 10.1212/WNL.0b013e31828d57dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Academy of Neurology (AAN) Practice parameter: the management of concussion in sports—report of the Quality Standards Subcommittee. Neurology. 1997;48:581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 14.Cantu R. Concussion classification: ongoing controversy. In: Slobounov S, Sebastianelli W, editors. Foundations of Sport-Related Brain Injuries. Springer Science and Business Media; New York, NY: 2006. pp. 87–110. [Google Scholar]
- 15.Marshall S, Bayley M, McCullagh S, Velikonja D, Berrigan L. Clinical practice guidelines for mild traumatic brain injury and persistent symptoms. Can Fam Physician. 2012;58(3):257–267. [e128-e140] [PMC free article] [PubMed] [Google Scholar]
- 16.Cantu R, editor. Foundations of Sport-Related Brain Injuries. Springer Science and Business; New York, NY: 2006. p. 92. [Google Scholar]
- 17.Friedland D. Improving the classification of traumatic brain injury: the Mayo classification system for traumatic brain injury severity. J Spine. 2013;S4:005. [Google Scholar]
- 18.Malec JF, Brown AW, Leibson CL. The Mayo classification system for traumatic brain injury severity. J Neurotrauma. 2007;24(9):1417–1424. doi: 10.1089/neu.2006.0245. [DOI] [PubMed] [Google Scholar]
- 19.Conidi FX, Drogan O, Giza CC, Kutcher JS, Alessi AG, Crutchfield KE. Sports neurology topics in neurologic practice: a survey of AAN members. Neurol Clin Pract. 2014;4(2):153–160. doi: 10.1212/01.CPJ.0000437697.63630.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Defense . 2010. Mild Traumatic Brain injury—Concussion: Pocket Guide for Clinicians. [updated 2010. Available at www.publichealth.va.gov/docs/exposures/TBI-pocketcard.pdf. Accessed February 8, 2016] [Google Scholar]
- 21.McCrory P, Meeuwisse WH, Aubry M. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport, Zurich, November 2012. J Athl Train. 2013;48(4):554–575. doi: 10.4085/1062-6050-48.4.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donovan J, Cancelliere C, Cassidy JD. Summary of the findings of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Chiropr Man Therap. 2014;22(1):38. doi: 10.1186/s12998-014-0038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cantu RC. Second-impact syndrome. Clin Sports Med. 1998;17(1):37–44. doi: 10.1016/s0278-5919(05)70059-4. [DOI] [PubMed] [Google Scholar]
- 24.Hartvigsen J, Boyle E, Cassidy JD, Carroll LJ. Mild traumatic brain injury after motor vehicle collisions: what are the symptoms and who treats them? A population-based 1-year inception cohort study. Arch Phys Med Rehabil. 2014;95(3, Suppl):S286–S294. doi: 10.1016/j.apmr.2013.07.029. [DOI] [PubMed] [Google Scholar]
- 25.Zonfrillo MR, Master CL, Grady MF, Winston FK, Callahan JM, Arbogast KB. Pediatric providers' self-reported knowledge, practices, and attitudes about concussion. Pediatrics. 2012;130(6):1120–1125. doi: 10.1542/peds.2012-1431. [DOI] [PubMed] [Google Scholar]
- 26.Carl RL, Kinsella SB. Pediatricians' knowledge of current sports concussion legislation and guidelines and comfort with sports concussion management: a cross-sectional study. Clin Pediatr (Phila) 2014;53:689–697. doi: 10.1177/0009922814526979. [DOI] [PubMed] [Google Scholar]
- 27.Naftel KG, Yust EM, Nichols MH, King WD, Davis D. Knowledge and management of sports concussions among coaches and certified athletic trainers in Alabama. South Med J. 2014;107(7):418–423. doi: 10.14423/SMJ.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 28.O’Donoghue EM, Onate J, Van Lunen B, Peterson CL. Assessment of high school coaches' knowledge of sport-related concussions. Athletic Train Sports Health Care. 2009;1(3):120–132. [Google Scholar]
- 29.Boggild M, Tator CH. Concussion knowledge among medical students and neurology/neurosurgery residents. Can J Neurol Sci. 2012;39(3):361–368. doi: 10.1017/s0317167100013524. [DOI] [PubMed] [Google Scholar]
- 30.Stoller J, Carson JD, Garel A. Do family physicians, emergency department physicians, and pediatricians give consistent sport-related concussion management advice? Can Fam Physician. 2014;60(6):548. [550-552] [PMC free article] [PubMed] [Google Scholar]
- 31.Council on Chiropractic Education (CCE) Author; Scottsdale, AZ: 2013. CCE Accreditation Standards. Principles, Processes & Requirements for Accreditation. [Available at http://www.cce-usa.org/uploads/2013_CCE_ACCREDITATION_STANDARDS.pdf] [Google Scholar]
- 32.Chrisman SP, Schiff MA, Rivara FP. Physician concussion knowledge and the effect of mailing the CDC's "Heads Up" toolkit. Clin Pediatr (Phila) 2011;50(11):1031–1039. doi: 10.1177/0009922811410970. [DOI] [PubMed] [Google Scholar]
- 33.Covassin T, Elbin R, III, Stiller-Ostrowski JL. Current sport-related concussion teaching and clinical practices of sports medicine professionals. J Athl Train. 2009;44(4):400–404. doi: 10.4085/1062-6050-44.4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferrara MS, McCrea M, Peterson CL, Guskiewicz KM. A survey of practice patterns in concussion assessment and management. J Athl Train. 2001;36(2):145–149. [PMC free article] [PubMed] [Google Scholar]
- 35.Gordon KE, Do MT, Thompson W, McFaull S. Concussion management by paediatricians: a national survey of Canadian paediatricians. Brain Inj. 2013;28(3):311–317. doi: 10.3109/02699052.2013.862740. [DOI] [PubMed] [Google Scholar]
- 36.Lebrun CM, Mrazik M, Prasad AS. Sport concussion knowledge base, clinical practises and needs for continuing medical education: a survey of family physicians and cross-border comparison. Br J Sports Med. 2012;47(1):54–59. doi: 10.1136/bjsports-2012-091480. [DOI] [PubMed] [Google Scholar]
- 37.Johnson CD, Green BN, Nelson RC, Moreau B, Nabhan D. Chiropractic and concussion in sport: a narrative review of the literature. J Chiropr Med. 2013;12(4):216–229. doi: 10.1016/j.jcm.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCrory P, Meeuwisse WH, Aubry M. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. J Sports Med. 2013;47(5):250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 39.Provvidenza CF, Johnston KM. Knowledge transfer principles as applied to sport concussion education. Br J Sports Med. 2009;43(suppl 1):i68–i75. doi: 10.1136/bjsm.2009.058180. [DOI] [PubMed] [Google Scholar]
- 40.Reichel S. Texas Chiropractic College; Pasadena, TX: 2016. Emergency Procedures Course Syllabus: Texas Chiropractic College, Division of Chiropractic Sciences. [Google Scholar]
- 41.Willer B, Leddy JJ. Management of concussion and post-concussion syndrome. Curr Treat Options Neurol. 2006;8(5):415–426. doi: 10.1007/s11940-006-0031-9. [DOI] [PubMed] [Google Scholar]
- 42.Kerr ZY, Mihalik JP, Guskiewicz KM, Rosamond WD, Evenson KR, Marshall SW. Agreement between athlete-recalled and clinically documented concussion histories in former collegiate athletes. Am J Sports Med. 2015;43(3):606–613. doi: 10.1177/0363546514562180. [DOI] [PubMed] [Google Scholar]
- 43.Finch CF, McCrory P, Ewing MT, Sullivan SJ. Concussion guidelines need to move from only expert content to also include implementation and dissemination strategies. Br J Sports Med. 2013;47(1):12–14. doi: 10.1136/bjsports-2012-091796. [DOI] [PubMed] [Google Scholar]
- 44.Center for Disease Control and Prevention, U.S. Department of Health and Human Services Heads Up—Facts for Physicians About Mild Traumatic Brain Injury (MTBI) http://www.concussiontreatment.com/images/CDC_Facts_for_Physicians_booklet.pdf Available at. Accessed May 14, 2016.
- 45.Concussion in Sport Group SCAT 3. Br J Sports Med. 2013;47(5):259. [Google Scholar]
- 46.Bell DR, Guskiewicz KM, Clark MA, Padua DA. Systematic review of the balance error scoring system. Sports Health. 2011;3(3):287–295. doi: 10.1177/1941738111403122. [DOI] [PMC free article] [PubMed] [Google Scholar]